Tyrosinase Inhibitory Ability and In Vitro, In Vivo Acute Oral and In Silico Toxicity Evaluation of Extracts Obtained from Algerian Fir (Abiesnumidica de Lannoy ex CARRIERE) Needles
Abstract
:1. Introduction
2. Results
2.1. Tyrosinase Inhibitory Ability
2.2. In Vitro, In Vivo and In Silico Toxicity of Extracts (EA and n-BuOH)
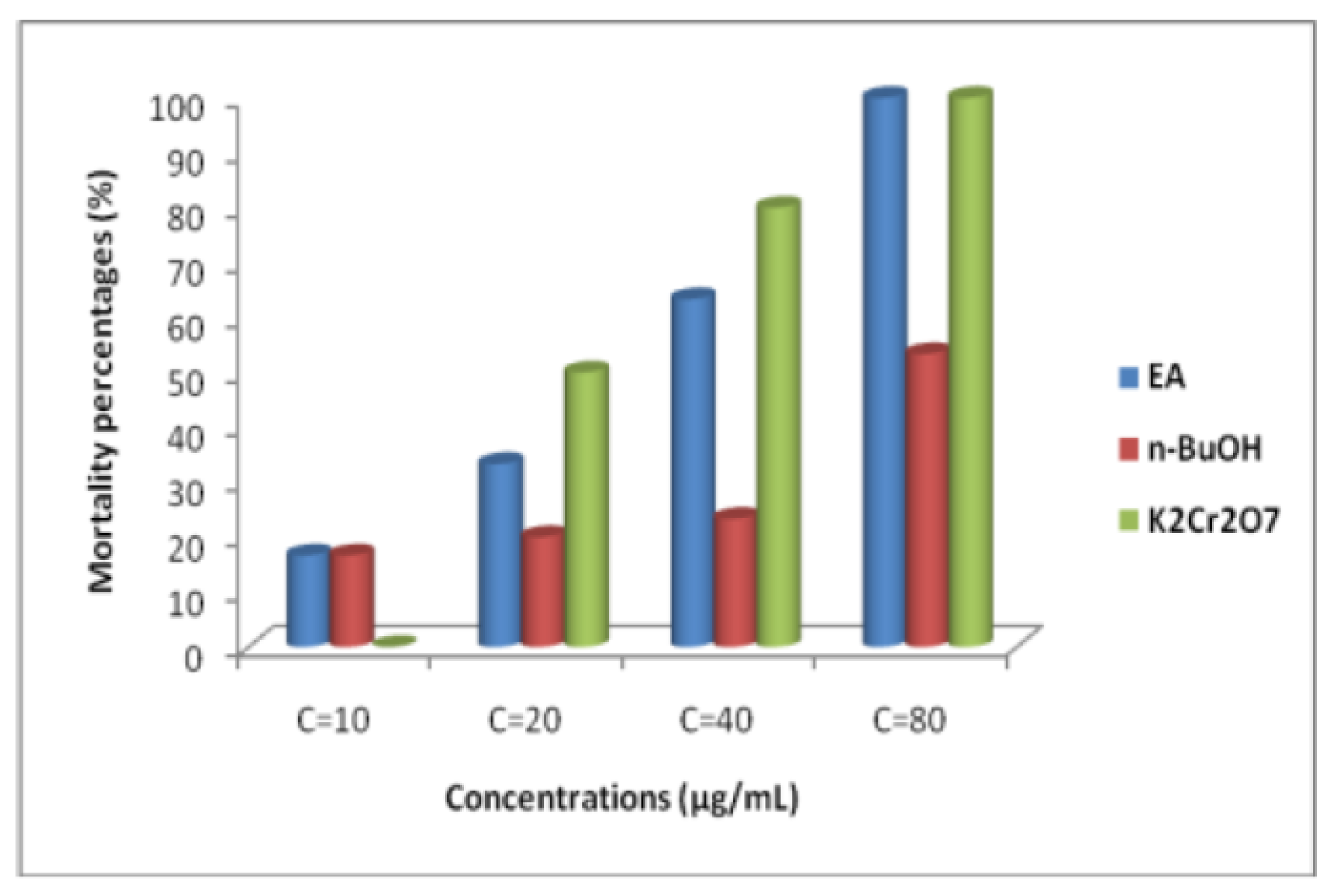
2.2.1. Brine Shrimp Lethality Test
2.2.2. In Vivo Oral Acute Toxicity
- Behaviors, toxicity signs, and body weight variations
- Biochemical parameters
- -
- Effect of extracts (EA and n-BuOH) on renal function
- -
- Effect of EA and n-BuOH on hepatic parameters
- -
- Effect of the extracts (EA and n-BuOH) on lipid profile
- -
- Effect of EA and n-BuOH extracts on organs tissues
2.2.3. ADMET Properties of Molecules Identified in A. numidica Leaves Extracts
Physico-Chemical Properties of Molecules
Pharmacokinetic Properties
Absorption
Distribution
- Volume of Distribution (DV)
- Permeability of the blood-brain barrier (BBB)
Metabolism
- -
- Quercetin is a CYP1A2 inhibitor
- -
- Luteolin is a CYP1A2 and CYP2C9 inhibitor
- -
- Apigetrin is an inhibitor of CYP1A2 and CYP2CA9
Clearance
- Total clearance
- Organic Cation Transporter (OCT2) Substrates
Toxicity
- Hepatotoxicity
Maximum Tolerated Dose (MTD)
3. Discussion
4. Materials and Methods
4.1. Extraction of Secondary Metabolites
4.2. Tyrosinase Inhibitory Ability of Extracts
4.3. Toxicity of Extracts In Vitro, In Vivo and In Silico
4.3.1. In Vitro Cytotoxicity Assay Using Brine Shrimp Lethality Assay
- Hatching Brine Shrimp eggs
- Brine Shrimp lethality assay
- -
- Control: larvae number in control group (n = 10)
- -
- Surviving: surviving larvae number
4.3.2. In Vivo Oral Acute Toxicity Assay
4.4. ADMET Properties In Silico
4.4.1. Identification of Bioactive Molecules in EA and n-BuOHFractions
4.4.2. Programs Used and Pharmacokinetic Properties in Silico Study
- PubChem database
- pkCSM Server and pharmacokinetic properties determination.
4.5. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Farhud, D.D. Impact of Lifestyle on Health. Iran J. Public Health 2015, 44, 1442–1444. [Google Scholar] [PubMed]
- Han, Y.; Yizhen, H.; Canqing, Y.; Yu, G.; Pei, P.; Ling, Y.; Yiping, C.; Huaidong, D.; Dianjianyi, S.; Yuanjie, P.; et al. Lifestyle, cardiometabolic disease, and multimorbidity in a prospective Chinese study. Eur. Heart J. 2021, 2020, 3374–3384. [Google Scholar] [CrossRef] [PubMed]
- Tabish, S.A. Lifestyle Diseases: Consequences, Characteristics, Causes and Control. J. Cardiol. Curr. Res. 2017, 9, 326. [Google Scholar]
