Exploring the Effect of Virtual Education on Student Pharmacists’ Confidence toward APPE Readiness
Abstract
:1. Introduction
2. Materials and Methods
2.1. APPE Readiness Survey
2.2. Academic Considerations
3. Results
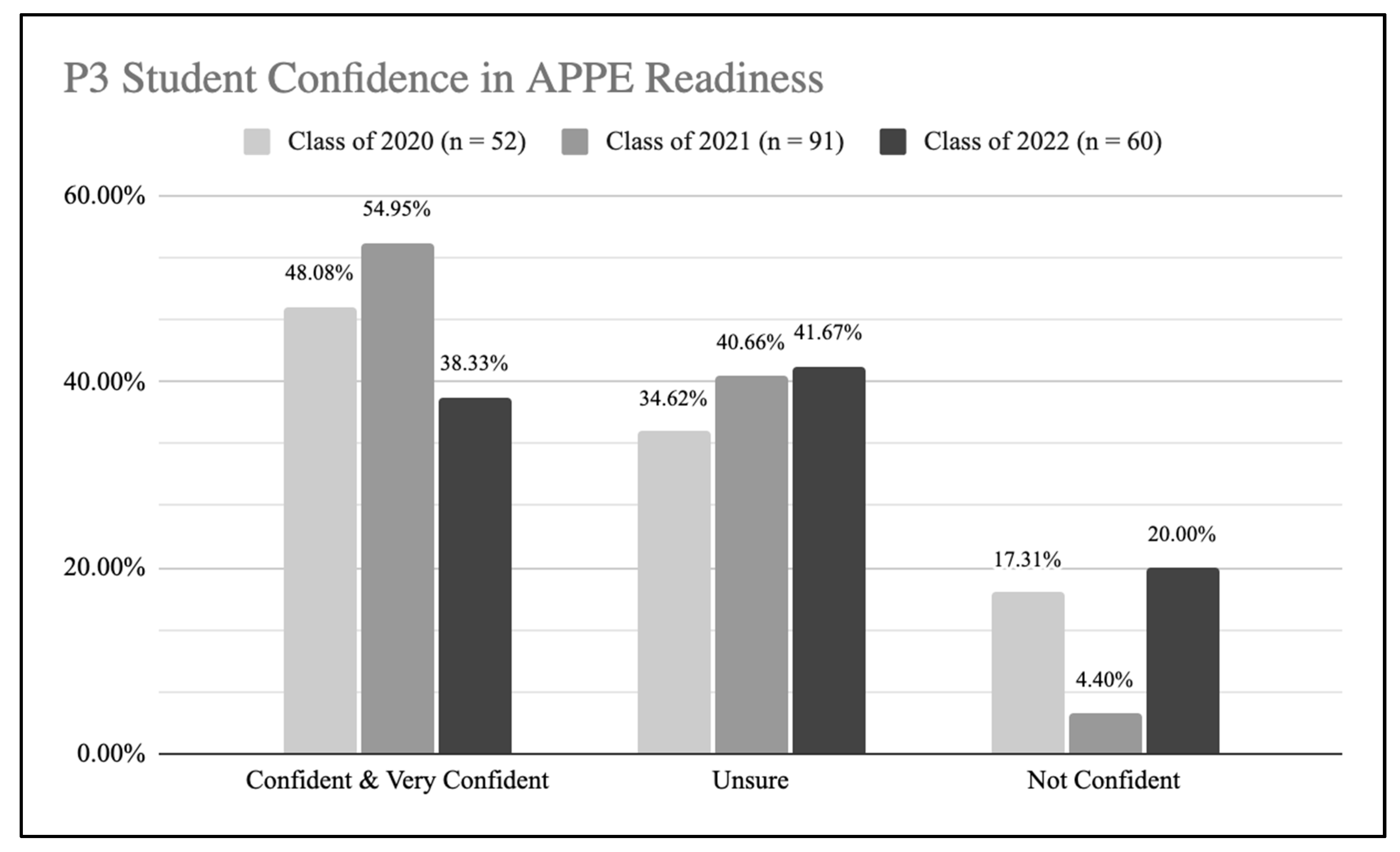
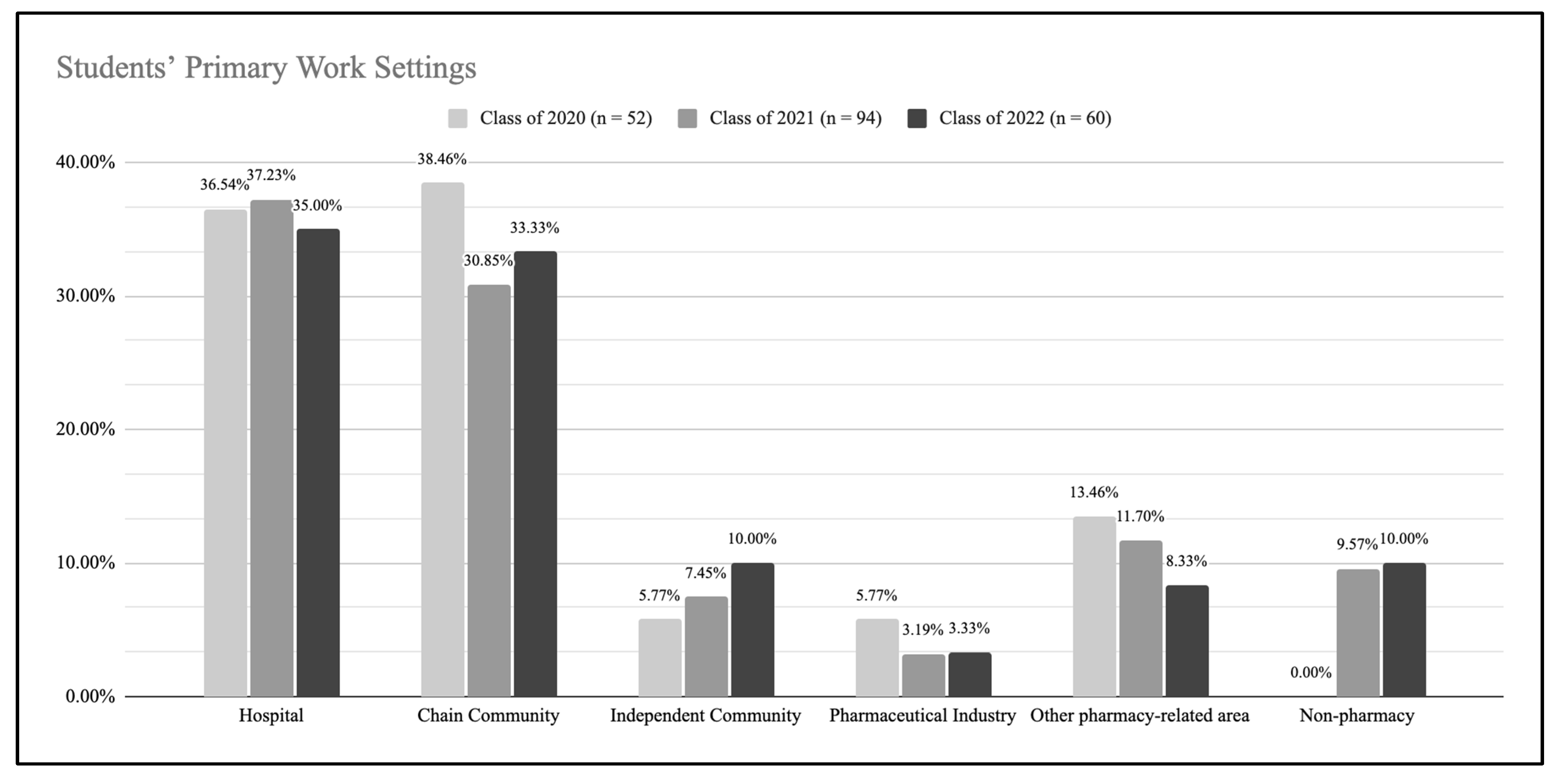
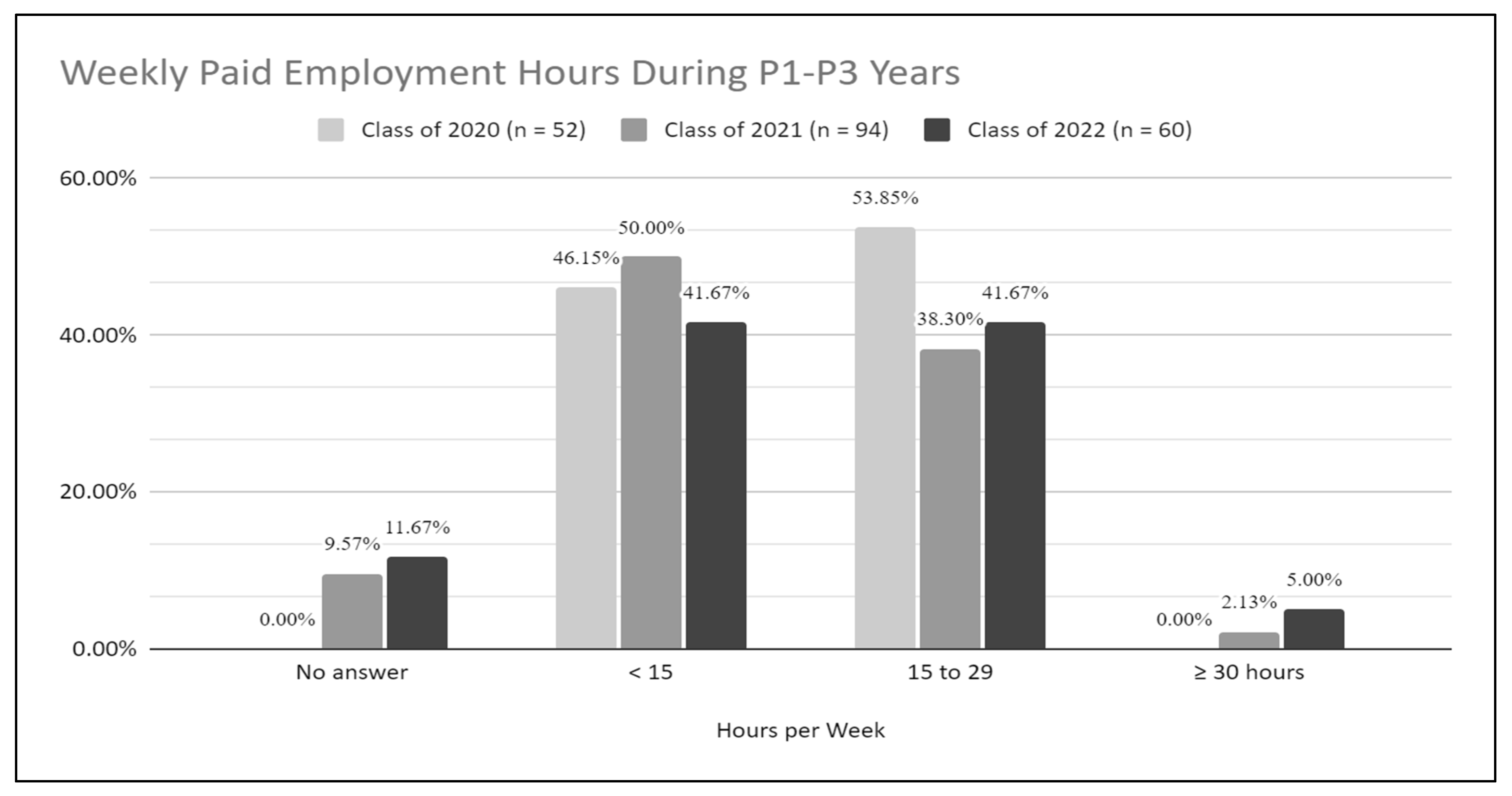
3.1. Survey Results
3.2. Curricular Changes
3.3. Academic Performance
3.4. APPE Evaluations and Performance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Accreditation Council for Pharmacy Education (ACPE). Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree; ACPE: Chicago, IL, USA, 2016. [Google Scholar]
- Smith, C.; Stewart, R.; Smith, G.; Anderson, H.G.; Baggarly, S. Developing and Implementing an Entrustable Professional Activity Assessment for Pharmacy Practice Experiences. Am. J. Pharm. Educ. 2020, 84, ajpe7876. [Google Scholar] [CrossRef] [PubMed]
- Jarrett, J.B.; Berenbrok, L.A.; Goliak, K.L.; Meyer, S.M.; Shaughnessy, A.F. Entrustable Professional Activities as a Novel Framework for Pharmacy Education. Am. J. Pharm. Educ. 2018, 82, 6256. [Google Scholar] [CrossRef] [PubMed]
- Gruenberg, K.; Hsia, S.; O’Brien, B.; O’Sullivan, P. Exploring Multiple Perspectives on Pharmacy Students’ Readiness for Advanced Pharmacy Practice Experiences. Am. J. Pharm. Educ. 2021, 85, 8358. [Google Scholar] [CrossRef] [PubMed]
- Haines, S.T.; Pittenger, A.L.; Stolte, S.K.; Plaza, C.M.; Gleason, B.L.; Kantorovich, A.; McCollum, M.; Trujillo, J.M.; Copeland, D.A.; Lacroix, M.M.; et al. Core Entrustable Professional Activities for New Pharmacy Graduates. Am. J. Pharm. Educ. 2017, 81, S2. [Google Scholar] [CrossRef]
- Porter, A.L.; Barnett, S.G.; Gallimore, C.E. Development of a Holistic Assessment Plan to Evaluate a Four-Semester Laboratory Course Series. Am. J. Pharm. Educ. 2017, 81, 33. [Google Scholar] [CrossRef]
