Abstract
While the need to measure burnout, stress and mental health among pharmacy students has been emphasized in the literature, there is limited information on which validated scales should be used. The objective of this scoping review was to identify published studies that used validated scales for burnout, stress and mental health among pharmacy students to provide recommendations for implementation at schools/colleges of pharmacy. Thirty-two out of 153 articles published in the United States from 1 January 2000 to 30 September 2022 were included and categorized into studies measuring stress (20), burnout (4) and depression/anxiety (8). The most common validated scales used to assess stress and burnout among pharmacy students were the Perceived Stress Scale (PSS) and the Maslach Burnout Inventory and the Oldenburg Burnout Inventory, respectively. For mental health, anxiety was most commonly investigated using a variety of scales such as the Generalized Anxiety Disorder-7; the Patient Health Questionnaire, 9-item was used to measure depression in two studies. Validity, ease of use, cost and generalizability are important considerations for selecting a scale. The PSS has been studied extensively in pharmacy students and has been correlated with other well-being domains. Studies that measured burnout and mental health (specifically, depression and anxiety) have less published evidence among pharmacy students.
1. Introduction
Clinician well-being has gained national attention due to increased reports of clinician burnout and its impact on patient care and professional disengagement [1]. Specifically within the pharmacy profession, in 2019, several large and influential pharmacy organizations were convened to develop meaningful and actionable recommendations aimed at promoting resiliency in our pharmacy workforce [2]. In the academic pharmacy community, concerns surrounding student wellness and mental health issues have been increasing. In the 2017–2018 American Association of Colleges of Pharmacy (AACP) Student Affairs Standing Committee Report, members outlined charges to identify best practices to promote student well-being and resilience [3]. More recently, the AACP has made “Achieving Well-being for All” one of its top 2021–2024 strategic priorities [4]. As a result, there has been an impetus for pharmacy educators to evaluate factors that impact student burnout and implement strategies that can improve their well-being.
The National Academy of Medicine recently launched a National Plan for Health Workforce Well-Being in an effort to drive policy and systems change to strengthen the health workforce well-being [5]. The plan outlines several priority areas, but specifically to pharmacy students, it focuses on assessment tools, strategies and research, and the need to recruit and retain a diverse and inclusive health workforce. Unfortunately, there is no clear recommendation for how “well-being” should be measured in the workforce, nor in academic institutions.
There are many scales (validated and unvalidated) that are used by pharmacy schools to measure well-being. As discussed by Dyrbye and colleagues [6], several characteristics should be considered by organizations when selecting the appropriate scale [6]. Organizations should consider (1) the domain of well-being that is important to the stakeholder (in this case, the school/college of pharmacy), (2) the organization burden (i.e., brevity of scale, easy scoring, low or no cost), (3) actionable measures stemming from the scale (with easily to interpret scores and established benchmarks), (4) strong psychometric properties (validity and reliability) and (5) broad applicability (in the case of students, to all levels of students in different types of pharmacy programs) [6]. The domains of well-being are especially important since there are numerous definitions of well-being and schools/colleges of pharmacy should be selective in which construct of well-being they want to measure [6].
A recently published review of well-being assessment and interventions in pharmacy students included 15 articles (seven studies conducted in the US and eight conducted internationally) [7]. The review focused on studies assessing student pharmacist well-being (physical, economic, social, emotional, psychological, life satisfaction and engaging activities) using validated and non-validated scales specific for well-being. The authors also assessed for gaps in the literature on the topic and evaluated interventions for improvement. Due to the myriad definitions of well-being used by academic institutions and investigators as well as the issues of mental health challenges that are often associated with the topic of well-being, we aimed to provide a review of validated scales of stress, burnout and depression/anxiety that have been used to study pharmacy students in the United States. Our scoping review, therefore, is more extensive and encompasses a review of mental health challenges that have been frequently assessed in conjunction with student well-being. For each area, we organized the literature into common predictors, associations with other constructs and non-pharmacologic interventions. The main objective of the review was to provide pharmacy educators with the knowledge and validated tools that can be used to measure stress, burnout and depression/anxiety among their students.
2. Methods
One of the investigators conducted a systematic search of literature surrounding stress, burnout and depression/anxiety issues for pharmacy students using PubMed, Google Scholar and Google. We used the following search terms: pharmacy student, stress, burnout, mental health, mental wellbeing, perceived stress scale, PharmD, academic success, success predictors, Five Facet Mindfulness Questionnaire (FFMQ), Jefferson Scale of Empathy, Maslach Burnout Inventory (MBI), student survey and wellness scales. We also conducted secondary source searches using references found in the literature from the original search. We also received librarian assistance to identify additional publications using MeSH search terms: stress, psychological, burnout, pharmacy student and education.
Once the articles were identified and recorded using Microsoft Excel, two investigators independently reviewed the articles for inclusion or exclusion in the study. Any conflicts in the choice of articles were resolved upon discussion by the two investigators. Inclusion criteria consisted of English language articles that were published from 1 January 2000 to 31 August 2022 and articles that studied pharmacy students in the areas of stress, burnout and depression/anxiety disorders. Studies that included other types of students (e.g., medical) were included as long as pharmacy students were also studied. We excluded any studies that were conducted outside of United States due to curricular and student demographics that could be vastly different and impact outcomes related to stress, burnout and depression/anxiety. We also excluded any articles that (1) were review or editorial in nature, (2) did not use a validated scale to measure their outcomes (i.e., lack of validity studies in any sample), (3) were qualitative only (i.e., focus groups/interviews), (4) were peripherally related to well-being but topics studied were beyond the scope of this article (e.g., grit, alcohol use, illicit substance use) and (5) were duplicate.
