Kidney Function Assessment in African American Patients: A Narrative Review for Pharmacists
Abstract
:1. Introduction
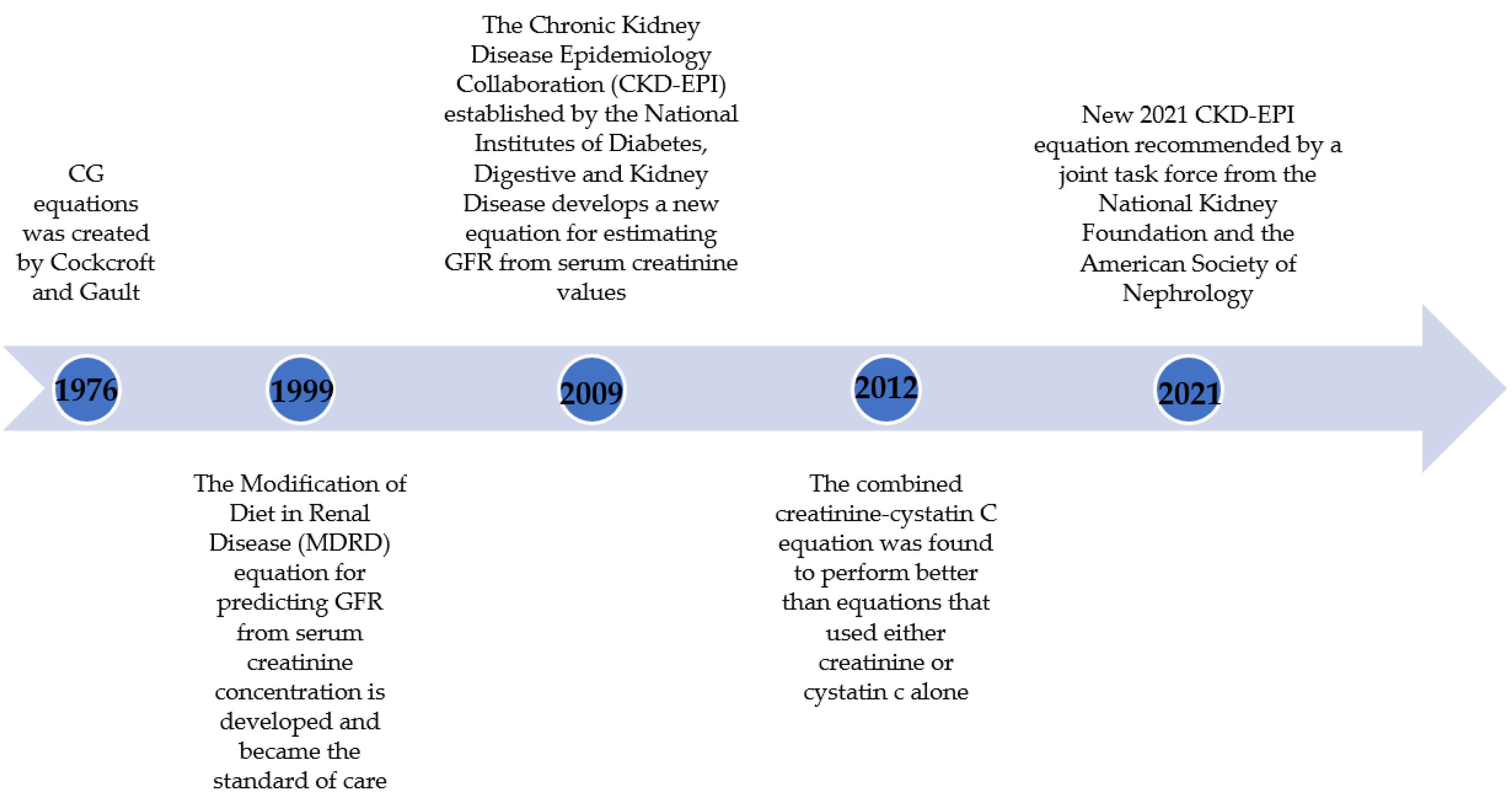
2. Evolution of Equations to Estimate Kidney Function
3. Race Coefficients in Equations Estimating GFR
4. Markers in eGFR Calculations and Consequences of Removing Race from GFR Estimation
5. Reassessment of the Use of Race in eGFR Estimating Equation and the New 2021 CKD-EPI Equation
6. Implications of the Change on Pharmacy Practice
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- United States Renal Data System. 2019 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States; National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, MD, USA, 2019.
