Ethnomedicinal Plants in Herbal Remedies Used for Treatment of Skin Diseases by Traditional Healers in Songkhla Province, Thailand
Abstract
:1. Introduction
2. Results and Discussion
2.1. Socio-Demographic Characteristics of Informants
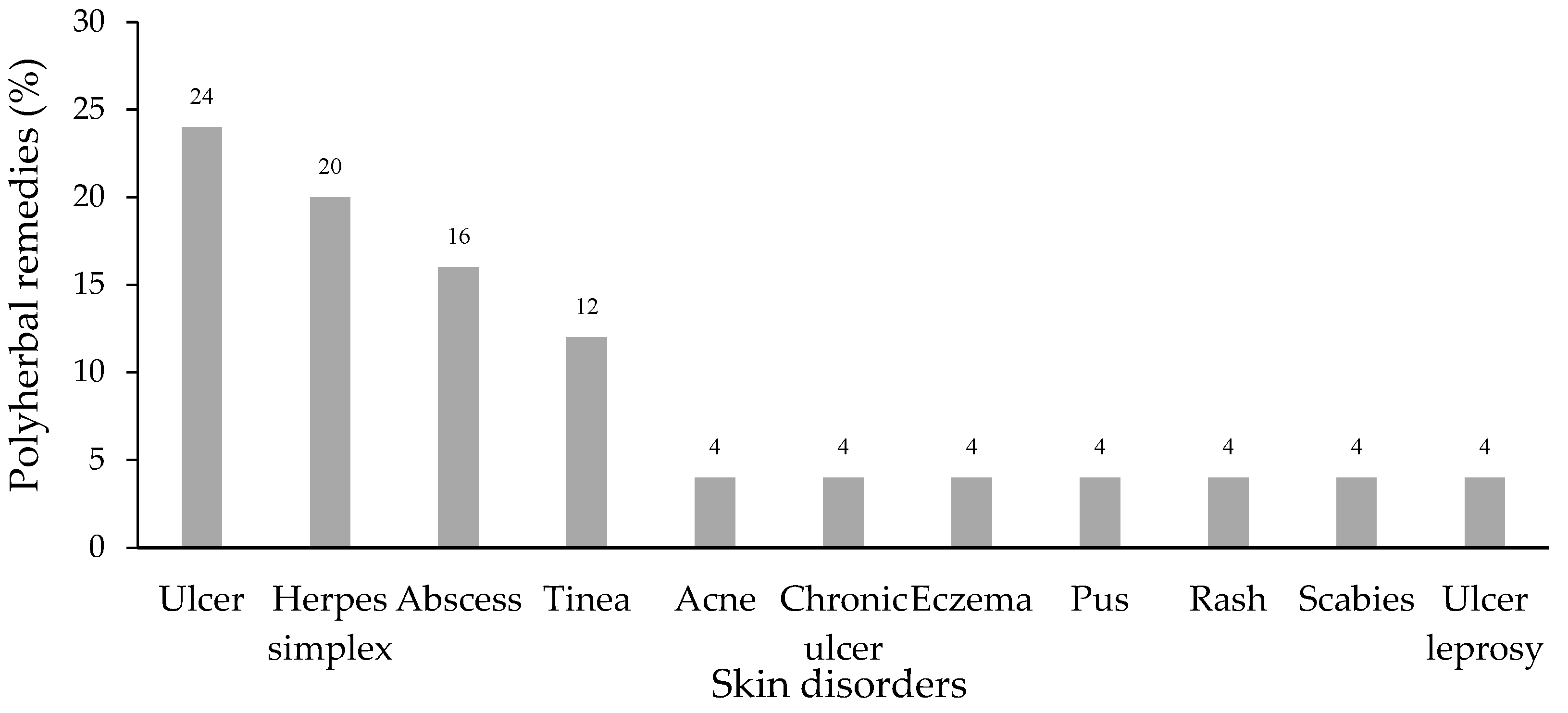
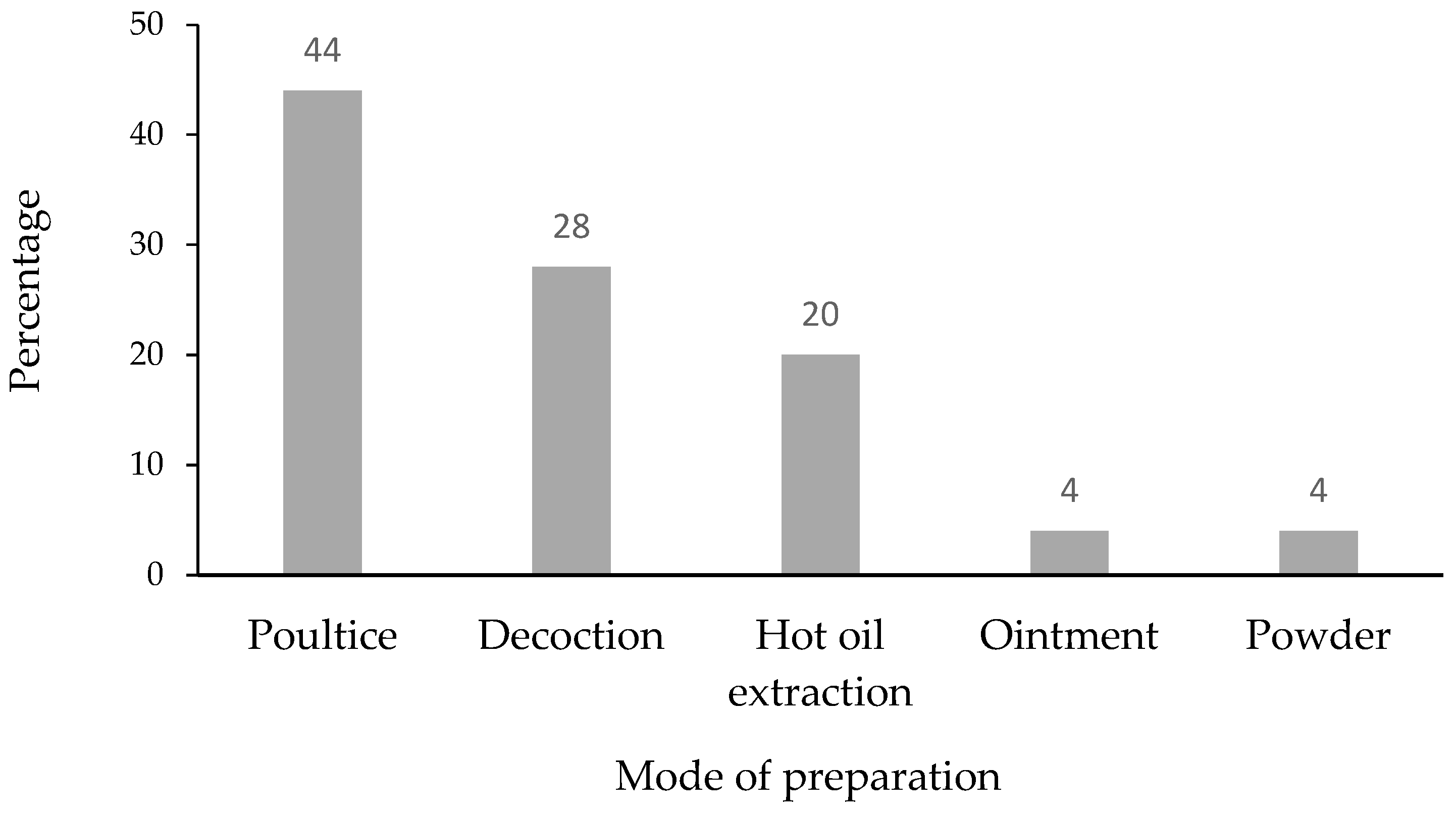
2.2. Prescriptions of Polyherbal Remedies Applied for the Treatment of Skin Diseases
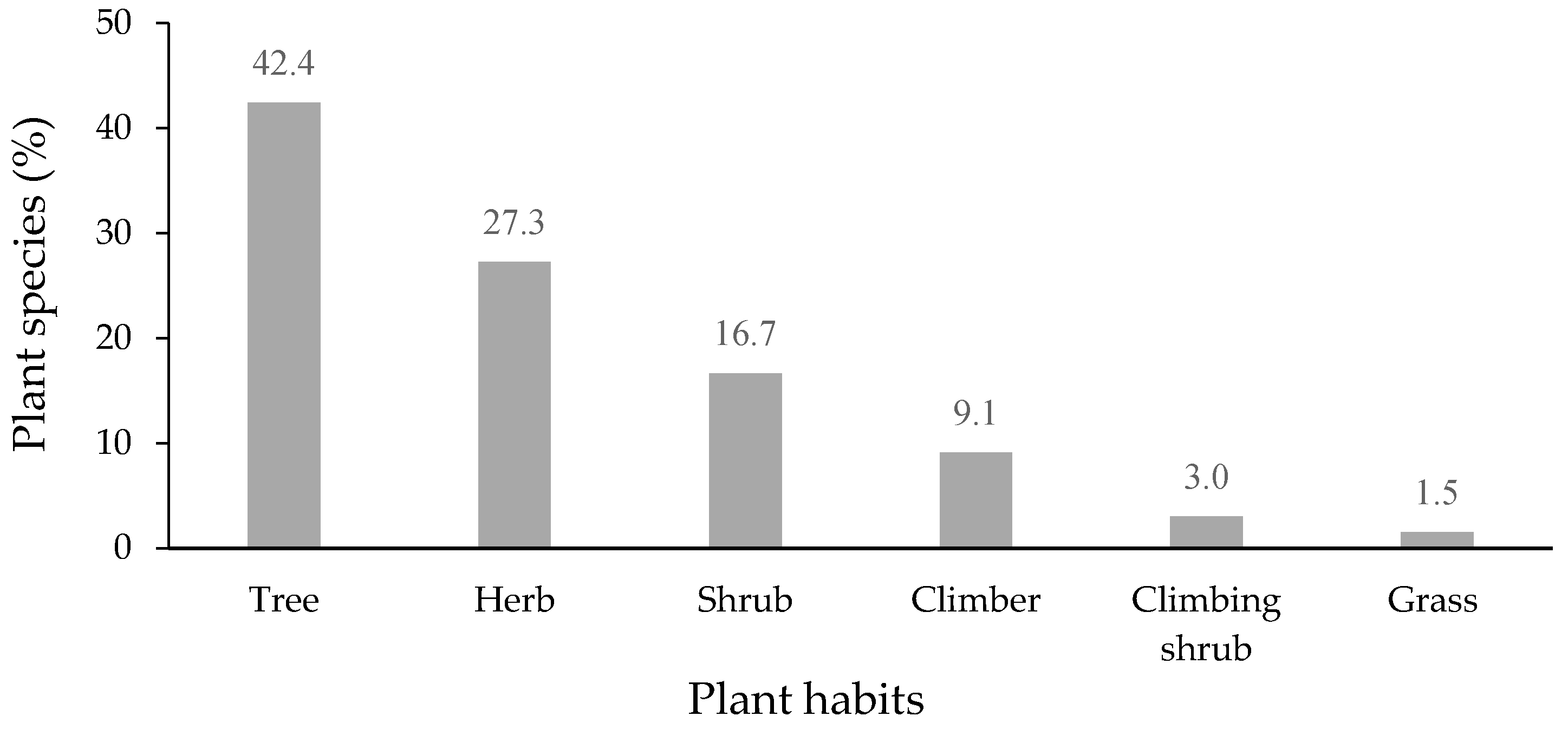
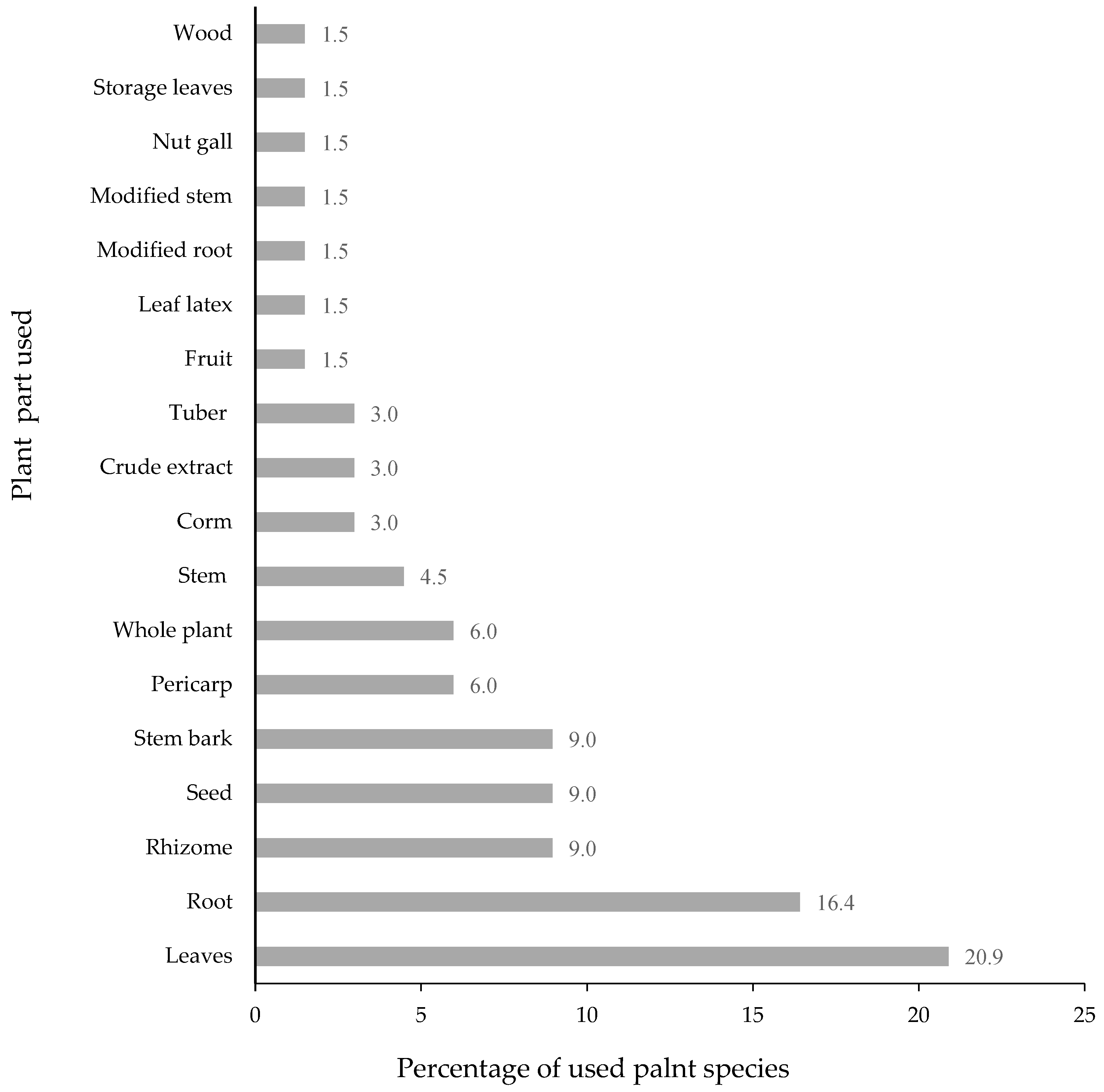
2.3. The Habits of Medicinal Plants and the Plant Part Used
2.4. A Variety of Plant Materials Used in Polyherbal Remedies for Skin Disorders
2.5. Preferred Plants Used in Polyherbal Recipes for Skin Disorder Treatment
3. Methods
3.1. Study Area
3.2. Informants
3.3. Ethnobotanical Data Collection
3.4. Data Analysis
3.5. Use Value (UV)
3.6. Relative Frequency of Citation (RFC)
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhang, X.J.; Wang, A.P.; Shi, T.Y.; Zhang, J.; Xu, H.; Wang, D.Q.; Feng, L. The psychosocial adaptation of patients with skin disease: A scoping review. BMC Public Health 2019, 19, 1404. [Google Scholar] [CrossRef] [PubMed]
- Hay, R.J.; Augustin, M.; Griffiths, C.E.M.; Sterry, W. The global challenge for skin health. Br. J. Dermatol. 2015, 172, 1469–1472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dawson, A.L.; Dellavalle, R.P.; Elston, D.M. Infectious skin diseases: A review and needs assessment. Dermatol. Clin. 2012, 30, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Li, V.C.; Chowdhury, M.M. Dermatological pharmacology: Topical agents. Medicine 2017, 45, 359–362. [Google Scholar] [CrossRef]
- Yuan, H.; Ma, Q.; Ye, L.; Piao, G. The Traditional medicine and modern medicine from natural products. Molecules 2016, 21, 559. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, V.A.; Patel, P.M.; Wilson, C.; Wang, H.; Ashack, K.A. Complementary and alternative medicine treatments for common skin diseases: A systematic review and meta-analysis. JAAD Int. 2021, 2, 76–93. [Google Scholar] [CrossRef]
- Tabassum, N.; Hamdani, M. Plants used to treat skin diseases. Pharmacogn. Rev. 2014, 8, 52–60. [Google Scholar] [CrossRef] [Green Version]
- Malik, K.; Ahmad, M.; Zafar, M.; Ullah, R.; Mahmood, H.M.; Parveen, B.; Rashid, N.; Sultana, S.; Shah, S.N. An ethnobotanical study of medicinal plants used to treat skin diseases in northern Pakistan. BMC Complement. Altern. Med. 2019, 19, 210. [Google Scholar] [CrossRef] [Green Version]
- Hussein, R.A.; El-Anssary, A.A. Plants secondary metabolites: The key drivers of the pharmacological actions of medicinal plants. In Herbal Medicine; Builders, P.F., Ed.; IntechOpen: London, UK, 2019; pp. 11–30. [Google Scholar] [CrossRef]
- Zaid, N.A.M.; Sekar, M.; Bonam, S.R.; Gan, S.H.; Lum, P.T.; Begum, M.Y.; Rani, N.N.I.M.; Vaijanathappa, J.; Wu, Y.S.; Subramaniyan, V.; et al. Promising natural products in new drug design, development, and therapy for skin disorders: An overview of scientific evidence and understanding their mechanism of action. Drug Des. Dev. Ther. 2020, 16, 23–66. [Google Scholar] [CrossRef]
- Maneenoon, K.; Khuniad, C.; Teanuan, Y.; Saedan, N.; Prom-In, S.; Rukleng, N.; Kongpool, W.; Pinsook, P.; Wongwiwat, W. Ethnomedicinal plants used by traditional healers in Phatthalung Province, Peninsular Thailand. J. Ethnobiol. Ethnomed. 2015, 11, 43. [Google Scholar] [CrossRef] [Green Version]
- Neamsuvan, O.; Komonhiran, P.; Boonming, K. Medicinal plants used for hypertension treatment by folk healers in Songkhla province, Thailand. J. Ethnopharmacol. 2018, 214, 58–70. [Google Scholar] [CrossRef] [PubMed]
- Neamsuvan, O.; Madeebing, N.; Mah, L.; Lateh, W. A survey of medicinal plants for diabetes treating from Chana and Nathawee district, Songkhla province, Thailand. J. Ethnopharmacol. 2015, 174, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Neamsuvan, O.; Sengnona, N.; Seemaphrika, N.; Chouychooa, M.; Rungrata, R.; Sujittra, B. Survey of medicinal plants around upper Songkhla lake, Thailand. Afr. J. Tradit. Complement. Altern. Med. 2015, 12, 133–143. [Google Scholar] [CrossRef] [Green Version]
- Neamsuvan, O.; Bunmee, P. A survey of herbal weeds for treating skin disorders from southern Thailand: Songkhla and Krabi province. J. Ethnopharmacol. 2016, 193, 574–585. [Google Scholar] [CrossRef]
- World Health Organization. Regional Office for South-East Asia. Traditional Herbal Remedies for Primary Health Care; WHO Regional Office for South-East Asia: New Delhi, India, 2010; pp. 1–167. ISBN 978-92-9022-382-5. [Google Scholar]
- Neamsuvan, O.; Phumchareon, T.; Bunphan, W.; Kaosaeng, W. Plant materials for gastrointestinal diseases used in Chawang district, Nakhon Si Thammarat province, Thailand. J. Ethnopharmacol. 2016, 194, 179–187. [Google Scholar] [CrossRef]
- Asong, J.; Ndhlovu, P.; Khosana, N.; Aremu, A.; Otang-Mbeng, W. Medicinal plants used for skin-related diseases among the Batswanas in Ngaka Modiri Molema District Municipality, South Africa. S. Afr. J. Bot. 2019, 126, 11–20. [Google Scholar] [CrossRef]
- Salhi, N.; Bouyahya, A.; Fettach, S.; Zellou, A.; Cherrah, Y. Ethnopharmacological study of medicinal plants used in the treatment of skin burns in occidental Morocco (area of Rabat). S. Afr. J. Bot. 2019, 121, 128–142. [Google Scholar] [CrossRef]
- Alamgeer; Sharif, A.; Asif, H.; Younis, W.; Riaz, H.; Bukhari, I.A.; Assiri, A.M. Indigenous medicinal plants of Pakistan used to treat skin diseases: A review. Chin. Med. 2018, 13, 52. [Google Scholar] [CrossRef] [Green Version]
