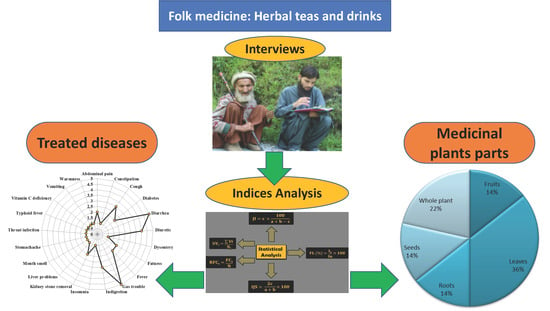
Herbal Teas and Drinks: Folk Medicine of the Manoor Valley, Lesser Himalaya, Pakistan
Abstract
1. Introduction
2. Results
2.1. Floristic Diversity
2.2. Treated Diseases
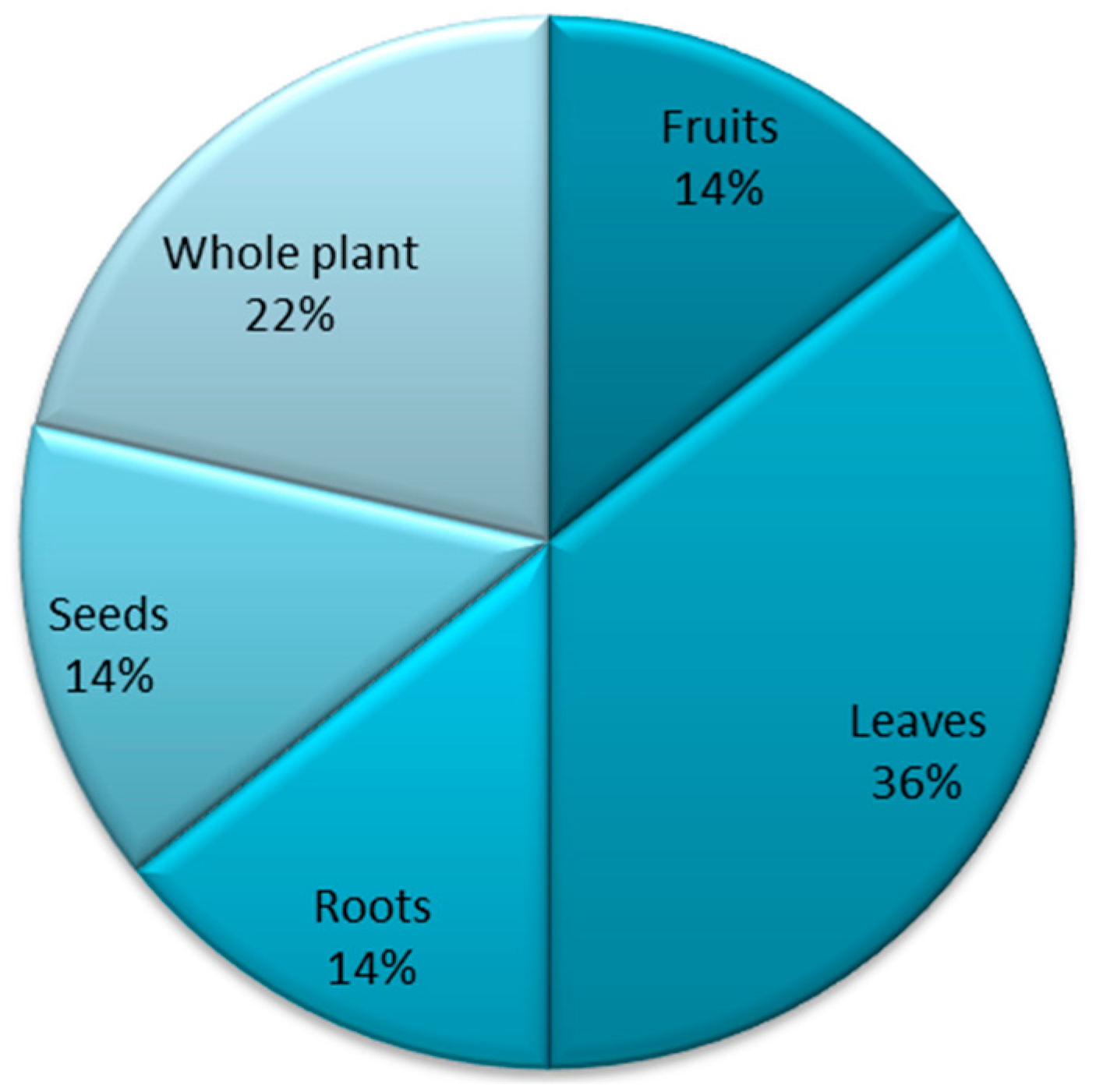
2.3. Medicinal Plants Parts Used
2.4. Use Value (UVi)
2.5. Relative Frequency Citations (RFCs)
2.6. Fidelity Level (%)
3. Discussion
4. Materials and Methods
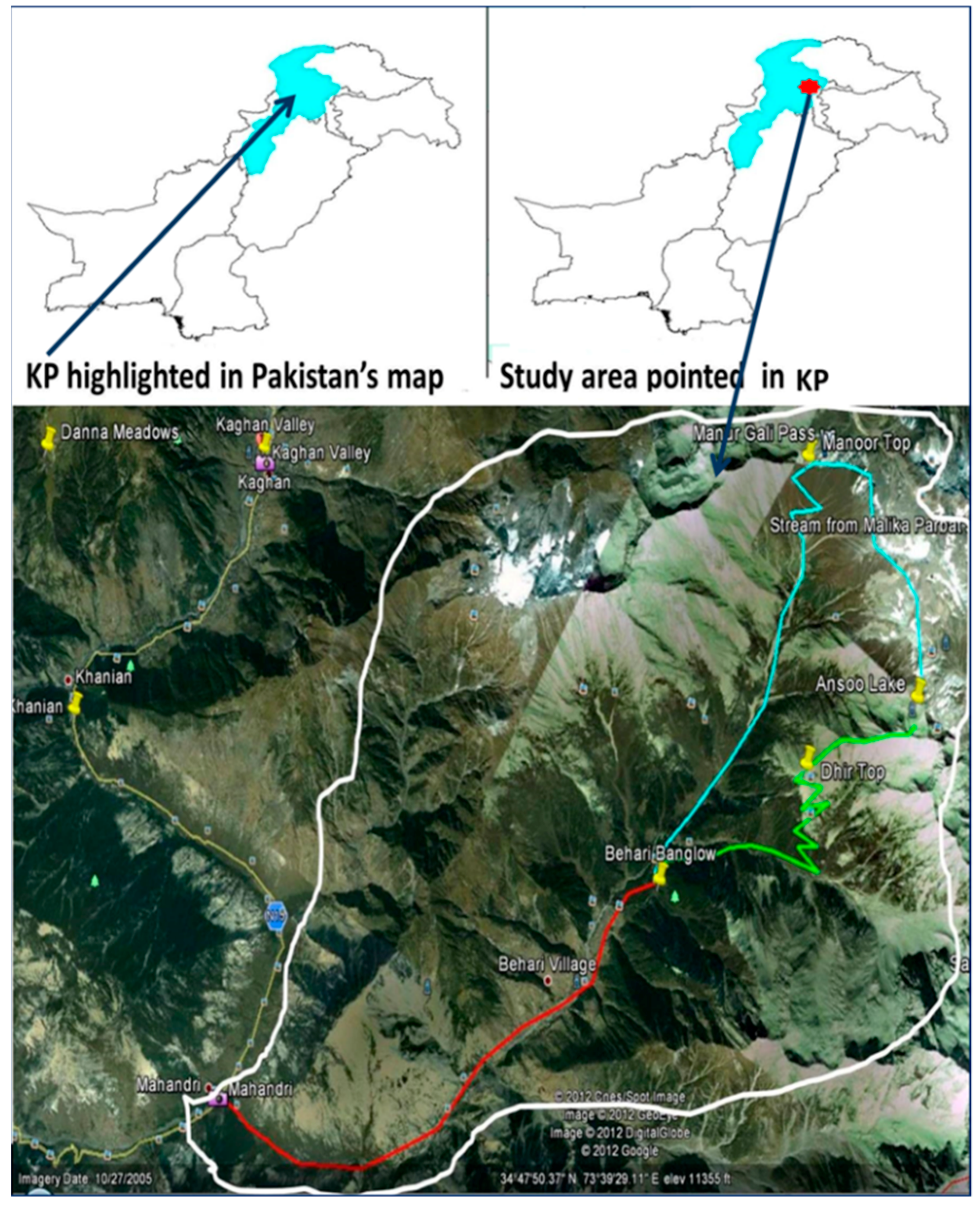
4.1. Study Area
4.2. Field Surveys, Plants Collection, Interviews, and Questionnaire
4.3. Tea and Drink Infusions Preparation
4.4. Herbarium Work and Plant Identification
4.5. Data Analysis
4.5.1. Use Value Index (UVi)
4.5.2. Relative Frequency Citations (RFCs)
4.5.3. Fidelity Level (FL%)
4.5.4. Sorensen’s Similarity Index (QS%)
4.5.5. Rahman’s Similarity Index (RSI)
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ravikumar, C. Review on Herbal Teas. J. Pharm. Sci. Res. 2014, 6, 236–238. [Google Scholar]
- Zielinski, A.A.F.; Haminiuk, C.W.I.; Alberti, A.; Nogueira, A.; Demiate, I.M.; Granato, D. A comparative study of the phenolic compounds and the in vitro antioxidant activity of different Brazilian teas using multivariate statistical techniques. Food Res. Int. 2014, 60, 246–254. [Google Scholar] [CrossRef]
- Mustafa, G.; Arif, R.; Atta, A.; Sharif, S.; Jamil, A. Bioactive Compounds from Medicinal Plants and Their Importance in Drug Discovery in Pakistan. Matrix Sci. Pharma 2017, 1, 17–26. [Google Scholar] [CrossRef]
- Rahman, I.U.; Afzal, A.; Iqbal, Z.; Ijaz, F.; Ali, N.; Bussmann, R.W. Traditional and ethnomedicinal dermatology practices in Pakistan. Clin. Dermatol. 2018, 36, 310–319. [Google Scholar] [CrossRef]
- Ijaz, F.; Iqbal, Z.; Rahman, I.U.; Alam, J.; Khan, S.M.; Shah, G.M.; Khan, K.; Afzal, A. Investigation of traditional medicinal floral knowledge of Sarban Hills, Abbottabad, KP, Pakistan. J. Ethnopharmacol. 2016, 179, 208–233. [Google Scholar] [CrossRef]
- Rahman, I.U.; Ijaz, F.; Afzal, A.; Iqbal, Z.; Ali, N.; Khan, S.M. Contributions to the phytotherapies of digestive disorders: Traditional knowledge and cultural drivers of Manoor Valley, Northern Pakistan. J. Ethnopharmacol. 2016, 192, 30–52. [Google Scholar] [CrossRef]
- Audu, B.S.; Ofojekwu, P.C.; Ujah, A.; Ajima, M.N.O. Phytochemical, proximate composition, amino acid profile and characterisation of Marijuana (Canabia sativa). J. Phytopharm. 2014, 3, 35–43. [Google Scholar]
- Sher, H.; Bussmann, R.W.; Hart, R.; De Boer, H.J. Traditional use of medicinal plants among Kalasha, Ismaeli and Sunni groups in Chitral District, Khyber Pakhtunkhwa province, Pakistan. J. Ethnopharmacol. 2016, 188, 57–69. [Google Scholar] [CrossRef]
- Uprety, Y.; Asselin, H.; Boon, E.K.; Yadav, S.; Shrestha, K.K. Indigenous use and bio-efficacy of medicinal plants in the Rasuwa District, Central Nepal. J. Ethnobiol. Ethnomed. 2010, 6, 3. [Google Scholar] [CrossRef]
- Ijaz, F. Biodiversity and Traditional Uses of Plants of Sarban Hills, Abbottabad. Master’s Thesis, Department of Botany, Hazara University Mansehra, Dhodial, Pakistan, 2014. [Google Scholar]
- Iqbal, M.; Khan, S.; Khan, M.; Rahman, I.; Abbas, Z.; Zahidullah. Exploration and inventorying of weeds in wheat crop of the district Malakand, Pakistan. Pak. J. Weed Sci. Res. 2015, 21, 435–452. [Google Scholar]
- Kumar, S.; Pandey, A.K. Chemistry and Biological Activities of Flavonoids: An Overview. Sci. World J. 2013, 2013, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Kichu, M.; Malewska, T.; Akter, K.; Imchen, I.; Harrington, D.; Kohen, J.; Vemulpad, S.R.; Jamie, J.F. An ethnobotanical study of medicinal plants of Chungtia village, Nagaland, India. J. Ethnopharmacol. 2015, 166, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Luitel, D.R.; Rokaya, M.B.; Timsina, B.; Münzbergová, Z. Medicinal plants used by the Tamang community in the Makawanpur district of central Nepal. J. Ethnobiol. Ethnomed. 2014, 10, 5. [Google Scholar] [CrossRef] [PubMed]