- Császár, N.; Kapócs, G.; Erdöfi-Szabó, A. Modern environmental and lifestyle risk factors, oxidative stress, perturbed epigenetic processes, and increasing incidence of neurodevelopmental, neurodegenerative and neurological disorders. Int. Res. J. Med. Med. Sci. 2021, 9, 68–93. [Google Scholar] [CrossRef]
- Bhargava, D.; Trivedi, H. A Study of Causes of Stress and Stress Management among Youth. Int. J. Manag. Soc. Sci. 2018, 11, 108–117. [Google Scholar] [CrossRef]
- Saito, S.; Givaldo, S.; Regineide, X.S.; Grace, G.; Cristina, P.; Martin, B. Astragalin from Cassia alata Induces DNA Adducts in vitro and Repairable DNA Damage in the Yeast Saccharomyces cerevisiae. Int. J. Mol. Sci. 2012, 13, 2846–2862. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Fengjun, S.; Wei, F.; Xuewen, Q.; Yao, L.; Bo, Y.; Yongchuan, C.; Peiyuan, X. Hyperoside inhibits biofilm formation of Pseudomonas aeruginosa. Exp. Ther. Med. 2017, 14, 1647–1652. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Kun, Z.; Xin, M.; Qiong, T.; Wenli, L.; Tianyuan, G.; Xiaona, M.; Jian, Z. Astragalin Attenuates UVB Radiation-induced Actinic Keratosis Formation. Anticancer Agents Med. Chem. 2018, 18, 1001–1008. [Google Scholar] [CrossRef]
- Riaz, A.; Rasul, A.; Hussain, G.; Zahoor, M.K.; Jabeen, F.; Subhani, Z.; Younis, T.; Ali, M.; Sarfraz, I.; Selamoglu, Z. Astragalin:A bioactive phytochemical with potential therapeutic activities. Adv. Pharmacol. Sci. 2018, 32, 9794625. [Google Scholar] [CrossRef]
- Uysala, S.; Asli, U.; Gokhan, Z.; Mehmet, C.B.; Yasemin, C.A.; Adriano, M.; Luisa, C.; Nuno, R.; Nengf, J.M.F.; Nogueiraf, M. Novel in vitro and in silico insights of the multi-biological activities andchemical composition of Bidens tripartita L. Food Chem. Toxicol. 2018, 111, 525–536. [Google Scholar] [CrossRef]
- Engwa, G.A. Free Radicals and the Role of Plant Phytochemicals as Antioxidants Against Oxidative Stress-Related Diseases. Phytochemicals—Source of Antioxidants and Role in Disease Prevention. In Phytochemicals; Chapter 4; InTechOpen: London, UK, 2018. [Google Scholar] [CrossRef] [Green Version]
- Prakash, V.; Anand, S. Analysis of Achyranthes Aspera, L. Extracts for Their α-Amylase and Urease Inhibitory Activities. J. Drug Deliv. Ther. 2021, 11, 108–112. [Google Scholar] [CrossRef]
- Tlili-Ait Kaki, Y.; Bennadja, S.; Chefrour, A. Révalorisationd’uneessence endémique: Le sapin de Numidie (Abiesnumidica). Flora Mediterr. 2013, 23, 123–129. [Google Scholar] [CrossRef]
- Ramdani, M.; Lograda, T.; Chalard, P.; Figueredo, G. Chemical and antimicrobial properties of essential oil of Abiesnumidica, endemic species of Algeria. Int. J. Phytopharm. 2014, 5, 432–440. [Google Scholar]