- Chotchoungchatchai, S.; Saralamp, P.; Jenjittikul, T.; Pornsiripongse, S.; Prathanturarug, S. Medicinal plants used with Thai traditional medicine in modern healthcare services: A case study in Kabchoeng Hospital, Surin Province, Thailand. J. Ethnopharmacol. 2012, 141, 193–205. [Google Scholar] [CrossRef]
- Kesornmas, S.; Nakthaworn, K.; Musikapong, K.; Viriyabubpa, C. A Study on the treatment with herbal remedies in seven groups of diseases: A case study of Mr. Prawit Kaewthong, Songkhla Province. J. Tradit. Thai Altern. Med. 2019, 17, 263–279. [Google Scholar]
- Palungwachira, P.; Tancharoen, S.; Phruksaniyom, C.; Klungsaeng, S.; Srichan, R.; Kikuchi, K.; Nararatwanchai, T. Antioxidant and anti-inflammatory properties of anthocyanins extracted from Oryza sativa L. in primary dermal fibroblasts. Oxid. Med. Cell Longev. 2019, 2019, 2089817. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amber, R.; Adnan, M.; Tariq, A.; Khan, S.N.; Mussarat, S.; Hashem, A.; Al-Huqail, A.A.; Al-Arjani, A.F.; Abd Allah, E.F. Anti-bacterial activity of selected medicinal plants of northwest Pakistan traditionally used against mastitis in livestock. Saudi J. Biol. Sci. 2018, 25, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Gu, C.Z.; Xia, X.M.; Lv, J.; Tan, J.W.; Baerson, S.R.; Pan, Z.Q.; Song, Y.Y.; Zeng, R.S. Diterpenoids with herbicidal and antifungal activities from hulls of rice (Oryza sativa). Fitoterapia 2019, 136, 104183. [Google Scholar] [CrossRef] [PubMed]
- Aoki, H.; Akaike, T.; Abe, K.; Kuroda, M.; Arai, S.; Okamura, R.; Negi, A.; Maeda, H. Antiviral effect of oryzacystatin, a proteinase inhibitor in rice, against herpes simplex virus type 1 in vitro and in vivo. Antimicrob. Agents Chemother. 1995, 39, 846–849. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manosroi, J.; Chankhampan, C.; Kitdamrongtham, W.; Zhang, J.; Abe, M.; Akihisa, T.; Manosroi, W.; Manosroi, A. In vivo anti-ageing activity of cream containing niosomes loaded with purple glutinous rice (Oryza sativa Linn.) extract. Int. J. Cosmet. Sci. 2020, 42, 622–631. [Google Scholar] [CrossRef] [PubMed]
- Ampawong, S.; Kengkoom, K.; Sukphopetch, P.; Aramwit, P.; Muangkaew, W.; Kanjanapruthipong, T.; Buaban, T. Evaluating the effect of rice (Oryza sativa L.: SRNC05053-6-2) crude extract on psoriasis using in vitro and in vivo models. Sci. Rep. 2020, 10, 17618. [Google Scholar] [CrossRef]
- Majaw, S.; Moirangthem, J. Qualitative and Quantitative Analysis of Clerodendron colebrookianum Walp. Leaves and Zingiber cassumunar Roxb. Rhizomes. Ethnobot. Leafl. 2009, 13, 578–589. [Google Scholar]
- Joram, A.; Das, A.K.; Mahanta, D. Evaluation of antioxidant and phenolic contents of Zingiber montanum (J. Koenig) Link ex Dietr.: A potential ethomedicinal plant of Arunachal Pradesh, India. Pleione 2018, 12, 255–264. [Google Scholar] [CrossRef]
- Verma, R.S.; Joshi, N.; Padalia, R.C.; Singh, V.R.; Goswami, P.; Verma, S.K.; Iqbal, H.; Chanda, D.; Verma, R.K.; Darokar, M.P.; et al. Chemical composition and antibacterial, antifungal, allelopathic and acetylcholinesterase inhibitory activities of cassumunar-ginger. J. Sci. Food Agric. 2018, 98, 321–327. [Google Scholar] [CrossRef]
- Siddique, H.; Pendry, B.; Rahman, M.M. Terpenes from Zingiber montanum and their screening against multi-drug resistant and methicillin resistant Staphylococcus aureus. Molecules 2019, 24, 385. [Google Scholar] [CrossRef] [Green Version]
- Liu, W.Y.; Tzeng, T.-F.; Liu, I.-M. Healing potential of zerumbone ointment on experimental full-thickness excision cutaneous wounds in rat. J. Tissue Viability 2017, 26, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Jamir, K.; Seshagirirao, K. Purification, biochemical characterization and antioxidant property of ZCPG, a cysteine protease from Zingiber montanum rhizome. Int. J. Biol. Macromol. 2018, 106, 719–729. [Google Scholar] [CrossRef] [PubMed]
- Jamir, K.; Ganguly, R.; Seshagirirao, K. ZCPG, a cysteine protease from Zingiber montanum rhizome exhibits enhanced anti-inflammatory and acetylcholinesterase inhibition potential. Int. J. Biol. Macromol. 2020, 163, 2429–2438. [Google Scholar] [CrossRef] [PubMed]
- Oeung, S.; Nov, V.; Ung, H.; Roum, K.; Yin, V.; Keo, S.; Chea, S. Phytochemical analysis of different extracts of leaves of Nicotiana tabacum L. of Cambodia. Asian J. Pharmacogn. 2017, 1, 18–26. [Google Scholar]
- Ameya, G.; Manilal, A.; Merdekios, B. In vitro antibacterial activity and phytochemical analysis of Nicotiana tabacum L. extracted in different organic solvents. Open Microbiol. J. 2017, 11, 352–359. [Google Scholar] [CrossRef]
- Shang, S.Z.; Zhao, W.; Tang, J.G.; Xu, X.M.; Sun, H.D.; Pu, J.X.; Liu, Z.H.; Miao, M.M.; Chen, Y.K.; Yang, G.Y. Antiviral sesquiterpenes from leaves of Nicotiana tabacum. Fitoterapia 2016, 108, 1–4. [Google Scholar] [CrossRef]
- Itankar, P.; Murkute, A.V. Evaluation of in vitro antidandruff activity of biotransformed material (extract) of Nicotiana tabacum leaves. J. Nat. Remedies 2015, 15, 65–70. [Google Scholar] [CrossRef]
- Araújo, C.A.C.; Leon, L.L. Biological activities of Curcuma longa L. Mem. Inst. Oswaldo. Cruz. 2001, 96, 723–728. [Google Scholar] [CrossRef]
- Kasai, H.; Yamane, Y.; Ikegami-Kawai, M.; Sudo, H. Analysis of compounds of Curcuma rhizome using mass spectrometry and investigation of the antioxidant activity of rhizome extracts. Med. Aromat. Plants 2019, 8, 336. [Google Scholar]
- Zandia, K.; Ramedania, E.; Mohammadi, K.; Tajbakhsh, S.; Deilami, I.; Rastian, Z.; Fouladvand, M.; Yousefi, F.; Farshadpour, F. Evaluation of antiviral activities of curcumin derivatives against HSV-1 in Vero cell line. Nat. Prod. Commun. 2010, 5, 1935–1938. [Google Scholar] [CrossRef] [Green Version]
