Process Evaluation of the Community Pharmacist-Led Allergic Rhinitis Management (C-PhARM) Service in Singapore
Abstract
1. Introduction
2. Objectives
3. Methodology
3.1. Study Design and Ethics Approval
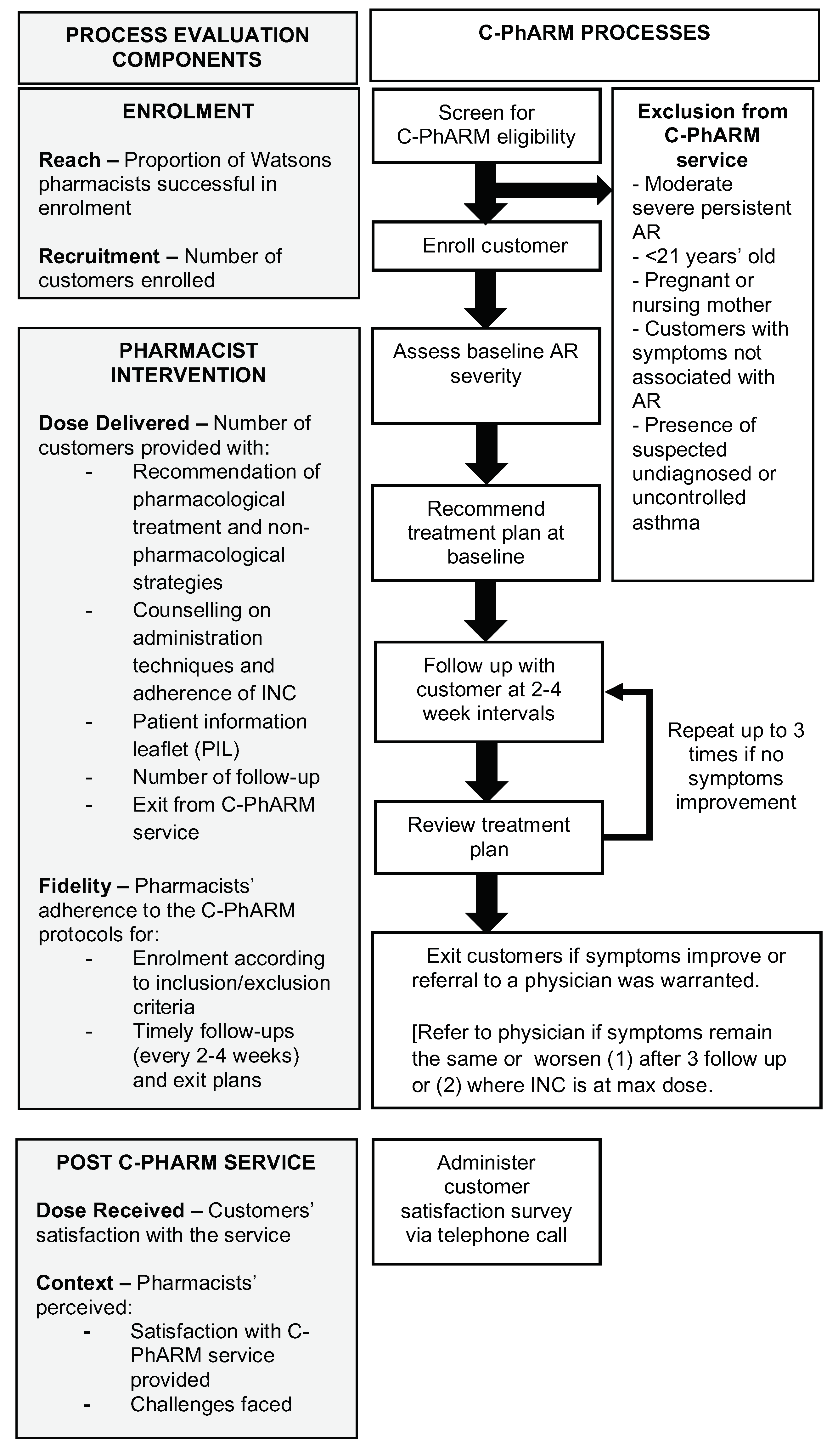
3.2. Description of the C-PhARM Service and Implementation
3.2.1. Pharmacist Interventions
Assessment and Recommendations at Baseline
Assessment and Recommendations at Follow-Up
Exit Plans and Protocol
3.2.2. Dissemination of the C-PhARM Protocol and Materials to Pharmacists
3.3. Definitions of the Process Evaluation Components and Outcome Measures
3.3.1. Reach and Recruitment
3.3.2. Dose Delivered
3.3.3. Fidelity
3.3.4. Dose Received
3.3.5. Context
3.4. Data Collection
3.5. Data Analysis
4. Results
4.1. Reach and Recruitment
4.2. Dose Delivered
4.2.1. Pharmacist Interventions at Baseline
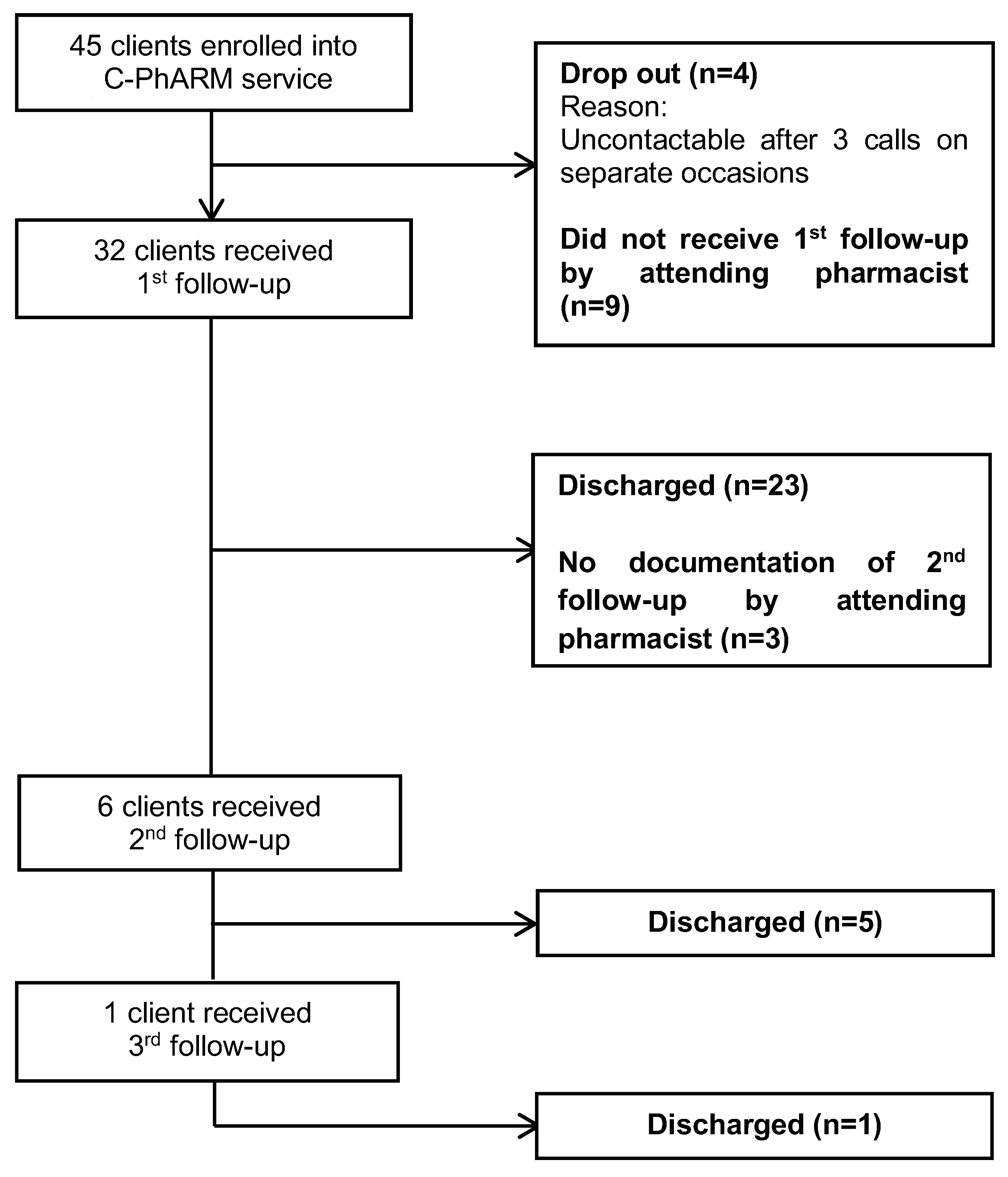
4.2.2. Pharmacist Interventions at Follow-Up and Exit Plans
4.3. Fidelity
4.3.1. Enrolment
4.3.2. Follow-Up and Exit Plans
4.4. Dose Received (Customer Satisfaction)
4.5. Context
4.5.1. Pharmacist Perceptions about the C-PhARM Service and Use of Guides
4.5.2. Barriers to the C-PhARM Service
5. Discussion
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bousquet, J.; Khaltaev, N.; Cruz, A.A.; Denburg, J.; Fokkens, W.J.; Togias, A.; Zuberbier, T.; Baena-Cagnani, C.E.; Canonica, G.W.; van Weel, C.; et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy 2008, 63 (Suppl. 86), 8–160. [Google Scholar] [CrossRef] [PubMed]