The objective of this scoping review was to summarize the literature that focused on measuring stress, burnout and depression/anxiety among pharmacy students in the United States using validated scales. The review summarizes the scales that were used to measure each theme, describes the overall findings from the studies and provides overall recommendations for scales that may be the most predictive and feasible for implementation within schools/colleges of pharmacy.
3. Results
In the systematic search, we initially identified 153 articles. Upon applying inclusion and exclusion criteria, 37 articles were selected for independent review by two investigators. The two investigators independently reviewed each article for inclusion or exclusion with a 95% (35/37) concordance rate. Upon resolution of conflicts between the two investigators, 32 articles were included in the systematic review (Figure 1).
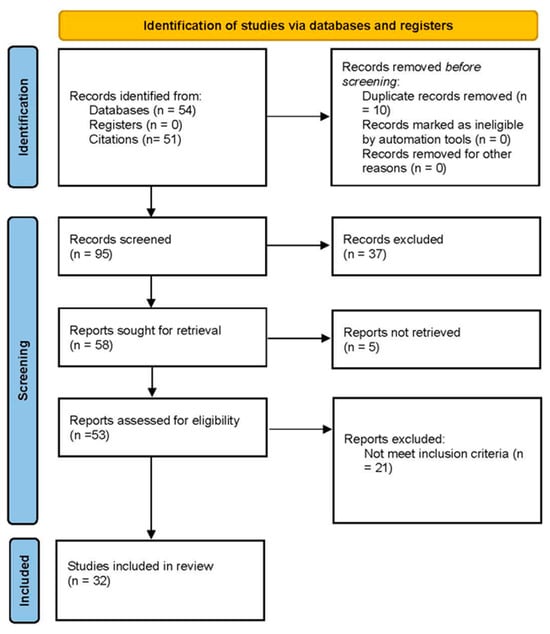
Figure 1.
PRISMA flow diagram.
We have summarized the scales that have been used in the studies along with their construct, scoring, accessibility and cost information (Table 1) [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33]. The articles from the systematic search are summarized under the following themes: (1) stress, (2) burnout and (3) depression/anxiety. We identified 20 articles for stress (Table 2) [12,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50], four articles for burnout (Table 3) [14,51,52,53], and eight articles for depression/anxiety (Table 4) [8,54,55,56,57,58,59,60]. For each theme, we provide a summary of published literature, including the scales used, major findings and limitations, and recommendations based upon validity, evidence and accessibility. Institutions should consider these factors in selecting the appropriate scale for their use. Modification of the validated scales is not recommended; however, institutions may combine the scales and/or add relevant programmatic questions regarding demographics and institution-specific offerings.

Table 1.
Scales used in pharmacy programs to measure student well-being.

Table 2.
Studies in perceived stress.

Table 3.
Studies in burnout.

Table 4.
Studies in depression and anxiety.
3.1. Stress
Stress is an emotional strain triggered by challenging factors like academic pressure, personal issues and environmental demands, especially in students. In our literature search, the most prevalent scale that was used to measure stress and reactions to stressful situations among pharmacy students was the Perceived Stress Scale (PSS 4, 10 or 14 item version) (Table 2). The PSS was used in 19 of 20 articles that were published after 2000 [12,32,33,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50]. In one article, the Student-life Stress Inventory (SSI) was used instead of PSS to measure stress [34].
3.1.1. Common Predictors of Stress
Among the studies evaluating stress and reported causes of stress, the commonly cited stressors for student pharmacists were academic course workload, high stakes activities such as examinations and reassessments, financial issues, and family and relationships [35,39,50]. In a study by Chisholm-Burns et al., investigators found that professional year 4 (P4) students who reported a greater “fear of debt” had also higher stress scores [41].
3.1.2. Associations with Other Constructs
Student pharmacists’ perceived stress has often been evaluated in relation to their academic achievement and Health-Related Quality of Life (HRQOL). Study results by Maynor et al. [45,46] and Saul Ballard et al. [47] have shown that increased stress was significantly correlated with decreased academic self-concept (how well an individual feels they can learn). Marshall et al. [35] have also found students’ high stress levels to be negatively correlated with mental HRQOL (p < 0.001) [35].
When evaluating race/ethnicity factors related to stress, two studies reported no differences in stress level or stressors experienced by student pharmacists [12,40]. However, when evaluating stress levels in the different Doctor of Pharmacy (PharmD) school years, varying results have been reported [37,39,42,45,46]. While Awe et al. [12] found no difference in stress levels among class cohorts, Ford et al. [39] reported P2 students having the highest level of stress related to academic workload. In other studies, Garber et al. [42] reported P3 students being more likely to have higher levels of stress than P1 or P4 students, while on the contrary, Maynor and Baugh [45] reported that perceived stress was significantly lower in P3 students compared to P1 and P2 students. Some studies have reported increasing stress levels observed in students as they progress through the PharmD curriculum [36,44,49]. In the study by Spivey et al. [44], female and minority students particularly experienced greater levels of stress at orientation. Similar findings have also been reported by other studies where female students had higher perceived stress levels compared to male students [34,37,38]. In one study by Votta and Benau, students with lower GPAs had higher stress than those with higher grade point averages (GPAs) [37]. Further, Marshall et al. [35] found that the most significant stressor for both men and women was examinations, while Beal et al. [40] found that time spent with family/friends was the most frequently reported stress reliever [35,40].
