Student Stress, Coping, and APPE Readiness at Two Public Institutions before and during the Pandemic
Abstract
1. Introduction
2. Materials and Methods
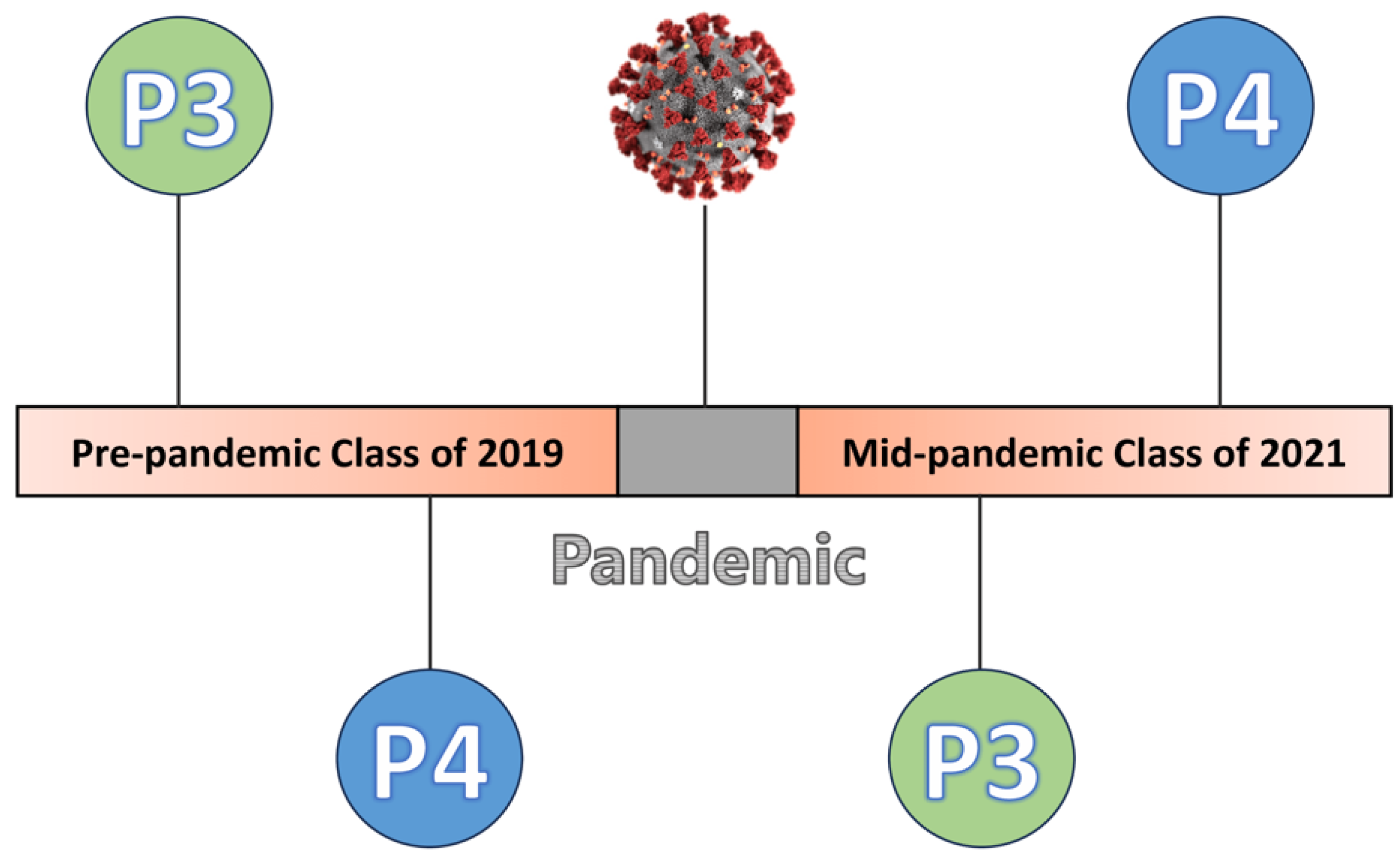
2.1. Design
2.2. Instruments
2.3. Data Collection
2.4. Data Analysis and Interpretation
3. Results
3.1. Perceived Stress
3.2. Brief COPE
3.3. Academic and Professional Development Skills
3.4. Confidence Level for APPE Practice Readiness
3.5. Correlation between PSS and Academic and Professional Development Skills
3.6. Correlation between PSS and APPE Practice Readiness
4. Discussion
4.1. Stress and Coping
4.2. Academic and Professional Developmental Skills
4.3. Confidence in APPE Practice Readiness
4.4. Correlations between PSS and Academic and Professional Development Skills and APPE Practice Readiness
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. “Standards 2025”. 2024. Available online: https://www.acpe-accredit.org/pdf/Standard2025DRAFTForComment.pdf (accessed on 13 June 2024).
