Pharmacists’ Mental Health during the First Two Years of the Pandemic: A Socio-Ecological Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
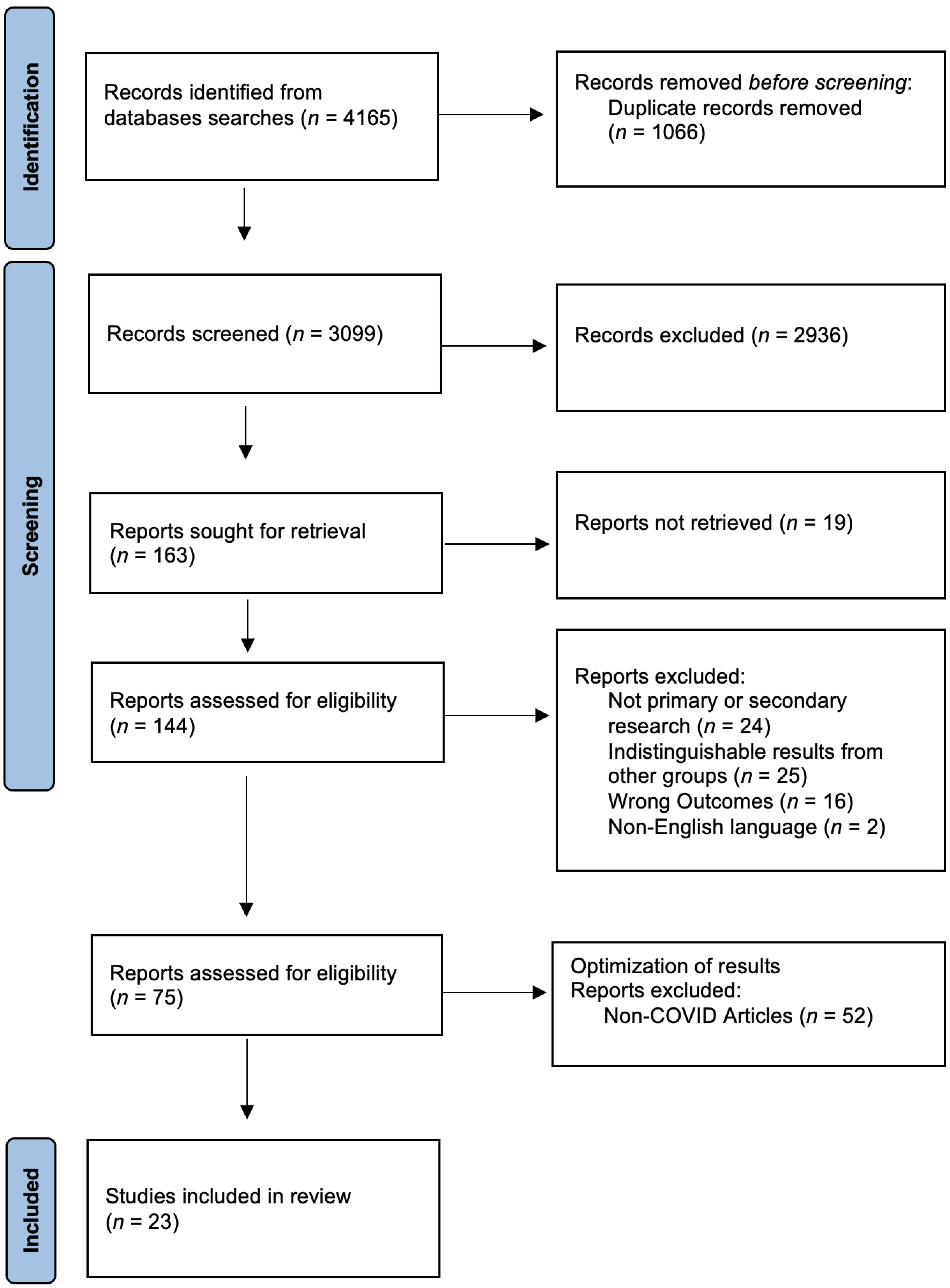
2.2. Screening, Study Selection, and Data Charting
3. Results
3.1. Mental Health and Antecedents
3.1.1. Individual Level
3.1.2. Interpersonal Level
3.1.3. Organizational Level
3.1.4. Community Level
3.1.5. Policy Level
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Nowrouzi-Kia, B.; Sithamparanathan, G.; Nadesar, N.; Gohar, B.; Ott, M. Factors associated with work performance and mental health of healthcare workers during pandemics: A systematic review and meta-analysis. J. Public Health 2021, 44, 731–739. [Google Scholar] [CrossRef]
- Meyerson, B.E.; Ryder, P.T.; Richey-Smith, C. Achieving Pharmacy-Based Public Health: A Call for Public Health Engagement. Public Health Rep. 2013, 128, 140–143. [Google Scholar] [CrossRef]
- Almalki, A.H.; Alzahrani, M.S.; Alshehri, F.S.; Alharbi, A.; Alkhudaydi, S.F.; Alshahrani, R.S.; Alzaidi, A.H.; Algarni, M.A.; Alsaab, H.O.; Alatawi, Y.; et al. The Psychological Impact of COVID-19 on Healthcare Workers in Saudi Arabia: A Year Later Into the Pandemic. Front. Psychiatry 2021, 12, 797545. [Google Scholar] [CrossRef] [PubMed]
- Balayssac, D.; Pereira, B.; Virot, J.; Collin, A.; Alapini, D.; Cuny, D.; Gagnaire, J.-M.; Authier, N.; Vennat, B. Burnout, associated comorbidities and coping strategies in French community pharmacies—BOP study: A nationwide cross-sectional study. PLoS ONE 2017, 12, e0182956. [Google Scholar] [CrossRef]
- Ball, A.M.; Schultheis, J.; Lee, H.-J.; Bush, P.W. Evidence of burnout in critical care pharmacists. Am. J. Health-Syst. Pharm. 2020, 77, 790–796. [Google Scholar] [CrossRef]
- Patel, S.K.; Kelm, M.J.; Bush, P.W.; Lee, H.-J.; Ball, A.M. Prevalence and risk factors of burnout in community pharmacists. J. Am. Pharm. Assoc. 2021, 61, 145–150. [Google Scholar] [CrossRef]