- Pawankar, R.; Bunnag, C.; Khaltaev, N.; Bousquet, J. Allergic Rhinitis and Its Impact on Asthma in Asia Pacific and the ARIA Update 2008. World Allergy Organ. J. 2012, 5 (Suppl. 3), S212–S217. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.Y.; Niti, M.; Smith, J.D.; Yeoh, K.H.; Ng, T.P. Rhinitis: Do diagnostic criteria affect the prevalence and treatment? Allergy 2002, 57, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Andiappan, A.K.; Puan, K.J.; Lee, B.; Nardin, A.; Poidinger, M.; Connolly, J.; Chew, F.T.; Wang, D.Y.; Rotzschke, O. Allergic airway diseases in a tropical urban environment are driven by dominant mono-specific sensitization against house dust mites. Allergy 2014, 69, 501–509. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.; Scadding, G. Is reliance on self-medication and pharmacy care adequate for rhinitis patients? Int. J. Clin. Pract. 2009, 63, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Tan, R.; Cvetkovski, B.; Kritikos, V.; Price, D.; Yan, K.; Smith, P.; Bosnic-Anticevich, S. Identifying the hidden burden of allergic rhinitis (AR) in community pharmacy: A global phenomenon. Asthma Res. Pract. 2017, 3, 8. [Google Scholar] [CrossRef] [PubMed]
