Implementation of a Health Risk Assessment into Workflow of the Appointment-Based Model at an Independent Community Pharmacy
Abstract
1. Introduction
2. Materials and Methods
2.1. Development of the Pilot Program
2.2. Project Participants and Data Collection
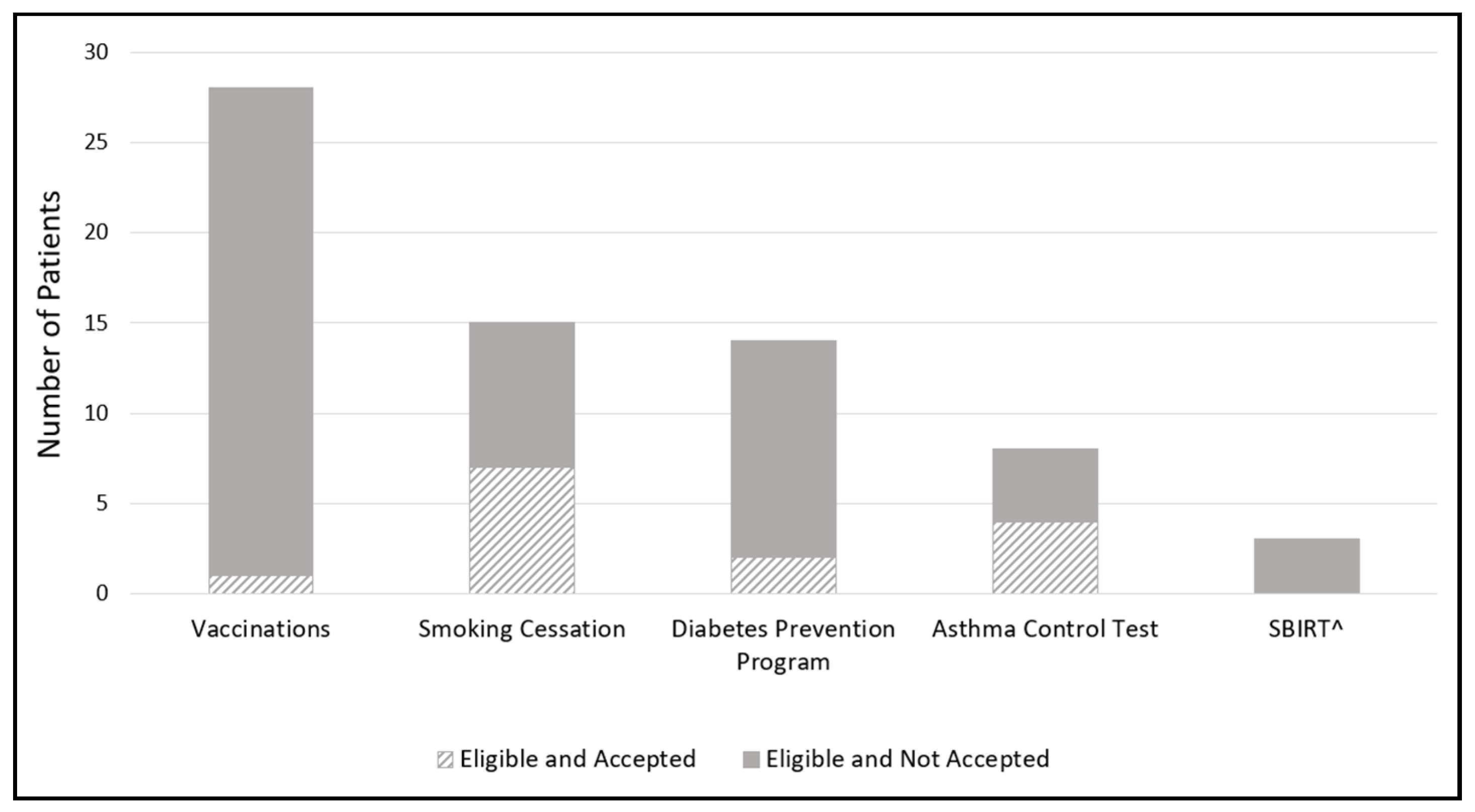
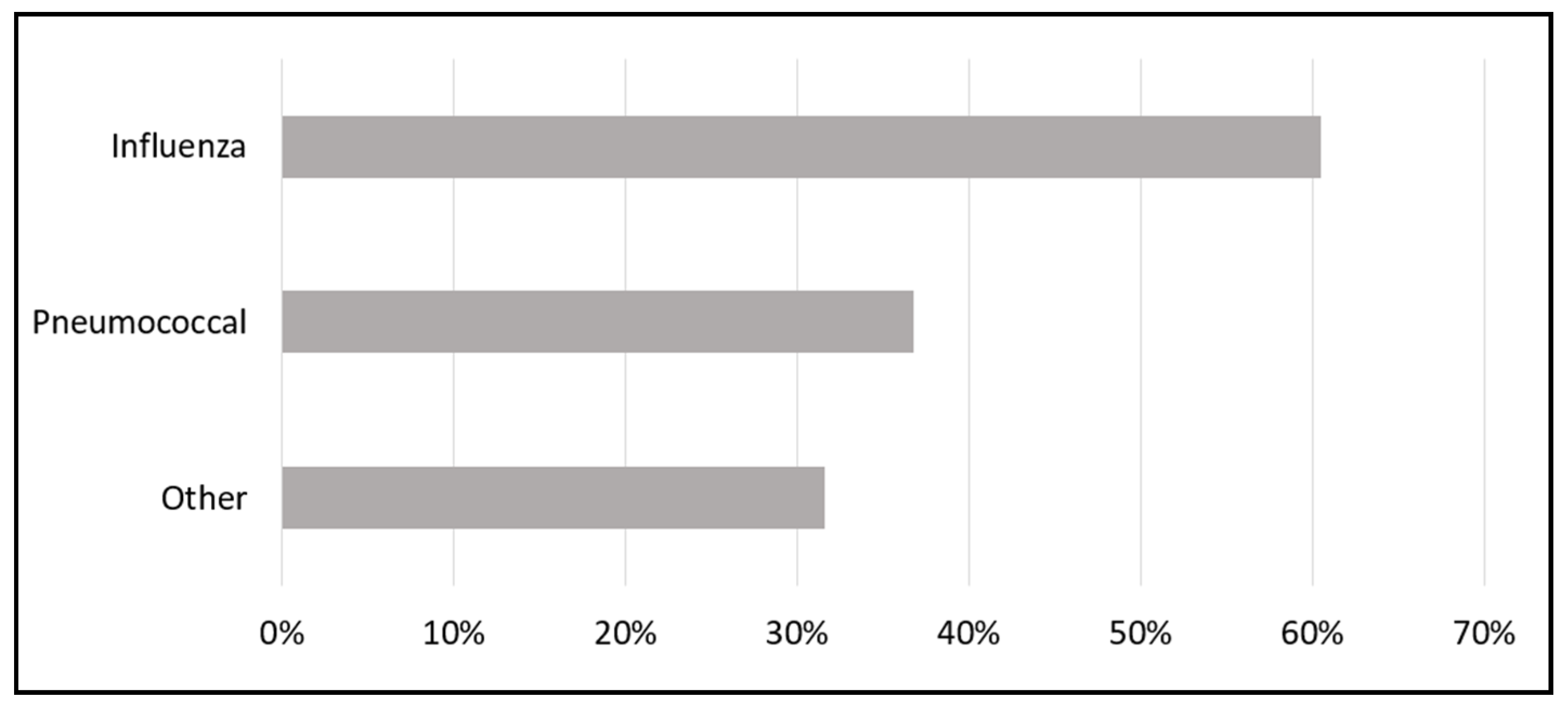
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shekelle, P.G.; Tucker, J.S.; Maglione, M.A.; Morton, S.C.; Roth, E.; Chao, B.; Rhodes, S.; Wu, S.; Newberry, S.J.; Gruman, J.; et al. Health Risk Appraisals and Medicare; Rand Corporation: Santa Monica, CA, USA, 2003; Available online: https://www.rand.org/pubs/reprints/RP1225.html (accessed on 15 September 2022).
- Goetzel, R.Z.; Staley, P.; Ogden, L.; Stange, P.; Fox, J.; Spangler, J.; Tabrizi, M.; Beckowski, M.; Kowlessar, N.; Glasgow, R.E.; et al. A Framework for Patient-Centered Health Risk Assessments—Providing Health Promotion and Disease Prevention Services to Medicare Beneficiaries; Centers for Disease Control and Prevention, US Department of Health and Human Services: Atlanta, GA, USA, 2011. Available online: http://www.cdc.gov/policy/opth/hra/ (accessed on 15 September 2022).