- Nagy, D.K.; Hall, J.J.; Charrois, T.L. The impact of the COVID-19 pandemic on pharmacy students’ personal and professional learning. Curr. Pharm. Teach. Learn. 2021, 13, 1312–1318. [Google Scholar] [CrossRef]
- Alghamdi, S.; Ali, M. Pharmacy Students’ Perceptions and Attitudes towards Online Education during COVID-19 Lockdown in Saudi Arabia. Pharmacy 2021, 9, 169. [Google Scholar] [CrossRef]
- Holmes, M.; Carter, C.; Moye, C.; Omeke, S.; Ikunika, B. The Impact of the COVID-19 Pandemic on Pharmacy Learners’ Academic Health. Pharmacy Times, 15 December 2021. [Google Scholar]
- Fuller, K.A.; Heldenbrand, S.D.; Smith, M.D.; Malcom, D.R. A Paradigm Shift in US Experiential Pharmacy Education Accelerated by the COVID-19 Pandemic. Am. J. Pharm. Educ. 2020, 84, ajpe8149. [Google Scholar] [CrossRef]
- Wu, M.; Brill, D.A.; Shirodkar, M.P.; Tan, J.; Poptani, M.; Wang, Y.; Haworth, I.S. Using technology to automate syllabus construction for programmatic, curricular, faculty, and experiential assessment activities. Int. J. Educ. Manag. 2022, 36, 49–62. [Google Scholar] [CrossRef]
- Mirzaian, E.; Franson, K.L. Leading a Digital Transformation in Pharmacy Education with a Pandemic as the Accelerant. Pharmacy 2021, 9, 19. [Google Scholar] [CrossRef]
- Smith, K.J.; Grundmann, O.; Moorman Li, R. The development and impact of active learning strategies on self-confidence in a newly designed first-year self-care pharmacy course-outcomes and experiences. Curr. Pharm. Teach. Learn. 2018, 10, 499–504. [Google Scholar] [CrossRef] [PubMed]
- Helmer, A.M.; Lisenby, K.M.; Smithgall, S.; Carroll, D.G.; Hester, E.K. Assessing student confidence in interprofessional communication during primary care advanced pharmacy practice experiences (APPEs). Curr. Pharm. Teach. Learn. 2020, 12, 1365–1370. [Google Scholar] [CrossRef] [PubMed]
- Er, H.M.; Jia Ming, M.K.; Keng, P.S.; Nadarajah, V.D. Pharmacy Students’ Perceptions of Reflective Portfolios and their Effect on Students’ Deep Information-Processing Skills. Am. J. Pharm. Educ. 2019, 83, 6851. [Google Scholar] [CrossRef]
