The Impacts of Clinical Pharmacists’ Interventions on Clinical Significance and Cost Avoidance in a Tertiary Care University Hospital in Oman: A Retrospective Analysis
Abstract
1. Introduction
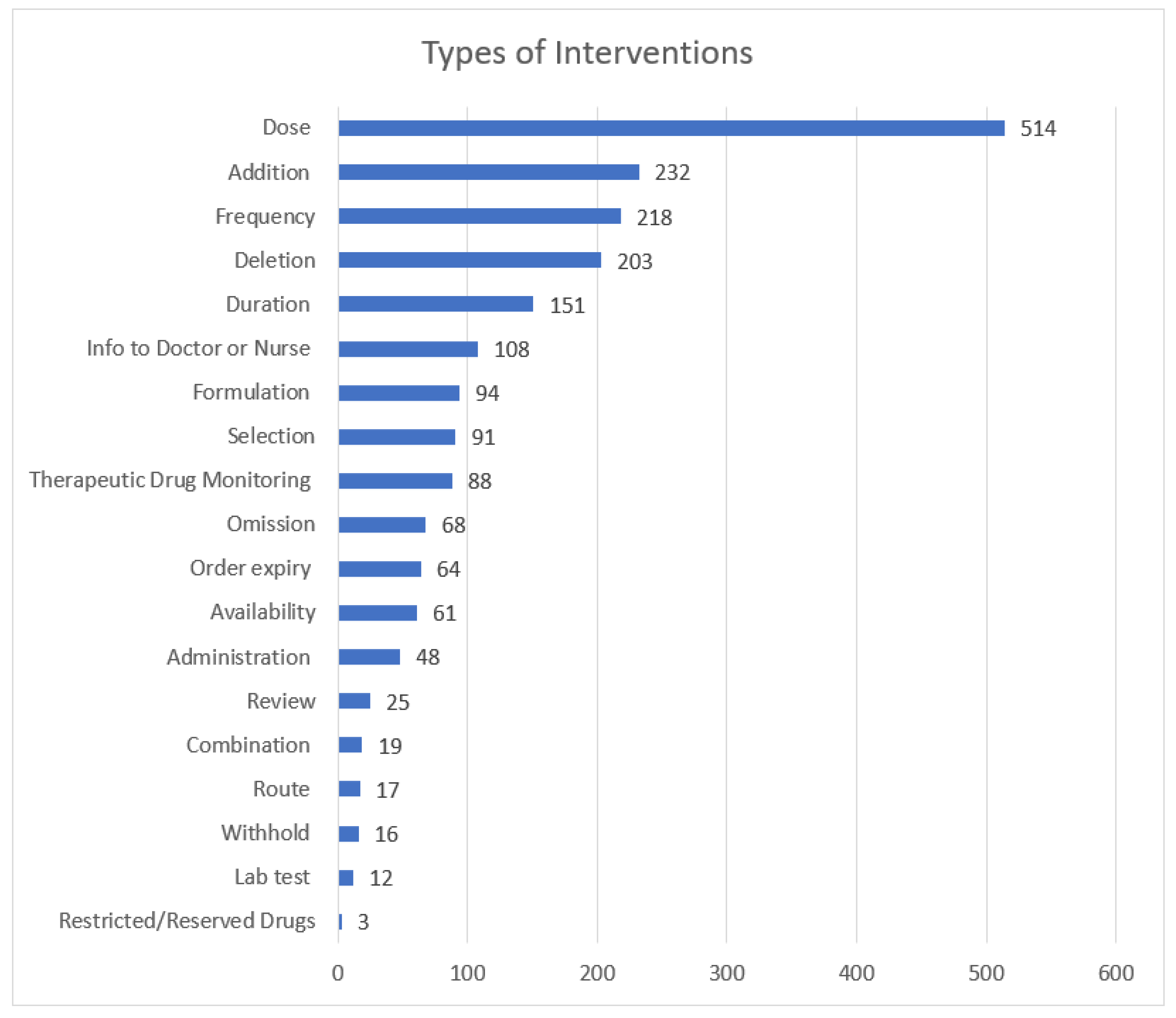
2. Methods