To manage stress, student pharmacists often employed more positive coping strategies: spending time with family and friends, active coping, planning and acceptance, physical activity, meditation and yoga [12,35,40,42,45,46]. Interestingly, according to Garber et al., students who used exercise as a coping mechanism reported lower perceived stress (p < 0.01); meanwhile, students using maladaptive coping mechanisms (behavioral disengagement, venting and self-blame) were associated with higher perceived stress (p < 0.05) [42]. In studies by Hirsch et al., students observed to have maladaptive coping mechanisms were also found to have poorer mental health during their first three (pre-clinical) years of the four-year curriculum [36,49]. Unfortunately, maladaptive coping mechanisms such as use of alcohol and prescription or nonprescription drugs for anxiety or to aid sleep have been commonly cited as stress-relieving activities for students [35,38].
3.1.3. Non-Pharmacological Interventions to Manage Stress
A few studies evaluated interventions to determine whether they were effective in helping students manage their stress. Lemay et al. conducted a 90 min yoga and meditation intervention and found that students’ Beck Anxiety Inventory (BAI) and PSS scores decreased significantly, and their Five Facet Mindfulness Questionnaire (FFMQ) scores increased significantly at the end of the six-week study period [58]. Similarly, Zollars et al. investigated the use of the Headspace™ app on mindfulness, mental well-being and perceived stress in pharmacy students [57]. Pharmacy students, who were in their P1, P2 and P3, were instructed to meditate at least 10 min daily for four weeks using the Headspace™ app. Study results showed that the intervention was associated with improved mindfulness, overall mental well-being and decreased perceived stress. Holman et al. [50] conducted a one-year pilot wellness program for P1 through P3 students, which consisted of the following interventions: orientation to the wellness program, session on nutrition and mindfulness, in-class brain breaks and promotion of on-campus resources. While the investigators found no statistical differences between pre- and post-PSS-10 scores for P1, P2, or P3 students, they did find that students had increased wellness practices in exercise and sleep (>4 h/night) (p = 0.02). Students also reported the greatest use of and satisfaction with 5–10 min in-class wellness breaks and provided the most feedback on curricular/schedule changes (e.g., reduced course load and rescheduling of campus wellness activities to fit into the course schedule) to improve student wellness.
3.2. Burnout
Our search revealed four studies matching our criteria to assess burnout in pharmacy students (Table 3). The Maslach Burnout Inventory (MBI) by Maslach et al. [13] was used in three of the studies while one utilized the Oldenburg Burnout Inventory (OLBI) [14,51,52,53]. Using the MBI, burnout is measured in three domains consisting of emotional exhaustion (EE), depersonalization (DP) and low personal accomplishment (PA) (Table 1). The OLBI uses two measures, disengagement and exhaustion. Using the MBI, Jacoby et al. [53] reported a prevalence of burnout in 82.3% of 62 third year pharmacy students (in a four-year program) and reported rates of high EE ranging between 46% and 85% of students in the first three years of pharmacy school [53]. For DP, high rates ranged from 25% to 33% depending on the year in school, and high rates of low PA were reported as 21% to 31% in the same study. Kaur et al. [52] and Ried et al. [51] reported average EE scores as 23 and 28, respectively, with a high score considered to be greater than 27 [51,52]. Per the MBI, a score of 7 to 12 in DP is considered moderate and 13 or greater is considered a high score and at risk for burnout [13]. The average range for DP reported in these studies was 6.7 to 15.9, showing low to high DP [51,52]. Also, per the MBI, low PA is defined as a score lower than 30. The average range reported for low PA in these studies was 13.5 to 8.9 [51,52]. The MBI scores show that pharmacy students in these studies were suffering from high EE and low PA, indicating possible burnout [51,52,53]. The OLBI showed average burnout scores of 45 (maximum score = 64) with disengagement having an average sum of 22 and exhaustion 23, resulting in the higher overall score of 45 [14]. Fuller et al. [14] reported mean scores of 2.7 for disengagement and 2.9 for exhaustion on a four-point scale. These scores for disengagement were cited by the authors as being higher than Greek (2.0 and 2.8), German (1.9 and 2.6) and medical residents (2.4 and 2.5) [14].
3.2.1. Common Predictors of Burnout
There were a few common predictors of burnout that appeared in the different studies that included gender, year in school and campus location. According to Ried et al. [51] and Jacoby et al. [53], females reported more EE than males, with Jacoby et al. reporting that the EE score in females averaged 4.7 points higher than the depersonalization score [53]. Both studies, however, reported males scoring higher in depersonalization [51,53], with Jacoby et al. showing 70% of males reporting cynicism versus 41% of females [53].