- Purohit, S.K.; Solanki, R.; Mathur, V.; Mathur, M. Evaluation of wound healing activity of ethanolic extract of Curcuma longa rhizomes in male albino rats. Asian J. Pharm. Res. 2013, 3, 79–81. [Google Scholar]
- Varghese, C.P.; Ambrose, C.; Jin, S.C.; Lim, Y.J.; Keisaban, T. Antioxidant and anti-inflammatory activity of Eurycoma longifolia Jack, a traditional medicinal plant in Malaysia. Int. J. Pharm. Sci. Nanotechnol. 2013, 5, 1875–1878. [Google Scholar] [CrossRef]
- Khanam, Z.; Wen, C.S.; Bhat, I.U.H. Phytochemical screening and antimicrobial activity of root and stem extracts of wild Eurycoma longifolia Jack (Tongkat Ali). J. King Saud Univ. Sci. 2015, 27, 23–30. [Google Scholar] [CrossRef] [Green Version]
- Tung, N.H.; Uto, T.; Hai, N.T.; Li, G.; Shoyama, Y. Quassinoids from the root of Eurycoma longifolia and their antiproliferative activity on human cancer cell lines. Pharmacogn. Mag. 2017, 13, 459–462. [Google Scholar] [PubMed]
- Pham, T.V.; Bach, H.K.T.; Ho, D.V.; Nguyen, B.C. Chemical constituents from the Knema globularia fruits and their in vitro cytotoxicity. Nat. Prod. Res. 2020, 36, 256–262. [Google Scholar] [CrossRef] [PubMed]
- Sriphana, U.; Yenjai, C.; Suthiwong, J.; Poopasit, K. A new diarylhexane and two new diarylpropanols from the roots of Knema globularia. Nat. Prod. Res. 2020. [Google Scholar] [CrossRef]
- Chuenban, C.; Sombatsri, A.; Sribuhom, T.; Pornchoo, C.; Prawan, A.; Tontapha, S.; Amornkitbamrung, V.; Yenjai, C. Knecorticosanones C–H from the fruits of Knema globularia (Lam.) warb. RSC Adv. 2021, 11, 4097–4103. [Google Scholar] [CrossRef]
- Mehta, J.P.; Parmar, P.H.; Kukadiya, N.B.; Godhani, D.R. Antimicrobial assay of extracts of Cassia Siamea (Lam.) and Cassia Javanica (Linn.). J. Pharm. Chem. Biol. Sci. 2018, 5, 386–395. [Google Scholar]
- Nas, F.; Oyeyi, T.; Ali, M. Antibacterial efficacy and phytochemical screening of Senna siamea leaves extracts on some pathogenic bacteria. J. Microbiol. Exp. 2018, 6, 159–163. [Google Scholar]
- Nsonde Ntandou, G.F.; Etou Ossibi, A.W.; Elion Itou, R.D.G.; Boumba, S.L.; Ouamba, J.M.; Abena, A.A. Laxative, antiinflammatory and analgesic effects of Cassia Siamea Lam (Fabaceae) leaves aqueous extract. IOSR J. Pharm. Biol. Sci. 2018, 13, 6–15. [Google Scholar]
- Tungcharoen, P.; Sudsai, T.; Leejae, S.; Wattanapiromsakul, C.; Tansakul, P.; Tewtrakul, S. Wound healing activity of Curcuma zedoaroides. Songklanakarin J. Sci. Technol. 2016, 38, 621–630. [Google Scholar]
- Fox, L.T.; Mazumder, A.; Dwivedi, A.; Gerber, M.; du Plessis, J.; Hamman, J.H. In vitro wound healing and cytotoxic activity of the gel and whole-leaf materials from selected aloe species. J. Ethnopharmacol. 2017, 200, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Siriwattanasatorn, M.; Itharat, A.; Thongdeeying, P.; Ooraikul, B. In Vitro Wound healing activities of three most commonly used Thai medicinal plants and their three markers. Evid. Based Complement. Altern. Med. 2020, 2020, 6795383. [Google Scholar] [CrossRef] [PubMed]
- Amal, B.; Veena, B.; Jayachandran, V.P.; Shilpa, J. Preparation and characterization of Punica granatum pericarp aqueous extract loaded chitosan-collagen-starch membrane: Role in wound healing process. J. Mater. Sci. Mater. Med. 2015, 26, 181. [Google Scholar] [CrossRef]
- Chokpaisarn, J.; Chusri, S.; Voravuthikunchai, S. Clinical randomized trial of topical Quercus infectoria ethanolic extract for the treatment of chronic diabetic ulcers. J. Herb. Med. 2020, 21, 100301. [Google Scholar] [CrossRef]
- Arcueno, R.O.; Retumban, J.L.B.; Echano, J.E.; Guerrero, J.J.G. Wound healing potential of Tinospora Crispa (Willd.) Miers [Menispermaceae] stem on diabetic mice. J. Med. Plants Stud. 2015, 3, 106–109. [Google Scholar]
- Rahman, H.; Eswaraiah, M.C.; Dutta, M. In-vitro Anti-inflammatory and anti-arthritic activity of Oryza sativa Var. Joha rice (An aromatic indigenous rice of Assam). Am. Eurasian J. Agric. Environ. Sci. 2015, 15, 115–121. [Google Scholar]
- Al-Amin, M.; Sultana, G.N.; Hossain, C.F. Antiulcer principle from Zingiber montanum. J. Ethnopharmacol. 2012, 141, 57–60. [Google Scholar] [CrossRef]
- Al-Amin, M.; Eltayeb, N.M.; Hossain, C.F.; Khairuddean, M.; Fazalul Rahiman, S.S.; Salhimi, S.M. Inhibitory activity of extract, fractions, and compounds from Zingiber montanum rhizomes on the migration of breast cancer cells. Planta Med. 2020, 86, 387–394. [Google Scholar] [CrossRef]
- Anumudu, C.; Nwachukwu, M.; Obasi, C.; Nwachukwu, I.; Ihenetu, F. Antimicrobial activities of extracts of tobacco leaf (Nicotiana tabacum) and its grounded snuff (Utaba) on Candida albicans and Streptococcus pyogenes. J. Trop. Dis. 2019, 7, 300. [Google Scholar]
- Ru, Q.M.; Wang, L.J.; Li, W.M.; Wang, J.L.; Ding, Y.T. In vitro antioxidant properties of flavonoids and polysaccharides extract from tobacco (Nicotiana tabacum L.) leaves. Molecules 2012, 17, 11281–11291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vaziri, S.; Mojarrab, M.; Farzaei, M.H.; Najafi, F.; Ghobadi, A. Evaluation of anti-aphthous activity of decoction of Nicotiana tabacum leaves as a mouthwash: A placebo-controlled clinical study. J. Tradit. Chin. Med. 2016, 36, 160–164. [Google Scholar] [CrossRef] [Green Version]
- Gupta, A.; Mahajan, S.; Sharma, R. Evaluation of antimicrobial activity of Curcuma longa rhizome extract against Staphylococcus aureus. Biotechnol. Rep. 2015, 6, 51–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, C.; Long, L.; Zhang, F.; Chen, Q.; Yu, X.; Liu, Q.; Bao, J.; Long, Z. Antifungal activity, main active components and mechanism of Curcuma longa extract against Fusarium graminearum. PLoS ONE 2018, 13, e0194284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ichsyani, M.; Ridhanya, A.; Risanti, M.; Desti, H.; Ceria, R.; Putri, D.; Sudiro, T.; Dewi, B. Antiviral effects of Curcuma longa L. against dengue virus in vitro and in vivo. IOP Conf. Ser. Earth Environ. Sci. 2017, 101, 012005. [Google Scholar] [CrossRef] [Green Version]