2.1. Study Design and Setting
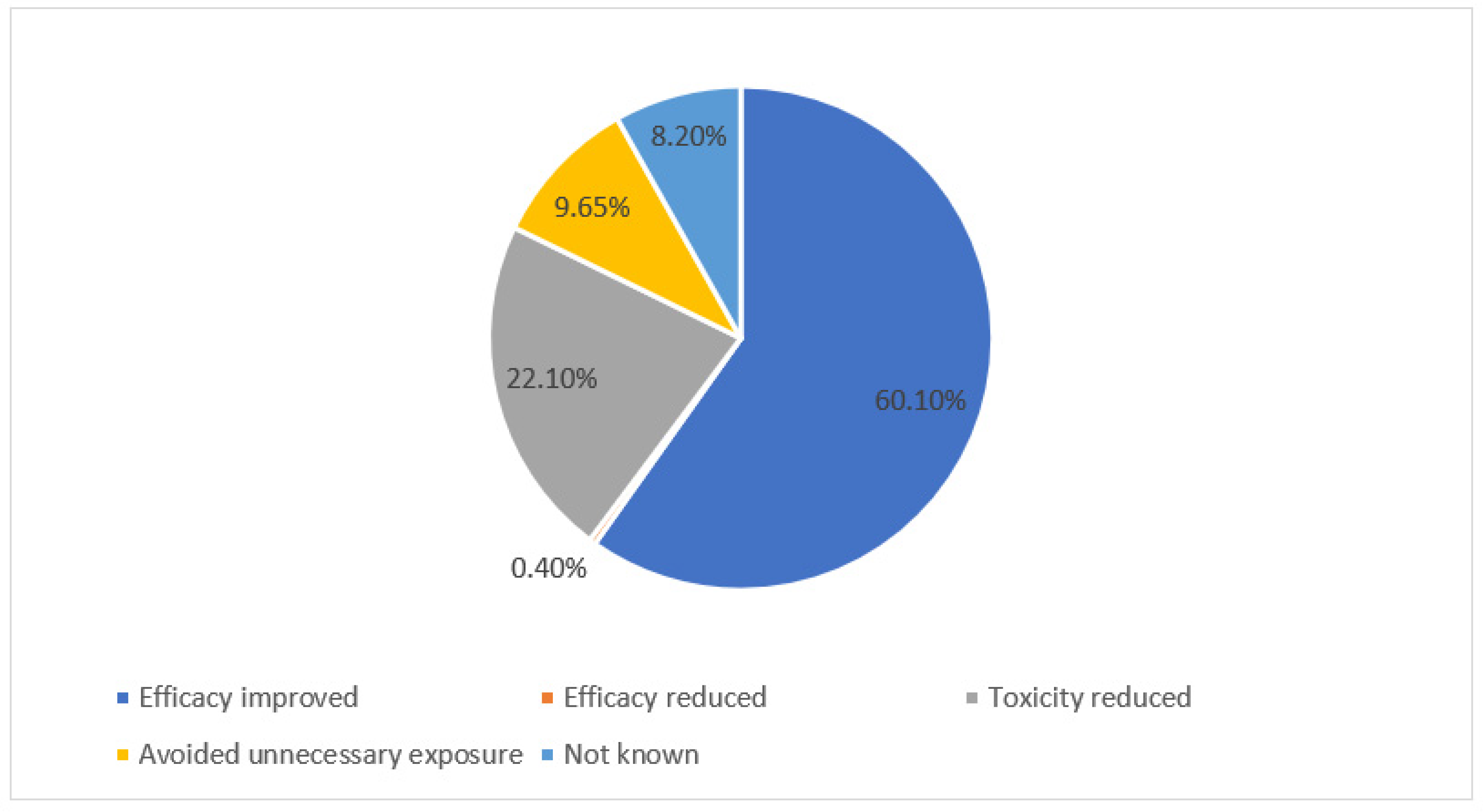
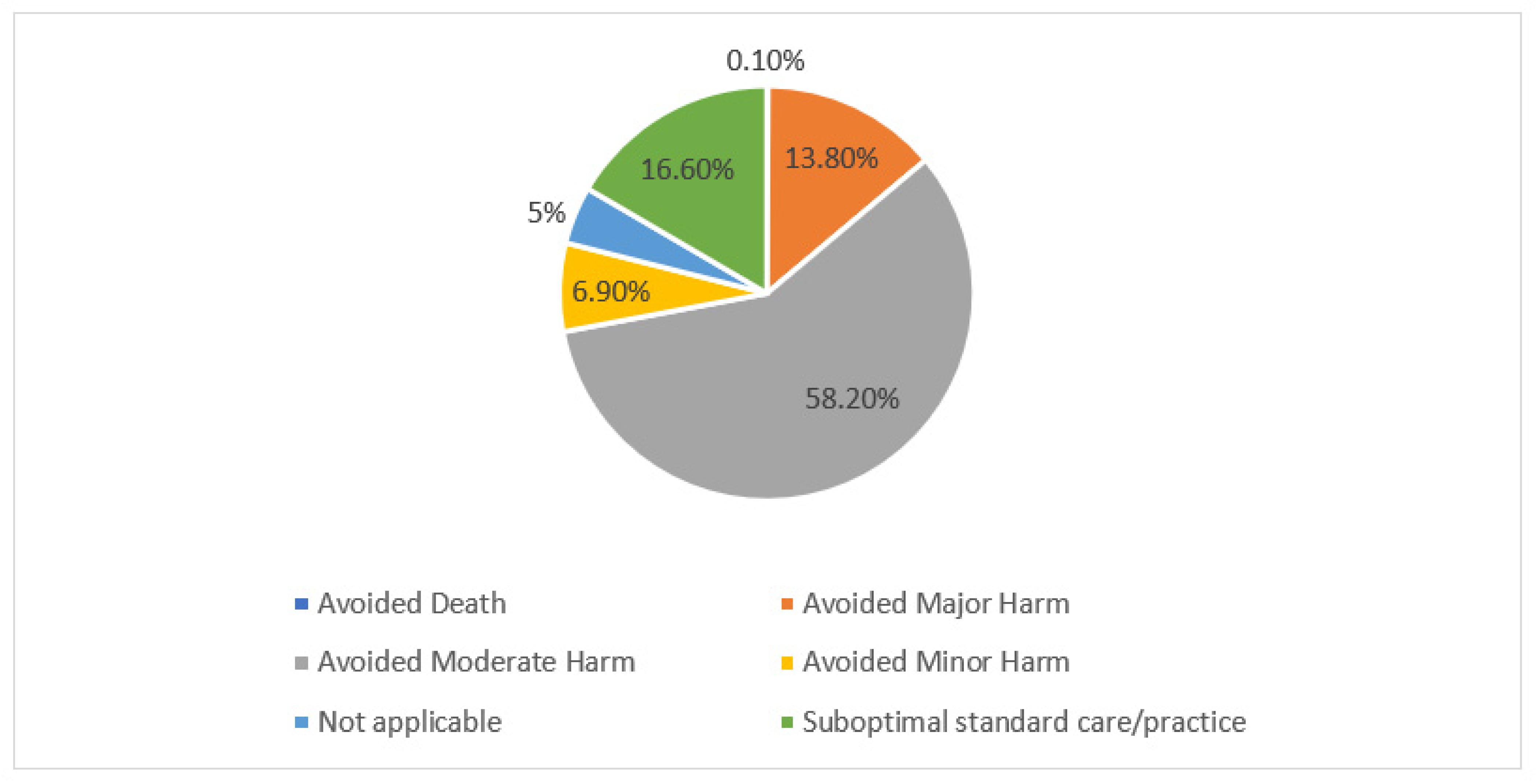
2.2. Study Measures
- The outcome: stratified into accepted, accepted with changes, rejected, or unknown.
- The clinical significance: stratified into efficacy improved, efficacy reduced, toxicity reduced, unnecessary exposure avoided, or not known.
- The grading of the clinical significance: stratified into death or major, moderate, minor, or suboptimal standard of care/practice.
