Study on the Consumption of Non-Steroidal Anti-Inflammatory Drugs and Antibiotics by the Brazilian Adult Population: A Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Target Population
2.2. Questionnaire
- Gender—( ) Female ( ) Male ( ) Prefer Not To Answer.
- Age—options with age groups.
- Education—options with schooling.
- Which region of Brazil do you live in?—options with Brazilian regions.
- Have you taken any medication for pain and/or inflammation in the last 90 days?—options with the most common generic and trade names of anti-inflammatory/analgesic drugs.
- For how many days?—day period options.
- What was the main reason you took the medication?—options with the most common types of pain/inflammation.
- Have you had any adverse reactions to the anti-inflammatory/analgesic?—options with the most common adverse reactions.
- Have you taken any medication to treat an infection in the last 90 days?—options with the most common generic and trade names of antibiotics.
- For how many days?—day interval options.
- What was the main reason you took the medicine?—options with the most common types of infections.
- Has this medicine been prescribed (this time) by a professional (doctor or dentist)? ( ) Yes ( ) No.
- Have you had any adverse reactions to the antibiotic?—options with the most common adverse reactions.
- Is there anything else you’d like to say?
3. Results
3.1. Sociodemographic Data
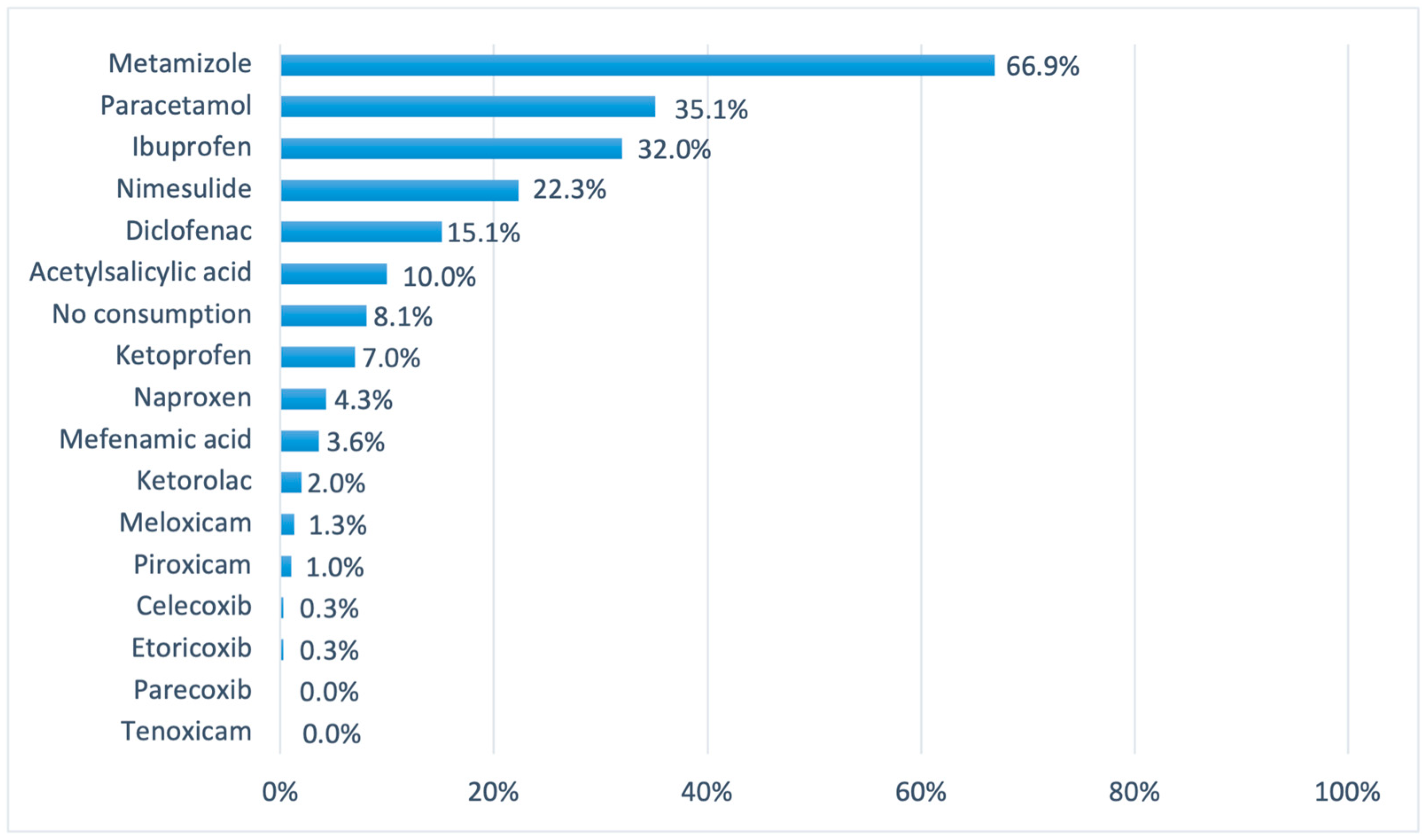
3.2. Consumption of NSAIDs and Antibiotics by Volunteers
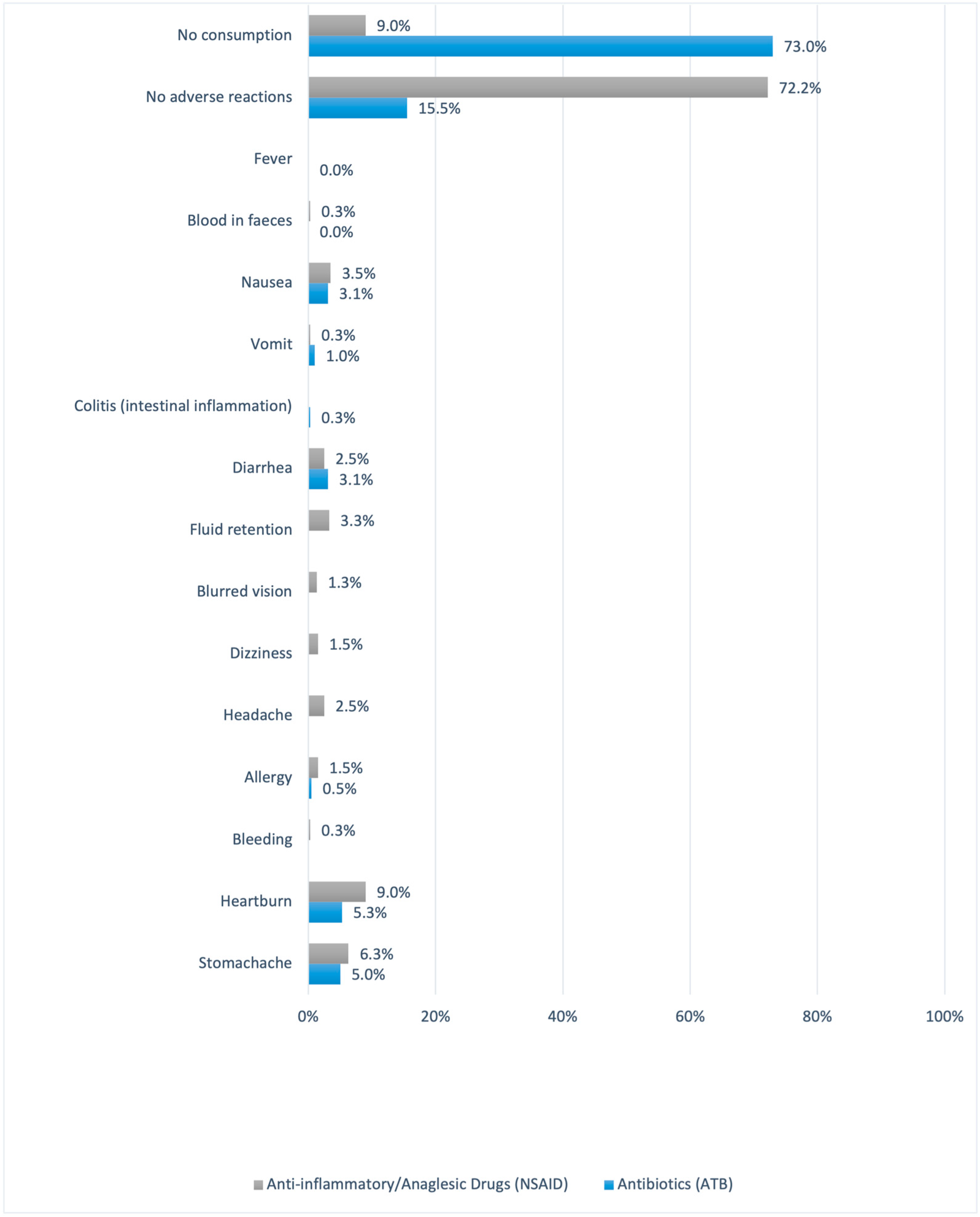
3.3. Adverse Effects