- Savaringal, J.P.; Lally, M.S. Anti-inflammatory effect of rhizome of Curcuma longa Linn, in albino rats by the method of carrageenin induced paw oedema. Int. J. Basic Clin. Pharmacol. 2018, 7, 229–233. [Google Scholar] [CrossRef] [Green Version]
- Stasiłowicz, A.; Tykarska, E.; Lewandowska, K.; Kozak, M.; Miklaszewski, A.; Kobus-Cisowska, J.; Szymanowska, D.; Plech, T.; Jenczyk, J.; Cielecka-Piontek, J. Hydroxypropyl-β-cyclodextrin as an effective carrier of curcumin-piperine nutraceutical system with improved enzyme inhibition properties. J. Enzyme Inhib. Med. Chem. 2020, 35, 1811–1821. [Google Scholar] [CrossRef]
- Alloha, I.B.; Aziz, N.A.L.B.; Faisal, G.G.; Abllah, Z.; Arzmi, M.H. Effects of Eurycoma Longifolia Jack (Tongkat Ali) alcoholic root extract against oral pathogens. Pharmacog. J. 2019, 11, 1299–1302. [Google Scholar] [CrossRef] [Green Version]
- Wan Hassan, W.N.A.; Zulkifli, R.M.; Ahmad, F.; Yunus, M.A.C. Antioxidant and tyrosinase inhibition activities of Eurycoma longifolia and Swietenia macrophylla. J. Appl. Pharm. Sci. 2015, 5, 6–10. [Google Scholar] [CrossRef] [Green Version]
- Phaiphan, A.; Baharin, B.S.; Tan, C.P.; Rahman, R.A.; Ganesan, P. Antioxidant and antibacterial activities of different solvent extractions from Cassia siamea (Lamk.) leaves. J. Chem. Pharm. 2014, 6, 655–662. [Google Scholar]
- Islam, M.; Hoshen, A.; Ayshasiddeka; Islam, F.; Yeasmin, T. Antimicrobial, membrane stabilizing and thrombolytic activities of ethanolic extract of Curcuma zedoaria Rosc. rhizome. J. Pharmacogn. Phytochem. 2017, 6, 38–41. [Google Scholar]
- Chachad, D.P.; Talpade, M.B.; Jagdale, S.P. Antimicrobial activity of rhizomes of Curcuma zedoaria Rosc. Int. J. Sci. Res. 2016, 5, 938–940. [Google Scholar]
- Huang, S.J.; Chyau, C.C.; Tsai, C.H.; Chen, C.C.; Mau, J.L.; Tsai, S.Y. Antioxidant properties of extracts from Curcuma zedoaria rhizome. Adv. Mat. Res. 2015, 1120, 920–925. [Google Scholar] [CrossRef]
- Lakshmi, S.; Padmaja, G.; Remani, P. Antitumour effects of isocurcumenol isolated from Curcuma zedoaria rhizomes on human and murine cancer cells. Int. J. Med. Chem. 2011, 2011, 253962. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bachheti, R.K.; Rai, I.; Mishra, V.K.; Joshi, A. Antioxidant and antimicrobial properties of seed oil of Datura metel. J. Environ. Biol. 2018, 39, 182–188. [Google Scholar] [CrossRef]
- Fakai, I.M.; Bagudo, A.I.; Aminu, H.; Isaac, M. Physico-chemical analysis and antifungal activity of Datura metel seed oil. Int. J. Pharm. Biosci. 2016, 3, 61–68. [Google Scholar]
- Roy, S.; Mukherjee, S.; Pawar, S.; Chowdhary, A. Evaluation of in vitro antiviral activity of Datura metel Linn. against rabies virus. Pharmacogn. Res. 2016, 8, 265–269. [Google Scholar] [CrossRef] [Green Version]
- Bhardwaj, K.; Kumar, S.; Ojha, S. Antioxidant activity and FT-IR analysis of Datura innoxia and Datura metel and seed methanolic extract. Afr. J. Tradit. Complement. Altern. Med. 2016, 13, 7–16. [Google Scholar]
- Tatiya-Aphiradee, N.; Chatuphonprasert, W.; Jarukamjorn, K. Anti-inflammatory effect of Garcinia mangostana Linn. pericarp extract in methicillin-resistant Staphylococcus aureus-induced superficial skin infection in mice. Biomed. Pharmacother. 2019, 111, 705–713. [Google Scholar] [CrossRef]
- Rahmayanti, F.; Sastradipura, D.F.S.; Masúd, Z.A.; Bachtiar, B.M.; Wimardhani, Y.S.; Permana, G. Ethyl acetate fraction of Garcinia mangostana Linn pericarp extract: Anti—Candida albicans and epithelial cytotoxicity. Asian J. Pharm. Clin. Res. 2016, 9, 357–360. [Google Scholar]
- Tarasuk, M.; Songprakhon, P.; Chimma, P.; Sratongno, P.; Na-Bangchang, K.; Yenchitsomanus, P.T. Alpha-mangostin inhibits both dengue virus production and cytokine/chemokine expression. Virus Res. 2017, 240, 180–189. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, G.; Ibrahim, S. New benzophenones and a dihydroflavanonol from Garcinia mangostana pericarps and their antioxidant and cytotoxic activities. Phytochem. Lett. 2020, 39, 43–48. [Google Scholar] [CrossRef]
- Wang, J.; Shi, Q.; Zhang, W.; Sanderson, B. Anti-skin cancer properties of phenolic-rich extract from the pericarp of mangosteen (Garcinia mangostana Linn.). Food Chem. Toxicol. 2012, 50, 3004–3013. [Google Scholar] [CrossRef] [PubMed]
- Ohno, R.; Moroishi, N.; Sugawa, H.; Maejima, K.; Saigusa, M.; Yamanaka, M.; Nagai, M.; Yoshimura, M.; Amakura, Y.; Nagai, R. Mangosteen pericarp extract inhibits the formation of pentosidine and ameliorates skin elasticity. J Clin. Biochem. Nutr. 2015, 57, 27–32. [Google Scholar] [CrossRef] [Green Version]
- Fitri, E.W.; Anwar, A.I.; Djawad, K.; Seweng, A.; Changara, H.; Alam, G. The effectiveness of topical mangosteen pericarp extract on the collagen of mice skin exposed to ultraviolet B. Am. J. Clin. Exp. Med. 2016, 4, 88–93. [Google Scholar] [CrossRef] [Green Version]
- Moorthy, K.; Punitha, T.; Vinodhini, R.; Sureshkumar, B.T.; Vijayalakshmi, P.; Thajuddin, N. Antimicrobial activity and qualtative phytochemical analysis of Punica granatum Linn. (Pericarp). J. Med. Plants Res. 2013, 7, 474–479. [Google Scholar]
- Anibal, P.C.; Peixoto, I.T.; Foglio, M.A.; Höfling, J.F. Antifungal activity of the ethanolic extracts of Punica granatum L. and evaluation of the morphological and structural modifications of its compounds upon the cells of Candida spp. Braz. J. Microbiol. 2013, 44, 839–848. [Google Scholar] [CrossRef] [Green Version]