- Ghadbane, M.; Bounar, R.; Khellaf, R.; Medjekal, S.; Belhadj, H.; Benderradji, L.; Smaili, T.; Harzallah, D. Antioxidant and antimicrobial activities of endemic tree Abies numidica growing in babor mountains from Algeria.Glob. J. Res. Med.PlantsIndig. Med. 2016, 5, 19–28. [Google Scholar]
- Belhadj Mostefa, M.; Abedini, A.; Voutquenne-Nazabadioko, L.; Gangloff, S.C.; Kabouche, A.; Kabouche, Z. Abietane diterpenes from the cones of Abies numidica de Lannoy ex Carrière (Pinaceae) and in vitro evaluation of their antimicrobial properties. Nat. Prod. Res. 2017, 31, 568–571. [Google Scholar] [CrossRef]
- Benouchenne, D.; Bellil, I.; Akkal, S.; Bensouici, C.; Khelifi, D. LC–MS/MS analysis, antioxidant and antibacterial activities of Algerian fir (Abies numidica de LANNOY ex CARRIÈRE) ethyl acetate fraction extracted from needles. J. King Saud. Univ. Sci. 2020, 32, 3321–3327. [Google Scholar] [CrossRef]
- Benouchenne, D.; Bellil, I.; Akkal, S.; Khelifi, D. Investigation of Phytochemical and Evaluation of Antioxidant and Antibacterial Activities from Abies Extract. Sci. J. King Faisal. Univ. 2021, 22, 26–32. [Google Scholar] [CrossRef]
- Benouchenne, D.; Bellil, I.; Bensouici, C.; Yilmaz, M.A.; Akkal, S.; Keskinkaya, H.B.; Khelifi, D. GC-MS Chemical Profile, Antioxidant Ability, Antibacterial Effect, A-Glucosidase, A-Amylase and Acetylcholinesterase Inhibitory Activity of Algerian Fir Essential Oil. Jordan J. Biol. Sci. 2022, 15, 303–310. [Google Scholar]
- Meyer, B.N.; Ferrigni, N.R.; Putnam, J.E.; Jacobsen, L.B.; Nicholas, D.E.; McLaughlin, J.L. Brine Shrimp: A Convenient General Bioassay for Active Plant Constituents. J. Med. Plant Res. 1982, 45, 31–34. [Google Scholar] [CrossRef]
- Fernandes, B.T.; FrojuelloSegretti, C.F.; Polli, M.C.; Parise-Filho, R. Analysis of the Applicability and Use of Lipinski’s Rule for Central Nervous System Drugs. Lett. Drug Des. Discov. 2016, 13, 999–1006. [Google Scholar] [CrossRef]
- Veber, D.F.; Stephen, R.J.; Hung, Y.C.; Smith, B.R.; Ward, K.W.; Kenneth, D.K. Molecular properties that influence the oral bioavailability of drug candidates. J. Med. Chem. 2002, 45, 2615. [Google Scholar] [CrossRef] [PubMed]
- Pires, D.E.V.; Blundell, T.L.; Ascher, D.B. pkCSM: Predicting small-molecule pharmacokinetic properties using graph-based signatures. J. Med. Chem. 2015, 58, 9. [Google Scholar] [CrossRef] [PubMed]
- Nur, W.; Atiqah, W.; Razauden, M.Z.; Farediah, A.; Mohd, A.; Che, Y. Antioxidant and tyrosinase inhibition activities of Eurycoma longifolia and Swietenia macrophylla. J. Appl. Pharm. Sci. 2015, 5, 6–10. [Google Scholar]
- Kim, S.S.; Hyun, C.; Choi, Y.H.; Lee, N.H. Tyrosinase inhibitory activities of the compounds isolated from Neolitseaaciculata (Blume) Koidz. J. Enzym. Inhib. Med. Chem. 2013, 28, 6366. [Google Scholar] [CrossRef] [PubMed]