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ghodkhande, K.P.; Choudhari, S.G.; Gaidhane, A. Self-Medication Practices among the Geriatric Population: A Systematic Literature Review. Cureus 2023, 15, e42282. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, C.T.; Nguyen, H.T.; Boyer, L.; Auquier, P.; Fond, G.; Do, K.N.; Dang, A.K.; Do, H.P.; Latkin, C.A.; Ho, R.C.M.; et al. Prevalence and impacts of self-medication in a disadvantaged setting: The importance of multi-dimensional health interventions. Front. Public Health 2023, 11, 1176730. [Google Scholar] [CrossRef] [PubMed]
- Chisavu, L.; Chisavu, F.; Marc, L.; Mihaescu, A.; Bob, F.; Licker, M.; Ivan, V.; Schiller, A. Bacterial Resistances and Sensibilities in a Tertiary Care Hospital in Romania—A Retrospective Analysis. Microorganisms 2024, 12, 1517. [Google Scholar] [CrossRef]
- Sachdev, C.; Anjankar, A.; Agrawal, J. Self-Medication with Antibiotics: An Element Increasing Resistance. Cureus 2022, 14, e30844. [Google Scholar] [CrossRef]
- Tang, K.W.K.; Millar, B.C.; Moore, J.E. Antimicrobial Resistance (AMR). Br. J. Biomed. Sci. 2023, 80, 11387. [Google Scholar] [CrossRef] [PubMed]
- Mdingi, V.S.; Gens, L.; Mys, K.; Varga, P.; Zeiter, S.; Marais, L.C.; Richards, R.G.; Moriarty, F.T.; Chittò, M. Short-Term Celecoxib Promotes Bone Formation without Compromising Cefazolin Efficacy in an Early Orthopaedic Device-Related Infection: Evidence from a Rat Model. Antibiotics 2024, 13, 715. [Google Scholar] [CrossRef]
- Amedi, D.; Gazerani, P. Deprescribing NSAIDs: The Potential Role of Community Pharmacists. Pharmacy 2024, 12, 116. [Google Scholar] [CrossRef]
- Gwee, K.A.; Goh, V.; Lima, G.; Setia, S. Coprescribing proton-pump inhibitors with nonsteroidal anti-inflammatory drugs: Risks versus benefits. J. Pain Res. 2018, 11, 361–374. [Google Scholar] [CrossRef]
- Guo, C.G.; Leung, W.K. Potential Strategies in the Prevention of Nonsteroidal Anti-inflammatory Drugs-Associated Adverse Effects in the Lower Gastrointestinal Tract. Gut Liver 2020, 14, 179–187. [Google Scholar] [CrossRef]