- Houston, D.M.J.; Bugert, J.J.; Denyer, S.P.; Heard, C.M. Potentiated virucidal activity of pomegranate rind extract (PRE) and punicalagin against herpes simplex virus (HSV) when co-administered with zinc (II) ions, and antiviral activity of PRE against HSV and aciclovir-resistant HSV. PLoS ONE 2017, 12, e0179291. [Google Scholar]
- Jacob, J.; Lakshmanapermalsamy, P.; Illuri, R.; Bhosle, D.; Sangli, G.K.; Mundkinajeddu, D. In vitro evaluation of antioxidant potential of isolated compounds and various extracts of peel of Punica granatum L. Pharmacogn. Res. 2018, 10, 44–48. [Google Scholar]
- Houston, D.; Bugert, J.; Denyer, S.; Heard, C. Anti-inflammatory activity of Punica granatum L. (Pomegranate) rind extracts applied topically to ex vivo skin. Eur. J. Pharm. Biopharm. 2017, 112, 30–37. [Google Scholar] [CrossRef]
- Seifabadi, S.; Vaseghi, G.; Ghannadian, M.; Javanmard, S. Standardized Punica granatum pericarp extract, suppresses tumor proliferation and angiogenesis in a mouse model of melanoma: Possible involvement of PPAR alpha and PPAR gamma pathways. Iran. J. Pharm. Sci. 2019, 18, 348–357. [Google Scholar]
- Wan Nor Amilah, W.A.; Masrah, M.; Hasmah, A.; Noor Izani, N.J. In vitro antibacterial activity of Quercus infectoria gall extracts against multidrug resistant bacteria. Trop. Biomed. 2014, 31, 680–688. [Google Scholar] [PubMed]
- Vanga, S.; Pingili, M.; Tharigoppula, S. Phytochemical screening and evaluation of antifungal activity of gall extracts of Quercus infectoria. Int. J. Pharm. Sci. Res. 2017, 8, 3010–3013. [Google Scholar]
- Ghafarzadeh, M.; Eatemadi, A. Clinical efficacy of liposome-encapsulated Aloe vera on melasma treatment during pregnancy. J. Cosmet. Laser Ther. 2017, 19, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Chokpaisarn, J.; Chusri, S.; Amnuaikit, T.; Udomuksorn, W.; Voravuthikunchai, S. Potential wound healing activity of Quercus infectoria formulation in diabetic rats. PeerJ 2017, 5, e3608. [Google Scholar] [CrossRef] [Green Version]
- Chokpaisarn, J.; Urao, N.; Voravuthikunchai, S.; Koh, T. Quercus infectoria inhibits Set7/NF-kappa B inflammatory pathway in macrophages exposed to a diabetic environment. Cytokine 2017, 94, 29–36. [Google Scholar] [CrossRef]
- Rahman, M.M.; Shamsuzzaman, M.; Khatun, M.; Rahman, M.M.; Hossain, A.S.M.S.; Alam, A.H.M.K.; Mosaddik, A.; Wahed, M.I.I. Phytochemical and antimicrobial properties of Tiliacora triandra stem bark. Br. J. Pharm. Res. 2017, 17, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Añibarro-Ortega, M.; Pinela, J.; Barros, L.; Ćirić, A.; Silva, S.P.; Coelho, E.; Mocan, A.; Calhelha, R.C.; Soković, M.; Coimbra, M.A.; et al. Compositional features and bioactive properties of Aloe vera leaf (fillet, mucilage, and rind) and flower. Antioxidants 2019, 8, 444. [Google Scholar] [CrossRef] [Green Version]
- Dziewulska, D.; Stenzel, T.; Smialek, M.; Tykalowski, B.; Koncicki, A. An evaluation of the impact of aloe vera and licorice extracts on the course of experimental pigeon paramyxovirus type 1 infection in pigeons. Poult. Sci. 2018, 97, 470–476. [Google Scholar] [CrossRef]
- Vijayalakshmi, D.; Dhandapani, R.; Jayaveni, S.; Jithendra, P.S.; Rose, C.; Mandal, A.B. In vitro anti-inflammatory activity of Aloe vera by down regulation of MMP-9 in peripheral blood mononuclear cells. J. Ethnopharmacol. 2012, 141, 542–546. [Google Scholar] [CrossRef]
- Fox, L.T.; du Plessis, J.; Gerber, M.; van Zyl, S.; Boneschans, B.; Hamman, J.H. In Vivo skin hydration and anti-erythema effects of Aloe vera, Aloe ferox and Aloe marlothii gel materials after single and multiple applications. Pharmacogn. Mag. 2014, 10, S392–S403. [Google Scholar] [PubMed] [Green Version]
- Fox, L.T.; Gerber, M.; du Preez, J.L.; du Plessis, J.; Hamman, J.H. Skin permeation enhancement effects of the gel and whole-leaf materials of Aloe vera, Aloe marlothii and Aloe ferox. J. Pharm. Pharmacol. 2015, 67, 96–106. [Google Scholar] [CrossRef] [PubMed]
- Dhanabal, S.P.; Priyanka Dwarampudi, L.; Muruganantham, N.; Vadivelan, R. Evaluation of the antipsoriatic activity of Aloe vera leaf extract using a mouse tail model of psoriasis. Phytother. Res. 2012, 26, 617–619. [Google Scholar] [CrossRef] [PubMed]
- Prakash, A.; Vadivel, V.; Banu, S.F.; Nithyanand, P.; Lalitha, C.; Brindhad, P. Evaluation of antioxidant and antimicrobial properties of solvent extracts of agro-food by-products (cashew nut shell, coconut shell and groundnut hull). Agric. Nat. Resour. 2018, 52, 451–459. [Google Scholar] [CrossRef]
- Sudjaroen, Y.; Thongkao, K.; Suwannahong, K. Antioxidant, antibacterial, and cytotoxicity activities of cashew (Anacardium occidentale) Nut Shell Waste. Int. J. Green Pharm. 2018, 12, S229–S234. [Google Scholar]
- Mahata, D.; Mandal, S.M.; Bharti, R.; Gupta, V.K.; Mandal, M.; Nag, A.; Nando, G.B. Self-assembled cardanol azo derivatives as antifungal agent with chitin-binding ability. Int. J. Biol. Macromol. 2014, 69, 5–11. [Google Scholar] [CrossRef] [PubMed]
- de Souza, M.Q.; Teotônio, I.M.S.N.; de Almeida, F.C.; Heyn, G.S.; Alves, P.S.; Romeiro, L.A.S.; Pratesi, R.; de Medeiros Nóbrega, Y.K.; Pratesi, C.B. Molecular evaluation of anti-inflammatory activity of phenolic lipid extracted from cashew nut shell liquid (CNSL). BMC. Complement. Altern. Med. 2018, 18, 181. [Google Scholar] [CrossRef]
- Faruk, M.O.; Sardar, R.; Haque, S.T.; Haque, M.E. Antimicrobial, cytotoxic and antioxidant activities of Barringtonia acutangula (L). Bioresearch Commun. 2016, 2, 205–209. [Google Scholar]
- Inampudi, V.K.; Jay Kumar, S.; Koshy, R.K.; Patel, Y.; Sujitha, P.J. Anti-oxidant and anti-inflammatory activities of Barringtonia acutangula linn. bark extracts on rats. Int. J. Curr. Res. 2014, 6, 9785–9790. [Google Scholar]