- Zolghadri, S.; Bahrami, A.; Hassan Khan, M.T.; Munoz-Munoz, J.; Garcia-Molina, F.; Garcia-Canovas, F.; Saboury, A.A. A comprehensive reviewontyrosinaseinhibitors. J. Enzyme Inhib. Med. Chem. 2019, 34, 279–309. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Zhe, W.; Wei, S.; Zhenli, Z.; Yong, Z. Isolation of proanthocyanidins from Pinus thunbergii needles and tyrosinase inhibition activity. Process Biochem. 2021, 100, 24551. [Google Scholar] [CrossRef]
- Li, W.; Zhang, Y.; Shi, S.; Gen, Y.; Liu, Z.; Wang, J.; Kang, W. Spectrum-effect relationship of antioxidant and tyrosinase activity with Malus pumila flowers by UPLC-MS/MS and component knock-out method. Food Chem. Toxicol. 2019, 133, 110754. [Google Scholar] [CrossRef] [PubMed]
- Mierziak, J.; Kostyn, K.; Kulma, A. Flavonoids as important molecules of plant interactions with the environment. Molecules 2014, 19, 16240–16265. [Google Scholar] [CrossRef] [PubMed]
- Şöhretoğlu, D.; Suat, S.; Burak, B.; Arzu, Ö. Tyrosinase inhibition by some flavonoids: Inhibitory activity, mechanism by in vitro and in silico studies. Bioorganic Chem. 2018, 81, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.X.; Nhan, T.N.; Mai, H.K.N.; Tho, H.L.; Truong, N.D.; Tran, M.H.; Mai Thanh, T.N. Tyrosinase inhibitory activity of flavonoids from Artocarpus heterophyllous. Chem. Cent. J. 2016, 10, 49. [Google Scholar] [CrossRef]
- Cockrem, M.C.M.; Meyer, R.A. Recovery of n-Butanol from Dilute Solution by Extraction. Sep. Sci. Technol. 1986, 21, 1059–1074. [Google Scholar] [CrossRef]
- Ahmed, W.; Mushtaq, A.; Rauf, A.; Sania, F.; Zakir, K. Phytochemistry and cytotoxicity of Prosopis spicigera using Brine Shrimp Lethality assay. J. Herb. Med. 2014, 3, 14–16. [Google Scholar]
- Akter, R.; Mohammed, A.; Satter, M.S.; Khan, M.S.; Rahman, N.U. Cytotoxic Effect of Five Medicinal Plants Extracts Using Brine Shrimp (Artemia salina) test. Bangladesh J. Sci. Ind. Res. 2012, 47, 133–136. [Google Scholar] [CrossRef]
- Sarah, Q.S.; Anny, F.C.; Misbahuddin, M. Brine shrimp lethality assay. Bangladesh J. Pharmacol. 2017, 12, 186–189. [Google Scholar] [CrossRef]
- Solis, P.N.; Wright, C.W.; Anderson, M.M.; Gupta, M.P.; Phillipson, J.D. A microwell cytotoxicity assay using Artemia salina (brine shrimp). PlantaMed. 1993, 59, 250–252. [Google Scholar] [CrossRef]
- Responte, M.A.; Maria, R.B.; Dacar, O.M.N.; Mylene, M.U. Brine shrimp lethality assay of whole plant extracts of Eleusine indica. AAB Bioflux 2015, 7, 90–95. [Google Scholar]
- Nieto, G.; Bañón, S.; Garrido, M.D. Incorporation of thyme leaves in the diet of pregnant and lactating ewes: Effect on the fatty acid profile of lamb. Small Rumin. Res. 2012, 105, 140–147. [Google Scholar] [CrossRef]