- Rao, S. Predictors of student preparedness for advanced pharmacy practice experiences. BMC Med. Educ. 2024, 24, 298. [Google Scholar] [CrossRef]
- Hanselin, M.R.; Martell, C.W.; Knutsen, S.; Haight, R.C.; Moote, R. Development of a capstone course to improve student confidence and pharmacotherapy knowledge prior to advanced pharmacy practice experiences. Curr. Pharm. Teach. Learn. 2016, 8, 323–331. [Google Scholar] [CrossRef]
- Frankart, L.M.; Matulewicz, A.T.; Crane, W.B.P.; Patterson, J.; Bond, R.; Donohoe, K.L. A classroom-based patient case activity as a potential formative indicator of pre-advanced pharmacy practice experience readiness. Curr. Pharm. Teach. Learn. 2022, 14, 514–520. [Google Scholar] [CrossRef] [PubMed]
- Call, W.B.; Grice, G.R.; Tellor, K.B.; Armbruster, A.L.; Spurlock, A.M.; Berry, T.M. Predictors of Student Failure or Poor Performance on Advanced Pharmacy Practice Experiences. Am. J. Pharm. Educ. 2020, 84, ajpe7890. [Google Scholar] [CrossRef]
- Alexander, K.; Eiland, L.S.; Andrus, M. Teaching of the patient workup process improves students’ perceptions of preparation for advanced pharmacy practice experiences. Curr. Pharm. Teach. Learn. 2022, 14, 366–371. [Google Scholar] [CrossRef] [PubMed]
- Son, C.; Hegde, S.; Smith, A.; Wang, X.; Sasangohar, F. Effects of COVID-19 on College Students’ Mental Health in the United States: Interview Survey Study. J. Med. Internet. Res. 2020, 22, e21279. [Google Scholar] [CrossRef] [PubMed]
- Elharake, J.A.; Akbar, F.; Malik, A.A.; Gilliam, W.; Omer, S.B. Mental Health Impact of COVID-19 among Children and College Students: A Systematic Review. Child. Psychiatry Hum. Dev. 2023, 54, 913–925. [Google Scholar] [CrossRef]
- Mirzaian, E.; White, S.J.; Karim, M.; Franson, K.L.; Wu, M.; Wang, Y. Exploring the Effect of Virtual Education on Student Pharmacists’ Confidence toward APPE Readiness. Pharmacy 2022, 10, 118. [Google Scholar] [CrossRef] [PubMed]
- Pham, D.M.; Yang, J.X.; Lee, K.C. Changes in Perceived Stress of Pharmacy Students Pre- and Mid-COVID-19 Pandemic. Pharmacy 2022, 10, 114. [Google Scholar] [CrossRef]
- Khosraviani, V.; Ip, E.J.; Li, S.A.; Kohsraviani, A.; Cariaga, J.; Caballero, J.; Lor, K.; Acree, L.; Echibe, C.; Barnett, M.J. Changes in perceived stress and food or housing insecurity associated with COVID-19 in doctor of pharmacy students: A pre- and current- COVID-19 survey. Explor. Res. Clin. Soc. Pharm. 2024, 13, 100391. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Janicki-Deverts, D. Who’s Stressed? Distributions of Psychological Stress in the United States in Probability Samples from 1983, 2006, and 2009. J. Appl. Soc. Psychol. 2012, 42, 1320–1334. [Google Scholar] [CrossRef]
- Marshall, L.L.; Allison, A.; Nykamp, D.; Lanke, S. Perceived Stress and Quality of Life Among Doctor of Pharmacy Students. Am. J. Pharm. Educ. 2008, 72, 137. [Google Scholar] [CrossRef] [PubMed]
- Maynor, L.; Gálvez-Peralta, M.; Barrickman, A.; Hanif, A.; Baugh, G. Perceived stress, academic self-concept, and coping mechanisms among pharmacy students following a curricular revision. Curr. Pharm. Teach. Learn. 2022, 14, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Saul, B.; Andrews, S.; Hartman, J.; Perez, S.; Chavez, M.L.; Frietze, G.A. Assessment of Stress and Quality of Life in Non-native and Native English-speaking Pharmacy Students. Am. J. Pharm. Educ. 2021, 85, 8351. [Google Scholar] [CrossRef]