- Anderson, R.T.; Balkrishnan, R.; Camacho, F. Risk classification of Medicare HMO enrollee cost levels using a decision-tree approach. Am. J. Manag. Care 2004, 10 Pt 1, 89–98. [Google Scholar] [PubMed]
- Andelin, J. Kaiser Survey Data Offer More Reasons to Rethink Health Risk Assessments. Am. J. Manag. Care 2018. Available online: https://www.ajmc.com/view/kaiser-survey-data-offer-more-reasons-to-rethink-health-risk-assessments (accessed on 15 September 2022).
- Kelley, A.T.; Goold, S.D.; Ayanian, J.Z.; Patel, M.; Zhang, E.; Beathard, E.; Chang, T.; Solway, E.; Tipirneni, R. Engagement with Health Risk Assessments and Commitment to Healthy Behaviors in Michigan’s Medicaid Expansion Program. J. Gen. Intern. Med. 2020, 35, 514–522. [Google Scholar] [CrossRef] [PubMed]
- Berenbrok, L.A.; Tang, S.; Gabriel, N.; Guo, J.; Sharareh, N.; Patel, N.; Dickson, S.; Hernandez, I. Access to community pharmacies: A nationwide geographic information systems cross-sectional analysis. J. Am. Pharm. Assoc. 2022, 62, 1816–1822.e2. [Google Scholar] [CrossRef] [PubMed]
- Berenbrok, L.A.; Gabriel, N.; Coley, K.C.; Hernandez, I. Evaluation of Frequency of Encounters with Primary Care Physicians vs Visits to Community Pharmacies Among Medicare Beneficiaries. JAMA Netw. Open 2020, 3, e209132. [Google Scholar] [CrossRef] [PubMed]
- Gregory, P.A.; Austin, Z. How do patients develop trust in community pharmacists? Res. Soc. Adm. Pharm. 2021, 17, 911–920. [Google Scholar] [CrossRef] [PubMed]
- Express Scripts Pharmacy. The Prescription of Trust: Pharmacists Transforming Patient Care. 12 January 2022. Available online: https://d17f9hu9hnb3ar.cloudfront.net/s3fs-public/2022-01/The%20Prescription%20of%20Trust-FINAL.pdf (accessed on 20 September 2022).
- Buss, V.H.; Deeks, L.S.; Shield, A.; Kosari, S.; Naunton, M. Analytical quality and effectiveness of point-of-care testing in community pharmacies: A systematic literature review. Res. Soc. Adm. Pharm. 2019, 15, 483–495. [Google Scholar] [CrossRef] [PubMed]
- Kiles, T.M.; Borja-Hart, N.; Wofford, B.R.; Renfro, C.P. Screening for social determinants of health in community pharmacy: Identifying best practices, barriers, and strategies for success. J. Am. Pharm. Assoc. 2021, 61, e59–e63. [Google Scholar] [CrossRef] [PubMed]
- American Pharmacists Association Foundation. Pharmacy’s Appointment-Based Model: A Prescription Synchronization Program that Improves Adherence. APhA Foundation White Paper. 2013. Available online: https://www.aphafoundation.org/sites/default/files/ckeditor/files/ABMWhitePaper-FINAL-20130923(3).pdf (accessed on 20 September 2022).
- Pennsylvania Pharmacists Care Network (PPCN). Available online: http://papharmacistsnetwork.com/ (accessed on 19 September 2022).
- Blanchard, C.; Livet, M.; Ward, C.; Sorge, L.; Sorensen, T.D.; McClurg, M.R. The active implementation frameworks: A roadmap for advancing implementation of comprehensive medication management in primary care. Res. Soc. Adm. Pharm. 2017, 13, 922–929. [Google Scholar] [CrossRef] [PubMed]
- Pharmacist eCare Plan Initiative. Available online: https://www.ecareplaninitiative.com/ (accessed on 30 September 2022).
- Centers for Disease Control and Prevention. National Diabetes Prevention Program: Program Eligibility. Available online: https://www.cdc.gov/diabetes/prevention/program-eligibility.html (accessed on 20 June 2021).
- Asthma Control Test. Available online: https://www.asthmacontroltest.com/welcome/ (accessed on 23 September 2022).
- Substance Abuse and Mental Health Services Administration. Screening, Brief Intervention, and Referral to Treatment (SBIRT). Rockville, MD, USA. Available online: https://www.samhsa.gov/sbirt (accessed on 20 June 2021).
- MCO Performance Metric Dashboard Summary Quarterly Business Review—Q3. 2020. Available online: https://www2.illinois.gov/hfs/SiteCollectionDocuments/MCOPerformanceMetricDashboardSummaryQBRQ32020.pdf (accessed on 25 September 2020).