- Haque, A.; Islam, A.; Shahriar, M. Antimicrobial, cytotoxicity and antioxidant activity of Tinospora crispa. J. Pharm. Biomed. Sci. 2011, 13, 1–4. [Google Scholar]
- Hipol, R.L.B.; Cariaga, M.F.N.M.; Hipol, R.M. Inflammatory activities of the aqueous extract of the stem of Tinospora Crispa (Family Menispermaceae). J. Nat. Stud. 2012, 11, 88–95. [Google Scholar]
- Songkhla Provincial Public Health Office, Ministry of Public Health, Thailand. 2019, pp. 13–14. Available online: https://www.skho.moph.go.th/strategy/inspec/2562/2/index.html#p=15 (accessed on 6 February 2022).
- Bridson, D.; Forman, L. The Herbarium Handbook; Royal Botanic Gardens: Kew, UK, 1992. [Google Scholar]
- The Plant List. Version 1.1. 2013. Available online: http://www.theplantlist.org/ (accessed on 13 January 2021).
- Umair, M.; Altaf, M.; Abbasi, A.M. An ethnobotanical survey of indigenous medicinal plants in Hafizabad district, Punjab-Pakistan. PLoS ONE 2017, 12, e0177912. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kayani, S.; Ahmad, M.; Zafar, M.; Sultana, S.; Khan, M.P.Z.; Ashraf, M.A.; Hussain, J.; Yaseen, G. Ethnobotanical uses of medicinal plants for respiratory disorders among the inhabitants of Gallies–Abbottabad, northern Pakistan. J. Ethnopharmacol. 2014, 156, 47–60. [Google Scholar] [CrossRef] [PubMed]
| Demographical Characteristics | Number of Informants (n = 6) |
|---|---|
| Sex | |
| Male | 6 |
| Age (years) | |
| 50–59 | 1 |
| 60–69 | 2 |
| >70 | 3 |
| Education level | |
| Primary school | 3 |
| Secondary school | 1 |
| Vocational diploma | 1 |
| Bachelor’s degree | 1 |
| Religion | |
| Buddhism | 5 |
| Islam | 1 |
| Prescription | Skin Disorder | Scientific Name/Voucher Number | Local Name | Family | Parts Used | Formulation Form |
|---|---|---|---|---|---|---|
| 1. SKHS1-SC1 | Herpes simplex | Jasminum sambac (L.) Aiton/ N. Kiankhun 009 | Ma li | Oleaceae | Root | Poultice |
| Oryza sativa L./ N. Kiankhun 010 | Khao | Poaceae | Seed | |||
| 2. SKHS2-SC2 | Herpes simplex | Mitragyna speciosa (Roxb.) Korth./ N. Kiankhun014 | Kra tom | Rubiaceae | Leaf | Poultice |
| 3. SKHS3-SC3 | Herpes simplex | Glycosmis pentaphylla (Retz.) DC./ N. Kiankhun 015 | Khoei tai | Rutaceae | Root | Poultice |
| Oryza sativa L./ N. Kiankhun 010 | Khao | Poaceae | Seed | |||
| 4. SKHS4-SC4 | Herpes simplex | Mirabilis jalapa L./ N. Kiankhun 016 | Ban yen | Nyctaginaceae | Root | Poultice |
| Oryza sativa L./ N. Kiankhun 010 | Khao | Poaceae | Seed | |||
| 5. SKHS5-SC5 | Herpes simplex | Euphorbia hirta L./ N. Kiankhun 017 | Nam num rat cha si | Euphorbiaceae | Whole plant | Poultice |
| Oryza sativa L./ N. Kiankhun 010 | Khao | Poaceae | Seed | |||
| 6. SKEC1-SC6 | Eczema | Tinospora crispa (L.) Miers ex Hook.f. & Thomson/N. Kiankhun 018 | Bor ra pet | Menispermaceae | Stem | Poultice |
| Psidium guajava L./ N. Kiankhun 019 | Pha rang | Myrtaceae | Leaf | |||
| Areca catechu (L.f.) Willd./ N. Kiankhun 020 | Mak | Arecaceae | Seed | |||
| Piper betle L./ N. Kiankhun 021 | Plu | Piperaceae | Leaf | |||
| 7. SKTI1-SC7 | Tinea | Quercus infectoria Oliv. * | Ben ga nee | Fagaceae | Nut gall * | Hot oil extraction |
| Acacia catechu (L.f.) Willd. * | Si siad tai | Fabaceae | Crude extract | |||
| Uncaria gambir (Hunter) Roxb. * | Si siad tet | Rubiaceae | Crude extract | |||
| Zingiber montanum (Koenig) Link ex Dietr./N. Kiankhun 025 | Phlai | Zingiberaceae | Rhizome | |||
| Aloe vera (L.) Burm.f. * | Wan hang cho ra khe | Xanthorrhoeaceae | Leaf’s latex (resin) | |||
| Anacardium occidentale L./ N. Kiankhun 044 | Ma muang him ma pan | Anacardiaceae | Pericarp | |||
| Entada rheedii Spreng./ N. Kiankhun 028 | Sa ba | Fabaceae | Seed | |||
| Knema globularia (Lamk.) Warb/ N. Kiankhun 029 | Han | Myristicaceae | Seed | |||
| Barringtonia acutangula (L.) Garetn./ N. Kiankhun 030 | Chik na | Lecythidaceae | Stem bark | |||
| 8. SKTI2-BK8 | Tinea | Datura metel L./ N. Kiankhun 032 | Lum pong ka sa lak | Solanaceae | Seed | Ointment |
| Pterocarpus indicus Willd./ N. Kiankhun 033 | Pra du | Fabaceae | Stem bark | |||
| Hopea odorata Roxb./ N. Kiankhun 034 | Ta kian | Dipterocarpaceae | Stem bark | |||
| Knema globularia (Lamk.) Warb/ N. Kiankhun 029 | Han | Myristicaceae | Seed | |||
| Tiliacora triandra (Colebr.) Diels./ N. Kiankhun 036 | Ya nang | Menispermaceae | Stem | |||
| Cratoxylun cochinchinense (Lour.) Blume/N. Kiankhun 037 | Tio | Hypericaceae | Stem bark | |||
| Curcuma zedoaria (L.) Roscoe ex Sm./ N. Kiankhun 094 | Ka min ooi | Zingiberaceae | Rhizome | |||
| 9. SKTI3-YH9 | Tinea | Typhonium trilobatum Schott./ N. Kiankhun 039 | Ut ta pid | Araceae | Corm | Hot oil extraction |
| Alocasia longiloba Miq./ N. Kiankhun040 | O nok | Araceae | Corm | |||
| Rhinacanthus nasutus (L.) Kurz./ N. Kiankhun 041 | Thong pan chang | Acanthaceae | Leaf | |||
| Nicotiana tabacum L./ N. Kiankhun042 | Ya sueb | Solanaceae | Leaf | |||
| 10. SKLY1-SC10 | Ulcer | Anacardium occidentale L./ N. Kiankhun044 | Ma muang him ma pan | Anacardiaceae | Pericarp | Hot oil extraction |
| Zingiber montanum (Koenig) Link ex Dietr./N. Kiankhun025 | Phlai | Zingiberaceae | Rhizome | |||
| Aloe vera (L.) Burm.f. * | Wan hang cho ra khe | Xanthorrhoeaceae | Leaf’s latex (resin) | |||
| 11. SKLY2-BK11 | Ulcer | Prismatomeris tetrandra (Roxb.) K. Schum/N. Kiankhun 048 | Kra duk kai | Rubiaceae | Root | Decoction |
| Eurycoma longifolia Jack/ N. Kiankhun 049 | Lai phueak | Simaroubaceae | Root | |||
| Dianella ensifolia (L.) DC./ N. Kiankhun 050 | Ya nu ton | Xanthorrhoeaceae | Root | |||