- Canonica, G.W.; Bousquet, J.; Mullol, J.; Scadding, G.K.; Virchow, J.C. A survey of the burden of allergic rhinitis in Europe. Allergy 2007, 62 (Suppl. 85), 17–25. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, E.O.; Nathan, R.; Derebery, J.; Stang, P.E.; Campbell, U.B.; Yeh, W.S.; Corrao, M.; Stanford, R. Sleep, quality of life, and productivity impact of nasal symptoms in the United States: Findings from the Burden of Rhinitis in America survey. Allergy Asthma Proc. 2009, 30, 244–254. [Google Scholar] [CrossRef]
- Wee, L. Allergic Rhinitis on the Rise among Children. 11 April 2013. The Straits Times. Available online: https://www.straitstimes.com/singapore/allergic-rhinitis-on-the-rise-among-children (accessed on 26 May 2019).
- Kulthanan, K.; Chusakul, S.; Recto, M.T.; Gabriel, M.T.; Aw, D.C.; Prepageran, N.; Wong, A.; Leong, J.L.; Foong, H.; Quang, V.T.; et al. Economic burden of the inadequate management of allergic rhinitis and urticaria in Asian countries based on the GA2LEN Model. Allergy Asthma Immunol. Res. 2018, 10, 370–378. [Google Scholar] [CrossRef]
- Fong, S.J.; Chia, S.X.; Chung, W.L.; Chong, B.K.; Chui, W.K.; Yap, K.Z. Intranasal corticosteroid use prevalence and adherence in allergic rhinitis—A cross-sectional study at community pharmacies in Singapore. Pharmacotherapy 2016, 16, e87–e88. [Google Scholar]
- Hardasmalani, R. Watsons Offers Free Allergy Consultations around S’pore. Available online: https://www.todayonline.com/business/watsons-offers-free-allergy-consultations-around-spore (accessed on 26 May 2019).