- Ijaz, F.; Iqbal, Z.; Alam, J.; Khan, S.M.; Afzal, A.; Rahman, I.U.; Afzal, M.; Islam, M. Sohail Ethno Medicinal Study upon Folk Recipes Against Various Human Diseases in Sarban Hills, Abbottabad, Pakistan. World J. Zool. 2015, 10, 41–46. [Google Scholar]
- Kunwar, R.M.; Nepal, B.K.; Kshhetri, H.B.; Rai, S.K.; Bussmann, R.W. Ethnomedicine in Himalaya: A case study from Dolpa, Humla, Jumla and Mustang districts of Nepal. J. Ethnobiol. Ethnomed. 2006, 2, 1–6. [Google Scholar] [CrossRef]
- Rahman, I.U.; Ijaz, F.; Iqbal, Z.; Afzal, A.; Ali, N.; Afzal, M.; Khan, M.A.; Muhammad, S.; Qadir, G.; Asif, M. A novel survey of the ethno medicinal knowledge of dental problems in Manoor Valley (Northern Himalaya), Pakistan. J. Ethnopharmacol. 2016, 194, 877–894. [Google Scholar] [CrossRef]
- Srithi, K.; Balslev, H.; Wangpakapattanawong, P.; Srisanga, P.; Trisonthi, C. Medicinal plant knowledge and its erosion among the Mien (Yao) in northern Thailand. J. Ethnopharmacol. 2009, 123, 335–342. [Google Scholar] [CrossRef]
- Chaudhary, N.I.; Schnapp, A.; Park, J.E. Pharmacologic Differentiation of Inflammation and Fibrosis in the Rat Bleomycin Model. Am. J. Respir. Crit. Care Med. 2006, 173, 769–776. [Google Scholar] [CrossRef]
- Musa, E.; Badwi, E.S.; Elnabi, J.M.; Osman, E.A.; Dahab, M.M. Hepatoprotective and toxicity assessment of Cannabis sativa seed oil in Albino rat. Int. J. Chem. Biochem. Sci. 2012, 1, 69–76. [Google Scholar]
- Prasad, M.P. Phytochemical analysis and DNA fingerprinting of Mentha species using RAPD molecular markers. Int. J. Adv. Biotechnol. Res. 2014, 5, 31–35. [Google Scholar]
- Atta, A.H.; Nasr, S.M.; Mouneir, S.M. Potential protective effect of some plant extracts against carbon tetrachloride-induced hepatotoxicity. Afr. J. Tradit. Complement. Altern. Med. 2006, 3, 1–9. [Google Scholar] [CrossRef]
- Rashid, S.; Ahmad, M.; Zafar, M.; Sultana, S.; Ayub, M.; Khan, M.A.; Yaseen, G. Ethnobotanical survey of medicinally important shrubs and trees of Himalayan region of Azad Jammu and Kashmir, Pakistan. J. Ethnopharmacol. 2015, 166, 340–351. [Google Scholar] [CrossRef] [PubMed]
- Aruna, K.; Rajeswari, P.D.R.; Prabu, K.; Ramkumar, M.; Chidambaram, R.; Sankar, S.R. Quantitative phytochemical analysis of Oxalis corniculata L. (Oxalidaceae). World J. Pharm. Pharm. Sci. 2014, 3, 711–716. [Google Scholar]
- Rao, Y.K.; Fang, S.-H.; Tzeng, Y.-M.; Yerra, K.R. Antiinflammatory activities of flavonoids and a triterpene caffeate isolated from Bauhinia variegata. Phytother. Res. 2008, 22, 957–962. [Google Scholar] [CrossRef]
- Yadava, R.; Reddy, V.M.S. Anti-inflammatory activity of a novel flavonol glycoside from the Bauhinia variegata Linn. Nat. Prod. Res. 2003, 17, 165–169. [Google Scholar] [CrossRef]
- Parekh, J.; Chanda, S. Antibacterial and phytochemical studies on twelve species of Indian medicinal plants. Afr. J. Biomed. Res. 2010, 10, 10. [Google Scholar] [CrossRef]
- Qureshi, S.J.; Khan, M.A.; Ahmad, M. A survey of useful medicinal plants of Abbottabad in northern Pakistan. Trakia J. Sci. 2008, 6, 39–51. [Google Scholar]
- Akhtar, N.; Rashid, A.; Murad, W.; Bergmeier, E. Diversity and use of ethno-medicinal plants in the region of Swat, North Pakistan. J. Ethnobiol. Ethnomed. 2013, 9, 25. [Google Scholar] [CrossRef]
- Kadir, M.F.; Bin Sayeed, M.S.; Setu, N.I.; Mostafa, A.; Mia, M.M.K. Ethnopharmacological survey of medicinal plants used by traditional health practitioners in Thanchi, Bandarban Hill Tracts, Bangladesh. J. Ethnopharmacol. 2014, 155, 495–508. [Google Scholar] [CrossRef]