- Taylor, J.M. Psychometric analysis of the Ten-Item Perceived Stress Scale. Psychol. Assess. 2015, 27, 90–101. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S. You want to measure coping but your protocol’ too long: Consider the brief cope. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Cat, T.B.; El-Ibiary, S.Y.; Lee, K.C. Evaluation of a Well-being Promotion (WelPro) Program on Advanced Pharmacy Practice Experience (APPE) Student Burnout. Am. J. Pharm. Educ. 2023, 87, 100071. [Google Scholar] [CrossRef]
- Peng, P.; Hao, Y.; Liu, Y.; Chen, S.; Wang, Y.; Yang, Q.; Wang, X.; Li, M.; Wang, Y.; He, L.; et al. The prevalence and risk factors of mental problems in medical students during COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2023, 321, 167–181. [Google Scholar] [CrossRef]
- Kerr, A.M.; Spaeth, L.D.; Gerome, J.M. Medical Students’ Stress and Uncertainty during the COVID-19 Pandemic. Health Commun. 2023, 38, 2247–2257. [Google Scholar] [CrossRef]
- Ramachandran, S.; Shayanfar, M.; Brondani, M. Stressors and mental health impacts of COVID-19 in dental students: A scoping review. J. Dent. Educ. 2023, 87, 326–342. [Google Scholar] [CrossRef] [PubMed]
- Votta, R.J.; Benau, E.M. Sources of stress for pharmacy students in a nationwide sample. Curr. Pharm. Teach. Learn. 2014, 6, 675–681. [Google Scholar] [CrossRef]
- Cohen, S.; Williamson, G.M. Perceived Stress in a Probability Sample of the United States. In The Social Psychology of Health; Spacapan, S., Oskamp, S., Eds.; Sage: Newbury Park, CA, USA, 1988; pp. 31–67. [Google Scholar]
- Lebovitz, L.; Rudolph, M. Update on Pharmacist Workforce Data and Thoughts on How to Manage the Oversupply. Am. J. Pharm. Educ. 2020, 84, ajpe7889. [Google Scholar] [CrossRef]
- ASHP Match Statistics. Available online: https://natmatch.com/ashprmp/stats.html (accessed on 13 June 2024).
- Maslach, C.; Jackson, S.E. The measurement of experienced burnout. J. Organ. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Zavaleta, J.C.; Alva, R.Y.; Vargas, S.V.; Medina, E.F.; Somoza, Y.P.; Andrade-Arenas, L. Relationship between Stress and Academic Performance: An Analysis in Virtual Mode. Int. J. Adv. Comput. Sci. Appl. 2021, 12, 823–833. [Google Scholar] [CrossRef]
- Hettinger, K.N.; Baker, C.M.; Brelage, M.E.; Smith, H.M.; Woodyard, J.L. The Impact of COVID-19 on Pharmacy Student Stress during High-Stakes, Performance-Based Assessments in Skills-Based Courses. Am. J. Pharm. Educ. 2023, 87, ajpe8874. [Google Scholar] [CrossRef]
- Liu, L.; Caliph, S.; Simpson, C.; Khoo, R.Z.; Neviles, G.; Muthumuni, S.; Lyongs, K.M. Pharmacy Student Challenges and Strategies towards Initial COVID-19 Curriculum Changes. Healthcare 2021, 9, 1322. [Google Scholar] [CrossRef] [PubMed]
- Carrion, A.J.; Ridley, A.; Rasaki, A.A.; Journee, B.; McCants, T.A. Impact of COVID-19 on the academic performance and mental health of HBCU pharmacy students. Curr. Pharm. Teach. Learn. 2023, 15, 123–129. [Google Scholar] [CrossRef]
- Rahmati, Z. The Study of Academic Burnout in Students with High and Low Level of Self-efficacy. Procedia Soc. Behav. Sci. 2015, 171, 49–55. [Google Scholar] [CrossRef]
- Kaur, M.; Long, J.W.; Luk, F.S.; Mar, J.; Nguyen, D.L.; Ouabo, T.; Singh, J.; Wu, B.; Rajagopalan, V.; Schulte, M.; et al. Relatio ship of Burnout and Engagement to Pharmacy Students’ Perception of Their Academic Ability. Am. J. Pharm. Educ. 2020, 84, 7571. [Google Scholar] [CrossRef]
- U.S.Department of Defense. Trump Administration Partners with CVS and Walgreens to Provide COVID-19 Vaccine to Protect Vulnerable Americans in Long-Term Care Facilities Nationwide. Available online: https://www.defense.gov/News/Releases/Release/Article/2384541/trump-administration-partners-with-cvs-and-walgreens-to-provide-covid-19-vaccin/ (accessed on 13 June 2024).
