The Role of a Simulation-Based Activity on Student Perceptions of Parenteral Nutrition Education
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
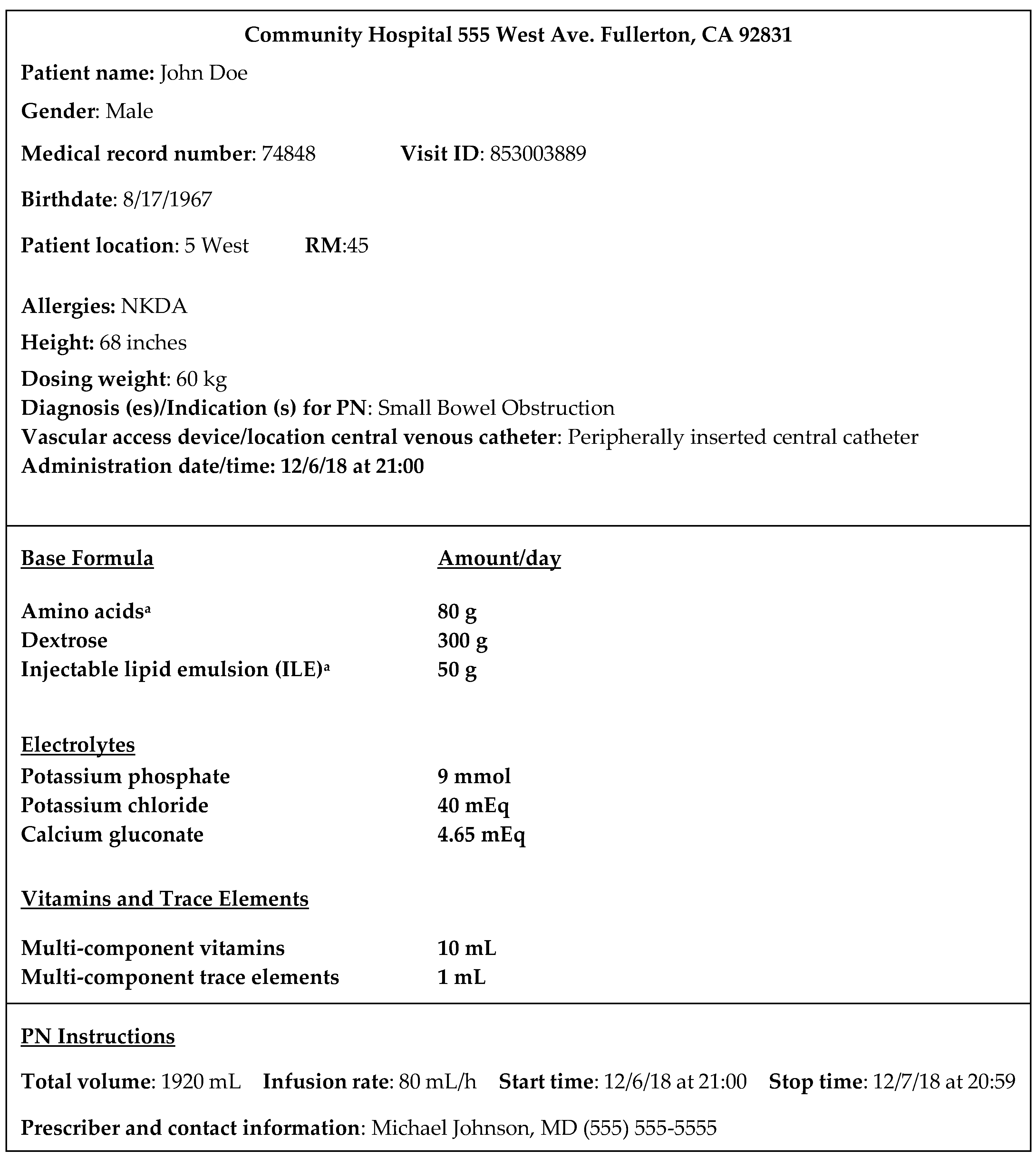
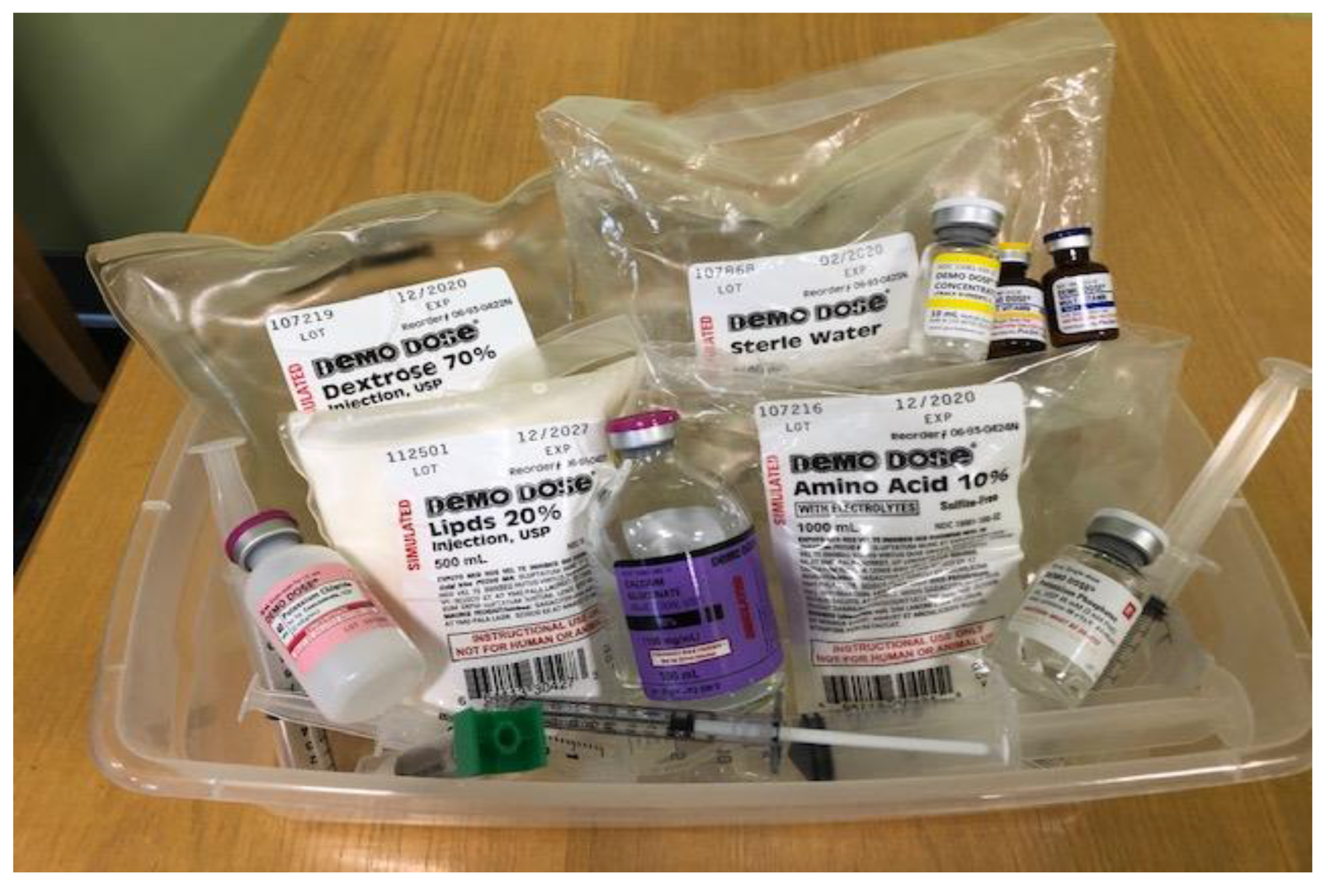
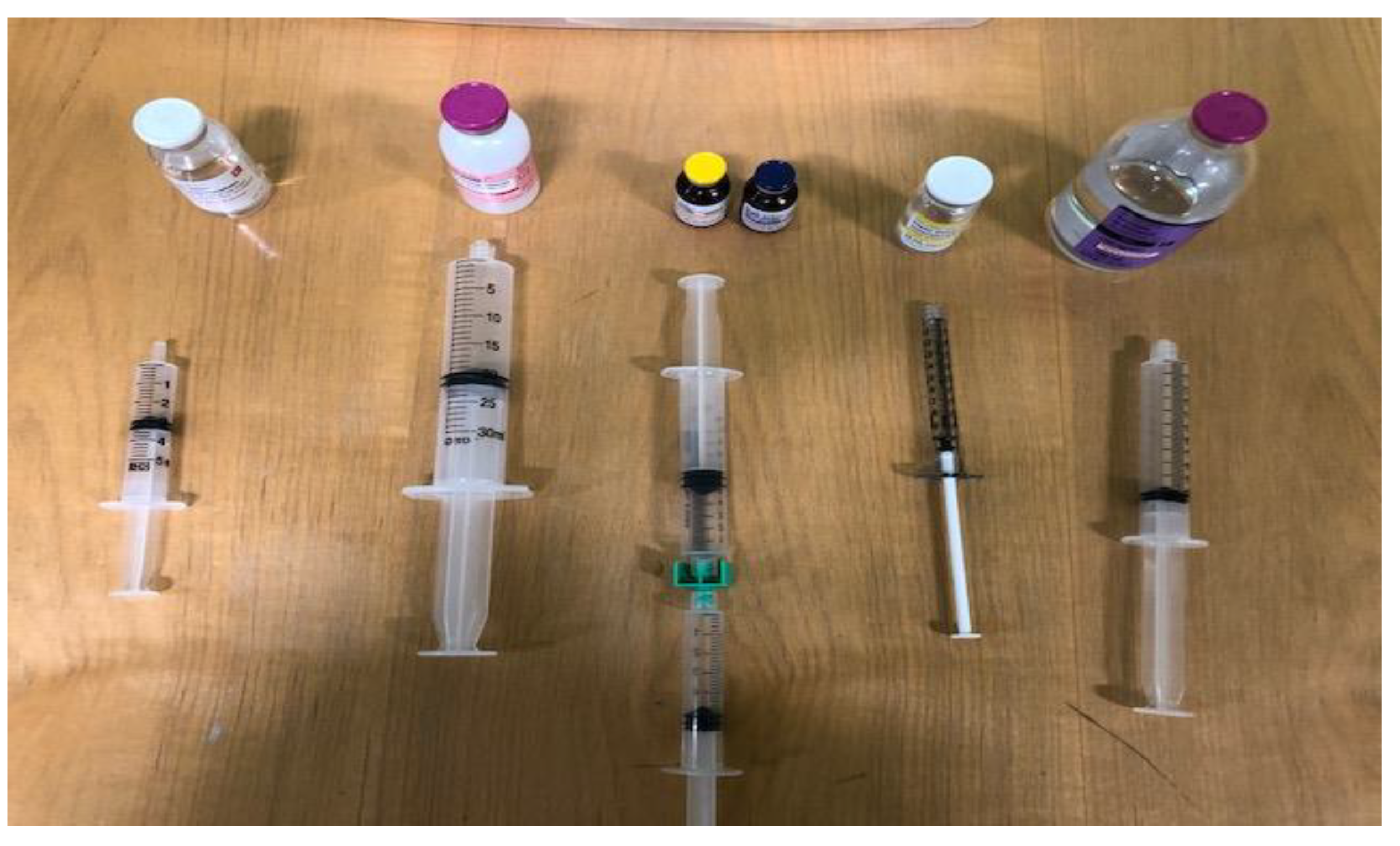
2.2. Methods
- Using the simulated materials, describe the process of combining individual PN ingredients together to form PN admixtures;
- Given a PN order and stock solution concentrations, calculate relevant PN parameters such as the required volume of macronutrients and micronutrients (given the amount in the order), calories and percentage calories for each of the macronutrients, and percentage weight-in-volume (w/v) of each macronutrient in the final PN admixture preparation;
- Demonstrate the order in which calcium gluconate and phosphate salt are added to PN to prevent calcium and phosphorus precipitation;
- Create a positive and engaging experience that stimulates interest in PN.