- Spiegel, T.; Nivette, A. The relative impact of in-class closed-book versus take-home open-book examination type on academic performance, student knowledge retention and wellbeing. Assess. Eval. High. Educ. 2021. [Google Scholar] [CrossRef]
- Block, R.M. A Discussion of the Effect of Open-book and Closed-book Exams on Student Achievement in an Introductory Statistics Course. Primus 2012, 22, 228–238. [Google Scholar] [CrossRef]
- Zagury-Orly, I.; Durning, S.J. Assessing open-book examination in medical education: The time is now. Med. Teach. 2021, 43, 972–973. [Google Scholar] [CrossRef]
- Agarwal, P.K.; Roediger, H.L. Expectancy of an open-book test decreases performance on a delayed closed-book test. Memory 2011, 19, 836–852. [Google Scholar] [CrossRef]
- Shaikh, H.; Crowl, A.N.; Shrader, S.; Burkhardt, C.D.O. Assessing Self-Perceived Interprofessional Collaborative Competency on Advanced Pharmacy Practice Experiences Through Interprofessional Simulations. Am. J. Pharm. Educ. 2020, 84, 7530. [Google Scholar] [CrossRef]
- Dennis, V.C. Longitudinal student self-assessment in an introductory pharmacy practice experience course. Am. J. Pharm. Educ. 2005, 69, 1. [Google Scholar] [CrossRef]
- Ameripour, D.; Matthews, M.; Wang, Y.; Mirzaian, E.; Kim, R.E. Mapping student perceptions of experiential interprofessional learning to the Interprofessional Education Collaborative (IPEC) competencies. Curr. Pharm. Teach. Learn. 2022, 14, 182–192. [Google Scholar] [CrossRef]
- Liu, L.; Caliph, S.; Simpson, C.; Khoo, R.Z.; Neviles, G.; Muthumuni, S.; Lyons, K.M. Pharmacy Student Challenges and Strategies towards Initial COVID-19 Curriculum Changes. Healthcare 2021, 9, 1322. [Google Scholar] [CrossRef] [PubMed]
- Schlesselman, L.S.; Cain, J.; DiVall, M. Improving and Restoring the Well-being and Resilience of Pharmacy Students during a Pandemic. Am. J. Pharm. Educ. 2020, 84, ajpe8144. [Google Scholar] [CrossRef] [PubMed]