- Ullah, S.; Khan, M.R.; Shah, N.A.; Shah, S.A.; Majid, M.; Farooq, M.A. Ethnomedicinal plant use value in the Lakki Marwat District of Pakistan. J. Ethnopharmacol. 2014, 158, 412–422. [Google Scholar] [CrossRef]
- Gunalan, G.; Saraswathy, A.; Krishnamurthy, V. Antimicrobial activity of medicinal plant Bauhinia variegata Linn. Int. J. Pharm. Biol. Sci. 2011, 1, 400–408. [Google Scholar]
- Rajkapoor, B.; Jayakar, B.; Murugesh, N.; Sakthisekaran, D. Chemoprevention and cytotoxic effect of Bauhinia variegata against N-nitrosodiethylamine induced liver tumors and human cancer cell lines. J. Ethnopharmacol. 2006, 104, 407–409. [Google Scholar] [CrossRef] [PubMed]
- Rajkapoor, B.; Jayakar, B.; Murugesh, N. Antitumour activity of Bauhinia variegata on Dalton’s ascitic lymphoma. J. Ethnopharmacol. 2003, 89, 107–109. [Google Scholar] [CrossRef]
- Rajani, G.; Ashok, P. In Vitro antioxidant and antihyperlipidemic activities of Bauhinia variegata Linn. Indian J. Pharmacol. 2009, 41, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Bhardwaaj, P.; Varshneya, C.; Telang, R.S. Anthelmintic activity of leaves of Bauhinia variegata. Indian Vet. J. 2005, 82, 855–857. [Google Scholar]
- Mandal, S.; Upadhyay, N.; Sharma, I.; Rohit, S.; Mandloi, A. A comparative antipyretic activity of the crude extracts of the ariel parts of Glycosmis pentaphylla and Bauhinia variegata. Recent Res. Sci. Technol. 2011, 3, 16–18. [Google Scholar]
- Patil, J.K.; Jalalpure, S.S.; Hamid, S.; Ahirrao, R.A. In Vitro Immunomodulatory Activity of extracts of Bauhinia vareigata Linn bark on Human Neutrophils. Iran. J. Pharmacol. Ther. 2010, 9, 41–46. [Google Scholar]
- Bhatia, L.; Bishnoi, H.; Chauhan, P.; Kinja, K.; Shailesh, S. In Vitro comparative antioxidant activity of ethanolic extracts of Glycosmis pentaphylla and Bauhinia variegata. Recent Res. Sci. Technol. 2011, 3, 1–3. [Google Scholar]
- Kulkarni, Y.A.; Warrier, S. Acute and repeated dose toxicity studies of methanol extract of Bauhinia variegata leaves. FASEB J. 2012, 26, 1124–1125. [Google Scholar] [CrossRef]
- Matin, A.; Khan, M.A.; Ashraf, M.; Qureshi, R.A. Traditional uses of herbs, shrubs and trees of shugran valley, Mansehra, Pakistan. Pak. J. Biol. Sci. 2001, 4, 1101–1107. [Google Scholar]
- Khan, S.M.; Page, S.; Ahmad, H.; Shaheen, H.; Ullah, Z.; Ahmad, M.; Harper, D.M. Medicinal flora and ethnoecological knowledge in the Naran Valley, Western Himalaya, Pakistan. J. Ethnobiol. Ethnomed. 2013, 9, 4. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, H.; Khan, S.M.; Ghafoor, S.; Ali, N. Ethnobotanical study of Upper Siran. J. Herbs Spices Med. Plants 2009, 15, 86–97. [Google Scholar]
- Bano, A.; Ahmad, M.; Zafar, M.; Sultana, S.; Rashid, S.; Khan, M.A. Ethnomedicinal knowledge of the most commonly used plants from Deosai Plateau, Western Himalayas, Gilgit Baltistan, Pakistan. J. Ethnopharmacol. 2014, 155, 1046–1052. [Google Scholar] [CrossRef] [PubMed]
- Özdemir, E.; Alpınar, K.; Alpinar, K. An ethnobotanical survey of medicinal plants in western part of central Taurus Mountains: Aladaglar (Nigde–Turkey). J. Ethnopharmacol. 2015, 166, 53–65. [Google Scholar] [CrossRef]
- Ahmad, K.S.; Kayani, W.K.; Hameed, M.; Ahmad, F.; Nawaz, T. Floristic diversity and ethnobotany of Senhsa, district Kotli, Azad Jammu & Kashmir (Pakistan). Pak. J. Bot. 2012, 44, 195–201. [Google Scholar]
- Ajaib, M.; Khan, Z. Ethnobotanical studies of useful trees of District Kotli, Azad Jammu and Kashmir. Biologia 2014, 60, 63–71. [Google Scholar]
- Ahmad, K.; Pieroni, A. Folk knowledge of wild food plants among the tribal communities of Thakht-e-Sulaiman Hills, North-West Pakistan. J. Ethnobiol. Ethnomed. 2016, 12, 17. [Google Scholar] [CrossRef]