- Murphy, D.; McCulloch, C.E.; Lin, F.; Banerjee, T.; Bragg-Gresham, J.L.; Eberhardt, M.S.; Morgenstern, H.; Pavkov, M.E.; Saran, R.; Powe, N.R.; et al. Trends in Prevalence of Chronic Kidney Disease in the United States. Ann. Intern. Med. 2016, 165, 473–481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, B.; Matsushita, K.; Abate, K.H.; Al-Aly, Z.; Ärnlöv, J.; Asayama, K.; Atkins, R.; Badawi, A.; Ballew, S.H.; Banerjee, A.; et al. Global Cardiovascular and Renal Outcomes of Reduced GFR. J. Am. Soc. Nephrol. 2017, 28, 2167–2179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hall, Y.N. Social Determinants of Health: Addressing Unmet Needs in Nephrology. Am. J. Kidney Dis. 2018, 72, 582–591. [Google Scholar] [CrossRef] [PubMed]
- Stevens, P.E.; Levin, A. Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: Synopsis of the kidney disease: Improving global outcomes 2012 clinical practice guideline. Ann. Intern. Med. 2013, 158, 825–830. [Google Scholar] [CrossRef] [Green Version]
- Eneanya, N.D.; Yang, W.; Reese, P.P. Reconsidering the Consequences of Using Race to Estimate Kidney Function. JAMA 2019, 322, 113–114. [Google Scholar] [CrossRef]
- United States Census. Available online: https://www.census.gov/quickfacts/fact/table/US/PST045221 (accessed on 20 May 2022).
- Soveri, I.; Berg, U.B.; Björk, J.; Elinder, C.-G.; Grubb, A.; Mejare, I.; Sterner, G.; Bäck, S.-E. Measuring GFR: A systematic review. Am. J. Kidney Dis. 2014, 64, 411–424. [Google Scholar] [CrossRef]
- Cockcroft, D.W.; Gault, M.H. Prediction of creatinine clearance from serum creatinine. Nephron 1976, 16, 31–41. [Google Scholar] [CrossRef]
- Levey, A.S.; Bosch, J.P.; Lewis, J.B.; Greene, T.; Rogers, N.; Roth, D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann. Intern. Med. 1999, 130, 461–470. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., III; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612, Erratum in Ann. Intern. Med. 2011 155, 408. [Google Scholar] [CrossRef]
- Inker, L.A.; Schmid, C.H.; Tighiouart, H.; Eckfeldt, J.H.; Feldman, H.I.; Greene, T.; Kusek, J.W.; Manzi, J.; Van Lente, F.; Zhang, Y.L.; et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N. Engl. J. Med. 2012, 367, 20–29, Erratum in N. Engl. J. Med. 2012, 367, 681; Erratum in N. Engl. J. Med. 2012, 367, 2060. [Google Scholar] [CrossRef] [Green Version]
- Teaford, H.R.; Barreto, J.N.; Vollmer, K.J.; Rule, A.D.; Barreto, E.F. Cystatin C: A Primer for Pharmacists. Pharmacy 2020, 8, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peters, B.J.; Rule, A.D.; Kashani, K.B.; Lieske, J.C.; Mara, K.C.; Dierkhising, R.A.; Barreto, E.F. Impact of Serum Cystatin C-Based Glomerular Filtration Rate Estimates on Drug Dose Selection in Hospitalized Patients. Pharmacotherapy 2018, 38, 1068–1073. [Google Scholar] [CrossRef] [PubMed]
- Jelliffe, R.W. Letter: Creatinine clearance: Bedside estimate. Ann. Intern. Med. 1973, 79, 604–605. [Google Scholar] [CrossRef] [PubMed]
- Salazar, D.E.; Corcoran, G.B. Predicting creatinine clearance and renal drug clearance in obese patients from estimated fat-free body mass. Am. J. Med. 1988, 84, 1053–1060. [Google Scholar] [CrossRef]
- Pottel, H.; Björk, J.; Courbebaisse, M.; Couzi, L.; Ebert, N.; Eriksen, B.O.; Dalton, R.N.; Dubourg, L.; Gaillard, F.; Garrouste, C.; et al. Development and Validation of a Modified Full Age Spectrum Creatinine-Based Equation to Estimate Glomerular Filtration Rate: A Cross-sectional Analysis of Pooled Data. Ann. Intern. Med. 2021, 174, 183–191. [Google Scholar] [CrossRef]
- Ebert, N.; Bevc, S.; Bökenkamp, A.; Gaillard, F.; Hornum, M.; Jager, K.J.; Mariat, C.; Eriksen, B.O.; Palsson, R.; Rule, A.D.; et al. Assessment of kidney function: Clinical indications for measured GFR. Clin. Kidney J. 2021, 14, 1861–1870. [Google Scholar] [CrossRef]