2.3. Presumed Cost Avoidance Calculation
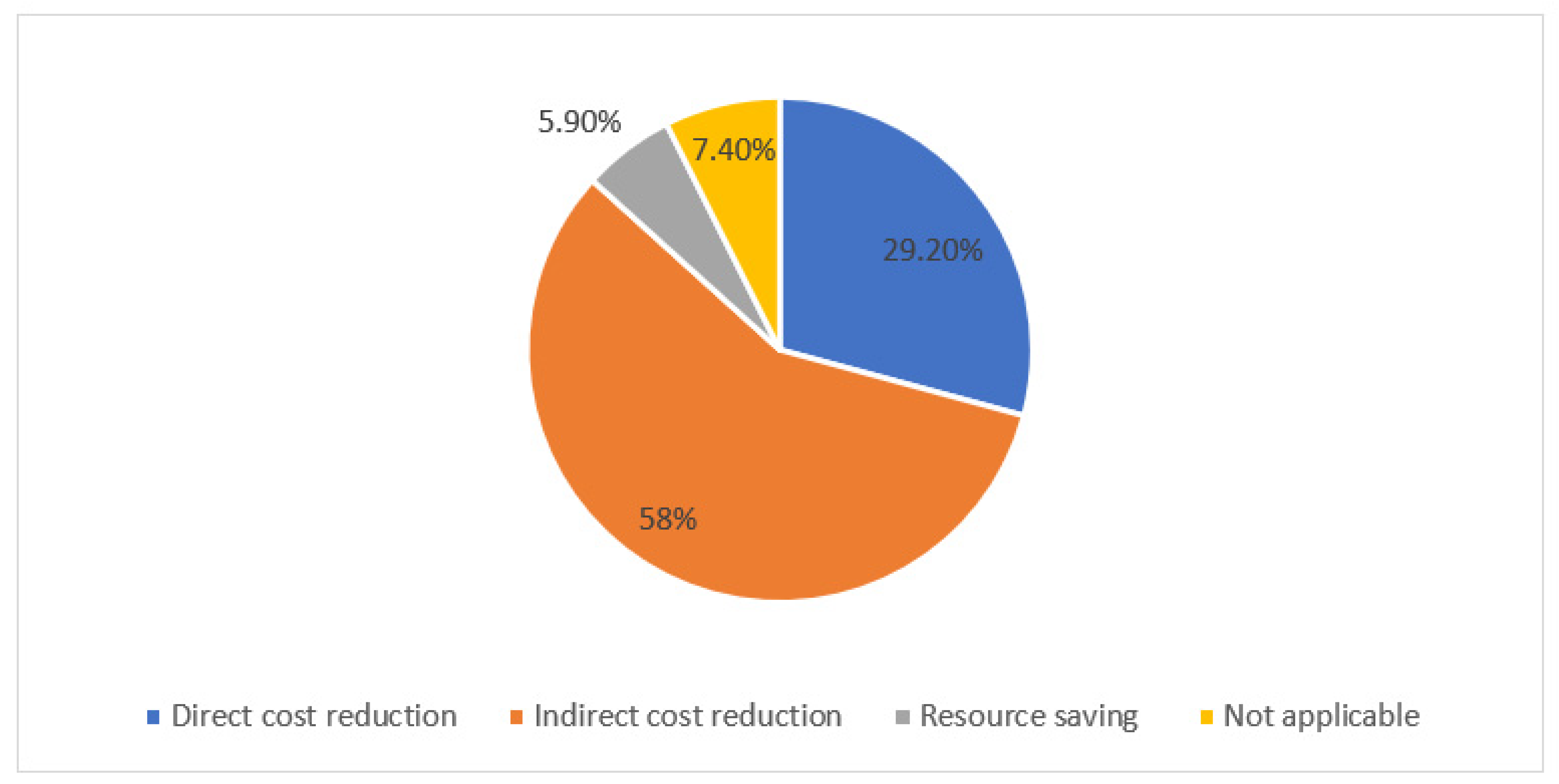
- Direct drug/investigation cost reduction: include interventions that are directly associated with absolute cost reduction such as discontinuation of unnecessary medicines, switching to less expensive agents, or altering the route of administration.
- In-direct drug/investigation cost reduction: include interventions that are associated with in-direct cost avoidance or reduction in LOS.
- Resource saving: include interventions that are associated with saving nursing, doctor, or pharmacist times or interventions that improve patients’ compliance with medications.
- Not applicable: include interventions that are not impacting the cost but rather are associated with better care/practice.