| Arcangelisia flava (L.) Merr./ N. Kiankhun 051 | Ka min kruea | Menispermaceae | Stem | |||
| 12. SKPU1-SC12 | Pus | Lasia spinosa (L.) Thw./ N. Kiankhun 053 | Pak nam | Araceae | Rhizome | Decoction |
| Nicotiana tabacum L./ N. Kiankhun 042 | Ya sueb | Solanaceae | Leaf | |||
| 13. SKAB1-BK13 | Abscess | Ceiba pentandra (L.) Gaertn./ N. Kiankhun056 | Nun | Malvaceae | Leaf | Poultice |
| Curcuma longa L./ N. Kiankhun 057 | Ka min chan | Zingiberaceae | Rhizome | |||
| Senna siamea (Lam.) Irwin & Barneby./N. Kiankhun 058 | Khi lek | Fabaceae | Leaf | |||
| Oryza sativa L./ N. Kiankhun 010 | Khao | Poaceae | Seed | |||
| 14. SKAB2-SC14 | Abscess | Garcinia mangostana L./ N. Kiankhun 061 | Mung kud | Clusiaceae | Pericarp | Poultice |
| Nicotiana tabacum L./ N. Kiankhun 042 | Ya sueb | Solanaceae | Leaf | |||
| 15. SKAB3-SC15 | Abscess | Tinospora crispa (L.) Miers ex Hook.f. & Thomson/N. Kiankhun 018 | Bor ra pet | Menispermaceae | Stem | Decoction |
| Eurycoma longifolia Jack/ N. Kiankhun 049 | Lai phueak | Simaroubaceae | Root | |||
| Olax psittacorum (Willd.) Vahl/ N. Kiankhun 065 | Nam chai krai | Oleaceae | Stem bark | |||
| 16. SKAB4-BP16 | Abscess | Smilax corbularia Kunth. * | Khoa yen neua | Smilacaceae | Tuber | Decoction |
| Smilax glabra Wall.ex Roxb. | Khoa yen tai | Smilacaceae | Tuber | |||
| Senna siamea (Lam.) Irwin & Barneby./N. Kiankhun 058 | Khi lek | Fabaceae | Wood | |||
| Hydnophytum formicarium Jack/N. Kiankhun 070 | Hua roi ru | Rubiaceae | Modified stem | |||
| Eurycoma longifolia Jack/ N. Kiankhun 049 | Lai phueak | Simaroubaceae | Root | |||
| Clerodendrum inerme (L.) Gaertn./ N. Kiankhun 072 | Sam ma nga | Lamiaceae | Root | |||
| Acanthus ebracteatus Vahl./ N. Kiankhun 073 | Ngueak pla mor | Acanthaceae | Whole plant | |||
| 17. SKTD1-YH17 | Ulcer | Sepia spp./Sepiella spp. (animal) * | Kra dong muk | Sepiidae | Cuttlebone | Powders |
| Quercus infectoria Oliv.* | Ben ga nee | Fagaceae | Nut gall | |||
| Punica granatum L./ N. Kiankhun 077 | Tub tim | Punicaceae | Pericarp | |||
| 18. SKCD1-SC1 | Rash | Citrus maxima (Burm.) Merrill./ N. Kiankhun 079 | Som O | Rutaceae | Pericarp | Decoction |
| Senna siamea (Lam.) Irwin & Barneby./N. Kiankhun 058 | Khi lek | Fabaceae | Leaf | |||
| Azadirachta indica A. Juss./ N. Kiankhun 081 | Sa dao | Meliaceae | Leaf | |||
| Cardiospermum halicacabum L./ N. Kiankhun 082 | Kok kra oom | Sapindaceae | Whole plant | |||
| Senna alata (L.) Roxb./ N. Kiankhun 083 | Chum hed tet | Fabaceae | Leaf | |||
| 19. SKSC1-SC19 | Chlonic ulcer | Annona squamosa L. (L.) Miers ex Hook.f.& Thomson/N. Kiankhun 083 | Noi na | Annonaceae | Root | Decoction |
| Phyllanthus emblica L./ N. Kiankhun 085 | Ma kam pom | Phyllanthaceae | Root | |||
| Streblus asper Lour./ N. Kiankhun 086 | Khoi | Moraceae | Root | |||
| Sandoricum koetjape (Burm. f.) Merr./N. Kiankhun 086 | Kra ton | Meliaceae | Root | |||
| Barringtonia acutangula (L.) Garetn./N. Kiankhun 030 | Chik na | Lecythidaceae | Stem bark | |||
| 20. SKCD2-SC20 | Ulcer | Clinacanthus nutans (Burm.f.) Lindau/N. Kiankhun 089 | Pha ya yor | Acanthaceae | Leaf | Poultice |
| Carallia brachiata (Lour.) Merr./ N. Kiankhun 090 | Chiang phra nang ae | Rhizophoraceae | Leaf | |||
| 21. SKTD2-BP21 | Ulcer | Garcinia mangostana L./ N. Kiankhun061 | Mung kud | Clusiaceae | Pericarp | Poultice |
| Punica granatum L./N. Kiankhun077 | Tub tim | Punicaceae | Pericarp | |||
| Curcuma zedoaria (L.) Roscoeex Sm./ N. Kiankhun094 | Ka min ooi | Zingiberaceae | Rhizome | |||
| Curcuma longa L./N. Kiankhun 057 | Ka min chan | Zingiberaceae | Rhizome | |||
| Zingiber montanum (Koenig) Link ex Dietr./N. Kiankhun 025 | Phlai | Zingiberaceae | Rhizome | |||
| Syzygium cf. claviflorum (Roxb.) A.M. Cowan& Cowan/N. Kiankhun097 | Wa | Myrtaceae | Stem bark | |||
| 22. SKTD3-KK22 | Ulcer | Combretum cf. quadrangulare Kurz/ N. Kiankhun 099 | Sang kae | Combretaceae | Leaf | |
| Quisqualis indica L./ N. Kiankhun100 | Leb muea nang | Combretaceae | Leaf | |||
| Phyllanthus amarus L./ N. Kiankhun 101 | Luk tai bai | Phyllanthaceae | Whole plant | |||
| 23. SKSB1-PB23 | Scabies | Knema globularia (Lamk.) Warb/ N. Kiankhun 029 | Han | Myristicaceae | Seed | Hot oil extraction |
| Tiliacora triandra (Colebr.) Diels./ N. Kiankhun 036 | Ya nang | Menispermaceae | Stem | |||
| Ceriscoides turgida (Roxb.) Tirveng. * | Kra bian | Rubiaceae | Fruit | |||
| Hydnocarpus anthelminthicus Pierre ex Laness./N. Kiankhun 106 | Kra bao | Flacourtiaceae | Seed | |||
| Allium sativum L./ N. Kiankhun 107 | Kra tiam | Alliaceae | Storage leaf | |||
| 24. SKAN1-SC25 | Acne | Justicia adhatoda L./ N. Kiankhun 109 | Sa niad | Acanthaceae | Leaf | Poultice |
| Zingiber montanum (Koenig) Link ex Dietr./N. Kiankhun 025 | Phlai | Zingiberaceae | Rhizome | |||
| Zingiber zerumbet (L.) Smith./ N. Kiankhun 111 | Ka thue | Zingiberaceae | Rhizome | |||
| Curcuma longa L./ N. Kiankhun057 | Ka min chan | Zingiberaceae | Rhizome | |||
| Curcuma aromatica Salisb./ N. Kiankhun 113 | Wan nang kum | Zingiberaceae | Rhizome | |||
| 25. SKLP1-SC25 | Ulcer leprosy | Nicotiana tabacum L./ N. Kiankhun 042 | Ya sueb | Solanaceae | Leaf | Hot oil extraction |
| Zingiber montanum (Koenig) Link ex Dietr./N. Kiankhun 025 | Phlai | Zingiberaceae | Rhizome | |||
| Curcuma zedoaria (L.) Roscoeex Sm./N. Kiankhun 094 | Ka min ooi | Zingiberaceae | Rhizome | |||
| Stemona tuberosa Lour./ N. Kiankhun 117 | Non tai yak | Stemonaceae | Modified root | |||
| Datura metel L./ N. Kiankhun 032 | Lum pong | Solanaceae | Seed |
| Families | Percent of Species | Families | Percent of Species |
|---|---|---|---|
| Fabaceae | 7.6 | Clusiaceae | 1.5 |