| Ability-Based Outcomes (ABOs) (n = 60) | Not Confident | Unsure | Confident & Very Confident |
|---|---|---|---|
| Promote Health & Wellness | 0 (0.00%) | 1 (1.67%) | 59 (98.33%) |
| Self-awareness (n = 59) | 0 (0.00%) | 1 (1.69%) | 58 (98.31%) |
| Professionalism in patient interations (n = 59) | 0 (0.00%) | 2 (3.39%) | 57 (96.61%) |
| Professionalism in interactions with society | 0 (0.00%) | 3 (5.00%) | 57 (95.00%) |
| Demonstrate accountability and ownership in all professional activities | 0 (0.00%) | 4 (6.67%) | 56 (93.33%) |
| Professionalism in healthcare provider interactions | 0 (0.00%) | 4 (6.67%) | 56 (93.33%) |
| Cultural Sensitivity | 0 (0.00%) | 4 (6.67%) | 56 (93.33%) |
| Exhibit behaviors & values that are consistent with the trust given to the profession | 0 (0.00%) | 4 (6.67%) | 56 (93.33%) |
| Communication | 0 (0.00%) | 5 (8.33%) | 55 (91.67%) |
| Patient Advocacy | 0 (0.00%) | 8 (13.33%) | 52 (86.67%) |
| Develop, Integrate, and Apply Knowledge from the Foundational Sciences | 1 (1.67%) | 7 (11.67%) | 52 (86.67%) |
| Provide Patient Centered Care | 1 (1.67%) | 9 (15.00%) | 50 (83.33%) |
| Problem Solving | 1 (1.67%) | 10 (16.67%) | 49 (81.67%) |
| Evaluate the Scientific Literature | 0 (0.00%) | 11 (18.33%) | 49 (81.67%) |
| Explain Drug Action | 0 (0.00%) | 12 (20.00%) | 48 (80.00%) |
| Leadership | 1 (1.67%) | 11 (18.33%) | 48 (80.00%) |
| Educator | 0 (0.00%) | 13 (21.67%) | 47 (78.33%) |
| Interprofessional Collaboration | 2 (3.33%) | 11 (18.33%) | 47 (78.33%) |
| Provide Population-Based Care | 1 (1.67%) | 13 (21.67%) | 46 (76.67%) |
| Optimize Safety & Efficacy of Medication Use Systems | 1 (1.67%) | 15 (25.00%) | 44 (73.33%) |
| Advance Population Health & Patient Centered Care | 1 (1.67%) | 16 (26.67%) | 43 (71.67%) |
| Solve Therapeutic Problems (n = 59) | 2 (3.39%) | 15 (25.42%) | 42 (71.19%) |
| Technological Resources (n = 59) | 1 (1.69%) | 20 (33.90%) | 38 (64.41%) |
| Physical Resources (n = 59) | 1 (1.69%) | 21 (35.59%) | 37 (62.71%) |