- Tariq, A.; Adnan, M.; Abdelsalam, N.M.; Fouad, H.; Hussain, K.; Ullah, R.; Ullah, A. Richness and Cover of Nontimber Economic Plants along Altitude in Temperate Himalayan Forest-Use Types. Sci. World J. 2014, 2014, 1–10. [Google Scholar] [CrossRef]
- Jan, G. An Ethnobotanical Survey on Fuel Wood and Timber Plant Species of Kaghan Valley, Khyber pakhtoonkhwa Province, Pakistan. Afr. J. Biotechnol. 2011, 10, 19075–19083. [Google Scholar]
- Abbasi, A.M.; Khan, S.M.; Ahmad, M.; Khan, M.A.; Quave, C.L.; Pieroni, A. Botanical ethnoveterinary therapies in three districts of the Lesser Himalayas of Pakistan. J. Ethnobiol. Ethnomed. 2013, 9, 84. [Google Scholar] [CrossRef]
- Jamal, Z.; Ahmad, M.; Zafar, M.; Sultana, S.; Khan, M.A.; Shah, G.M. Medicinal plants used in folk recipes by the local communities of Kaghan valley, Mansehra, Pakistan. Indian J. Tradit. Knowl. 2012, 11, 634–639. [Google Scholar]
- Ummara, U.; Bokhari, Z.; Altaf, A.; Younis, U.; Dasti, A.A. Pharmacological study of Shogran Valley Flora, Pakistan. Int. J. Sci. Eng. Res. 2013, 4, 1419–1427. [Google Scholar]
- Rahman, I.U.; Afzal, A.; Iqbal, Z.; Abd Allah, E.F.; Alqarawi, A.A.; Calixto, E.S.; Ali, N.; Ijaz, F.; Kausar, R.; Alsubeie, M.S.; et al. Role of multivariate approaches in floristic diversity of Manoor Valley (Himalayan Region), Pakistan. Appl. Ecol. Environ. Res. 2019, 17, 1475–1498. [Google Scholar] [CrossRef]
- Rahman, I.U.; Afzal, A.; Iqbal, Z.; Ijaz, F.; Ali, N.; Asif, M.; Alam, J.; Majid, A.; Hart, R.; Bussmann, R.W. First insights into the floristic diversity, biological spectra and phenology of Manoor Valley, Pakistan. Pak. J. Bot. 2018, 50, 1113–1124. [Google Scholar]
- Majid, A.; Ahmad, H.; Saqib, Z.; Rahman, I.U.; Khan, U.; Alam, J.; Shah, A.H.; Jan, S.A.; Ali, N. Exploring threatened traditional knowledge; ethnomedicinal studies of rare endemic flora from Lesser Himalayan region of Pakistan. Rev. Bras. Farmacogn. 2019. [Google Scholar] [CrossRef]
- Malik, Z.A.; Bhat, J.A.; Ballabha, R.; Bussmann, R.W.; Bhatt, A. Ethnomedicinal plants traditionally used in health care practices by inhabitants of Western Himalaya. J. Ethnopharmacol. 2015, 172, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Khan, K.; Rahman, I.U.; Soares, E.C.; Ali, N.; Ijaz, F. Ethnoveterinary therapeutic practices and conservation status of the medicinal flora of Chamla Valley, Khyber Pakhtukhwa, Pakistan. Front. Vet. Sci. 2019, 6, 122. [Google Scholar] [CrossRef]
- Nasir, E.; Ali, S.I. Flora West of Pakistan; Department of Botany, University of Karachi, Karachi and National Herbarium: Islamabad, Pakistan, 1971–1989. [Google Scholar]
- Ali, S.I.; Qaiser, M. A phytogeographical analysis of the phanerogams of Pakistan and Kashmir. Proc. Roy. Soc. Edinb. B Boil. Sci. 1986, 89, 89–101. [Google Scholar] [CrossRef]
- Ali, S.I.; Qaiser, M. Flora of Pakistan; Department of Botany, University of Karachi: Karachi, Pakistan, 1995–2017. [Google Scholar]
- Phillips, O.L.; Hall, P.; Gentry, A.H.; Sawyer, S.A.; Vasquez, R. Dynamics and species richness of tropical rain forests. Proc. Natl. Acad. Sci. USA 1994, 91, 2805–2809. [Google Scholar] [CrossRef]
- Khan, K.U.; Shah, M.; Ahmad, H.; Ashraf, M.; Rahman, I.U.; Iqbal, Z.; Khan, S.M.; Majid, A. Investigation of Traditional Veterinary Phytomedicines Used in Deosai Plateau, Pakistan. Glob. Vet. 2015, 15, 381–388. [Google Scholar]
- Tardío, J.; Pardo-De-Santayana, M. Cultural Importance Indices: A Comparative Analysis Based on the Useful Wild Plants of Southern Cantabria (Northern Spain)1. Econ. Bot. 2008, 62, 24–39. [Google Scholar] [CrossRef]