- Grol, R.; Wensing, M. What drives change? Barriers to and incentives for achieving evidence-based practice. Med. J. Aust. 2004, 180 (Suppl. 6), S57–S60. [Google Scholar] [PubMed]
- Saunders, R.P.; Evans, M.H.; Joshi, P. Developing a process-evaluation plan for assessing health promotion program implementation: A how-to guide. Health Promot. Pract. 2005, 6, 134–147. [Google Scholar] [CrossRef] [PubMed]
- Moore, G.F.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T.; Wight, D.; et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015, 350, h1258. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The Role of Pharmacist in the Health Care System; WHO: Geneva, Switzerland, 1994. [Google Scholar]
- Wang, K.; Wang, C.; Xi, L.; Zhang, Y.; Ouyang, Y.; Lou, H.; Zhang, W.; Zhang, L. A randomized controlled trial to assess adherence to allergic rhinitis treatment following a daily short message service (SMS) via the mobile phone. Int. Arch. Allergy Immunol. 2014, 163, 51–58. [Google Scholar] [CrossRef]
- Hughes, C.M.; Hawwa, A.F.; Scullin, C.; Anderson, C.; Bernsten, C.B.; Björnsdóttir, I.; Cordina, M.A.; da Costa, F.A.; De Wulf, I.; Eichenberger, P.; et al. Provision of pharmaceutical care by community pharmacists: A comparison across Europe. Pharm. World Sci. 2010, 32, 472–487. [Google Scholar] [CrossRef]
- American College of Clinical Pharmacy; Kirwin, J.; Canales, A.E.; Bentley, M.L.; Bungay, K.; Chan, T.; Dobson, E.; Holder, R.M.; Johnson, D.; Lilliston, A.; et al. Process indicators of quality clinical pharmacy services during transitions of care. Pharmacotherapy 2012, 32, e338–e347. [Google Scholar] [CrossRef] [PubMed]
- Chui, W.K.; Li, S.C. Advice-giving on self-medication: Perspectives of community pharmacists and consumers in Singapore. J. Clin. Pharm. Ther. 2005, 30, 225–231. [Google Scholar] [CrossRef]
- Jack, S.M.; Sheehan, D.; Gonzalez, A.; MacMillan, H.L.; Catherine, N.; Waddell, C.; British Columbia Healthy Connections Project Process Evaluation Research Team. British Columbia Healthy Connections Project process evaluation: A mixed methods protocol to describe the implementation and delivery of the Nurse-Family Partnership in Canada. BMC Nurs. 2015, 14, 47. [Google Scholar] [CrossRef]
- Marple, B.F.; Fornadley, J.A.; Patel, A.A.; Fineman, S.M.; Fromer, L.; Krouse, J.H.; Lanier, B.Q.; Penna, P.; American Academy of Otolaryngic Allergy Working Group on Allergic Rhinitis. Keys to successful management of patients with allergic rhinitis: Focus on patient confidence, compliance, and satisfaction. Otolaryngol. Head Neck Surg. 2007, 136 (Suppl. 6), S107–S124. [Google Scholar] [CrossRef]
- Yellen, E.; Davis, G.C.; Ricard, R. The measurement of patient satisfaction. J. Nurs. Care Qual. 2002, 16, 23–29. [Google Scholar] [CrossRef]
- Bosnic-Anticevich, S.; Costa, E.; Menditto, E.; Lourenço, O.; Novillino, E.; Bialek, S.; Briedis, V.; Buonaluto, R.; Chrystyn, H.; Cvetkovski, B.; et al. ARIA pharmacy 2018 “Allergic rhinitis care pathways for community pharmacy”: AIRWAYS ICPs initiative (European Innovation Partnership on Active and Healthy Ageing, DG CONNECT and DG Santé) POLLAR (Impact of Air POLLution on Asthma and Rhinitis) GARD Demonstration project. Allergy 2018. [Google Scholar] [CrossRef]