- Martínez, J.; Nieto, G.; Castillo, J.; Ros, G. Influence of in vitro gastrointestinal digestion and/or grape seed extract addition on antioxidant capacity of meat emulsions. LWT 2014, 59, 834–884. [Google Scholar] [CrossRef]
- Martínez, L.; Ros, G.; Nieto, G. Fe, Zn and Se bioavailability in chicken meat emulsions enriched with minerals, hydroxytyrosol and extra virgin olive oil as measured by Caco-2 cell model. Nutrients 2018, 10, 969. [Google Scholar] [CrossRef]
- Martínez, J.; Nieto, G.; Ros, G. Total antioxidant capacity of meat and meat products consumed in a reference ‘Spanish standard diet’. Int. J. Food Sci. Technol. 2014, 49, 12577. [Google Scholar] [CrossRef]
- Martínez, L.; Jongberg, S.; Ros, G.; Skibsted, L.H.; Nieto, G. Plant derived ingredients rich in nitrates or phenolics for protection of pork against protein oxidation. Food Res. Int. 2020, 129, 108789. [Google Scholar] [CrossRef]
- Nieto, G. A Review on Applications and Uses ofThymusin the Food Industry. Plants 2020, 9, 961. [Google Scholar] [CrossRef] [PubMed]
- Milla, P.; Peñalver, R.; Nieto, G. Health Benefits of Uses and Applications ofMoringa oleiferain Bakery Products. Plants 2021, 10, 318. [Google Scholar] [CrossRef] [PubMed]
- Brighent, I.M.C.; Diad, M.; Verdi, L.G.; Pizzolatti, M.G. Antioxidant Activity and Total Phenolic Content of Some Brazilian Species. Pharm. Biol. 2008, 45, 156–161. [Google Scholar] [CrossRef]
- Söderberg, T.A.; Johansson, A.; Gref, R. Toxic effects of some conifer resin acids and tea tree oil on human epithelial and fibroblast cells. Toxicology 1996, 107, 99–109. [Google Scholar] [CrossRef]
- Lima, C.; Madureira, J.; Melo, R.; Carolino, M.M.; Noronha, J.P.; Margaça, F.M.A.; Verde, S.C. A biodegradation bench study of cork wastewater using gamma radiation. J. Adv. Oxid. Technol. 2016, 19, 73–78. [Google Scholar] [CrossRef]
- Saleem, U.; Amin, S.; Ahmad, B.; Azeem, H.; Anwar, F.; Mary, S. Acute oral toxicity evaluation of aqueous ethanolic extract of Saccharum munja Roxb. roots in albino mice as per OECD 425 TG. Toxicol. Rep. 2017, 4, 580–585. [Google Scholar] [CrossRef]
- Deveci, E.; Tel-çayan, G.; Duru, M.E. Phenolic profile, antioxidant, anticholinesterase, and anti-tyrosinase activities of the various extracts of Ferulaelaeochytris and Sideritis stricta. Int. J. Food Prop. 2018, 21, 771–783. [Google Scholar] [CrossRef]
- Ogbonnia, S.O.; Mbaka, G.O.; Anyika, E.N.; Osegbo, O.M.; Igbokwe, N.H. Evaluation of acute toxicity in mice and subchronic toxicity of hydro- ethanolic extract of Chromolaena odorata (L.) King and Robinson (Fam. Asteraceae) in rats. Agric. Biol. J. N. Am. 2010, 1, 859–865. [Google Scholar] [CrossRef]