- Marshall, E. DNA studies challenge the meaning of race. Science 1998, 282, 654–655. [Google Scholar] [CrossRef]
- Flamant, M.; Vidal-Petiot, E.; Metzger, M.; Haymann, J.-P.; Letavernier, E.; Delatour, V.; Karras, A.; Thervet, E.; Boffa, J.-J.; Houillier, P.; et al. Performance of GFR estimating equations in African Europeans: Basis for a lower race-ethnicity factor than in African Americans. Am. J. Kidney Dis. 2013, 62, 182–184. [Google Scholar] [CrossRef]
- Bukabau, J.B.; Yayo, E.; Gnionsahé, A.; Monnet, D.; Pottel, H.; Cavalier, E.; Nkodila, A.; Makulo, J.R.R.; Mokoli, V.M.; Lepira, F.B.; et al. Performance of creatinine- or cystatin C-based equations to estimate glomerular filtration rate in sub-Saharan African populations. Kidney Int. 2019, 95, 1181–1189. [Google Scholar] [CrossRef] [Green Version]
- Bukabau, J.B.; Sumaili, E.K.; Cavalier, E.; Pottel, H.; Kifakiou, B.; Nkodila, A.; Makulo, J.R.R.; Mokoli, V.M.; Zinga, C.V.; Longo, A.L.; et al. Performance of glomerular filtration rate estimation equations in Congolese healthy adults: The inopportunity of the ethnic correction. PLoS ONE 2018, 13, e0193384. [Google Scholar] [CrossRef]
- Levey, A.S.; Coresh, J.; Greene, T.; Stevens, L.A.; Zhang, Y.L.; Hendriksen, S.; Kusek, J.W.; Van Lente, F.; Chronic Kidney Disease Epidemiology Collaboration. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann. Intern. Med. 2006, 145, 247–254, Erratum in Ann. Intern. Med. 2008, 149, 519; Erratum in Ann. Intern. Med. 2021, 174, 584. [Google Scholar] [CrossRef]
- Eneanya, N.D.; Boulware, L.E.; Tsai, J.; Bruce, M.A.; Ford, C.L.; Harris, C.; Morales, L.S.; Ryan, M.J.; Reese, P.P.; Thorpe, R.J.; et al. Health inequities and the inappropriate use of race in nephrology. Nat. Rev. Nephrol. 2022, 18, 84–94. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; Tighiouart, H.; Titan, S.M.; Inker, L.A. Estimation of Glomerular Filtration Rate with vs without Including Patient Race. JAMA Intern. Med. 2020, 180, 793–795. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S. Measurement of renal function in chronic renal disease. Kidney Int. 1990, 38, 167–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsu, C.Y.; Yang, W.; Parikh, R.V.; Anderson, A.H.; Chen, T.K.; Cohen, D.L.; He, J.; Mohanty, M.J.; Lash, J.P.; Mills, K.T.; et al. Race, Genetic Ancestry, and Estimating Kidney Function in CKD. N. Engl. J. Med. 2021, 385, 1750–1760. [Google Scholar] [CrossRef]
- Grubb, A.; Horio, M.; Hansson, L.O.; Björk, J.; Nyman, U.; Flodin, M.; Larsson, A.; Bökenkamp, A.; Yasuda, Y.; Blufpand, H.; et al. Generation of a new cystatin C-based estimating equation for glomerular filtration rate by use of 7 assays standardized to the international calibrator. Clin. Chem. 2014, 60, 974–986. [Google Scholar] [CrossRef]
- Delgado, C.; Baweja, M.; Crews, D.C.; Eneanya, N.D.; Gadegbeku, C.A.; Inker, L.A.; Mendu, M.L.; Miller, W.G.; Moxey-Mims, M.M.; Roberts, G.V.; et al. A Unifying Approach for GFR Estimation: Recommendations of the NKF-ASN Task Force on Reassessing the Inclusion of Race in Diagnosing Kidney Disease. Am. J. Kidney Dis. 2022, 79, 268–288.e1. [Google Scholar] [CrossRef]
- Inker, L.A.; Eneanya, N.D.; Coresh, J.; Tighiouart, H.; Wang, D.; Sang, Y.; Crews, D.C.; Doria, A.; Estrella, M.M.; Froissart, M.; et al. New Creatinine- and Cystatin C-Based Equations to Estimate GFR without Race. N. Engl. J. Med. 2021, 385, 1737–1749. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. Guidance for Industry: Pharmacokinetics in Patients with Impaired Renal Function—Study Design, Data Analysis and Impact on Dosing and Labeling. 1998. Available online: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm072127.pdf (accessed on 3 May 2022).