- Brozek, J.L.; Bousquet, J.; Agache, I.; Agarwal, A.; Bachert, C.; Bosnic-Anticevich, S.; Brignardello-Petersen, R.; Canonica, G.W.; Casale, T.; Chavannes, N.H.; et al. Allergic rhinitis and its impact on Asthma (ARIA) guidelines—2016 revision. J. Allergy Clin. Immunol. 2017, 140, 950–958. [Google Scholar] [CrossRef] [PubMed]
| Customer Profile | n | (%) |
|---|---|---|
| Gender | ||
| Male | 18 | 40.0 |
| Female | 27 | 60.0 |
| Age | ||
| 21–30 | 17 | 37.8 |
| 31–40 | 11 | 24.4 |
| 41–50 | 9 | 20.0 |
| 51–60 | 6 | 13.3 |
| >60 | 2 | 4.4 |
| Ethnicity | ||
| Chinese | 40 | 88.9 |
| Malay | 3 | 6.7 |
| Indian | 0 | 0.0 |
| Other | 2 | 4.4 |
| Education level | ||
| Primary school and below | 1 | 2.2 |
| Secondary school | 7 | 15.6 |
| Polytechnic/ Junior college/ Institute of Technical Education | 7 | 15.6 |
| University and above | 30 | 66.7 |
| Level of physical activity | ||
| Less than 150 min/week | 28 | 62.2 |
| About 150 min/week | 9 | 20.0 |
| More than 150 min/week | 8 | 17.8 |
| Smoking status | ||
| Yes | 1 | 2.2 |
| Ex-smoker | 4 | 8.9 |
| No | 40 | 88.9 |
| Associated comorbidities | ||
| Asthma only | 9 | 20.0 |
| Eczema only | 10 | 22.2 |
| Both asthma and eczema | 2 | 4.4 |
| None | 24 | 53.3 |
| Pharmacist Intervention | Number of Interventions Provided, n | (%) |
|---|---|---|
| BASELINE | ||
| Assessment of AR | ||
| Mild intermittent | 10 | 22.2 |
| Mild persistent | 8 | 17.8 |
| Moderate—severe intermittent | 15 | 33.3 |
| Moderate—severe persistent | 12 | 26.7 |
| Recommendations/Interventions | ||
| First-generation antihistamine ± decongestant only | 2 | 4.4 |
| Second-/third-generation antihistamine ± decongestant only | 13 | 28.9 |
| INC only | 11 | 24.4 |
| INC + antihistamine (any) | 17 | 37.8 |
| Non-pharmacological strategies† | 27 | 60.0 |
| Counselling on INC administration technique and adherence‡ | 17 | 37.8 |
| Provision of AR PIL | 5 | 11.1 |
| FOLLOW-UP | ||
| Number of follow-ups | ||
| 1 | 26 | 57.8 |
| ≥ 2 | 6 | 13.3 |
| Interventions at first follow-up | ||
| Dose adjustment | 6 | 13.3 |
| Maintain current regimen | 13 | 28.9 |
| Discontinue current regimen | 9 | 20.0 |
| INC adherence counselling | 2 | 4.4 |
| Referral to a doctor | 4 | 8.9 |
| Non-pharmacological strategies† | 13 | 28.9 |
| Interventions at second/third follow-up | ||
| Dose adjustment | 0 | |
| Maintain current regimen | 3 | 6.7 |
| Discontinue current regimen | 1 | 2.2 |
| INC adherence counselling | 0 | |
| Referral to a doctor | 0 | |
| Non-pharmacological strategies† | 1 | 2.2 |
| Exits plans§ | 29 | 64.4 |
| Survey Item | Median (IQR)† |
|---|---|
| I have a better understanding of AR and related medication use through this service. | 4 (3.25–4.75) |
| Watsons’ pharmacists are professional and knowledgeable in providing clear and detailed information about my condition | 4 (4.00–5.00) |
| I am comfortable with the frequency of follow-up. | 4 (4.00–4.75) |
| The PIL is a good reference for me.‡ | 4 (3.00–5.00) |
| This program improves my overall experience with community pharmacy. | 4 (4.00–4.75) |
| I would recommend this allergic rhinitis service to my friend. | 4 (3.25–4.75) |
| Survey Item | Median (IQR)† |
|---|---|
| Overall C-PhARM service | (N = 43) |