| 30 min | 6 h | 24 h | 48 h | 7 days | 14 days | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Observation | C | Mtr | C | Mtr | C | Mtr | C | Mtr | C | Mtr | C | Mtr | |
| weight | N | N | N | N | N | N | N | N | N | N | N | N | N |
| Food consumption | N | N | N | N | N | N | N | N | N | N | N | N | N |
| Respiration | N | N | N | N | N | N | N | N | N | N | N | N | N |
| Tremors | A | A | A | A | A | A | A | A | A | A | A | A | A |
| Pains | A | A | A | A | A | A | A | A | A | A | A | A | A |
| Convulsions | A | A | A | A | A | A | A | A | A | A | A | A | A |
| Skin changset | A | A | A | A | A | A | A | A | A | A | A | A | A |
| Drowsiness | A | A | A | A | A | A | A | A | A | A | A | A | A |
| Sedation | A | A | A | A | A | A | A | A | A | A | A | A | A |
| Coma | A | A | A | A | A | A | A | A | A | A | A | A | A |
| Surviving/death | V | V | V | V | V | V | V | V | V | V | V | V | V |
| Body Weight (g) | |||
|---|---|---|---|
| Groups | 1st Day | 7th Days | 14th Days |
| Contrl | 24.00 ± 1.00 | 28.00 ± 1.73 | 26.00 ± 2.00 |
| EA (2000 mg/kg) | 22.66 ± 1.5 | 26.00 ± 1.00 | 26.00 ± 0.00 |
| n-BuOH (2000 mg/kg) | 25.33 ± 0.94 | 27.33 ± 1.69 | 28.66 ± 1.24 |
| Parameters | Unit | Control | EA (2000 mg/kg) | n-BuOH (2000 mg/kg) |
|---|---|---|---|---|
| Creatinine | mg/L | 2.4 | 3.1 * | 4.4 * |
| Urea | g/L | 0.50 | 0.45 | 0.43 |
| Parameters | Unit | Control | EA | n-BuOH |
|---|---|---|---|---|
| (2000 mg/kg) | ||||
| AST | UI/L | 105 | 137 * | 132 * |
| ALT | UI/L | 33 | 45 * | 111 * |
| Alkaline Phosphatase | UI/L | 98 | 209 * | 192 * |
| Total Bilirubine | mg/L | 2 | 2 | 2 |
| Direct Bilirubine | mg/L | 1 | 1 | 1 |
| Gamma-Glutamyl-Transferase | UI/L | 2 | 2 | 1 |
| Parameter | Unit | Control | EA | n-BuOH |
|---|---|---|---|---|
| (2000 mg/kg) | ||||
| Triglycerides | g/L | 1.26 | 1.88 | 0.86 |
| Total Cholesterol | g/L | 1.16 | 1.05 | 0.98 |
| Organ | T | EA | n-BuOH |
|---|---|---|---|
| Liver | 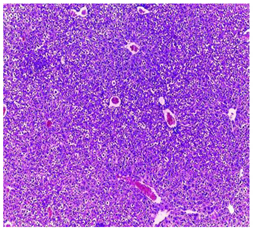 |  | 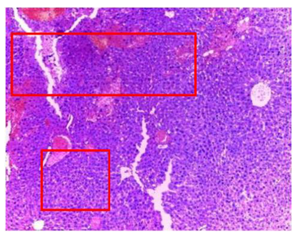 |
| Hepatic parenchyma with conserved architecture | Vascular congestion, balonization of cytoplasm with clear nucleus, presence of necrosis, acidophilic bodies, basophils, small hyperchromatic nucleus, lobular lymphocyte filtrate. | ||
| Kidneys |  |  |  |
| Round parenchyma surrounded by a fibro-adipose capsule of preserved architecture | Seat of vascular congestion with lesion of interstitial nephritis mainly made up of lymphocytes dispersed between the tubules and by sectors surrounding glomeruli. There was no objective glomerular damage on the limits of the sectors examined. Presence of surrenal gland with conserved morphology and cytology. | ||