- Alexiades, M.N. Collecting ethnobotanical data: An introduction to basic concepts and techniques. Adv. Econ. Bot. 1996, 10, 53–94. [Google Scholar]
- Sorensen, T.A. A method of establishing groups of equal amplitude in plant sociology based on similarity of species content, and its application to analyses of the vegetation on Danish commons. K. Danske Vidensk Selsk. Biol. Skr. 1948, 5, 1–34. [Google Scholar]
- Rahman, I.U.; Hart, R.; Afzal, A.; Iqbal, Z.; Ijaz, F.; Abd Allah, E.F.; Ali, N.; Khan, S.M.; Alqarawi, A.A.; Alsubeie, M.S.; et al. A new ethnobiological similarity index for the evaluation of novel use reports. Appl. Ecol. Environ. Res. 2019, 17, 2765–2777. [Google Scholar] [CrossRef]

| Gender | Local Inhabitants Age (years) | ||
|---|---|---|---|
| 21 to 40 | 41 to 60 | 61 to 80 | |
| Male | 21 | 14 | 7 |
| Female | 8 | 5 | 0 |
| Total | 29 | 19 | 7 |
| Scientific Name | Vernacular Name (Hindko) | Family | PH | PU | MU | UVi | RFCs | URs |
|---|---|---|---|---|---|---|---|---|
| Ajuga integrifolia Buch.-Ham. | Khauri buti | Lamiaceae | H | Wp | Diabetes | 0.78 | 0.45 | 25 |
| Bauhinia variegata L. | Kachnar | Fabaceae | T | R | Obesity | 0.82 | 0.42 | 23 |
| Cannabis sativa L. | Bhang | Cannabaceae | H | L | Warmness, insomnia | 0.97 | 0.58 | 32 |
| Cichorium intybus L. | Hand | Asteraceae | H | R | Typhoid fever | 0.86 | 0.55 | 30 |
| Convolvulus arvensis L. | Laili | Convolvulaceae | H | Wp | Diarrhea, dysentery | 0.63 | 0.35 | 19 |
| Dysphaniaambrosioides (L.) Mosyakin & Clemants | Baljawain | Chenopodiaceae | H | Sd | Fever | 0.46 | 0.22 | 12 |
| Indigofera heterantha Brandis | Kainthi | Fabaceae | S | R | Diuretic | 0.68 | 0.47 | 26 |
| Justicia adhatoda L. | Baiker | Acanthaceae | S | L, R | Throat infection, cough | 0.58 | 0.33 | 18 |
| Malva parviflora L. | Sounchal | Malvaceae | H | L | Gas trouble | 0.54 | 0.27 | 15 |
| Medicago sativa L. | Sengi | Fabaceae | H | L | Gas trouble | 0.80 | 0.51 | 28 |
| Mentha longifolia (L.) L. | Jangli podina | Lamiaceae | H | Wp | Abdominal pain, gas trouble | 0.90 | 0.65 | 36 |
| Mentha royleana Wall. ex Benth. | Safaid podina | Lamiaceae | H | L | Diarrhea, vomiting | 0.69 | 0.44 | 24 |
| Oxalis corniculata L. | Khati buti | Oxalidaceae | H | Wp | Vitamin C deficiency, mouth smell | 0.86 | 0.56 | 31 |
| Plantago major L. | Bartang | Plantaginaceae | H | Sd | Diarrhea, Obesity | 0.90 | 0.47 | 26 |
| Polygonum plebeium R.Br. | Rani pal | Polygonaceae | H | Wp | Cough | 0.45 | 0.25 | 14 |
| Portulaca oleracea L. | Lunak | Portulacaceae | H | L | Diuretic | 0.50 | 0.31 | 17 |
| Punica granatum L. | Daruna | Lythraceae | S | Fr | Gas troubles, indigestion | 0.81 | 0.55 | 30 |
| Ricinus communis L. | Arand | Euphorbiaceae | S | Sd | Constipation | 0.57 | 0.29 | 16 |
| Salvia moorcroftiana Wall. ex Benth. | Kaljari | Lamiaceae | H | L | Cough, diarrhea | 0.37 | 0.20 | 11 |
| Silybum marianum (L.) Gaertn. | Kandyara | Asteraceae | H | Sd | Liver problems | 0.52 | 0.31 | 17 |
| Taraxacum officinale F.H. Wigg. | Dhodal | Asteraceae | H | L | Diabetes | 0.76 | 0.51 | 28 |
| Trachyspermum amii (L.) Sprague | Ajwain | Apiaceae | H | Fr | Diuretic, kidney stone removal | 0.66 | 0.38 | 21 |
| Trifolium repens L. | Shaftal | Fabaceae | H | Wp | Fever | 0.63 | 0.44 | 24 |
| Verbascum thapsus L. | Gidar tambacu | Scrupholariaceae | H | L | Diarrhea | 0.45 | 0.24 | 13 |
| Vitex negundo L. | Marwani | Verbenaceae | S | L | Indigestion, stomachache, gas trouble | 0.59 | 0.36 | 20 |
| Xanthium strumarium L. | Katula | Asteraceae | S | Fr | Diuretic, kidney stone removal | 0.29 | 0.20 | 11 |
| Zanthoxylum armatum DC. | Timber | Rutaceae | S | Fr | Abdominal pain, indigestion | 0.69 | 0.44 | 24 |
| Botanical Name | Dosage | Traditional Folk Recipe |
|---|---|---|