- Zhang, E.; Tipirneni, R.; Beathard, E.R.; Lee, S.; Kirch, M.A.; Salman, C.; Solway, E.; Clark, S.J.; Haggins, A.N.; Kieffer, E.C.; et al. Health Risk Assessments in Michigan’s Medicaid Expansion: Early Experiences in Primary Care. Am. J. Prev. Med. 2020, 58, e79–e86. [Google Scholar] [CrossRef] [PubMed]
- 2021 NCPA Community Pharmacy Start-Up Benchmarking Report. Available online: https://ncpa.org/sites/default/files/2021-12/2021-ncpa-startup-report.pdf (accessed on 27 September 2022).
- Fitzpatrick, R.M.; Witry, M.J.; Doucette, W.R.; Kent, K.; Deninger, M.J.; Mcdonough, R.P.; Veach, S. Retrospective analysis of drug therapy problems identified with a telephonic appointment-based model of medication synchronization. Pharm. Pract. Granada 2019, 17, 1373. [Google Scholar] [CrossRef] [PubMed]
- Healthy People 2030. Social Determinants of Health. Available online: https://health.gov/healthypeople/objectives-and-data/social-determinants-health (accessed on 24 June 2021).
- Pauling, E.E.; Nguyen, T.T.; Valentino, A.S.; Ducker Coleman, M. Using the Pharmacists’ Patient Care Process to address social determinants of health in patients with diabetes. J. Am. Pharm. Assoc. 2022, 62, 685–692. [Google Scholar] [CrossRef] [PubMed]
- Wilder, M.E.; Kulie, P.; Jensen, C.; Levett, P.; Blanchard, J.; Dominguez, L.W.; Portela, M.; Srivastava, A.; Li, Y.; McCarthy, M.L. The Impact of Social Determinants of Health on Medication Adherence: A Systematic Review and Meta-analysis. J. Gen. Intern. Med. 2021, 36, 1359–1370. [Google Scholar] [CrossRef] [PubMed]
- Curran, G.M.; Shoemaker, S.J. Advancing pharmacy practice through implementation science. Res. Soc. Adm. Pharm. 2017, 13, 889–891. [Google Scholar] [CrossRef] [PubMed]
- Livet, M.; Haines, S.; Curran, G.M.; Seaton, T.L.; Ward, C.S.; Sorensen, T.; McClurg, M.R. Implementation science to advance care delivery: A primer for pharmacists and other health professionals. Pharmacotherapy 2018, 38, 490–502. [Google Scholar] [CrossRef] [PubMed]
- Crespo-Gonzalez, C.; Garcia-Cardenas, V.; Benrimoj, S.I. The next phase in professional services research: From implementation to sustainability. Res. Soc. Adm. Pharm. 2017, 13, 896–901. [Google Scholar] [CrossRef] [PubMed]
- Simundic, A.-M. Bias in research. Biochem. Med. 2013, 23, 12–15. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jackson, E.; McGrath, S.H.; Carroll, J.C.; McGivney, M.S.; Pitzarella, S.; Coley, K.C. Implementation of a Health Risk Assessment into Workflow of the Appointment-Based Model at an Independent Community Pharmacy. Pharmacy 2022, 10, 148. https://doi.org/10.3390/pharmacy10060148
Jackson E, McGrath SH, Carroll JC, McGivney MS, Pitzarella S, Coley KC. Implementation of a Health Risk Assessment into Workflow of the Appointment-Based Model at an Independent Community Pharmacy. Pharmacy. 2022; 10(6):148. https://doi.org/10.3390/pharmacy10060148
Chicago/Turabian StyleJackson, Erica, Stephanie Harriman McGrath, Joni C. Carroll, Melissa Somma McGivney, Samantha Pitzarella, and Kim C. Coley. 2022. "Implementation of a Health Risk Assessment into Workflow of the Appointment-Based Model at an Independent Community Pharmacy" Pharmacy 10, no. 6: 148. https://doi.org/10.3390/pharmacy10060148
APA StyleJackson, E., McGrath, S. H., Carroll, J. C., McGivney, M. S., Pitzarella, S., & Coley, K. C. (2022). Implementation of a Health Risk Assessment into Workflow of the Appointment-Based Model at an Independent Community Pharmacy. Pharmacy, 10(6), 148. https://doi.org/10.3390/pharmacy10060148