- Goldstein, J.L.; Cryer, B. Gastrointestinal injury associated with NSAID use: A case study and review of risk factors and preventative strategies. Drug Healthc. Patient Saf. 2015, 7, 31–41. [Google Scholar] [CrossRef]
- Rehman, M.; Ahmed, S.; Ahmed, U.; Tamanna, K.; Sabir, M.S.; Niaz, Z. An overview of self-medication: A major cause of antibiotic resistance and a threat to global public health. J. Pak. Med. Assoc. 2021, 71, 943–949. [Google Scholar] [CrossRef] [PubMed]
- Hijos-Mallada, G.; Sostres, C.; Gomollón, F. NSAIDs, gastrointestinal toxicity and inflammatory bowel disease. Gastroenterol. Hepatol. 2022, 45, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Bindu, S.; Mazumder, S.; Bandyopadhyay, U. Non-steroidal anti-inflammatory drugs (NSAIDs) and organ damage: A current perspective. Biochem. Pharmacol. 2020, 180, 114147. [Google Scholar] [CrossRef] [PubMed]
- Lucas, G.N.C.; Leitaõ, A.C.C.; Alencar, R.L.; Xavier, R.M.F.; Daher, E.D.F.; Silva, G.B.D. Pathophysiological aspects of nephropathy caused by non-steroidal anti-inflammatory drugs. J. Bras. Nefrol. 2019, 41, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Drożdżal, S.; Lechowicz, K.; Szostak, B.; Rosik, J.; Kotfis, K.; Machoy-Mokrzyńska, A.; Białecka, M.; Ciechanowski, K.; Gawrońska-Szklarz, B. Kidney damage from nonsteroidal anti-inflammatory drugs—Myth or truth? Review of selected literature. Pharmacol. Res. Perspect. 2021, 9, e00817. [Google Scholar] [CrossRef]
- Agência Nacional de Vigilância Sanitária (ANVISA). Available online: https://antigo.anvisa.gov.br/listagem-de-alertas/-/asset_publisher/R6VaZWsQDDzS/content/alerta-snvs-anvisa-nuvig-ufarm-n-4-de-9-de-novembro-de-2006/33868?inheritRedirect=false (accessed on 11 September 2024).