- Durham, M.E.; Bush, P.W.; Ball, A.M. Evidence of burnout in health-system pharmacists. Am. J. Health-Syst. Pharm. 2018, 75, S93–S100. [Google Scholar] [CrossRef]
- Jones, G.M.; Roe, N.A.; Louden, L.; Tubbs, C.R. Factors Associated with Burnout among US Hospital Clinical Pharmacy Practitioners: Results of a Nationwide Pilot Survey. Hosp. Pharm. 2017, 52, 742–751. [Google Scholar] [CrossRef] [PubMed]
- Spoorthy, M.S.; Pratapa, S.K.; Mahant, S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J. Psychiatr. 2020, 51, 102119. [Google Scholar] [CrossRef]
- Bronfenbrenner, B. The Ecology of Human Development; Harvard University Press: Cambridge, UK, 1979. [Google Scholar]
- Ingram, M.; Wolf, A.M.A.; López-Gálvez, N.I.; Griffin, S.C.; Beamer, P.I. Proposing a social ecological approach to address disparities in occupational exposures and health for low-wage and minority workers employed in small businesses. J. Expo. Sci. Environ. Epidemiol. 2021, 31, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Government of Canada. About Mental Health 2022. Available online: https://www.canada.ca/en/public-health/services/about-mental-health.html (accessed on 9 July 2022).
- Lan, Y.; Huang, W.; Kao, C.; Wang, H. The relationship between organizational climate, job stress, workplace burnout, and retention of pharmacists. J. Occup. Health 2020, 62, e12079. [Google Scholar] [CrossRef]
- Hedima, E.W.; Okoro, R.N.; Yelmis, G.A.; Adam, H. Assessment of the impact of COVID-19 pandemic on the mental health and wellbeing of pharmacists: A nationwide survey. Explor. Res. Clin. Soc. Pharm. 2022, 5, 100109. [Google Scholar] [CrossRef] [PubMed]
- Langran, C.; Mantzourani, E.; Hughes, L.; Hall, K.; Willis, S. “I’m at breaking point”; Exploring pharmacists’ resilience, coping and burnout during the COVID-19 pandemic. Explor. Res. Clin. Soc. Pharm. 2022, 5, 100104. [Google Scholar] [CrossRef] [PubMed]
- Veritas Health Innovation. Covidence Systematic Review Software. Available online: https://www.covidence.org/ (accessed on 1 May 2022).