| Ajuga integrifolia Buch.-Ham. | Drink twice a day (240 mL) | Fresh plant crushed and extract is taken. Mix 15 g powder in a glass of water. |
| Bauhinia variegata L. | Drink twice a day (240 mL) | Roots are shade dried and grinded. Mix 15 g powder in a glass of water. |
| Cannabis sativa L. | Drink once in a week (240 mL) | Fresh leaves are shade dried, and grinded powder (15 g) is mixed with almond and khaskhaas in milk. Mostly used in severe summer. This drink is locally named (Sardai). |
| Dysphania ambrosioides (L.) Mosyakin & Clemants | A cup of tea once in a day | Seeds are sun dried, boiled in water with sugar to make tea. |
| Cichorium intybus L. | Drink half cup before breakfast | Roots are dried and grinded. Mix 5 g of powder in 2 L of water and boiled for 2 h, placed for a night in open sky. |
| Convolvulus arvensis L. | Drink once in a day (240 mL) | Whole plant is sun dried and grinded. 15 g of powder is mixed in a glass of water or milk. |
| Indigofera heterantha Brandis | Drink twice a day (240 mL) | Root bark dried and powdered. 5 g of powder and sugar mixed with water to make drink. |
| Justicia adhatoda L. | Drink twice a day (240 mL) | Shade dried leaves and roots are grinded. The powdered material and sugar is used to make tea. |
| Malva parviflora L. | Drink twice a day (240 mL) | Leaves are shade dried and grinded. Powdered material and ginger powder is mixed in water and boiled with the addition of sugar to make tea. |
| Medicago sativa L. | Drink twice a day (240 mL) | Fresh leaves are boiled in water with ginger for half an hour to make tea. Sugar is added for taste. |
| Mentha longifolia (L.) L. | Drink twice a day (240 mL) | Shade dried leaves are used to make tea by adding sugar. |
| Mentha royleana Wall. ex Benth. | Drink twice a day (240 mL) | Leaves are shade dried and grinded. Powdered material is used to make tea by adding sugar. |
| Oxalis corniculata L. | Drink twice a day (240 mL) | Fresh leaves are boiled in water for 2 h and placed for cooling. |
| Plantago major L. | For diarrhea, drink twice a day (240 mL) and for obesity, drink before breakfast (240 mL) | Half boil a glass of milk with sugar. Then, add 30 g of seeds in it. This drink is for diarrhea. In water, 15 g of seeds are dipped and placed for whole night. Then, in early morning, it is mixed in a glass of water (clean). This drink is for reduction of obesity. |
| Polygonum plebeium R.Br. | Drink twice a day (240 mL) | Fresh plant is boiled in water for 2 h with the addition of sugar to make tea. |
| Portulaca oleracea L. | Drink twice a day (240 mL) | Fresh leaves are boiled in water for 1 h, sugar added to make tea. |
| Punica granatum L. | Drink after meal (240 mL) | Sundried fruit epicarp is grinded. Then, 3 g of powder is mixed with same amount of Citrus medica epicarp and 45 g of black salt. Put its 15 g to a glass of water for making a drink. |
| Ricinus communis L. | Drink once in a day (240 mL) | Oil is extracted from seeds and its 2 drops is mixed in a glass of milk. |
| Salvia moorcroftiana Wall. ex Benth. | Drink twice a day (240 mL) | Fresh leaves are sundried and grinded. Then, 15 g of powder and honey each is mixed in water. |
| Silybum marianum (L.) Gaertn. | Drink once in a day (240 mL) | Ripened seeds are sundried and powdered. The grinded material is mixed in water to make a drink. |
| Taraxacum officinale F.H. Wigg. | Drink once in a day (240 mL) | Fresh leaves are boiled in water till it becomes viscous. Then, add 5 mL of this liquid to a glass of fresh water for making a drink. |
| Trachyspermum amii (L.) Sprague | Drink twice a day (240 mL) | Fresh fruits are sundried and grinded. Then, 15 g of sugar and powder each is added to a glass of water. |