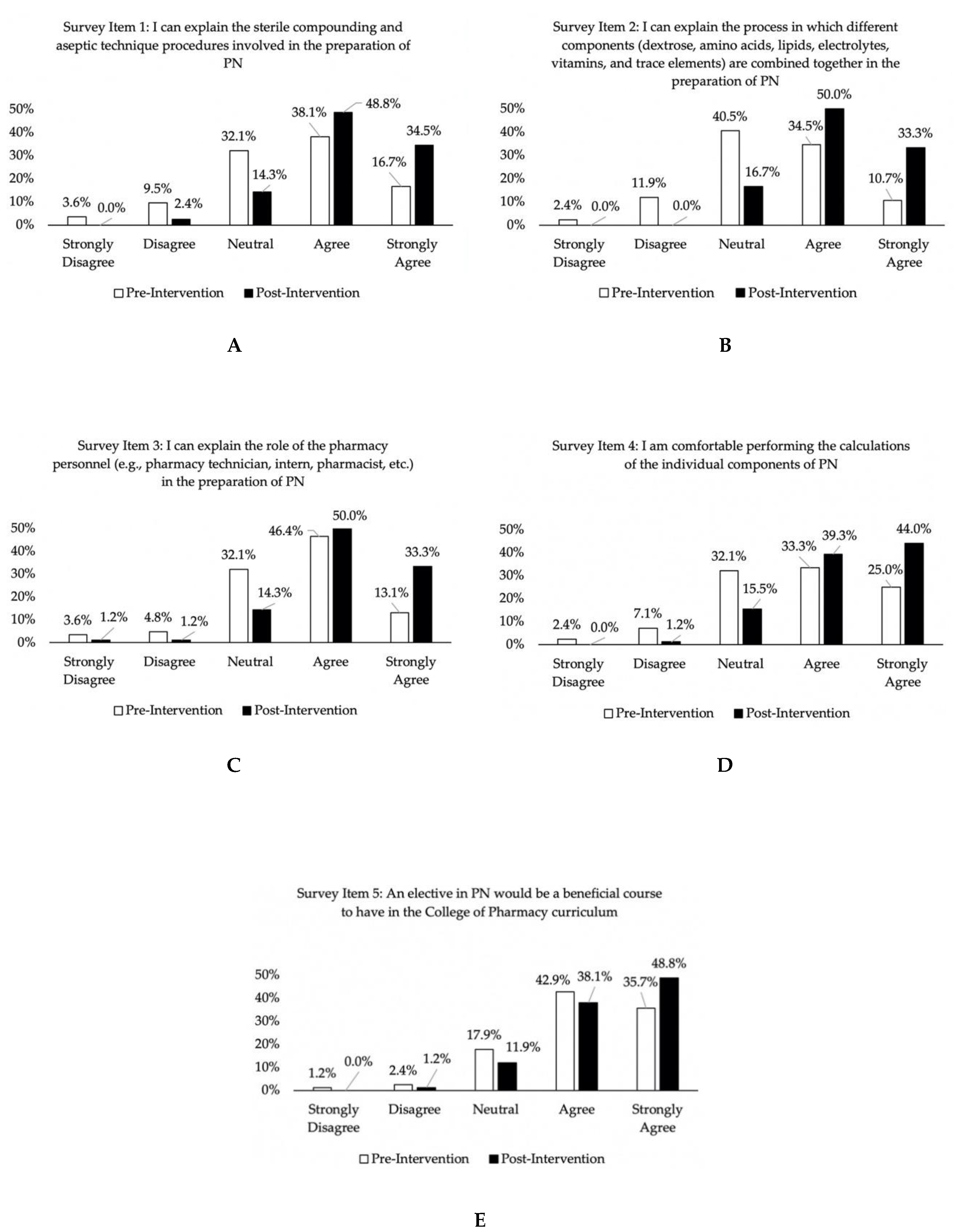
- “I can explain the sterile compounding and aseptic technique procedures involved in the preparation of PN”;
- “I can explain the process in which different components (dextrose, amino acids, injectable lipid emulsion, electrolytes, vitamins, and trace elements) are combined together in the preparation of PN”;
- “I can explain the role of the pharmacy personnel (pharmacy technician, intern, pharmacist, etc.) in the preparation of PN”;
- “I am comfortable performing the calculations of the individual components of PN”;
- “An elective in PN would be a beneficial course to have in the College of Pharmacy curriculum”.