- Pai, M.P. Estimating the glomerular filtration rate in obese adult patients for drug dosing. Adv. Chronic Kidney Dis. 2010, 17, e53–e62. [Google Scholar] [CrossRef]
- Dowling, T.C.; Wang, E.S.; Ferrucci, L.; Sorkin, J.D. Glomerular filtration rate equations overestimate creatinine clearance in older individuals enrolled in the Baltimore Longitudinal Study on Aging: Impact on renal drug dosing. Pharmacotherapy 2013, 33, 912–921. [Google Scholar] [CrossRef] [Green Version]
- Hudson, J.Q.; Nolin, T.D. Pragmatic Use of Kidney Function Estimates for Drug Dosing: The Tide Is Turning. Adv. Chronic Kidney Dis. 2018, 25, 14–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matzke, G.R.; Aronoff, G.R.; Atkinson, A.J., Jr.; Bennett, W.M.; Decker, B.S.; Eckardt, K.-U.; Golper, T.; Grabe, D.W.; Kasiske, B.; Keller, F.; et al. Drug dosing consideration in patients with acute and chronic kidney disease-a clinical update from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2011, 80, 1122–1137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- FDA. Guidance for Industry Pharmacokinetics in Patients with Impaired Renal Function—Study Design, Data Analysis, and Impact on Dosing. Available online: https://www.fda.gov/media/78573/download (accessed on 3 May 2022).
- Ahmed, S.; Nutt, C.T.; Eneanya, N.D.; Reese, P.P.; Sivashanker, K.; Morse, M.; Sequist, T.; Mendu, M.L. Examining the potential impact of race multiplier utilization in estimated glomerular filtration rate calculation on African-American care outcomes. J. Gen. Intern. Med. 2021, 36, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Walther, C.P.; Winkelmayer, W.C.; Navaneethan, S.D. Black race coefficient in GFR estimation and diabetes medications in CKD: National estimates. J. Am. Soc. Nephrol. 2021, 32, 1319–1321. [Google Scholar] [CrossRef] [PubMed]
- Vondracek, S.F.; Teitelbaum, I.; Kiser, T.H. Principles of Kidney Pharmacotherapy for the Nephrologist: Core Curriculum 2021. Am. J. Kidney Dis. 2021, 78, 442–458. [Google Scholar] [CrossRef] [PubMed]

| Equation | Year | Formula | Parameter |
|---|---|---|---|
| Cockcroft and Gault | 1976 | ((140 − age) × weight)/(72 × Scr) | Age, sex, weight, serum creatinine |
| Modification of Diet in Renal Disease (MDRD) | 1999 | GFR = 175 × Serum Cr−1.154 × age−0.203 × 1.212 (if patient is black) × 0.742 (if female) | Age, sex, race, serum creatinine |
| Chronic Kidney Disease Epidemiology (CKD-EPI)-creatinine | 2009 | A × (Scr/B)C × 0.993age × (1.159 if black), where A, B, and C are the following: Female: if Scr ≤ 0.7: A = 144, B = 0.7 C = −0.329. if Scr > 0.7: A = 144, B = 0.7, C = −1.209. Male: if Scr ≤ 0.9: A = 141, B = 0.9 C = −0.411. if Scr > 0.9: A = 141, B = 0.9, C = −1.209 | Age, sex, race, serum creatinine |
| Chronic Kidney Disease Epidemiology (CKD-EPI)-creatinine-cystatin C | 2012 | 133 × (Scys/0.8)A × 0.996age × B, where A and B are the following: Female: if Scr ≤ 0.8: A = −0.499, B = 0.932 if Scr > 0.8: A = −0.499, B = 0.932. Male: if Scr ≤ 0.8: A = −0.499, B = 1.0 if Scr > 0.8: A = −0.499, B = 1.0 | Age, sex, race, serum creatinine, serum cystatin C |
| Equation | Marker | Year | Age | Gender-Women | Black Race |