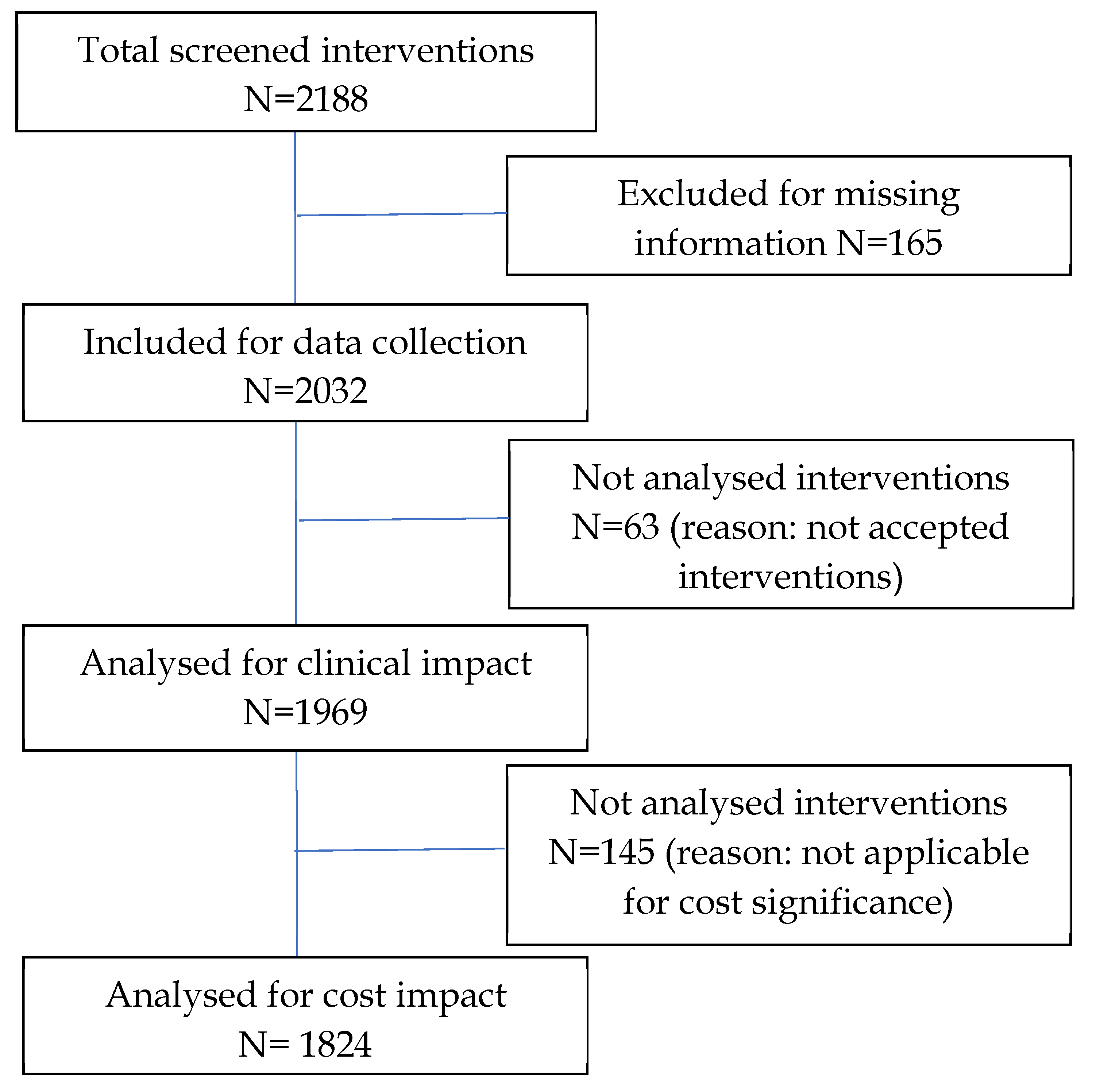
2.4. Inclusion and Exclusion Criteria for Analyses of Clinical and Cost Impacts
2.5. Statistical Analysis
2.6. Ethics Approval
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Al Salmi, Z. Clinical Audit of Pharmaceutical Care provided by a Clinical Pharmacist in Cardiology and Infectious Disease in-patients at the Royal Hospital, Muscat/Oman. Oman Med. J. 2009, 24, 89–94. [Google Scholar] [PubMed]
- Anderson, S.V.; Schumock, G.T. Evaluation and justification of clinical pharmacy services. Expert Rev. Pharmacoecon. Outcomes Res. 2009, 9, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Benavides, S.; Rodriguez, J.C.; Maniscalco-Feichtl, M. Pharmacist involvement in improving asthma outcomes in various healthcare settings: 1997 to present. Ann. Pharmacother. 2009, 43, 85–97. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.R.; Nelson, L.A.; Elliott, E.; Hieber, R.; Sommi, R.W. Analysis of cost avoidance from pharmacy students’ clinical interventions at a psychiatric hospital. Am. J. Pharm. Educ. 2011, 75, 8. [Google Scholar] [CrossRef]
- Chiatti, C.; Bustacchini, S.; Furneri, G.; Mantovani, L.; Cristiani, M.; Misuraca, C.; Lattanzio, F. The economic burden of inappropriate drug prescribing, lack of adherence and compliance, adverse drug events in older people: A systematic review. Drug Saf. 2012, 35 (Suppl. 1), 73–87. [Google Scholar] [CrossRef]
- Gallagher, C.T.; Hickman, A.C.; Hannbeck, L.; Flynn, R.W. Analysis of enquiries to the National Pharmacy Association following major changes to controlled drug legislation in the UK. Int. J. Pharm. Pract. 2012, 20, 50–56. [Google Scholar] [CrossRef]
- Gallagher, J.; Byrne, S.; Woods, N.; Lynch, D.; McCarthy, S. Cost-outcome description of clinical pharmacist interventions in a university teaching hospital. BMC Health Serv. Res. 2014, 14, 177. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, J.; McCarthy, S.; Byrne, S. Economic evaluations of clinical pharmacist interventions on hospital inpatients: A systematic review of recent literature. Int. J. Clin. Pharm. 2014, 36, 1101–1114. [Google Scholar] [CrossRef] [PubMed]
- Jourdan, J.P.; Muzard, A.; Goyer, I.; Ollivier, Y.; Oulkhouir, Y.; Henri, P.; Parienti, J.J.; Breuil, C. Impact of pharmacist interventions on clinical outcome and cost avoidance in a university teaching hospital. Int. J. Clin. Pharm. 2018, 40, 1474–1481. [Google Scholar] [CrossRef]
- Khalili, H.; Karimzadeh, I.; Mirzabeigi, P.; Dashti-Khavidaki, S. Evaluation of clinical pharmacist’s interventions in an infectious diseases ward and impact on patient’s direct medication cost. Eur. J. Intern. Med. 2013, 24, 227–233. [Google Scholar] [CrossRef]