The year in pharmacy school was also another common predictor. It seems the second year in pharmacy has consistently shown increases in measures related to burnout based on the available studies. Jacoby et al. conducted surveys at the start of the first year and end of the first three years of pharmacy school in a four-year program [53]. Of the students who completed all four surveys throughout the years, it was noted that burnout, which was defined as EE or cynicism in the study, increased after the start of pharmacy school and remained high through the years (p < 0.0001). Personal accomplishment scores were lower for the end of the first and second years compared to the start of the first year but there was no difference between the start of the first year and the end of the third year. Ried et al. reported that second-year students had significantly higher EE scores, by an average of 4.4 points, than first- or third-year students [51]. For PA, however, students in the second year scored higher than first-year students. Students further in the program perceived a greater lack of PA. Second-professional-year students were also more likely than first-year students to score higher on the DP domain [51].
Using the OBI, authors reported that second-year students had a 2.7 times higher risk of exhaustion than first-year students (95% CI, 1.2–6.2) [14]. Unlike exhaustion, disengagement risk was three times higher for second- and third-year students compared with first-year pharmacy students, (95% CI, 1.6–3.0) and (95% CI, 1.6–5.5), respectively. The same study also reported that unmarried students had a two times higher risk of exhaustion compared to married students (95% CI, 1.0–4.8), although this was not statistically significant.
Other findings by Jacoby et al. included students having higher EE levels when attending the main campus versus various satellite campuses [51]. When evaluating variables such as postgraduate plans, work involvement, extracurricular or co-curricular involvement, Fuller et al. did not find these variables to be significant predictors of student burnout [14].
3.2.2. Associations with Other Constructs
Jacoby et al. [53] measured empathy using the Jefferson Scale of Empathy (JSE) along with the MBI starting at the beginning of the first year and then assessing at the end of each year in pharmacy school for three years. While burnout seemed to increase from the start of the first year, empathy remained the same throughout all years [53]. Kaur et al. [52] assessed burnout and engagement in P1 and P2 students using the MBI and the Utrecht Work Engagement Scale, and correlated scores to academic self-perception measured by a subscale of the School Attitude Assessment Survey-Revised. The study found that EE and low PA had a negative correlation with students’ academic self-perception (self-perceived academic abilities) [52].
3.2.3. Non-Pharmacological Interventions to Manage Burnout
Studies assessing interventions for burnout in student pharmacists were not available. It is interesting to note that studies found similarities in terms of student characteristics leading to burnout. These include female gender and later year in school showing higher levels of EE (second and third years); higher levels of DP were also reported in males. In addition, low personal accomplishment scores were seen in the middle years of pharmacy school for most of the studies. Perhaps, interventions targeting these factors and populations may be of help as pharmacy schools work to improve overall well-being in students.
3.3. Depression and Anxiety
Our search generated eight articles that investigated pharmacy students’ depression and anxiety using validated rating scales (Table 4). There was no consistent scale or measurement used to measure students’ depression (consisting of low mood, anhedonia or other physical or cognitive symptoms) [59] or anxiety (i.e., feeling nervous, inability to control worrying, anticipatory anxiety) [59] in the published studies. The Patient Health Questionnaire, 9-item (PHQ-9) was used to measure depression in one study [59] while anxiety was measured using a variety of scales (i.e., the Generalized Anxiety Disorder, 7-item [GAD-7] [59], Beck Anxiety Inventory [58], Zung Self-Rating Anxiety Scale [60], State Trait Anxiety Inventory [STAI] [54]). Psychological or general mental health was measured using Counseling Center Assessment of Psychological Symptoms (CCAPS-62) in two studies [8,55] and Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS) in one study [15].
Overall, pharmacy students in different cohorts have high levels of anxiety that meet clinical thresholds for anxiety diagnosis; Fischbein and Bonfine [56] found pharmacy students had higher rates of anxiety when compared to medical students [56]. In two studies by Shangraw et al. and Khorassani et al., second-year pharmacy students were shown to have the highest rate of anxiety compared to students in other years of study [59,60]. Students in second year (of four-year programs) tended to have high self-reported anxiety compared to those in other years, especially fourth-year students [59,60]. This is consistent with the findings from a study by Zakeri et al. [8] who found that female students were also shown to have higher anxiety than male students as well as decreased mental health [8]. In a study by Sabourin et al. [55], no association between mental health status and GPA or exercise was shown.
According to Geslani et al., pharmacy students not only had worse mental health compared to medical students, but they also had higher levels of stigma toward mental health treatment, were less likely to seek help from counseling services or know where to seek help [33]. Academic distress should be an area of focus for student support and intervention.
3.3.1. Associations with Other Constructs
In two studies by Sabourin et al. and Fischbein et al., academic distress was shown to be correlated with depression and anxiety and moderately correlated with social anxiety [55,56]. High academic distress and family distress were associated with high clinical general anxiety [8].
3.3.2. Non-Pharmacological Interventions to Manage Mental Health Disorders
There was little published information on interventions to reduce depression or anxiety among pharmacy students. Mindfulness meditation was associated with improved mental health, anxiety and stress [57,58].
4. Discussion
Student well-being is a growing concern within academic pharmacy because studies have found high levels of student pharmacist burnout associated with maladaptive coping mechanisms [36,49,53]. Multiple intrinsic and extrinsic factors, such as personal relationship and the culture and values of the learning environment, can influence student pharmacist stress and burnout [12,61,62]. As a result, there has been an increased interest in measuring well-being within pharmacy institutions.