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- Bakken, B.K.; Winn, A.N. Clinician burnout during the COVID-19 pandemic before vaccine administration. J. Am. Pharm. Assoc. 2021, 61, e71–e77. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.; Ma, X.; Fu, S.; Zhao, J.; Aierken, A.; Teng, L.; Gao, X. COVID-19 Knowledge and Pandemic-Associated Distress Among the Hospital Pharmacist Workforce in China. Disaster Med. Public Health Prep. 2023, 17, e75. [Google Scholar] [CrossRef]
- Hayat, K.; Arshed, M.; Fiaz, I.; Afreen, U.; Khan, F.U.; Khan, T.A.; Kadirhaz, M.; Shukar, S.; Saeed, A.; Gill, M.R.; et al. Impact of COVID-19 on the Mental Health of Healthcare Workers: A Cross-Sectional Study From Pakistan. Front. Public Health 2021, 9, 603602. [Google Scholar] [CrossRef]
- Aljuffali, L.A.; Alshabanah, M.O.; Almalag, H.M. Cross-sectional study to evaluate burnout among pharmacy staff in Saudi Arabia during COVID-19 pandemic. Saudi Pharm. J. 2022, 30, 440–453. [Google Scholar] [CrossRef]
- Alameddine, M.; Bou-Karroum, K.; Hijazi, M.A. A national study on the resilience of community pharmacists in Lebanon: A cross-sectional survey. J. Pharm. Policy Pract. 2022, 15, 8. [Google Scholar] [CrossRef]
- Golbach, A.P.; McCullough, K.B.; Soefje, S.A.; Mara, K.C.; Shanafelt, T.D.; Merten, J.A. Evaluation of Burnout in a National Sample of Hematology-Oncology Pharmacists. JCO Oncol. Pract. 2022, 18, e1278–e1288. [Google Scholar] [CrossRef] [PubMed]
- Jakovljevic, B.; Stojanovic, K.; Nikolic Turnic, T.; Jakovljevic, V.L.J. Burnout of Physicians, Pharmacists and Nurses in the Course of the COVID-19 Pandemic: A Serbian Cross-Sectional Questionnaire Study. Int. J. Environ. Res. Public Health 2021, 18, 8728. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.M.; Clark, J.S.; Mohammad, R.A. Burnout and secondary traumatic stress in health-system pharmacists during the COVID-19 pandemic. Am. J. Health-Syst. Pharm. 2021, 78, 818–824. [Google Scholar] [CrossRef] [PubMed]
- Youssef, D.; Youssef, J.; Hassan, H.; Abou-Abbas, L. Prevalence and risk factors of burnout among Lebanese community pharmacists in the era of COVID-19 pandemic: Results from the first national cross-sectional survey. J. Pharm. Policy Pract. 2021, 14, 111. [Google Scholar] [CrossRef]
- GebreEyesus, F.A.; Tarekegn, T.T.; Amlak, B.T.; Shiferaw, B.Z.; Emeria, M.S.; Geleta, O.T.; Terefe, T.F.; Tadereregew, M.M.; Jimma, M.S.; Degu, F.S.; et al. Levels and predictors of anxiety, depression, and stress during COVID-19 pandemic among frontline healthcare providers in Gurage zonal public hospitals, Southwest Ethiopia, 2020: A multicenter cross-sectional study. PLoS ONE 2021, 16, e0259906. [Google Scholar] [CrossRef] [PubMed]
- Hawari, F.I.; Obeidat, N.A.; Dodin, Y.I.; Albtoosh, A.S.; Manasrah, R.M.; Alaqeel, I.O.; Mansour, A.H. The inevitability of Covid-19 related distress among healthcare workers: Findings from a low caseload country under lockdown. PLoS ONE 2021, 16, e0248741. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Cai, J.; Fang, M.; Wang, Y.; Xu, F. Young hospital pharmacists’ job stress and career prospects amidst the COVID-19 pandemic in China. J. Pharm. Policy Pract. 2021, 14, 66. [Google Scholar] [CrossRef]
- Baldonedo-Mosteiro, C.; Franco-Correia, S.; Mosteiro-Diaz, M.-P. Psychological impact of COVID19 on community pharmacists and pharmacy technicians. Explor. Res. Clin. Soc. Pharm. 2022, 5, 100118. [Google Scholar] [CrossRef]
- dos Santos, P.M.; da Silva, C.R.; Costa, D.; Torre, C. Burnout in the Pharmaceutical Activity: The Impact of COVID-19. Front. Psychiatry 2022, 12, 2389. [Google Scholar] [CrossRef]
- Johnston, K.; O’Reilly, C.L.; Scholz, B.; Georgousopoulou, E.N.; Mitchell, I. Burnout and the challenges facing pharmacists during COVID-19: Results of a national survey. Int. J. Clin. Pharm. 2021, 43, 716–725. [Google Scholar] [CrossRef]