| Innovation & Entrepreneurship | 3 (5.00%) | 20 (33.33%) | 37 (61.67%) |
| Human Resources (n = 59) | 3 (5.08%) | 23 (38.98%) | 33 (55.93%) |
| Financial Resources | 5 (8.33%) | 28 (46.67%) | 27 (45.00%) |
| Appendix 1 Topics | Confident or Very Confident | ||
|---|---|---|---|
| Class of 2022 | Class of ’20 & ’21 Combined | Percent Δ | |
| Biochemistry | 66.67% | 88.03% | −21.36% |
| Pharmacy Law & Regulatory Affairs | 60.00% | 71.79% | −11.79% |
| Immunology | 65.00% | 76.22% | −11.22% |
| Human Physiology | 71.67% | 78.17% | −6.50% |
| Pharmacogenomics/genetics | 56.67% | 61.97% | −5.31% |
| Public Health | 77.97% | 80.99% | −3.02% |
| Medical Microbiology | 63.33% | 65.28% | −1.94% |
| Medication Dispensing, Distribution, & Administration | 88.14% | 88.67% | −0.53% |
| Professional Communication | 91.67% | 92.20% | −0.53% |
| Practice Management | 56.67% | 57.04% | −0.38% |
| Ethics | 95.00% | 92.86% | 2.14% |
| Pharmacoepidemiology | 60.00% | 57.86% | 2.14% |
| Biostatistics/research design | 54.17% | 50.21% | 3.95% |
| Patient Assessment | 83.05% | 77.78% | 5.27% |
| Natural Products and Alternative and Complementary Therapies | 57.63% | 52.11% | 5.51% |
| Extemporaneous Compounding | 65.00% | 57.64% | 7.36% |
| Pharmacoeconomics | 61.67% | 52.82% | 8.85% |
| Medicinal Chemistry | 71.67% | 60.00% | 11.67% |
| Pharmaceutics/Biopharmaceutics | 70.00% | 55.94% | 14.06% |
| Pharmacotherapy | 84.75% | 69.72% | 15.03% |
| Pharmacology and Toxicology | 78.33% | 62.89% | 15.45% |
| Healthcare Systems | 71.67% | 52.45% | 19.22% |
| Pharmacokinetics/Clinical Pharmacokinetics | 76.47% | 56.16% | 20.31% |
| Class of 2022 vs. (2021 & 2020) Ranked by Strongly Agree/Agree (2022 < 2021&2020) | |||
|---|---|---|---|
| Topic | Agree/ Strongly Agree | ||
| Class of 2022 | Class of 2021 & 2020 | Percent Δ 2022 vs. (2021 & 2020) | |
| Assess the health needs of a given patient population. | 44/59 (74.58%) | 114/140 (81.43%) | −6.85% |