- Gov.br—Governo Federal. Available online: https://www.in.gov.br/en/web/dou/-/instrucao-normativa-in-n-285-de-7-de-marco-de-2024-547762853 (accessed on 11 September 2024).
- Sandoval, A.C.; Fernandes, D.R.; Silva, E.A.; Terra Júnior, A.T. O uso indiscriminado dos Anti-Inflamatórios Não Esteroidais (AINES). Rev. Científica Fac. Educ. E Meio Ambiente 2017, 8, 165–176. [Google Scholar] [CrossRef]
- Política Nacional de Medicamentos—Ministério da Saúde. Available online: https://bvsms.saude.gov.br/bvs/publicacoes/politica_medicamentos.pdf (accessed on 13 September 2024).
- Uso Racional de Medicamentos—Ministério da Saúde. Available online: https://www.gov.br/saude/pt-br/composicao/sectics/daf/uso-racional-de-medicamentos (accessed on 13 September 2024).
- Lam, W.Y.; Fresco, P. Medication Adherence Measures: An Overview. Biomed. Res. Int. 2015, 2015, 217047. [Google Scholar] [CrossRef]
- Albarqouni, L.; Palagama, S.; Chai, J.; Sivananthajothy, P.; Pathirana, T.; Bakhit, M.; Arab-Zozani, M.; Ranakusuma, R.; Cardona, M.; Scott, A.; et al. Overuse of medications in low- and middle-income countries: A scoping review. Bull. World Health Organ. 2023, 101, 36. [Google Scholar] [CrossRef]
- Machowska, A.; Lundborg, C.S. Drivers of Irrational Use of Antibiotics in Europe. Int. J. Environ. Res. Public Health 2019, 16, 27. [Google Scholar] [CrossRef]
- Naves, J.d.O.S.; Silver, L.D. Evaluation of pharmaceutical assistance in public primary care in Brasilia, Brazil. Rev. Saude Publica 2005, 39, 223–230. [Google Scholar] [CrossRef]
- Ferreira, F.d.C.G.; de Luna, G.G.; Izel, I.C.M.; de Almeida, A.C.G. O impacto da prática da automedicação no Brasil: Revisão Sistemática/The impact of the practice of self-medication in Brazil: Systematic Review. Braz. Appl. Sci. Rev. 2021, 5, 1505–1518. [Google Scholar] [CrossRef]
- Behzadifar, M.; Behzadifar, M.; Aryankhesal, A.; Ravaghi, H.; Baradaran, H.R.; Sajadi, H.S.; Khaksarian, M.; Bragazzi, N.L. Prevalence of self-medication in university students: Systematic review and meta-analysis. East. Mediterr. Health J. 2020, 26, 846–857. [Google Scholar] [CrossRef] [PubMed]
- Fetensa, G.; Tolossa, T.; Etafa, W.; Fekadu, G. Prevalence and predictors of self-medication among university students in Ethiopia: A systematic review and meta-analysis. J. Pharm. Policy Pract. 2021, 14, 107. [Google Scholar] [CrossRef]
- Consolazio, D.; Gattoni, M.E.; Russo, A.G. Exploring gender differences in medication consumption and mortality in a cohort of hypertensive patients in Northern Italy. BMC Public Health 2022, 22, 768. [Google Scholar] [CrossRef] [PubMed]
- Redondo-Sendino, Á.; Guallar-Castillón, P.; Banegas, J.R.; Rodríguez-Artalejo, F. Gender differences in the utilization of health-care services among the older adult population of Spain. BMC Public Health 2006, 6, 155. [Google Scholar] [CrossRef]
- Hiller, J.; Schatz, K.; Drexler, H. Gender influence on health and risk behavior in primary prevention: A systematic review. J. Public Health 2017, 2, 339–349. [Google Scholar] [CrossRef]
- Conaghan, P.G. A turbulent decade for NSAIDs: Update on current concepts of classification, epidemiology, comparative efficacy, and toxicity. Rheumatol. Int. 2012, 32, 1491–1502. [Google Scholar] [CrossRef]
- Brune, K.; Patrignani, P. New insights into the use of currently available non-steroidal anti-inflammatory drugs. J. Pain Res. 2015, 8, 105–118. [Google Scholar] [CrossRef]