2.3. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- What is Nutrition Support Therapy? The American Society for Parenteral and Enteral Nutrition. Available online: https://www.nutritioncare.org/About_Clinical_Nutrition/What_is_Nutrition_Support_Therapy/ (accessed on 3 May 2020).
- Ayers, P.; Adams, S.; Boullata, J.; Gervasio, J.; Holcombe, B.; Kraft, M.D.; Marshall, N.; Neal, A.; Sacks, G.; Seres, D.S.; et al. ASPEN parenteral nutrition safety consensus recommendations. JPEN J. Parenter. Enter. Nutr. 2014, 38, 296–333. [Google Scholar] [CrossRef] [PubMed]
- High-Alert Medications in Acute Care Settings; Institute of Safe Medication Practices (ISMP): Horsham, PA, USA, 2018; Available online: https://www.ismp.org/recommendations/high-alert-medications-acute-list (accessed on 24 March 2019).
- Schneider, P.J.; Pedersen, C.A.; Scheckelhoff, D.J. ASHP national survey of pharmacy practice in hospital settings: Dispensing and administration-2017. Am. J. Health Syst. Pharm. 2018, 75, 1203–1226. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, C.A.; Schneider, P.J.; Ganio, M.C.; Scheckelhoff, D.J. ASHP national survey of pharmacy practice in hospital settings: Prescribing and transcribing-2019. Am. J. Health Syst. Pharm. 2020, 77, 1026–1050. [Google Scholar] [CrossRef] [PubMed]
- Mutz, A.B.; Beyer, J.; Dickson, W.L.; Gutman, I.; Yucebay, F.; Lepkowsky, M.; Chan, J.; Carter, K.; Shaffer, C.L.; Fuller, P.D. Student preparation for PGY1 residency training by US colleges of pharmacy: Survey of the residency program director perspective. Hosp. Pharm. 2017, 52, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Solomon, D.M.; Emery, E.Z.; Kavelak, H.L.; Pontiggia, L.; Hollands, J.M.; Bingham, A.L. Impact of implementation of the American Society for Parenteral and Enteral Nutrition model for parenteral nutrition order writing and review on competency, attitudes, and perceptions. Nutr. Clin. Pract. 2019, 34, 597–605. [Google Scholar] [CrossRef] [PubMed]
- Flannery, A.H.; Soric, M.M.; Benavides, S.; Bobbitt, L.J.; Chan, A.; Crannage, A.J.; Flores, E.K.; Gibson, C.M.; Gurgle, H.E.; Kolanczyk, D.M.; et al. 2019 Update to the American College of Clinical Pharmacy pharmacotherapy didactic curriculum toolkit. J. Am. Coll. Clin. Pharm. 2020, 3, 455–464. [Google Scholar] [CrossRef]
- Proceedings of the 71st Annual Session of the ASHP House of Delegates, Boston, MA, USA, 9 and 11 June 2019. American Society of Health-System Pharmacists: Bethesda, MD, USA. Available online: https://www.ashp.org/-/media/4D2DBE635E5947478111A5E1504B9107.ashx (accessed on 16 February 2020).
- Resident Matching Program: Summary of Programs and Positions Offered and Filled 2020 Match-Combined Phase I and Phase II; American Society of Health-System Pharmacists: Bethesda, MD, USA, 2020; Available online: https://natmatch.com/ashprmp/stats/2020summpos.pdf (accessed on 4 July 2020).
- Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree (“Standards 2016”); Accreditation Council for Pharmacy Education: Chicago, IL, USA, 2015; Available online: https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf (accessed on 12 May 2020).
- NAPLEX Competency Statements; National Association of Boards of Pharmacy (NABP): Mount Prospect, IL, USA, 2020; Available online: https://nabp.pharmacy/naplex-competency-statements/ (accessed on 11 July 2020).
- Cooper, C.; Almgren, M.M.; Maxwell, W.D.; Baker, J.L. Instruction on compounded sterile preparations at schools of pharmacy. Am. J. Health Syst. Pharm. 2018, 75, 845–847. [Google Scholar] [CrossRef] [PubMed]
- Nemec, E.C.; Petraglia, C.; Mattison, M.J. Design considerations of a compounded sterile preparations course. Am. J. Pharm. Educ. 2016, 80, 12. [Google Scholar] [CrossRef] [PubMed]
- Vyas, D.; Bray, B.S.; Wilson, M.N. Use of simulation-based teaching methodologies in US colleges and schools of pharmacy. Am. J. Pharm. Educ. 2013, 77, 53. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.; Travlos, D.V.; Wadelin, J.W.; Vlasses, P.H. Simulation and introductory pharmacy practice experiences. Am. J. Pharm. Educ. 2011, 75, 209. [Google Scholar] [CrossRef] [PubMed]
- Dang, Y.H. Using simplistic simulations to enhance learning in a nephrology pharmacotherapeutics module. Curr. Pharm. Teach. Learn. 2017, 9, 898–902. [Google Scholar] [CrossRef] [PubMed]
- Bowers, R.; Tunney, R.; Kelly, K.; Mills, B.; Trotta, K.; Wheeless, C.N.; Drew, R. Impact of standardized simulated patients on first-year pharmacy students’ knowledge retention of insulin injection technique and counseling skills. Am. J. Pharm. Educ. 2017, 81, 113. [Google Scholar] [CrossRef] [PubMed]
- Seybert, A.L.; Barton, C.M. Simulation-based learning to teach blood pressure assessment to doctor of pharmacy students. Am. J. Pharm. Educ. 2007, 71, 48. [Google Scholar] [CrossRef] [PubMed]
- Basheti, I.A. The effect of using simulation for training pharmacy students on correct device technique. Am. J. Pharm. Educ. 2014, 78, 177. [Google Scholar] [CrossRef] [PubMed]
- Marken, P.A.; Zimmerman, C.; Kennedy, C.; Schremmer, R.; Smith, K.V. Human simulators and standardized patients to teach difficult conversations to interprofessional health care teams. Am. J. Pharm. Educ. 2010, 74, 120. [Google Scholar] [CrossRef] [PubMed]
- Medina, M.S.; Plaza, C.M.; Stowe, C.D.; Robinson, E.T.; DeLander, G.; Beck, D.E.; Melchert, R.B.; Supernaw, R.B.; Roche, V.F.; Gleason, B.L.; et al. Center for the Advancement of Pharmacy Education Educational Outcomes 2013. Am. J. Pharm. Educ. 2013, 77, 162. Available online: https://www.aacp.org/sites/default/files/2017-10/CAPEoutcomes2013%20%281%29.pdf (accessed on 26 April 2020). [CrossRef] [PubMed]
- Ayers, P.; Bobo, E.S.; Hurt, R.T.; Mays, A.A.; Worthington, P.H. ASPEN Parenteral Nutrition Handbook, 3rd ed.; American Society for Parenteral and Enteral Nutrition: Silver Spring, MD, USA, 2020. [Google Scholar]
- Sacks, G.S. The shrinking of formalized nutrition education in health professions curricula and postgraduate training. JPEN J. Parenter. Enter. Nutr. 2017, 41, 217–225. [Google Scholar] [CrossRef] [PubMed]