The PSS has been validated in numerous populations to measure stress; therefore, this scale was frequently used as the measurement of choice for studies evaluating stress within pharmacy students (Table 2). Furthermore, this freely available scale with numerous versions (4, 10, 14 items) are easily accessible and scored and can be correlated with other areas that may be of interest for pharmacy schools (e.g., academic resilience) (Table 1). The SSI was also used in one study and the College Stress Inventory (CSI) scale was used alongside the PSS. Unlike the PSS, however, the high number of survey items as well as accessibility limit the frequent utility of these scales. Numerous studies showed that there are differences in perceived stress by gender and year in curriculum [37,41,44,47,48]; academic institutions may consider measuring perceived stress among their students at baseline and, possibly, every year to evaluate this pattern at their specific institution and design appropriate interventions. This regular assessment may also be helpful if there are curricular or programmatic revisions; the validated scale may potentially be used to measure the impact of these changes on students’ perceived stress.
Surprisingly, despite the emphasis of burnout on wellness and well-being among healthcare professionals, there were very few studies using validated instruments to measure burnout among pharmacy students (Table 3). The potential reasons for this could be due to the accessibility and cost issues surrounding the gold standard scale for burnout, the MBI (Table 1). The MBI is only available through a copyright purchase agreement from MindGarden.com (accessed on 7 October 2024) and licenses are available for specific periods of time, which may not allow for easy implementation within academic institutions where repeated longitudinal assessments are necessary. While studies are limited, other burnout scales available may be an alternative solution, such as the OLBI, which is free for use (Table 1). The Copenhagen Burnout Inventory (CBI) is also another free instrument used to measure burnout. While both the OLBI and the CBI have no associated costs, there are no data available to compare the results to general population [6]. The CBI, to our knowledge, has also not been used in studies involving pharmacy students. The MBI, on the other hand, has national benchmark data that can be used to compare outcomes among pharmacy students to those among the general population and other samples. This type of normative data is not available for the OLBI or CBI. The burden to complete the burnout scales is similar, with the MBI having 22 items, the OLBI having 19 items, and the CBI having 16 items.
Mental health may be more challenging since there is a wide spectrum of domains that may encompass mental health. We chose to focus on depression and anxiety since these disorders have been highlighted as important factors among young individuals, especially in light of the COVID-19 pandemic [63]. We found that the PHQ-9 and GAD-7, both scales that are used clinically to screen for depression and anxiety, respectively, have been studied in pharmacy students. These scales may especially be desirable since they are easy to administer and score and are freely accessible (Table 1). The HRQOL scale may also be an alternate tool to measure overall health status since it is also relatively short and freely accessible from the Centers for Disease Control and Prevention [26].
Limitations
Despite our attempt to be as thorough as possible in our literature search, there may be studies that could have been missed. Publications that are not in English or those that were not available in the selected databases could have been omitted.
5. Summary and Recommendations
There are numerous validated scales to measure well-being among pharmacy students and the selection of a specific tool may depend on the construct of well-being that institutions would like to measure. Critical factors such as validity, ease of use, cost and generalizability are also important considerations.
Based on the findings from the selected studies, pharmacy students are suffering from stress, burnout, depression and anxiety. Mental health and well-being are critical to the success of pharmacy students. Pharmacy schools should consider assessing student stress using the PSS-10, depression with PHQ-9 and anxiety using the GAD-7, particularly in the second year, where there were higher rates reported. Of note, the PSS has been studied extensively in pharmacy students and has been correlated with other domains of well-being. These tools are straightforward, free for use, easy to administer and will help identify struggling students who can benefit from support. Burnout may also be assessed if the institution has the funding to cover the cost of the MBI, which is the gold standard due to the normative data comparisons available. If cost is a concern, other burnout tools as mentioned may be used to obtain an idea of how students are feeling but using those instruments will have fewer data comparisons. Assessing burnout in the second and third years may be particularly helpful to institutions to determine whether burnout exists in their student population; if so, institutions may be able to implement programs or interventions to address these specific years where burnout seems most prevalent. Of available validated scales, the PSS-10, MBI, PHQ-9 and GAD-7 are the most published among pharmacy students and are viable options to assess stress, burnout, depression and anxiety, respectively.