- Opam, K.; de León, C. The New York Times. Why Are States Imposing Coronavirus Curfews? Available online: https://www.nytimes.com/2020/11/21/us/coronavirus-curfew.html (accessed on 13 June 2024).
- Nam, J. Best Colleges 2023. How Has COVID Affected College Students? Available online: https://www.bestcolleges.com/research/how-has-covid-affected-college-students/ (accessed on 13 June 2024).
- U.S. Bureau of Labor Statistics. 6.2 Million Unable to Work Because Employer Closed or Lost Business Due to the Pandemic. June 2021. Available online: https://www.bls.gov/opub/ted/2021/6-2-million-unable-to-work-because-employer-closed-or-lost-business-due-to-the-pandemic-june-2021.htm (accessed on 13 June 2024).
- Garofoli, G.K.; Gálvez-Peralta, M.; Barrickman, A.L.; Goodhart, A.L.; Johnson, H.; McMillan, A.N.; Elswick, B.M.; Newmeyer, E.S.; Burrell, C.N.; Capehart, K.D.; et al. Establishment and evaluation of scalable COVID-19 vaccine clinics at a large university. J. Am. Pharm. Assoc. 2022, 62, 1430–1437. [Google Scholar] [CrossRef] [PubMed]
- Aruru, M.; Truong, H.A.; Clark, S. Pharmacy Emergency Preparedness and Response (PEPR): A proposed framework for expanding pharmacy professionals’ roles and contributions to emergency preparedness and response during the COVID-19 pandemic and beyond. Res. Soc. Adm. Pharm. 2021, 17, 1967–1977. [Google Scholar] [CrossRef] [PubMed]
- Hannings, A.N.; Duke, L.J.; Logan, L.D.; Upchurch, B.L.; Kearney, J.C.; Darley, A.; Welch, L.H.; Brooks, K.L.; McElhannon, M.B. Patient perceptions of student pharmacist–run mobile influenza vaccination clinics. J. Am. Pharm. Assoc. 2019, 59, 228–231.e1. [Google Scholar] [CrossRef] [PubMed]
- Luli, A.J.; Morello, C.M.; Lorentz, S.M.; Bounthavong, M.; Brandl, K.; Hart, L.A. A Systematic Approach to Providing COVID-19 Vaccinations in the Community by Student Pharmacists. Pharmacy 2022, 10, 93. [Google Scholar] [CrossRef] [PubMed]
- Nagy, D.K.; Hall, J.J.; Charrois, T.L. The impact of the COVID-19 pandemic on pharmacy students’ personal and professional learning. Curr. Pharm. Teach. Learn. 2021, 13, 1312–1318. [Google Scholar] [CrossRef] [PubMed]
- Diec, S.; Patel, P.H.; Samuel, N.G.; Hernandez-Munoz, J.J. Student perceptions of non-technical skills development during advanced pharmacy practice experiences. Curr. Pharm. Teach. Learn. 2021, 13, 1510–1516. [Google Scholar] [CrossRef]
- Dy-Boarman, E.A.; Ulrich, E. Implementation and evaluation of a practice transformation advanced pharmacy practice experience. Curr. Pharm. Teach. Learn. 2022, 14, 758–764. [Google Scholar] [CrossRef]
| Class of 2019 n = 249 Mean (SD) | Class of 2021 n = 250 Mean (SD) | p-Value | |
|---|---|---|---|
| PSS | 17.3 (6.37) | 18.5 (6.73) | 0.036 |
| Class of 2019 n = 248 Mean (SD) | Class of 2021 n = 246 Mean (SD) | p-Value | |
|---|---|---|---|