- Jovičić-Bata, J.; Pavlović, N.; Milošević, N.; Gavarić, N.; Goločorbin-Kon, S.; Todorović, N.; Lalić-Popović, M. Coping with the burden of the COVID-19 pandemic: A cross-sectional study of community pharmacists from Serbia. BMC Health Serv. Res. 2021, 21, 304. [Google Scholar] [CrossRef]
- Lange, M.; Licaj, I.; Boulouard, M.; Garon, D.; Richard, E.; Le Bas, J.; Salmon, R.; Stroiazzo, R.; Le Bas, F.; Humbert, X. Psychological impact of the COVID-19 outbreak in community pharmacists: A longitudinal study. J. Am. Pharm. Assoc. 2022, 62, 1359–1363. [Google Scholar] [CrossRef] [PubMed]
- Johnston, K.; O’Reilly, C.L.; Scholz, B.; Mitchell, I. The experiences of pharmacists during the global COVID-19 pandemic: A thematic analysis using the jobs demands-resources framework. Res. Soc. Adm. Pharm. 2022, 18, 3649–3655. [Google Scholar] [CrossRef] [PubMed]
- Silva-Suárez, G.; Alvarado Reyes, Y.; Hernandez-Diaz, A.; Rodriguez Ramirez, K.; Colón-Pratts, F.M. The voices of community pharmacists during the COVID-19 pandemic in Puerto Rico. J. Am. Pharm. Assoc. 2022, 62, 202–208.e3. [Google Scholar] [CrossRef]
- Abdelsadig Mohammed, H.; Elamin, S.A.; El-Awaisi, A.; El Hajj, M.S. Use of the job demands-resource model to understand community pharmacists’ burnout during the COVID-19 pandemic. Res. Soc. Adm. Pharm. 2022, 18, 3568–3579. [Google Scholar] [CrossRef]
- Liu, S.; Yang, L.; Zhang, C.; Xu, Y.; Cai, L.; Ma, S.; Wang, Y.; Cai, Z.; Du, H.; Li, R.; et al. Gender differences in mental health problems of healthcare workers during the coronavirus disease 2019 outbreak. J. Psychiatr. Res. 2021, 137, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Guan, Z.; Sun, L.; Zhou, T.; Guan, R. COVID-19 exposure, pandemic-related appraisals, coping strategies, and psychological symptoms among the frontline medical staff and gender differences in coping processes. Appl. Cogn. Psychol. 2022, 36, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Smallwood, N.; Karimi, L.; Bismark, M.; Putland, M.; Johnson, D.; Dharmage, S.C.; Barson, E.; Atkin, N.; Long, C.; Ng, I.; et al. High levels of psychosocial distress among Australian frontline healthcare workers during the COVID-19 pandemic: A cross-sectional survey. Gen. Psychiatr. 2021, 34, e100577. [Google Scholar] [CrossRef]
- Guille, C.; Frank, E.; Zhao, Z.; Kalmbach, D.A.; Nietert, P.J.; Mata, D.; Sen, S. Work-Family Conflict and the Sex Difference in Depression Among Training Physicians. JAMA Intern. Med. 2017, 177, 1766. [Google Scholar] [CrossRef]
- Luo, M.; Guo, L.; Yu, M.; Jiang, W.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef]
- Amanullah, S.; Ramesh Shankar, R. The Impact of COVID-19 on Physician Burnout Globally: A Review. Healthcare 2020, 8, 421. [Google Scholar] [CrossRef] [PubMed]
- Razu, S.R.; Yasmin, T.; Arif, T.B.; Islam, S.; Islam, S.M.S.; Gesesew, H.A.; Ward, P. Challenges Faced by Healthcare Professionals During the COVID-19 Pandemic: A Qualitative Inquiry from Bangladesh. Front. Public Health 2021, 9, 1024. [Google Scholar] [CrossRef] [PubMed]
- Firouzkouhi, M.; Alimohammadi, N.; Kako, M.; Abdollahimohammad, A.; Bagheri, G.; Nouraie, M. Ethical challenges of nurses related COVID-19 pandemic in inpatient wards: An integrative review. Ethics Med. Public Health 2021, 18, 100669. [Google Scholar] [CrossRef] [PubMed]
- Lake, J.D.; Rosenberg-Yunger, Z.R.S.; Dainty, K.N.; Rolf von den Baumen, T.; Everall, A.C.; Guilcher, S.J.T. Understanding perceptions of involving community pharmacy within an integrated care model: A qualitative study. BMC Health Serv. Res. 2020, 20, 396. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Jia, X.; Shi, H.; Niu, J.; Yin, X.; Xie, J.; Wang, X. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 281, 91–98. [Google Scholar] [CrossRef]