Author Contributions
Conceptualization, K.C.L. and S.Y.E.-I.; methodology, K.C.L., S.Y.E.-I. and A.Y.; validation, K.C.L. and S.Y.E.-I.; formal analysis, K.C.L., S.Y.E.-I. and T.B.C.; investigation, K.C.L., S.Y.E.-I. and T.B.C.; data curation, A.Y.; writing—original draft preparation, K.C.L., S.Y.E.-I., T.B.C. and A.Y.; writing—review and editing, K.C.L., S.Y.E.-I. and T.B.C.; visualization, K.C.L., S.Y.E.-I. and T.B.C.; supervision, K.C.L.; project administration, K.C.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Acknowledgments
The authors would like to thank Lisette Kaya for her research assistance.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| AACP | American College Clinical Pharmacy |
| ASCS | Academic Self-Concept Scale |
| BAI | Beck Anxiety Inventory |
| CBI | Copenhagen Burnout Inventory |
| CCAPS | Counseling Center Assessment of Psychological Symptoms |
| COPE | Coping Orientation to Problems Experienced Inventory |
| CSI | College Stress Inventory |
| DASS-21 | Depression, Anxiety and Stress Scale |
| DP | Depersonalization |
| EE | Emotional Exhaustion |
| FFMQ | Five Facet Mindfulness Questionnaire |
| FMD | Frequent Mental Distress |
| GAD-7 | Generalized Anxiety Disorder, 7 item |
| GPA | Grade Point Average |
| HRQOL | Health-Related Quality of Life Measures |
| JSE (-MS) | Jefferson Scale of Empathy, for medical students |
| OLBI | Oldenburg Burnout Inventory |
| PA | Personal Accomplishment |
| PHQ-9 | Patient Health Questionnaire, 9-item |
| PSS (-10) (-14) | Perceived Stress Scale; 10-item, 14-item |
| PS1 | Pharmacy Student Year 1 |
| PS2 | Pharmacy Student Year 2 |
| PS3 | Pharmacy Student Year 3 |
| PS4 | Pharmacy Student Year 4 |
| SF (-12) (-36) | Medical Outcome Study Health Questionnaire; 12 items, 36 items |
| SSI | Student-life Stress Inventory |
| STAI | Spielberger State-Trait Anxiety Index |
| WEMWBS | Warwick-Edinburgh Mental Well-Being Scale |
References
- National Academies of Sciences, Engineering, and Medicine. Taking Action against Clinician Burnout: A Systems Approach to Professional Well-Being; The National Academies Press: Washington, DC, USA, 2019. [Google Scholar] [CrossRef]
- Enhancing Well-Being and Resilience among the Pharmacist Workforce: A National Consensus Conference. Available online: https://www.pharmacist.com/consensusrecs (accessed on 21 September 2024).
- Miller, M.L.; Boyer, C.; Emerson, M.R.; Neville, M.W.; Skoy, E.T.; Vogt, E.M.; Volino, L.; Worrall, C.L.; Zitko, K.L.; Ross, L.J. Report of the 2017–2018 Student Affairs Standing Committee. Am. J. Pharm. Educ. 2018, 82, 7159. [Google Scholar] [CrossRef] [PubMed]
- American Association of Colleges of Pharmacy. Preparing Pharmacists and the Academy to Thrive in Challenging Times. 2021–2024 Strategic Plan Priorities, Goals and Objectives. 22 July 2021. Available online: https://www.aacp.org/sites/default/files/2023-05/StrategicPlan-2021-2024.pdf (accessed on 21 September 2024).
- National Academy of Medicine. National Plan for Health Workforce Well-Being; Dzau, V.J., Kirch, D., Murthy, V., Nasca, T., Eds.; NAM Special Publication; The National Academies Press: Washington, DC, USA, 2022; Available online: https://nap.nationalacademies.org/catalog/26744/national-plan-for-health-workforce-well-being (accessed on 21 September 2024).
- Dyrbye, L.N.; Meyers, D.; Ripp, J.; Dalal, N.; Bird, S.B.; Sen, S.; Agency for Healthcare Research & Quality; Collaborative for Healing and Renewal in Medicine; Emory University. A Pragmatic Approach for Organizations to Measure Health Care Professional Well-Being NAM Perspectives; Discussion Paper; National Academy of Medicine: Washington, DC, USA, 2018. [Google Scholar] [CrossRef]
- Mayberry, K.; Zapata, L.V.; Byers, M.; Thurston, M.M. A scoping review of well-being assessment and interventions in student pharmacists. Am. J. Pharm. Educ. 2022, 86, 8793. [Google Scholar] [CrossRef] [PubMed]
- Zakeri, M.; De La Cruz, A.; Wallace, D.; Sansgiry, S.S. General anxiety, academic distress, and family distress among doctor of pharmacy students. Am. J. Pharm. Educ. 2021, 85, 8522. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Janicki-Deverts, D. Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. J. Appl. Soc. Psychol. 2012, 42, 1320–1334. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Gadzella, B.M. Student-Life Stress Inventory: Identification of and reactions to stressors. Psychol. Rep. 1994, 74, 395–402. [Google Scholar] [CrossRef]
- Awe, C.; Gaither, C.A.; Crawford, S.Y.; Tieman, J. A comparative analysis of perceptions of pharmacy students’ stress and stressors across two multicampus universities. Am. J. Pharm. Educ. 2016, 80, 82. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E. The measurement of experienced burnout. J. Occup. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Fuller, M.; Schadler, A.; Cain, J. An investigation of prevalence and predictors of disengagement and exhaustion in pharmacy students. Am. J. Pharm. Educ. 2020, 84, 7945. [Google Scholar] [CrossRef]
- Tennant, R.; Hiller, L.; Fishwick, R.; Platt, S.; Joseph, S.; Weich, S.; Parkinson, J.; Secker, J.; Stewart-Brown, S. The Warwick-Edinburgh Mental Well-being scale (WEMWBS): Development and UK validation. Health Qual. Life Outcomes 2007, 5, 63. [Google Scholar] [CrossRef]
- Locke, B.D.; Buzolitz, J.S.; Lei, P.-W.; Boswell, J.F.; McAleavey, A.A.; Sevig, T.D.; Dowis, J.D.; Hayes, J.A. Development of the Counseling Center Assessment of Psychological Symptoms-62 (CCAPS-62). J. Couns. Psychol. 2011, 58, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.; Vagg, P.R.; Jacobs, G.A. Manual for the State-Trait Anxiety Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.; Rief, W.; Klaiberg, A.; Braehler, E. Validity of the Brief Patient Health Questionnaire Mood Scale (PHQ-9) in the general population. Gen. Hosp. Psychiatry 2006, 28, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Lowe, B.; Decker, O.; Muller, S.; Brähler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care 2008, 46, 266–274. [Google Scholar] [CrossRef]
- Beck, A.T.; Epstein, N.; Brown, G.; Steer, R.A. An inventory for measuring clinical anxiety: Psychometric properties. J. Consult. Clin. Psychol. 1988, 56, 893–897. [Google Scholar] [CrossRef]
- Julian, L.J. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res. 2011, 63, S467–S472. [Google Scholar] [CrossRef]
- Henry, J.D.; Crawford, J.R. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2005, 44, 227–239. [Google Scholar] [CrossRef]
- Dunstan, D.A.; Scott, N. Norms for Zung’s Self-rating Anxiety Scale. BMC Psychiatry 2020, 20, 90. [Google Scholar] [CrossRef]
- Zung, W.W. A rating instrument for anxiety disorders. Psychosomatics 1971, 12, 371–379. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Measuring Healthy Days: Population Assessment of Health-Related Quality of Life. 2000. Available online: https://stacks.cdc.gov/view/cdc/6406 (accessed on 21 September 2024).