| Trifolium repens L. | Drink twice a day (240 mL) | Whole plant is boiled in water for an hour. Then, add 15 g of sugar and place it to cool. |
| Verbascum thapsus L. | Drink twice a day (240 mL) | Shade dried leaves are powdered. Then, 15 g of grinded material is added to a glass of water. |
| Vitex negundo L. | Drink once in a day (240 mL) | Fresh leaves are mashed, and extract is filtered. Then, 15 mL extract is added to a glass of water. |
| Xanthium strumarium L. | Drink twice a day (240 mL) | Fresh fruits are sundried and powdered. Then, 15 g of powder is mixed in a glass of water. |
| Zanthoxylum armatum DC. | Drink twice a day (240 mL) | Fresh fruits are sundried and powdered. Add 5 g in a glass of water. |
| A) Plants with High Fidelity Level and Reported for One Ailment (FL = 100%) |
| Diabetes |
| Ajuga integrifolia |
| Taraxacum officinale |
| Obesity |
| Bauhinia variegata |
| Fever |
| Dysphania ambrosioides |
| Trifolium repens |
| Typhoid fever |
| Cichorium intybus |
| Diuretic |
| Indigofera heterantha |
| Portulaca oleracea |
| Gas trouble |
| Malva parviflora |
| Medicago sativa |
| Cough |
| Polygonum plebeium |
| Constipation |
| Ricinus communis |
| Liver problem |
| Silybum marianum |
| Diarrhea |
| Verbascum thapsus |
| B) Plants Fidelity Level Reported with Most Cited Medicinal Uses |
| Warmness |
| Cannabis sativa (FL = 93.75%) |
| Diarrhea |
| Plantago major (FL = 92.31%) |
| Gas trouble |
| Mentha longifolia (FL = 88.89%) |
| Mouth smell |
| Oxalis corniculata (FL = 74.19%) |
| Vomiting |
| Mentha royleana (FL = 70.83%) |
| Dysentery |
| Convululus arvensis (FL = 68.42%) |
| Diuretic |
| Trachyspermum amii (FL = 66.67%) |
| Xanthium strumarium (FL = 63.64%) |
| Throat infection |
| Justicia adhatoda (FL = 61.11%) |
| Indigestion |
| Zanthoxylum armatum (FL = 62.50%) |
| Punica granatum (FL = 60%) |
| Cough |
| Salvia moorcroftiana (FL = 54.55%) |
| Gas trouble |
| Vitex negundo (FL = 45%) |
| Botanical Name | Similar Uses from Literature | Dissimilar Uses from Literature | Literature Comparison |
|---|---|---|---|
| Ajuga integrifolia Buch.-Ham. | NR | Jaundice, hypertension 5,12, malarial fever 5, abdominal pain 7, tonic, dental, hepatic stimulant 11, throat sore, colic, purifying blood, epilepsy 12 | 5●, 7●, 11●, 12● |
| Bauhinia variegata L. | Fatness 14 | Anthelmintic, tonic, astringent, skin diseases, ulcer, scrofula 4, fuel wood 4,8, fodder, vegetable, skin diseases, leprosy, ornamental 8, gastrointestinal problems 18 | 4●, 8●, 14●, 18● |
| Cannabis sativa L. | Cold drink (Tandai) for Warmness 12 | Bowels, dyspepsia, gonorrhea, tonic 3, sedative 3,5, anodyne, anti-lice 5, appetite, abdominal swelling 7, narcotic 3,5,17, anti-diarrheal, stimulant 17, stomachache 18 | 3●, 5●, 7●, 12■, 17●, 18● |
| Dysphania ambrosioides (L.) Mosyakin & Clemants | NR | Piles, stomach problems 5 | 5● |
| Cichorium intybus L. | NR | Bile secretion, digestion, stomachache, tonic, carminative, cordial, obstructed, menstrual disorder, dropsy 3, fever 12 | 3●, 12■ |
| Convolvulus arvensis L. | NR | Bowels 2, brain tonic, diuretic, sedative, anti-septic, skin diseases 3,5, stomach problems 5, constipation 7, skin problems 12, purgative 2,3,5,12, anthelmintic, galactagogue 17 | 2●, 3●, 5●, 7●, 12●, 17●, |
| Indigofera heterantha Brandis | NR | Hepatitis, whooping cough, blackening of hairs 2, fuelwood 4, scabies, stomach problems 12, stomach problems 14 | 2●, 4●, 12●, 14● |
| Justicia adhatoda L. | Throat infection 3,4,14, cough 20 | NR | 3■, 4■, 14■, 20■ |
| Malva parviflora L. | NR | Cold, cough, sore throat, blocked nose 17 | 17● |
| Medicago sativa L. | NR | NR | |