| Provide patient-centered care based on evidence-based best practices; design strategies and solutions to address patient-care problems. | 140/176 (79.55%) | 273/321 (85.05%) | −5.50% |
| Apply knowledge from the foundational clinical, pharmaceutical, and biomedical sciences to the provision of patient care. | 92/118 (77.97%) | 192/236 (81.36%) | −3.39% |
| Effectively communicate (verbal, non-verbal, written) when interacting with individuals, groups, and organizations. | 49/59 (83.05%) | 163/191 (85.34%) | −2.29% |
| Act in a manner consistent with the trust given to pharmacists by patients, other healthcare providers, and society. | 52/59 (88.14%) | 127/142 (89.44%) | −1.30% |
| Class of 2022 vs (2021 & 2020) Ranked by Strongly disagree/disagree (2022 > 2021&2020) | |||
| Topic | Disagree/ Strongly Disagree | ||
| Class of 2022 | Class of 2021 & 2020 | Percent Δ 2022 vs. (2021 & 2020) | |
| Provide patient-centered care based on evidence-based best practices; design strategies and solutions to address patient-care problems. | 10/176 (5.68%) | 9/321 (2.80%) | 2.88% |
| Ability Based Outcomes (ABOs) | Average Final Evaluation Scores |
|---|---|
| Provided patient centered care | 4.42 (n = 3560) |
| Promoted health and wellness | 4.39 (n = 3641) |
| Provided population-based care | 4.31 (n= 3407) |
| Develop, integrate, and apply knowledge from the foundational sciences | 4.28 (n = 3955) |
| Evaluate the scientific literature | 4.29 (n = 3949) |
| Explain drug action | 4.21 (n = 3779) |
| Solve therapeutic problems | 4.17 (n = 3661) |
| Advance population health and patient centered care | 4.25 (n = 3501) |
| Demonstrate problem solving skills | 4.34 (n = 4020) |
| Demonstrate educator skills | 4.34 (n = 3868) |
| Engage in patient advocacy | 4.40 (n = 3585) |
| Demonstrate inter-professional collaboration | 4.60 (n = 4173) |
| Demonstrate cultural sensitivity | 4.54 (n = 4027) |
| Demonstrate effective communication skills | 4.47 (n = 4143) |