|---|---|---|---|---|---|
| MDRD | Creatinine (eGFRcr) | 1999 | Age−0.203 | 0.74 | 1.21 |
| CKD-EPI | Creatinine (eGFRcr) | 2009 | 0.993Age | 0.75 | 1.159 |
| CKD-EPI | Cystatin C (eGFRcys) | 2012 | 0.996Age | 0.93 | NA |
| CKD-EPI | Creatinine-cystatin C (eGFRcr-sys) | 2012 | 0.995Age | 0.83 | 1.08 |
| All Individuals (N = 8254) a | Black Individuals (n =2601) | ||
|---|---|---|---|
| Coefficients used in the equation a | Black race coefficient | Root mean square error | Root mean square error |
| (95% CI) b | (95% CI) | ||
| Serum creatinine, age, sex, race | 1.16 | 0.236 | 0.243 |
| (0.229 to 0.242) | (0.232 to 0.254) | ||
| Serum creatinine, age, sex | N/A | 0.244 | 0.258 |
| (0.238 to 0.251) | (0.248 to 0.268) | ||
| Serum creatinine, age, race, sex, height, and weight | 1.15 | 0.235 | 0.242 |
| (0.229 to 0.242) | (0.232 to 0.253) | ||
| Serum creatinine, age, sex, height, and weight | N/A | 0.243 | 0.255 |
| (0.237 to 0.250) | (0.245 to 0.265) | ||
| Markers and Non-GFR Determinants Used | P30 | P30 % Difference between Black and Non-Black | Correct Classification |
|---|---|---|---|
| 2009 CKD-EPI-Scr, Age, Sex, Race | Black 85% | −4% | Black 63% |
| Non-Black 89% | Non-Black 69% | ||
| 2021 CKD-EPI-Scr, Age, Sex | Black 87% | 1% | Black 62% |
| Non-Black 86% | Non-Black 67% | ||
| 2009 CKD-EPI-Cys-C Age, Sex | Black 89% | −3% | Black 68% |
| Non-Black 92% | Non-Black 71% | ||
| 2021 CKD-EPI-Cys-C/Scr Age, Sex | Black 90.5% | −0.3% | Black 68% |
| Non-Black 90.8% | Non-Black 70% |
| Equation * | Intercept μ (95% CI) | Coefficients for Creatinine (95% CI) ** | Coefficient c for Age (95% CI) | Coefficient d for Female Sex (95% CI) | Coefficient e for Black Race (95% CI) | |
|---|---|---|---|---|---|---|
| a1 | a2 | |||||
| 2009 CKD-EPI creatinine | 141 | F: −0.329 (−0.428 to −0.230); M: −0.411 (−0.508 to −0.314) | −1.209 | 0.9929 | 1.018 | 1.159 |
| (139 to 144) | (−1.220 to −1.198) | (0.9925 to 0.9933) | (1.007 to 1.029) | (1.144 to 1.170) | ||
| 2021 CKD-EPI creatinine (without race) | 142 | F: −0.241 (−0.344 to −0.138); M: −0.302 (−0.403 to −0.202) | −1.200 | 0.9938 | 1.012 | --- |
| (139 to 144) | (−1.211 to −1.189) | (0.9935 to 0.9942) | (1.000 to 1.023) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rungkitwattanakul, D.; Chaijamorn, W.; Han, E.; Aldhaeefi, M. Kidney Function Assessment in African American Patients: A Narrative Review for Pharmacists. Pharmacy 2022, 10, 65. https://doi.org/10.3390/pharmacy10030065
Rungkitwattanakul D, Chaijamorn W, Han E, Aldhaeefi M. Kidney Function Assessment in African American Patients: A Narrative Review for Pharmacists. Pharmacy. 2022; 10(3):65. https://doi.org/10.3390/pharmacy10030065
Chicago/Turabian StyleRungkitwattanakul, Dhakrit, Weerachai Chaijamorn, Eunice Han, and Mohammed Aldhaeefi. 2022. "Kidney Function Assessment in African American Patients: A Narrative Review for Pharmacists" Pharmacy 10, no. 3: 65. https://doi.org/10.3390/pharmacy10030065
APA StyleRungkitwattanakul, D., Chaijamorn, W., Han, E., & Aldhaeefi, M. (2022). Kidney Function Assessment in African American Patients: A Narrative Review for Pharmacists. Pharmacy, 10(3), 65. https://doi.org/10.3390/pharmacy10030065