| Mentha longifolia (L.) L. | Gas expeller 2, stomach problem 6, abdominal pain 19 | Aromatic, stomachache, stimulant, mouthwash, vomiting 5 | 2■, 5●, 6■, 19■ |
| Mentha royleana Wall. ex Benth. | Vomiting, diarrhea 2, 12 | NR | 2■, 12■ |
| Oxalis corniculata L. | Mouth smell 14 | Anti-septic, skin curing, stomach troubles, cleaning rusted vessel 3,5, digestion 12, food 16 | 3●, 5●, 12●, 14■, 16● |
| Plantago major L. | NR | Constipation, intestinal problems 5, infected hooves 7, bedsores, candidiasis 12 | 2●, 5●, 6●, 7●, 12●, |
| Polygonum plebeium R.Br. | Cough 14 | Pneumonia, bowels 5 | 2●, 5●, 14■ |
| Portulaca oleracea L. | NR | Liver 12, kidney diseases 12,14, abdominal pain, diabetes, asthma 14 | 12●, 14● |
| Punica granatum L. | NR | Dysentery 7,8,13,18, cough 8,12,17, fuel wood, tonic, anthelmintic 8,12, skin diseases 13, heart palpitation, blood pressure 14, food 16. cold, flu, nasal decongestant 17, diarrhoea 18 | 7●, 9●, 12●, 13●, 14●, 16●, 17●, 18● |
| Ricinus communis L. | Constipation 1,5,7 | Purgative, lubricant 3, bowels 12, rheumatic joints, swellings, inflamed muscle, toothache 13, purgative, anti-flatulent, anti-inflammatory, analgesic 17, laxative, diarrhoea 18, leg sore, piles, edema 20 | 1■, 3■, 5■, 7■, 12●, 13●, 17●, 18●, 20● |
| Salvia moorcroftiana Wall. ex Benth. | Liver problems 3 | Abscesses, dysentery, colic 2, wounds healing 12, white juicy part of stem as food 16 | 2●, 12●, 16● |
| Silybum marianum (L.) Gaertn. | Jaundice, hepatitis, cirrhosis 1 | NR | 1■, 3■ |
| Taraxacum officinale F.H. Wigg. | NR | Hepatitis, appetite 1, urination, kidney disorders 2, tonic 2,6, diuretic, laxative, anti-inflammatory, digestive disorders 6 | 1●, 2●, 6● |
| Trachyspermum amii (L.) Sprague | NR | Appetite stimulant, galactagogue 7 | 7● |
| Trifolium repens L. | NR | Worms removal 2 | 2● |
| Verbascum thapsus L. | Diarrhea 3,5,7,14 | Respiratory tract infection, ear infection, dry cough 1, aphrodisiac, skin problems, irritability 2 | 1●, 2●, 3■, 5■, 7■, 14■ |
| Vitex negundo L. | Gas troubles 14 | Aromatic, tonic, febrifuge, diuretic, anthelmintic, headache, fuel wood 8, chest pain 13, skin problems, child crying, snake bite 20 | 9●, 13●, 14■, 20● |
| Xanthium strumarium L. | NR | Skin problems 5, malarial fever 5,14, carminative 14 | 5●, 12●, 14● |
| Zanthoxylum armatum DC. | NR | Vomiting, indigestion 7, fuel wood, digestion, aromatic, condiment, gum diseases 8, carminative, pile 8,13, malarial fever, antipyretic 12, stomachache 12,13, fever, cholera 13 | 7●, 8●, 12●, 13● |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rahman, I.U.; Afzal, A.; Iqbal, Z.; Hart, R.; Abd_Allah, E.F.; Hashem, A.; Alsayed, M.F.; Ijaz, F.; Ali, N.; Shah, M.; et al. Herbal Teas and Drinks: Folk Medicine of the Manoor Valley, Lesser Himalaya, Pakistan. Plants 2019, 8, 581. https://doi.org/10.3390/plants8120581
Rahman IU, Afzal A, Iqbal Z, Hart R, Abd_Allah EF, Hashem A, Alsayed MF, Ijaz F, Ali N, Shah M, et al. Herbal Teas and Drinks: Folk Medicine of the Manoor Valley, Lesser Himalaya, Pakistan. Plants. 2019; 8(12):581. https://doi.org/10.3390/plants8120581
Chicago/Turabian StyleRahman, Inayat Ur, Aftab Afzal, Zafar Iqbal, Robbie Hart, Elsayed Fathi Abd_Allah, Abeer Hashem, Mashail Fahad Alsayed, Farhana Ijaz, Niaz Ali, Muzammil Shah, and et al. 2019. "Herbal Teas and Drinks: Folk Medicine of the Manoor Valley, Lesser Himalaya, Pakistan" Plants 8, no. 12: 581. https://doi.org/10.3390/plants8120581
APA StyleRahman, I. U., Afzal, A., Iqbal, Z., Hart, R., Abd_Allah, E. F., Hashem, A., Alsayed, M. F., Ijaz, F., Ali, N., Shah, M., Bussmann, R. W., & Calixto, E. S. (2019). Herbal Teas and Drinks: Folk Medicine of the Manoor Valley, Lesser Himalaya, Pakistan. Plants, 8(12), 581. https://doi.org/10.3390/plants8120581