| Lung | 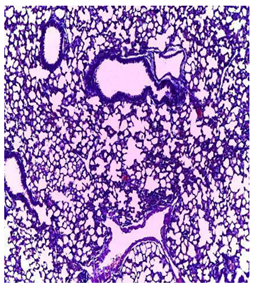 | 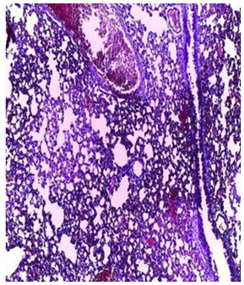 |  |
| A pulmonary parenchyma, made of optically empty cavity (alveoli) separated by fibrous septa | Lung parenchyma seat of vascular congestion The vessels have a hyalinised wall with the presence of haemorrhagic diffusion. | Presence of vascular congestion Presence of lymphocytes inflammatory infiltrate | |
| N° | Analyte | EA (µg/g) | n-BuOH (µg/g) | SMILES |
|---|---|---|---|---|
| 1 | Hesperidine | 7.83 | 42.02 | CC1C(C(C(C(O1)OCC2C(C(C(C(O2)OC3=CC(=C4C(=O)CC(OC4=C3)C5=CC(=C(C=C5)OC)O)O)O)O)O)O)O)O |
| 2 | protocatechic acid | 71.62 | N.D | C1=CC(=C(C=C1C(=O)O)O)O |
| 3 | chlorogenic acid | 15.59 | 9.66 | C1C(C(C(CC1(C(=O)O)O)OC(=O)C=CC2=CC(=C(C=C2)O)O)O)O |
| 4 | Luteolin-7-glucoside | 43.17 | 14.6 | C1=CC(=C(C=C1C2=CC(=O)C3=C(C=C(C=C3O2)OC4C(C(C(C(O4)CO)O)O)O)O)O)O |
| 5 | Hyperoside | 3370.96 | 399.91 | C1=CC(=C(C=C1C2=C(C(=O)C3=C(C=C(C=C3O2)O)O)OC4C(C(C(C(O4)CO)O)O)O)O)O |
| 6 | Rutin | 27.58 | 102.62 | CC1C(C(C(C(O1)OCC2C(C(C(C(O2)OC3=C(OC4=CC(=CC(=C4C3=O)O)O)C5=CC(=C(C=C5)O)O)O)O)O)O)O)O |
| 7 | Apigetrin | 192.56 | 23.19 | C1=CC(=CC=C1C2=CC(=O)C3=C(C=C(C=C3O2)OC4C(C(C(C(O4)CO)O)O)O)O)O |
| 8 | Quercitrin | 2300.33 | 23.19 | C[C@H]1[C@@H]([C@H]([C@H]([C@@H](O1)OC2=C(OC3=CC(=CC(=C3C2=O)O)O)C4=CC(=C(C=C4)O)O)O)O)O |
| 9 | Astragaline | 3391.36 | 147.22 | C1=CC(=CC=C1C2=C(C(=O)C3=C(C=C(C=C3O2)O)O)O[C@H]4[C@@H]([C@H]([C@@H]([C@H](O4)CO)O)O)O)O |
| 10 | Quercetin | 24.75 | N.D | C1=CC(=C(C=C1C2=C(C(=O)C3=C(C=C(C=C3O2)O)O)O)O)O |
| 11 | Luteolin | 2.41 | N.D | C1=CC(=C(C=C1C2=CC(=O)C3=C(C=C(C=C3O2)O)O)O)O |
| 12 | Apigenin | 6.64 | N.D | C1=CC(=CC=C1C2=CC(=O)C3=C(C=C(C=C3O2)O)O)O |
| a: Pharmacokinetic Properties | ||||||||||
| N | Analyte | Lipinski Rules | Absorption | Distribution | ||||||
| MW (g/mol) | log P | RT | A | D | Intest (%) | Skin (log Kp) | DV (log L/kg) | BBB (log BB) | ||
| 1 | Hesperidin | 610.565 | −1.1566 | 7 | 15 | 8 | 31.481 | −2.735 | 0.996 | −1.715 |
| 2 | Protocatechic acid | 154.121 | 0.796 | 1 | 3 | 3 | 71.174 | −2.727 | −1.298 | −0.683 |
| 3 | chlorogenic acid | 354.31 | −0.6459 | 4 | 8 | 6 | 36.377 | −2.735 | 0.581 | −1.407 |
| 4 | Luteolin-7-glucoside | 448.38 | −0.2445 | 4 | 11 | 7 | 37.556 | −2.735 | 0.884 | −1.564 |
| 5 | Hyperoside | 464.379 | −0.5389 | 4 | 12 | 8 | 37.556 | 0.884 | −1.564 | |
| 6 | Rutin | 610.521 | −1.6871 | 6 | 16 | 10 | 23.446 | 1.663 | −1.899 | |
| 7 | Apigetrin | 432.381 | 0.0499 | 4 | 10 | 6 | 37.609 | 0.342 | −1.391 | |
| 8 | Quercitrin | 448.38 | 0.4887 | 3 | 11 | 7 | 52.709 | 1.517 | −1.495 | |