- Balmanno, A.; Falconer, J.R.; Ravuri, H.G.; Mills, P.C. Strategies to Improve the Transdermal Delivery of Poorly Water-Soluble Non-Steroidal Anti-Inflammatory Drugs. Pharmaceutics 2024, 16, 675. [Google Scholar] [CrossRef]
- Ylä-Rautio, H.; Siissalo, S.; Leikola, S. Drug-related problems and pharmacy interventions in non-prescription medication, with a focus on high-risk over-the-counter medications. Int. J. Clin. Pharm. 2020, 42, 786. [Google Scholar] [CrossRef]
- Chaaban, T.; Ezzeddine, Z.; Ghssein, G. Antibiotic Misuse during the COVID-19 Pandemic in Lebanon: A Cross-Sectional Study. COVID 2024, 4, 921–929. [Google Scholar] [CrossRef]
- Munita, J.M.; Arias, C.A. Mechanisms of Antibiotic Resistance. Microbiol. Spectr. 2016, 4. [Google Scholar] [CrossRef] [PubMed]
- Bhuvaraghan, A.; King, R.; Larvin, H.; Aggarwal, V.R. Antibiotic Use and Misuse in Dentistry in India—A Systematic Review. Antibiotics 2021, 10, 1459. [Google Scholar] [CrossRef] [PubMed]
- Semenova, Y.; Kassym, L.; Kussainova, A.; Aimurziyeva, A.; Makalkina, L.; Avdeyev, A.; Yessmagambetova, A.; Smagul, M.; Aubakirova, B.; Akhmetova, Z.; et al. Knowledge, Attitudes, and Practices towards Antibiotics, Antimicrobial Resistance, and Antibiotic Consumption in the Population of Kazakhstan. Antibiotics 2024, 13, 718. [Google Scholar] [CrossRef]


| Percentage (%) | ||
|---|---|---|
| Gender | Male | 28.2% |
| Female | 71.8% | |
| Age | 18 to 28 years old | 52.3% |
| 29 to 39 years old | 18.5% | |
| 40 to 50 years old | 13.5% | |
| 51 to 61 years old | 10.3% | |
| 62 years old and over | 5.5% | |
| Education | Incomplete Elementary School | 0.5% |
| Complete Elementary School | 0.5% | |
| Incomplete High School | 0.8% | |
| Complete High School | 16% | |
| Incomplete Higher Education | 35% | |
| Complete Higher Education | 21.3% | |
| Postgraduate, Master’s and PhD | 26% | |
| Brazil region | South Region | 3.8% |
| Southeast Region | 81% | |
| Central-West Region | 8.8% | |
| North Region | 1.2% | |
| Northeast Region | 5.2% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pedrolongo, D.A.; Sagioneti, F.T.; Weckwerth, G.M.; Oliveira, G.M.; Santos, C.F.; Calvo, A.M. Study on the Consumption of Non-Steroidal Anti-Inflammatory Drugs and Antibiotics by the Brazilian Adult Population: A Cohort Study. Pharmacy 2024, 12, 150. https://doi.org/10.3390/pharmacy12050150
Pedrolongo DA, Sagioneti FT, Weckwerth GM, Oliveira GM, Santos CF, Calvo AM. Study on the Consumption of Non-Steroidal Anti-Inflammatory Drugs and Antibiotics by the Brazilian Adult Population: A Cohort Study. Pharmacy. 2024; 12(5):150. https://doi.org/10.3390/pharmacy12050150
Chicago/Turabian StylePedrolongo, Douglas Araujo, Fernanda Teixeira Sagioneti, Giovana Maria Weckwerth, Gabriela Moraes Oliveira, Carlos Ferreira Santos, and Adriana Maria Calvo. 2024. "Study on the Consumption of Non-Steroidal Anti-Inflammatory Drugs and Antibiotics by the Brazilian Adult Population: A Cohort Study" Pharmacy 12, no. 5: 150. https://doi.org/10.3390/pharmacy12050150
APA StylePedrolongo, D. A., Sagioneti, F. T., Weckwerth, G. M., Oliveira, G. M., Santos, C. F., & Calvo, A. M. (2024). Study on the Consumption of Non-Steroidal Anti-Inflammatory Drugs and Antibiotics by the Brazilian Adult Population: A Cohort Study. Pharmacy, 12(5), 150. https://doi.org/10.3390/pharmacy12050150