- Baer, R.A.; Smith, G.T.; Hopkins, J.; Krietemeyer, J.; Toney, L. Using self-report assessment methods to explore facets of mindfulness. Assessment 2006, 13, 27–45. [Google Scholar] [CrossRef]
- Park, T.; Yusuf, A.A.; Hadsall, R.S. Pharmacy students’ attitudes toward debt. Am. J. Pharm. Educ. 2015, 79, 52. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S. You want to measure coping but your protocol’s too long: Consider the brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, W.M. Measurement of academic self-concept in college students. J. Personal. Assess. 1988, 52, 223–240. [Google Scholar] [CrossRef]
- Leidy, N.K. Operationalizing Maslow’s theory: Development and testing of the basic need satisfaction inventory. Issues Ment. Health Nurs. 1994, 15, 277–295. [Google Scholar] [CrossRef]
- Canales-Gonzales, P.L.; Kranz, P.L. Perceived stress by students in a pharmacy curriculum. Education 2008, 129, 139–144. [Google Scholar]
- Geslani, G.P.; Gaebelein, C.J. Perceived stress, stressors, and mental distress among doctor of pharmacy students. Soc. Behav. Pers. 2013, 41, 1457–1468. [Google Scholar] [CrossRef]
- Gupchup, G.V.; Borrego, M.E.; Konduri, N. The impact of student life stress on health related quality of life among doctor of pharmacy students. Coll. Stud. J. 2004, 38, 292–302. [Google Scholar]
- Marshall, L.L.; Allison, A.; Nykamp, D.; Lanke, S. Perceived stress and quality of life among doctor of pharmacy students. Am. J. Pharm. Educ. 2008, 72, 137. [Google Scholar] [CrossRef]
- Hirsch, J.D.; Do, A.H.; Hollenbach, K.A.; Manoguerra, A.S.; Adler, D.S. Students’ health-related quality of life across the preclinical pharmacy curriculum. Am. J. Pharm. Educ. 2009, 73, 147. [Google Scholar] [CrossRef]
- Votta, R.J.; Benau, E.M. Predictors of stress in doctor of pharmacy students: Results from a nation wide survey. Curr. Pharm. Teach. Learn. 2013, 5, 365–372. [Google Scholar] [CrossRef]
- Frick, L.J.; Frick, J.L.; Coffman, R.E.; Dey, S. Student stress in a three-year doctor of pharmacy program using a mastery learning educational model. Am. J. Pharm. Educ. 2011, 75, 64. [Google Scholar] [CrossRef] [PubMed]
- Ford, K.C.; Busuyi, O.S.; Thach, A.V. Factors contributing to perceived stress among doctor of pharmacy (PharmD) students. Coll. Stud. J. 2014, 48, 189–198. [Google Scholar]
- Beall, J.W.; DeHart, R.M.; Riggs, R.M.; Hensley, J. Perceived stress, stressors, and coping mechanisms among doctor of pharmacy students. Pharmacy 2015, 3, 344–354. [Google Scholar] [CrossRef] [PubMed]
- Chisholm-Burns, M.A.; Spivey, C.A.; Jaeger, M.C.; Williams, J. Associations between pharmacy students’ attitudes toward debt, stress, and student loans. Am. J. Pharm. Educ. 2017, 81, 5918. [Google Scholar] [CrossRef]
- Garber, M.C. Exercise as a stress coping mechanism in a pharmacy student population. Am. J. Pharm. Educ. 2017, 81, 50. [Google Scholar] [CrossRef]
- Garber, M.C.; Huston, S.A.; Breese, C.R. Sources of stress in a pharmacy student population. Curr. Pharm. Teach. Learn. 2019, 11, 329–337. [Google Scholar] [CrossRef]
- Spivey, C.A.; Havrda, D.; Stallworth, S.; Renfro, C.; Chisholm-Burns, M.A. Longitudinal examination of perceived stress and academic performance of first-year student pharmacists. Curr. Pharm. Teach. Learn. 2020, 12, 1116–1122. [Google Scholar] [CrossRef]
- Maynor, L.M.; Baugh, G.M. Perceived stress, academic self concept, and coping strategies of pharmacy students. Int. J. Pharm. Educ. Pr. 2012, 9, 2–9. [Google Scholar]
- Maynor, L.; Galvez-Peralta, M.; Barrickman, A.; Hanif, A.; Baugh, G. Perceived stress, academic self-concept, and coping mechanisms among pharmacy students following a curricular revision. Curr. Pharm. Teach. Learn. 2022, 14, 159–165. [Google Scholar] [CrossRef]