| Exhibit behaviors and values that are consistent with the profession of pharmacy | 4.67 (n = 4320) |
| Demonstrate professionalism in interactions with patients | 4.68 (n = 3574) |
| Demonstrate professionalism in interactions with other healthcare providers | 4.66 (n = 4231) |
| Demonstrate professionalism in interactions with society | 4.64 (n = 3809) |
| Exhibit behaviors that demonstrate accountability and ownership in all professional activities | 4.59 (n = 4271) |
| Optimize safety and efficacy of medication use systems | 4.36 (n = 3161) |
| Manage human resources | 4.36 (n = 1717) |
| Manage financial resources | 4.31 (n = 1447) |
| Manage technological resources | 4.49 (n = 3372) |
| Manage physical resources | 4.44 (n = 2675) |
| Demonstrate self-awareness | 4.53 (n = 4207) |
| Demonstrate leadership | 4.26 (n = 3729) |
| Innovation and entrepreneurship | 4.25 (n = 3128) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mirzaian, E.; White, S.J.; Karim, M.; Franson, K.L.; Wu, M.; Wang, Y. Exploring the Effect of Virtual Education on Student Pharmacists’ Confidence toward APPE Readiness. Pharmacy 2022, 10, 118. https://doi.org/10.3390/pharmacy10050118
Mirzaian E, White SJ, Karim M, Franson KL, Wu M, Wang Y. Exploring the Effect of Virtual Education on Student Pharmacists’ Confidence toward APPE Readiness. Pharmacy. 2022; 10(5):118. https://doi.org/10.3390/pharmacy10050118
Chicago/Turabian StyleMirzaian, Edith, Samara Jasmine White, Mona Karim, Kari L. Franson, Maryann Wu, and Ying Wang. 2022. "Exploring the Effect of Virtual Education on Student Pharmacists’ Confidence toward APPE Readiness" Pharmacy 10, no. 5: 118. https://doi.org/10.3390/pharmacy10050118
APA StyleMirzaian, E., White, S. J., Karim, M., Franson, K. L., Wu, M., & Wang, Y. (2022). Exploring the Effect of Virtual Education on Student Pharmacists’ Confidence toward APPE Readiness. Pharmacy, 10(5), 118. https://doi.org/10.3390/pharmacy10050118