- Kilcup, M.; Schultz, D.; Carlson, J.; Wilson, B. Postdischarge pharmacist medication reconciliation: Impact on readmission rates and financial savings. J. Am. Pharm. Assoc. 2013, 53, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Kopp, B.J.; Mrsan, M.; Erstad, B.L.; Duby, J.J. Cost implications of and potential adverse events prevented by interventions of a critical care pharmacist. Am. J. Health Syst. Pharm. 2007, 64, 2483–2487. [Google Scholar] [CrossRef]
- Kuo, G.M.; Touchette, D.R.; Marinac, J.S. Drug errors and related interventions reported by United States clinical pharmacists: The American College of Clinical Pharmacy practice-based research network medication error detection, amelioration and prevention study. Pharmacotherapy 2013, 33, 253–265. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Kang, J.E.; Park, S.H.; Jin, H.K.; Jang, S.M.; Kim, S.A.; Rhie, S.J. Nutrition and Clinical Outcomes of Nutrition Support in Multidisciplinary Team for Critically Ill Patients. Nutr. Clin. Pract. 2018, 33, 633–639. [Google Scholar] [CrossRef]
- Mair, A.; Wilson, M.; Dreischulte, T. Addressing the Challenge of Polypharmacy. Annu Rev. Pharmacol. Toxicol. 2020, 60, 661–681. [Google Scholar] [CrossRef]
- Qin, S.B.; Zhang, X.Y.; Fu, Y.; Nie, X.Y.; Liu, J.; Shi, L.W.; Cui, Y.M. The impact of the clinical pharmacist-led interventions in China: A systematic review and Meta-Analysis. Int. J. Clin. Pharm. 2020, 42, 366–377. [Google Scholar] [CrossRef] [PubMed]
- Ronan, S.; Shannon, N.; Cooke, K.; McKeon, T.; Walsh, E.K.; Kearney, A.; Sahm, L.J. The Role of the Clinical Pharmacist in an Irish University Teaching Hospital: A Mixed-Methods Study. Pharmacy 2020, 8, 14. [Google Scholar] [CrossRef]
- Saberi, P.; Dong, B.J.; Johnson, M.O.; Greenblatt, R.M.; Cocohoba, J.M. The impact of HIV clinical pharmacists on HIV treatment outcomes: A systematic review. Patient Prefer. Adherence 2012, 6, 297–322. [Google Scholar] [CrossRef]
- Salman, B.; Al-Hashar, A.; Al-Khirbash, A.; Al-Zakwani, I. Clinical and Cost Implications of Clinical Pharmacist Interventions on Antimicrobial Use at Sultan Qaboos University Hospital in Oman. Int. J. Infect. Dis. 2021, 109, 137–141. [Google Scholar] [CrossRef]
- Santschi, V.; Chiolero, A.; Burnand, B.; Colosimo, A.L.; Paradis, G. Impact of pharmacist care in the management of cardiovascular disease risk factors: A systematic review and meta-analysis of randomized trials. Arch. Intern. Med. 2011, 171, 1441–1453. [Google Scholar] [CrossRef]
- Scott, I.A.; Hilmer, S.N.; Reeve, E.; Potter, K.; Le Couteur, D.; Rigby, D.; Gnjidic, D.; Del Mar, C.B.; Roughead, E.E.; Page, A.; et al. Reducing inappropriate polypharmacy: The process of deprescribing. JAMA Intern. Med. 2015, 175, 827–834. [Google Scholar] [CrossRef] [PubMed]
- Shull, M.T.; Braitman, L.E.; Stites, S.D.; DeLuca, A.; Hauser, D. Effects of a pharmacist-driven intervention program on hospital readmissions. Am. J. Health Syst. Pharm. 2018, 75, e221–e230. [Google Scholar] [CrossRef] [PubMed]
- Viktil, K.K.; Blix, H.S. The impact of clinical pharmacists on drug-related problems and clinical outcomes. Basic Clin. Pharmacol. Toxicol. 2008, 102, 275–280. [Google Scholar] [CrossRef]