- Saul, B.; Andrews, S.; Hartman, J.; Perez, S.; Chavez, M.L.; Frietze, G.A. Assessment of stress and quality of life in non-native and native english-speaking pharmacy students. Am. J. Pharm. Educ. 2021, 85, 8351. [Google Scholar] [CrossRef]
- Verdone, M.; Murray, M. Stress and basic need satisfaction of first-year healthcare professional students. Med. Sci. Educ. 2021, 31, 519–525. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, J.D.; Nemlekar, P.; Phuong, P.; Hollenbach, K.A.; Lee, K.C.; Adler, D.S.; Morello, C.M. Patterns of stress, coping and health-related quality of life in doctor of pharmacy students. Am. J. Pharm. Educ. 2020, 84, 7547. [Google Scholar] [CrossRef] [PubMed]
- Holman, S.K.; Folz, H.N.; Ford, B.; Moore, S.; Moody, A. Design and implementation of a pilot student wellness program at a school of pharmacy. Curr. Pharm. Teach. Learn. 2021, 13, 1471–1477. [Google Scholar] [CrossRef] [PubMed]
- Ried, L.D.; Motycka, C.; Mobley, C.; Meldrum, M. Comparing self-reported burnout of pharmacy students on the founding campus with those at distance campuses. Am. J. Pharm. Educ. 2006, 70, 114. [Google Scholar] [CrossRef] [PubMed]
- Kaur, M.; Long, J.W.; Luk, F.S.; Mar, J.; Nguyen, D.L.; Ouabo, T.; Singh, J.; Wu, B.; Rajagopalan, V.; Schulte, M.; et al. Relationship of burnout and engagement to pharmacy students’ perception of their academic ability. Am. J. Pharm. Educ. 2020, 84, 7571. [Google Scholar] [CrossRef]
- Jacoby, J.L.; Cole, J.D.; Ruble, M.J.; Smith, A.B.; Laubach, L.T.; Greenberg, M.R.; Macfarlan, J.E.; DeWaay, D.J.; Barraco, R.D.; Shigo, E.; et al. Measures of burnout and empathy in United States doctor of pharmacy students: Time for a change? J. Pharm. Pr. 2022, 35, 940–946. [Google Scholar] [CrossRef]
- Longyhore, D.S. Pharmacy student anxiety and success with objective structured clinical examinations. Am. J. Pharm. Educ. 2017, 81, 7. [Google Scholar] [CrossRef]
- Sabourin, A.A.; Prater, J.C.; Mason, N.A. Assessment of mental health in doctor of pharmacy students. Curr. Pharm. Teach. Learn. 2019, 11, 243–250. [Google Scholar] [CrossRef]
- Fischbein, R.; Bonfine, N. Pharmacy and medical Students’ mental health symptoms, experiences, attitudes and help-seeking behaviors. Am. J. Pharm. Educ. 2019, 83, 7558. [Google Scholar] [CrossRef]
- Zollars, I.; Poirier, T.I.; Pailden, J. Effects of mindfulness meditation on mindfulness, mental well-being, and perceived stress. Curr. Pharm. Teach. Learn. 2019, 11, 1022–1028. [Google Scholar] [CrossRef]
- Lemay, V.; Hoolahan, J.; Buchanan, A. Impact of a yoga and meditation intervention on students’ stress and anxiety levels. Am. J. Pharm. Educ. 2019, 83, 7001. [Google Scholar] [CrossRef] [PubMed]
- Shangraw, A.M.; Silvers, J.; Warholak, T.; Vadiei, N. Prevalence of anxiety and depressive symptoms among pharmacy students. Am. J. Pharm. Educ. 2021, 85, 8166. [Google Scholar] [CrossRef] [PubMed]
- Khorassani, F.; Hassani, B.; Conry, J.; Espejo, G. Evaluation of anxiety in doctor of pharmacy students in their first through fourth professional years. Curr. Pharm. Teach. Learn. 2021, 13, 628–634. [Google Scholar] [CrossRef] [PubMed]
- Schommer, J.C.; Gaither, C.A.; Goode, J.-V.R.; Owen, J.A.; Scime, G.M.; Skelton, J.B.; Cernasev, A.; Hillman, L.A. Pharmacist and student pharmacist views of professional and personal well-being and resilience. JAPhA 2020, 60, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Babal, J.C.; Abraham, O.; Webber, S.; Watterson, T.; Moua, P.; Chen, J. Student pharmacist perspectives on factors that influence wellbeing during pharmacy school. Am. J. Pharm. Educ. 2020, 84, ajpe7831. [Google Scholar] [CrossRef]
- Czeisler, M.É.; Lane, R.I.; Petrosky, E.; Wiley, J.F.; Christensen, A.; Njai, R.; Weaver, M.D.; Robbins, R.; Facer-Childs, E.R.; Barger, L.K.; et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic—United States, 24–30 June 2020. MMWR. Morb. Mortal. Wkly. Rep. 2020, 69, 1049–1057. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).