- Coccia, M. Pandemic Prevention: Lessons from COVID-19. Encyclopedia 2021, 1, 433–444. [Google Scholar] [CrossRef]
- Gohar, B.; Larivière, M.; Nowrouzi-Kia, B. Sickness absence in healthcare workers during the COVID-19 pandemic. Occup. Med. 2020, 70, 338–342. [Google Scholar] [CrossRef]
- Gohar, B.; Larivière, M.; Lightfoot, N.; Wenghofer, E.; Larivière, C.; Nowrouzi-Kia, B. Meta-analysis of nursing-related organizational and psychosocial predictors of sickness absence. Occup. Med. 2020, 70, 593–601. [Google Scholar] [CrossRef]
| First Author, Year/Origin | Origin | Study Design | Pandemic Period | Pharmacist Setting and Sample Size | Mental Health Outcome(s) Specific to Pharmacists |
|---|---|---|---|---|---|
| Almalki, 2021 [3] | Saudi Arabia | Cross-Sectional | January–March 2021 | Community and hospital; (N = 501) | Anxiety; depression; stress |
| Hedima, 2022 [14] | Nigeria | Cross-sectional | December 2020–February 2021 | Community, hospital, academic, pharmaceutical industry, primary care; (N = 426) | Burnout |
| Langran, 2022 [15] | United Kingdom | Mixed-method (Cross-sectional) | June–July 2020 | Community; hospital; general practice; (N = 199) | Burnout; resilience; well-being |
| Bakken, 2021 [19] | United States | Cross-Sectional | August–September 2020 | Community hospital and health systems; (N = 439) | Burnout; emotional health (including anxiety and depression) |
| Yang, 2021 [20] | China | Cross-sectional | February 2020 | Hospital; (N = 365) | Psychological distress, including anxiety, depression |
| Hayat, 2021 [21] | Pakistan | Cross-sectional | May–June 2020 | General practice (among other groups; pharmacist n = 75) | Anxiety; depression |
| Aljuffali, 2022 [22] | Saudi Arabia | Mixed-Method (Cross-sectional) | June–September 2020 | Community and hospital; (N = 502) | Burnout |
| Alameddine, 2022 [23] | Lebanon | Cross-sectional | December 2020–January 2021 | Community; (N = 459) | Burnout/resilience |
| Golbach, 2021 [24] | United States | Cross-sectional | October–November 2020 | Hematological oncology; (N = 550) | Burnout |
| Jakovljevic, 2021 [25] | Serbia | Cross-sectional | June–December 2020 | General practice (among other groups; pharmacist n = 40) | Burnout |
| Jones, 2021 [26] | United States | Cross-sectional | April–May 2020 | Unspecified; (N = 484) | Burnout; secondary trauma stress |
| Youssef, 2021 [27] | Lebanon | Cross-sectional | February–March 2021 | Community; (N = 387) | Burnout |
| GebreEyesus, 2021 [28] | Ethiopia | Cross-sectional | November 2020 | Unspecified; (among other groups; pharmacist n = 38) | Depression |
| Hawari, 2021 [29] | Jordan | Cross-sectional | April–May 2020 | Community and hospital; (n = 166) | Stress |
| Wu, 2021 [30] | China | Cross-sectional | August–September 2020 | Hospital (among other groups; pharmacist n = 249) | Job Stress |
| Baldonedo-Mosteiro, 2022 [31] | Spain | Cross-sectional | April 2020 | Community (among other groups; pharmacist n = 739) | Stress |
| dos Santos, 2022 [32] | Portugal | Cross-sectional | Unknown | Community; hospital; (N = 1362) | Burnout |
| Johnston, 2021 [33] | Australia | Cross-sectional | April–June 2020 | Community; hospital; (N = 647) | Burnout; survey-based questions |
| Jovičić-Bata et al., 2021 [34] | Serbia | Cross-sectional | April–May 2020 | Community (chains and independent); (N = 392) | Stress; coping with burden |
| Lange, 2022 [35] | France | Cohort | Initial: April 2020; follow-up: September 2020 | Community (initial n = 135; follow-up n = 67) | Burnout; perceived stress; post-traumatic stress |
| Johnston, 2022 [36] | Australia | Qualitative (open text) | April–June 2020 | Community; hospital; (N = 215) | Stressors during the pandemic |
| Silva-Suarez, 2022 [37] | Puerto Rico | Qualitative (Open-text analysis) | May–June 2020 | Community; (N = 233) | Stressors during the pandemic |