| 9 | Astragalin | 448.38 | −0.2445 | 4 | 11 | 7 | 48.052 | 1.444 | −1.514 | |
| 10 | Quercetin | 302.238 | 1.988 | 1 | 7 | 5 | 77.207 | 1.559 | −1.098 | |
| 11 | Luteolin | 286.239 | 2.2824 | 1 | 6 | 4 | 81.13 | 1.153 | −0.907 | |
| 12 | Apigenin | 270.24 | 2.5768 | 1 | 5 | 3 | 93.25 | 0.822 | −0.734 | |
| b: Pharmacokinetic Properties | ||||||||||
| N | Analyte | Metabolsim | Clearance | Toxicity | ||||||
| P450 (Yes/No) | P450 Substrats | TC | Subs. OCT2 (Yes/No) | Hepatotoxicity (Yes/No) | MTD | |||||
| 1 | Hesperidine | No | No | 0.211 | No | No | 0.525 | |||
| 2 | protocatechic acid | No | No | 0.551 | 0.814 | |||||
| 3 | chlorogenic acid | No | No | 0.307 | −0.134 | |||||
| 4 | Luteolin-7-glucoside | No | No | 0.478 | 0.584 | |||||
| 5 | Hyperoside | No | No | 0.394 | 0.569 | |||||
| 6 | Rutin | No | No | −0.369 | 0.452 | |||||
| 7 | Apigetrin | No | No | 0.547 | 0.515 | |||||
| 8 | Quercitrin | No | No | 0.364 | 0.495 | |||||
| 9 | Astragalin | No | No | 0.462 | 0.582 | |||||
| 10 | Quercetin | Inhi. CYP1A2 | No | 0.407 | 0.499 | |||||
| 11 | Luteolin | Inhi. CYP1A2 | No | 0.495 | 0.499 | |||||
| 12 | Apigenin | Inhi. CYP1A2 and CYP2C19 | No | 0.566 | 0.328 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benouchenne, D.; Bellil, I.; Tachour, S.H.; Akkal, S.; Djeghim, H.; Kebaili, F.F.; Nieto, G.; Khelifi, D. Tyrosinase Inhibitory Ability and In Vitro, In Vivo Acute Oral and In Silico Toxicity Evaluation of Extracts Obtained from Algerian Fir (Abiesnumidica de Lannoy ex CARRIERE) Needles. Plants 2022, 11, 2389. https://doi.org/10.3390/plants11182389
Benouchenne D, Bellil I, Tachour SH, Akkal S, Djeghim H, Kebaili FF, Nieto G, Khelifi D. Tyrosinase Inhibitory Ability and In Vitro, In Vivo Acute Oral and In Silico Toxicity Evaluation of Extracts Obtained from Algerian Fir (Abiesnumidica de Lannoy ex CARRIERE) Needles. Plants. 2022; 11(18):2389. https://doi.org/10.3390/plants11182389
Chicago/Turabian StyleBenouchenne, Djamila, Ines Bellil, Sana Hazar Tachour, Salah Akkal, Hanène Djeghim, Fethi Farouk Kebaili, Gema Nieto, and Douadi Khelifi. 2022. "Tyrosinase Inhibitory Ability and In Vitro, In Vivo Acute Oral and In Silico Toxicity Evaluation of Extracts Obtained from Algerian Fir (Abiesnumidica de Lannoy ex CARRIERE) Needles" Plants 11, no. 18: 2389. https://doi.org/10.3390/plants11182389
APA StyleBenouchenne, D., Bellil, I., Tachour, S. H., Akkal, S., Djeghim, H., Kebaili, F. F., Nieto, G., & Khelifi, D. (2022). Tyrosinase Inhibitory Ability and In Vitro, In Vivo Acute Oral and In Silico Toxicity Evaluation of Extracts Obtained from Algerian Fir (Abiesnumidica de Lannoy ex CARRIERE) Needles. Plants, 11(18), 2389. https://doi.org/10.3390/plants11182389