- Vo, H.T.; Charpiat, B.; Chanoine, S.; Juste, M.; Roubille, R.; Rose, F.X.; Conort, O.; Allenet, B.; Bedouch, P. CLEO: A multidimensional tool to assess clinical, economic and organisational impacts of pharmacists’ interventions. Eur. J. Hosp. Pharm. 2021, 28, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Walsh, E.K.; Hansen, C.R.; Sahm, L.J.; Kearney, P.M.; Doherty, E.; Bradley, C.P. Economic impact of medication error: A systematic review. Pharmacoepidemiol. Drug Saf. 2017, 26, 481–497. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Qian, X.; Zhang, L.; Hu, L.; Fan, L.; Wang, Q.; Lan, B.; Sheng, C.; Li, L.; Zheng, W.; et al. Evaluation of the Effectiveness of Clinical Pharmacists’ Consultation in the Treatment of Infectious Diseases: A Single-Arm, Prospective Cohort Study. Front. Pharmacol. 2019, 10, 187. [Google Scholar] [CrossRef]
| Intervention Type according to the Paper (Campbell) | Intervention Type according to (SQUH) | Cost per Intervention of Respective Type ($) |
|---|---|---|
| Addition | Addition, order expiry, or extended duration | 62.81 |
| Change medication | Selection or availability: A change of formulary item to another formulary item due to non-availability. | 61.75 |
| Discontinuation of a medication | Deletion (includes double order) or reduced duration | 50.39 |
| Dosage form change | Formulation, IV-oral, or route | 54.33 |
| Dose adjustment | Dose or frequency | 61.72 |
| Drug information | Information to doctor or nurse, administration (includes timing) | 24.64 |
| Medication reconciliation | Withhold or re-start (includes omission) | 27.58 |
| Monitoring laboratory order | Lab request | 77.92 |
| Non-formulary consultation | Restricted/Revered (specialty consultation regarding a non-formulary/reserved item approval for use) | 47.86 |
| Non-formulary to formulary conversion | Restricted/Revered (a change of non-formulary item to formulary item without a specialty consultation) or availability (A change of non-formulary item to formulary/or non- formulary due to non-availability) | 36.73 |
| Pharmacokinetic monitoring—level adjustment | TDM request, TDM follow up, or TDM dose | 77.45 |
| Prevention of adverse drug event | Combination (includes contraindication, interaction, combination of meds, or therapeutic duplication) | 470.99 |
| Prompted medical follow-up | Review (includes referral) | 56.58 |
| Class of the Involved Drug | Number of Interventions | (%) |
|---|---|---|
| Antimicrobial | 610 | 30.1 |
| Cardiovascular system (including anticoagulants) | 371 | 18.3 |
| Nutrition & Metabolic disorders | 215 | 10.6 |
| Endocrine system | 210 | 10.3 |
| Gastrointestinal system | 149 | 7.3 |
| Nervous system | 123 | 6.0 |
| Respiratory system | 77 | 3.7 |
| Analgesia (including opioids) | 66 | 3.2 |
| Blood disorders and Immunoglobulins | 60 | 2.9 |