| Abdelsadig Mohammed, 2022 [38] | Qatar | Qualitative (focus groups and interviews) | February–April 2021 | Community; (N = 45) | Burnout |
| Levels | Mental Health | Antecedents |
|---|---|---|
| Individual: Risk | Psychological Distress (including anxiety and depression) | History of a mental illness [20] |
| Burnout/resilience | Low resiliency [23]; younger pharmacists [14,15,22,27]; older pharmacists [24]; women [14,15,22,27,31] but men had higher depersonalization [25,33]; less work experience [32]; bachelor’s degree (vs. graduate) [14]; insufficient sleep [27]; lacking confidence [32]; high COVID-19 threat perception [27] | |
| Job Stress | Feeling scared or unsafe [15,36,37] * [31] | |
| Individual: Protective | Burnout | Coping skills [38] * |
| Interpersonal: Risk | Burnout | Single [14,23]; family/marital issues [22] *; having dependents [27]; fulfilling family role [38] *; isolated/lonely [38] * [32]; fear of infecting family members [37,38] * |
| Interpersonal: Protective | Burnout | Working from home [15] *; social support [15,38] * |
| Stress | Low safety concern for family [34] | |
| Organizational: Risk | Burnout | High workload [26,37,38] * [19,26]; increased work hours [22,27]; difficulty connecting with colleagues/poor work culture [22] * [19]; colleague diagnosed with COVID-19 [27]; staff shortage [22,37,38] *; full-time (vs. part-time) [14]; vs. other professions [25]; Community vs. independently owned [34]; unrealistic work expectations [15] *; poor leadership [15] *; inability to reach physicians due to lockdown [38] |
| Psychological Distress (including anxiety and depression) | Poor working conditions [20] | |
| Anxiety | vs. physicians [21] | |
| Job stress | High report of job stress [30]; vs. other professions [29,34]; high workload; supporting others in their role *; completing duties of other roles [36] *; poor leadership [36] *; inadequate training [36] * | |
| Depression | vs. other occupations [28] | |
| Organizational: Protective | Burnout | Peer support [15,38] *; opportunities for professional development [15] * |
| Community: Risk | Burnout | Difficulty connecting with patients [19]; lack of awareness of wellness programs; sense of responsibility to community; |
| Job Stress | Inability to reach physicians due to lockdown [37] *; feeling unappreciated/negative patients [36] * [34] | |
| Community: Protective | Burnout | Technological advances allowed for more patient interactions [15] *; positive shift in patient attitude [15] * |
| Policy: Risk | Stress | Feeling unsupported by government [37] *; receiving unclear communication [36] * |
| Policy: Protective | Burnout | Supported by the government [38] * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ishaky, L.; Sivanthan, M.; Tadrous, M.; Nowrouzi-Kia, B.; McCarthy, L.; Papadopoulos, A.; Gohar, B. Pharmacists’ Mental Health during the First Two Years of the Pandemic: A Socio-Ecological Scoping Review. Pharmacy 2023, 11, 64. https://doi.org/10.3390/pharmacy11020064
Ishaky L, Sivanthan M, Tadrous M, Nowrouzi-Kia B, McCarthy L, Papadopoulos A, Gohar B. Pharmacists’ Mental Health during the First Two Years of the Pandemic: A Socio-Ecological Scoping Review. Pharmacy. 2023; 11(2):64. https://doi.org/10.3390/pharmacy11020064
Chicago/Turabian StyleIshaky, Liam, Myuri Sivanthan, Mina Tadrous, Behdin Nowrouzi-Kia, Lisa McCarthy, Andrew Papadopoulos, and Basem Gohar. 2023. "Pharmacists’ Mental Health during the First Two Years of the Pandemic: A Socio-Ecological Scoping Review" Pharmacy 11, no. 2: 64. https://doi.org/10.3390/pharmacy11020064
APA StyleIshaky, L., Sivanthan, M., Tadrous, M., Nowrouzi-Kia, B., McCarthy, L., Papadopoulos, A., & Gohar, B. (2023). Pharmacists’ Mental Health during the First Two Years of the Pandemic: A Socio-Ecological Scoping Review. Pharmacy, 11(2), 64. https://doi.org/10.3390/pharmacy11020064