| The C-PhARM service workflow is clear. | 4 (3–4) |
| The hardcopy C-PhARM service forms are user-friendly. | 4 (3–4) |
| The C-PhARM service is beneficial in helping patients manage their AR condition. | 4 (3–4) |
| The Watsons AR PIL is useful in assisting me during patient education. | 3 (3–3) |
| I am motivated to recruit patients. | 4 (3–4) |
| Overall, I am satisfied with the C-PhARM service. | 4 (3–4) |
| C-PhARM in-house protocols and guidelines | (N = 43) |
| The workflow protocol for patient enrolment and follow-up process is useful. | 4 (4–4) |
| The clinical executive summary for patient assessment and management is useful. | 4 (4–4) |
| The INC recommendation guidelines are useful. | 4 (4–4) |
| The antihistamine recommendation guidelines are useful. | 4 (3–4) |
| I prefer to use my own discretion when providing treatment recommendations. | 3 (3–4) |
| Overall, I am satisfied with the materials in the C-PhARM kit. | 4 (4–4) |
| Individual one-on-one detailing at the store‡ | (N = 17) |
| The above is effective in helping me better understand the workflow. | 4 (4–4) |
| The above is effective in answering my queries about the C-PhARM service. | 4 (3–4) |
| Overall, I am satisfied with the above. | 4 (4–4) |
| Challenges faced by pharmacists | (N = 43) |
| I find the patient enrolment process confusing. | 3 (2–3) |
| I am too busy to enrol patients in the C-PhARM service. | 3 (3–4) |
| I need one-on-one dedicated, undisturbed time at baseline consultation | 4 (4–4) |
| Patient is not interested in participating. | 4 (4–4) |
| Patient is reluctant to fill in baseline assessment form. | 4 (3–4) |
| I am unsure of how to approach patients. | 3 (2–3) |
| I do not see the need to enrol patients in the C-PhARM service as there is no value in the service to optimise a patient’s AR condition. | 2 (2–3) |
| I find the patient follow-up process confusing. | 2 (2–3) |
| I am too busy to follow up with patients. | 3 (3–4) |
| I find it difficult to conduct phone follow-ups with patients without being interrupted by patients from the shop floor. | 4 (3–4) |
| I do not see the need to follow up patients as AR can be easily self-managed. | 3 (2–3) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yap, J.S.Y.; Tang, C.W.Q.; Hor, H.M.L.; Chong, J.B.K.; Yap, K.Z. Process Evaluation of the Community Pharmacist-Led Allergic Rhinitis Management (C-PhARM) Service in Singapore. Pharmacy 2019, 7, 56. https://doi.org/10.3390/pharmacy7020056
Yap JSY, Tang CWQ, Hor HML, Chong JBK, Yap KZ. Process Evaluation of the Community Pharmacist-Led Allergic Rhinitis Management (C-PhARM) Service in Singapore. Pharmacy. 2019; 7(2):56. https://doi.org/10.3390/pharmacy7020056
Chicago/Turabian StyleYap, Joanne Shi Ying, Colin Wei Qiang Tang, Helena Mei Ling Hor, Joy Boon Ka Chong, and Kai Zhen Yap. 2019. "Process Evaluation of the Community Pharmacist-Led Allergic Rhinitis Management (C-PhARM) Service in Singapore" Pharmacy 7, no. 2: 56. https://doi.org/10.3390/pharmacy7020056
APA StyleYap, J. S. Y., Tang, C. W. Q., Hor, H. M. L., Chong, J. B. K., & Yap, K. Z. (2019). Process Evaluation of the Community Pharmacist-Led Allergic Rhinitis Management (C-PhARM) Service in Singapore. Pharmacy, 7(2), 56. https://doi.org/10.3390/pharmacy7020056