| Cytotoxic drugs/Immunosuppressants | 47 | 2.3 |
| Genito-urinary system | 20 | 1.0 |
| Skin preparation | 17 | 0.8 |
| Vaccine | 16 | 0.8 |
| Musculoskeletal system | 12 | 0.6 |
| Ear, eye, nose & oropharynx | 19 | 0.9 |
| Anesthesia | 3 | 0.1 |
| Type of Intervention according to Campbell * | Frequency over the Study Period (3 Months) | Total Presumed Cost Avoidance during the Study Period ($) (3 Months) | Potential Annual Cost Avoidance ($) |
|---|---|---|---|
| Addition | 358 | 22,485.98 | 89,943.92 |
| Change medication | 106 | 6545.5 | 26,182 |
| Discontinuation of a medication | 263 | 13,252.57 | 53,010.28 |
| Dosage form change | 81 | 4400.73 | 17,602.92 |
| Dose adjustment | 673 | 41,537.56 | 16,6150.2 |
| Drug information | 127 | 3129.28 | 12,517.12 |
| Medication reconciliation | 81 | 2233.98 | 8935.92 |
| Monitoring laboratory order | 11 | 857.12 | 3428.48 |
| Non-formulary consultation | 3 | 143.58 | 574.32 |
| Non-formulary to formulary conversion | 6 | 220.38 | 881.52 |
| Pharmacokinetic monitoring—level adjustment | 83 | 6428.35 | 25,713.4 |
| Prevention of adverse drug event | 16 | 7535.84 | 30,143.36 |
| Prompted medical follow-up | 17 | 961.86 | 3847.44 |
| Total | 1824 | 109,732.73 | 438,931 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Maqbali, J.S.; Taqi, A.; Al-Ajmi, S.; Al-Hamadani, B.; Al-Hamadani, F.; Bahram, F.; Al-Balushi, K.; Gamal, S.; Al-Lawati, E.; Al Siyabi, B.; et al. The Impacts of Clinical Pharmacists’ Interventions on Clinical Significance and Cost Avoidance in a Tertiary Care University Hospital in Oman: A Retrospective Analysis. Pharmacy 2022, 10, 127. https://doi.org/10.3390/pharmacy10050127
Al-Maqbali JS, Taqi A, Al-Ajmi S, Al-Hamadani B, Al-Hamadani F, Bahram F, Al-Balushi K, Gamal S, Al-Lawati E, Al Siyabi B, et al. The Impacts of Clinical Pharmacists’ Interventions on Clinical Significance and Cost Avoidance in a Tertiary Care University Hospital in Oman: A Retrospective Analysis. Pharmacy. 2022; 10(5):127. https://doi.org/10.3390/pharmacy10050127
Chicago/Turabian StyleAl-Maqbali, Juhaina Salim, Aqila Taqi, Samyia Al-Ajmi, Buthaina Al-Hamadani, Farhat Al-Hamadani, Fatima Bahram, Kifah Al-Balushi, Sarah Gamal, Esra Al-Lawati, Bushra Al Siyabi, and et al. 2022. "The Impacts of Clinical Pharmacists’ Interventions on Clinical Significance and Cost Avoidance in a Tertiary Care University Hospital in Oman: A Retrospective Analysis" Pharmacy 10, no. 5: 127. https://doi.org/10.3390/pharmacy10050127
APA StyleAl-Maqbali, J. S., Taqi, A., Al-Ajmi, S., Al-Hamadani, B., Al-Hamadani, F., Bahram, F., Al-Balushi, K., Gamal, S., Al-Lawati, E., Al Siyabi, B., Al Siyabi, E., Al-Sharji, N., & Al-Zakwani, I. (2022). The Impacts of Clinical Pharmacists’ Interventions on Clinical Significance and Cost Avoidance in a Tertiary Care University Hospital in Oman: A Retrospective Analysis. Pharmacy, 10(5), 127. https://doi.org/10.3390/pharmacy10050127