| Rubiaceae | 7.6 | Dipterocarpaceae | 1.5 |
| Zingiberaceae | 7.6 | Euphorbiaceae | 1.5 |
| Acanthaceae | 6.1 | Fagaceae | 1.5 |
| Araceae | 4.5 | Flacourtiaceae | 1.5 |
| Menispermaceae | 4.5 | Hypericaceae | 1.5 |
| Combretaceae | 3.0 | Lamiaceae | 1.5 |
| Meliaceae | 3.0 | Lecythidaceae | 1.5 |
| Myrtaceae | 3.0 | Malvaceae | 1.5 |
| Oleaceae | 3.0 | Moraceae | 1.5 |
| Phyllanthaceae | 3.0 | Myristicaceae | 1.5 |
| Rutaceae | 3.0 | Nyctaginaceae | 1.5 |
| Smilacaceae | 3.0 | Piperaceae | 1.5 |
| Solanaceae | 3.0 | Poaceae | 1.5 |
| Xanthorrhoeaceae | 3.0 | Punicaceae | 1.5 |
| Alliaceae | 1.5 | Rhizophoraceae | 1.5 |
| Anacardiaceae | 1.5 | Sapindaceae | 1.5 |
| Annonaceae | 1.5 | Simaroubaceae | 1.5 |
| Arecaceae | 1.5 | Stemonaceae | 1.5 |
| Scientific Name | UV | RFC | Part Used | Pharmacological Activity |
|---|---|---|---|---|
| Oryza sativa L. | 0.83 | 0.33 | Seed | Anti-oxidant and anti-inflammatory activity [23] Antibacterial activity [24] Antifungal activity [25] Antiviral effect [26] Anti-aging activity [27] Reduction of psoriasis severity [28] Anti-arthritic Activity [59] |
| Zingiber montanum (Koenig) Link ex Dietr. | 0.83 | 0.33 | Rhizome | Antioxidant activity [34] Anti-inflammatory activity [35] Antibacterial activity [32] Antifungal activity [31] Anti-ulcer property [60] Anticancer activity [61] |
| Nicotiana tabacum L. | 0.67 | 0.33 | Leaf | Antibacterial and antifungal activity [62] Antiviral activity [38] Anti-oxidant activity [63] Anti-dandruff [39] Anti-aphthous activity [64] |
| Curcuma longa L. | 0.50 | 0.50 | Rhizome | Antibacterial activity [65] Antifungal activity [66] Antiviral activity [67] Antioxidant activity [41] Anti-inflammatory activity [68] Wound healing activity [43] Hyaluronidase inhibitor activity [69] |
| Eurycoma longifolia Jack | 0.50 | 0.50 | Root | Antioxidant and anti-inflammatory activity [44] Antibacterial and antifungal activity [45,70] Anticancer activity [46] Tyrosinase inhibition activity [71] |
| Knema globularia (Lamk.) Warb | 0.50 | 0.50 | Seed | Cytotoxicity activity [47] (fruit), [48] (root) |
| Senna siamea (Lam.) Irwin & Barneby. | 0.50 | 0.50 | Leaf | Antibacterial and antifungal activity [50,51] Anti-inflammatory and analgesic activity [52] Antioxidant activity [72] |
| Curcuma zedoaria (L.) Roscoeex Sm. | 0.33 | 0.33 | Rhizome | Antibacterial and anti-inflammatory activity [73] Antifungal activity [74] Anti-oxidant activity [75] Wound healing activity [53] Antitumor activity [76] |
| Datura metel L. | 0.33 | 0.33 | Seed | Antibacterial activity [77] Antifungal activity [78] Antiviral activity [79] Antioxidant activity [80] |
| Garcinia mangostana L. | 0.33 | 0.33 | Pericarp | Antibacterial activity [81] Antifungal activity [82] Antiviral activity [83] Antioxidant activity [84] Anti-inflammatory activity [81] Anti-skin cancer property [85] Remedial effect on skin conditions [86] Cell proliferation and Wound healing activity [55] Increased skin collagen thickness and density [87] |
| Punica granatum L. | 0.33 | 0.33 | Pericarp | Antibacterial activity [88] Antifungal activity [89] Antiviral activity [90] Antioxidant activity [91] Anti-inflammatory activity [92] Anti-melanoma activity [93] Wound healing activity [56] |
| Quercus infectoria Oliv. | 0.33 | 0.33 | Gall | Antibacterial activity [94] Antifungal activity [95] Antioxidant activity [96] Anti-inflammatory activity [97] Wound healing activity [57,98] |
| Tiliacora triandra (Colebr.) Diels. | 0.33 | 0.33 | Stem | Antibacterial and antifungal activity [99] |
| Aloe vera (L.) Burm.f. | 0.33 | 0.17 | Leaf latex | Antibacterial, antifungal, and anti-oxidant activity [100] Antiviral activity [101] Anti-inflammatory activity [102] Skin hydration and anti-erythema effect [103] Skin permeation-enhancing effect [104] Wound healing activity [54] Melasma decreasing activity [96] Anti-psoriatic activity [105] |
| Anacardium occidentale L. | 0.33 | 0.17 | Pericarp | Anti-bacterial and anti-oxidant activity [106,107] Antifungal activity [108] Anti-inflammatory activity [109] |
| Barringtonia acutangular (L.) Garetn. | 0.33 | 0.17 | Stem bark | Anti-bacterial, antifungal, and anti-oxidant activity [110] Anti-inflammatory activity [111] |
| Tinospora crispa (L.) Miers ex Hook.f. & Thomson | 0.33 | 0.17 | Stem | Antibacterial, antifungal, and anti-oxidant activity [112] Anti-inflammatory activity [113] Wound healing activity [58] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saising, J.; Maneenoon, K.; Sakulkeo, O.; Limsuwan, S.; Götz, F.; Voravuthikunchai, S.P. Ethnomedicinal Plants in Herbal Remedies Used for Treatment of Skin Diseases by Traditional Healers in Songkhla Province, Thailand. Plants 2022, 11, 880. https://doi.org/10.3390/plants11070880
Saising J, Maneenoon K, Sakulkeo O, Limsuwan S, Götz F, Voravuthikunchai SP. Ethnomedicinal Plants in Herbal Remedies Used for Treatment of Skin Diseases by Traditional Healers in Songkhla Province, Thailand. Plants. 2022; 11(7):880. https://doi.org/10.3390/plants11070880
Chicago/Turabian StyleSaising, Jongkon, Katesarin Maneenoon, Oraphan Sakulkeo, Surasak Limsuwan, Friedrich Götz, and Supayang Piyawan Voravuthikunchai. 2022. "Ethnomedicinal Plants in Herbal Remedies Used for Treatment of Skin Diseases by Traditional Healers in Songkhla Province, Thailand" Plants 11, no. 7: 880. https://doi.org/10.3390/plants11070880
APA StyleSaising, J., Maneenoon, K., Sakulkeo, O., Limsuwan, S., Götz, F., & Voravuthikunchai, S. P. (2022). Ethnomedicinal Plants in Herbal Remedies Used for Treatment of Skin Diseases by Traditional Healers in Songkhla Province, Thailand. Plants, 11(7), 880. https://doi.org/10.3390/plants11070880