| Brief COPE Subscales | |||
| Problem-Focused | 22.0 (5.16) | 21.7 (4.89) | 0.484 |
| Emotion-Focused | 27.4 (5.82) | 28.0 (6.11) | 0.270 |
| Avoidant Coping | 13.0 (2.97) | 13.7 (3.54) | 0.017 |
| Class of 2019 n = 248 | Class of 2021 n = 246 | p-Value | |
|---|---|---|---|
| Academic and Professional Development Skills | |||
| Problem-Solving Skills | 243.31 | 251.72 | 0.466 |
| Time Management Skills | 247.43 | 247.57 | 0.991 |
| Study Skills | 251.79 | 243.18 | 0.476 |
| Class of 2019 | Class of 2021 | |||||
|---|---|---|---|---|---|---|
| P3 n = 145 | P4 n = 103 | p-Value | P3 n = 127 | P4 n = 119 | p-Value | |
| Confidence Level for APPE Practice Readiness | ||||||
| Being an effective member of a patient care team | 117.30 | 134.64 | 0.048 | 104.02 | 144.29 | <0.001 |
| Being an excellent practicing pharmacist | 118.98 | 132.27 | 0.132 | 111.67 | 136.13 | 0.005 |
| Leadership skills | 121.29 | 129.02 | 0.378 | 115.12 | 132.44 | 0.044 |
| Scientific investigation skills | 121.11 | 129.27 | 0.361 | 111.91 | 135.87 | 0.006 |
| Life-long learning skills | 123.10 | 126.48 | 0.698 | 113.71 | 133.95 | 0.019 |
| Class of 2019 n = 249 c | Class of 2021 n = 250 d | |||
|---|---|---|---|---|
| r-Value f | p-Value | r-Value f | p-Value | |
| Academic and Professional Development Skills e | ||||
| Problem-Solving Skills | −0.204 | 0.001 | −0.205 | 0.001 |
| Time Management Skills | −0.368 | <0.001 | −0.178 | 0.005 |
| Study Skills | −0.241 | <0.001 | −0.228 | <0.001 |
| Confidence Level g for APPE Practice Readiness | ||||
| Being an effective member of a patient care team | −0.255 | <0.001 | −0.232 | <0.001 |
| Being an excellent practicing pharmacist | −0.234 | <0.001 | −0.209 | <0.001 |
| Leadership skills | −0.195 | 0.002 | −0.124 | 0.052 |
| Scientific investigation skills | −0.229 | <0.001 | −0.150 | 0.019 |
| Life-long learning skills | −0.256 | <0.001 | −0.230 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cat, T.B.; El-Ibiary, S.Y.; Lee, K.C. Student Stress, Coping, and APPE Readiness at Two Public Institutions before and during the Pandemic. Pharmacy 2024, 12, 121. https://doi.org/10.3390/pharmacy12040121
Cat TB, El-Ibiary SY, Lee KC. Student Stress, Coping, and APPE Readiness at Two Public Institutions before and during the Pandemic. Pharmacy. 2024; 12(4):121. https://doi.org/10.3390/pharmacy12040121
Chicago/Turabian StyleCat, Tram B., Shareen Y. El-Ibiary, and Kelly C. Lee. 2024. "Student Stress, Coping, and APPE Readiness at Two Public Institutions before and during the Pandemic" Pharmacy 12, no. 4: 121. https://doi.org/10.3390/pharmacy12040121
APA StyleCat, T. B., El-Ibiary, S. Y., & Lee, K. C. (2024). Student Stress, Coping, and APPE Readiness at Two Public Institutions before and during the Pandemic. Pharmacy, 12(4), 121. https://doi.org/10.3390/pharmacy12040121