| Variable | Cohort 1 n (%) | Cohort 2 n (%) | Chi-Square p-Value |
|---|---|---|---|
| Gender | 0.74 | ||
| Male | 15 (41.7) | 17 (35.4) | |
| Female | 18 (50) | 28 (58.3) | |
| Prefer not to disclose | 3 (8.3) | 3 (6.3) | |
| Age | 0.56 | ||
| 20–24 | 4 (11.1) | 9 (18.8) | |
| 25–34 | 25 (69.4) | 34 (70.8) | |
| 35–44 | 2 (5.6) | 1 (2.1) | |
| Prefer not to disclose | 5 (13.9) | 4 (8.3) | |
| Bachelor’s degree | 0.92 | ||
| Yes | 33 (91.7) | 45 (93.8) | |
| No | 2 (5.6) | 3 (6.3) | |
| Information not disclosed | 1 (2.8) | 0 (0) | |
| Bachelor’s degree subject area | 0.07 | ||
| Basic sciences | 17 (47.2) | 34 (70.1) | |
| Humanities or social sciences | 5 (13.9) | 4 (8.3) | |
| Other | 8 (22.2) | 7 (14.6) | |
| Information not disclosed | 4 (11.1) | 0 (0) | |
| Not applicable | 2 (5.6) | 3 (6.3) | |
| Work experience—pharmacy technician | 0.65 | ||
| Yes | 2 (5.6) | 4 (8.3) | |
| No | 33 (91.7) | 44 (91.7) | |
| Information not disclosed | 1 (2.8) | 0 (0) | |
| Work experience—pharmacy intern | 0.44 | ||
| Yes | 5 (13.9) | 10 (20.8) | |
| No | 30 (83.3) | 38 (79.2) | |
| Information not disclosed | 1 (2.8) | 0 (0) | |
| Ideal way of learning | 0.10 | ||
| Watching a video | 1 (2.8) | 1 (2.1) | |
| Hands-on training | 6 (16.7) | 10 (20.8) | |
| Listening to a lecture | 9 (25) | 3 (6.3) | |
| Watching a video and hands-on training | 4 (11.1) | 9 (18.8) | |
| Watching a video and listening to a lecture | 2 (5.6) | 1 (2.1) | |
| Hands-on training and listening to a lecture | 2 (5.6) | 0 (0) | |
| Watching a video, hands-on training, and listening to a lecture | 12 (33.3) | 24 (50) |
| Comments |
|---|
| I really enjoyed that the instructor brought in the PN bags. |
| The instructor made learning exciting and engaging by bringing in mock medications for us to practice. |
| PN lab was informative. |
| We were taught how to fill PN, but we did not have practice in writing them. It would have been a good opportunity for a cumulative case study. |
| I liked the visual education with PN. |
| This hands-on activity enhanced what we learned about PN. It was helpful to do the calculations, draw out the volume, and set it up as if we were in the hospital. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salman, G.; Hua, H.; Nguyen, M.; Rios, S.; Hernandez, E.A. The Role of a Simulation-Based Activity on Student Perceptions of Parenteral Nutrition Education. Pharmacy 2020, 8, 123. https://doi.org/10.3390/pharmacy8030123
Salman G, Hua H, Nguyen M, Rios S, Hernandez EA. The Role of a Simulation-Based Activity on Student Perceptions of Parenteral Nutrition Education. Pharmacy. 2020; 8(3):123. https://doi.org/10.3390/pharmacy8030123
Chicago/Turabian StyleSalman, Genene, Henry Hua, Michelle Nguyen, Sandy Rios, and Elvin A. Hernandez. 2020. "The Role of a Simulation-Based Activity on Student Perceptions of Parenteral Nutrition Education" Pharmacy 8, no. 3: 123. https://doi.org/10.3390/pharmacy8030123
APA StyleSalman, G., Hua, H., Nguyen, M., Rios, S., & Hernandez, E. A. (2020). The Role of a Simulation-Based Activity on Student Perceptions of Parenteral Nutrition Education. Pharmacy, 8(3), 123. https://doi.org/10.3390/pharmacy8030123






