A Robotic System to Anchor a Patient in a Lateral Position and Reduce Nurses’ Physical Strain
Abstract
:1. Introduction
- If possible, the patient anchors themself on the side;
- The use of anchoring cushions;
- A second nurse anchors the patient.
- Evaluation of a telemanipulation system for anchoring a patient in a lateral position with professional caregivers;
- Demonstration of its physical relief potential;
- Investigation of its acceptance and trust in human–robot collaboration experienced by nurses.
2. Materials and Methods
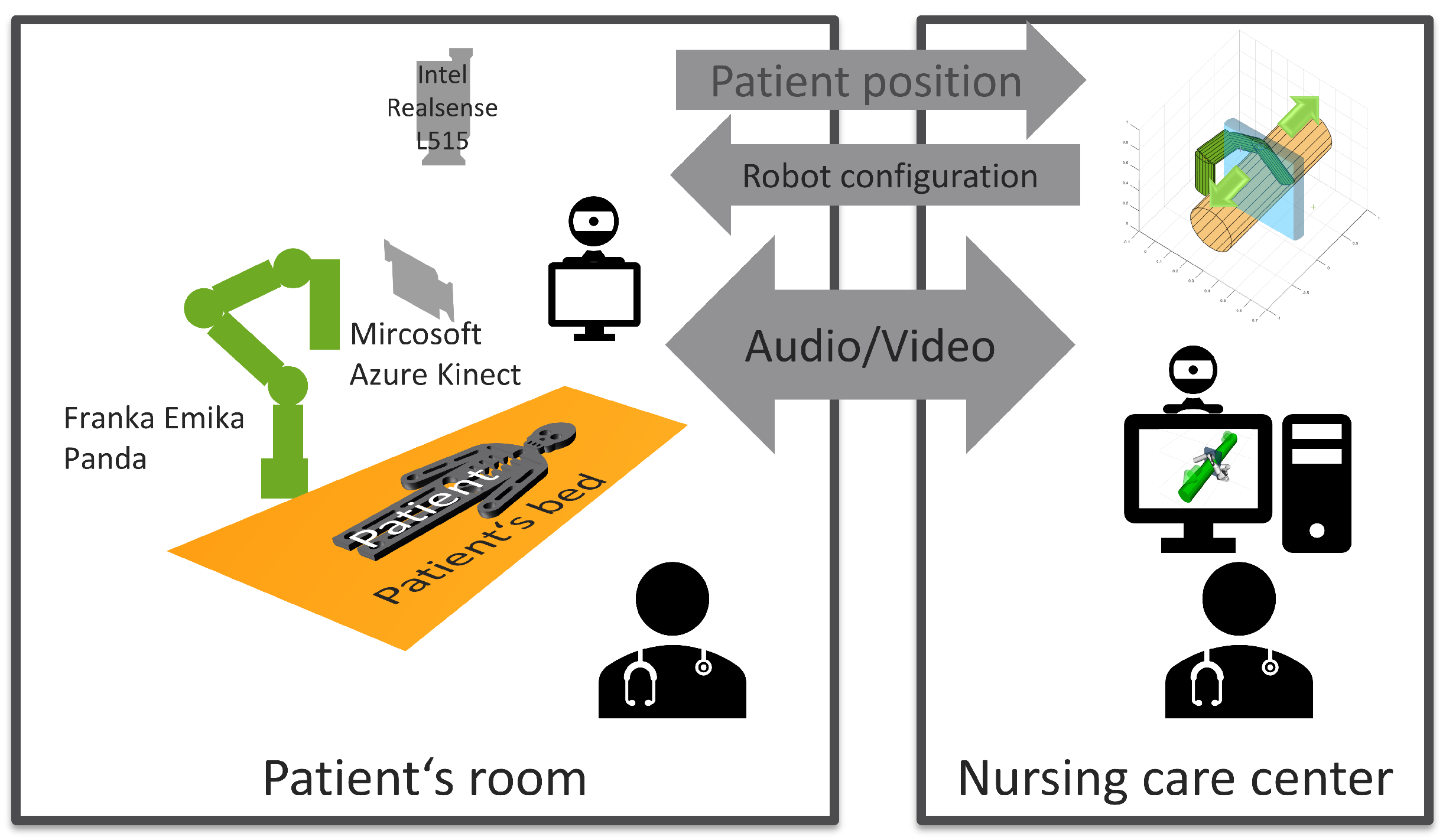
2.1. System Design
- Preparation: Addressing and uncovering the patient, and preparation of washing utensils.
- Mobilization to the side: Mobilize the patient onto the side so that the patient’s back is freely accessible.
- Holding until the robot takes over (only when performed with robotic assistance): Communication between the bedside nurse and remote nurse to coordinate where the robot should hold the patient. The remote nurse then commands the robot into this position. If necessary, the position is corrected.
- Washing patient’s back (main phase of examination): Washing the patient’s back while holding the patient on their side either manually or with the robot. The nurses’ postures are measured throughout this phase.
- Holding until the robot has moved back into its parked position (only when performed with robotic assistance): Taking over the patient from the robot and requesting the release of the robot from the remote nurse. The remote nurse moves the robot to its parking position.
- Mobilization to the back position: Mobilizing the patient onto their back.
- Postprocessing: Covering up the patient and performing further follow-up work (such as disposal of washing utensils).
2.2. System Implementation
2.2.1. The Robot
2.2.2. Pose Generation and Patient Anchoring
2.2.3. Safety
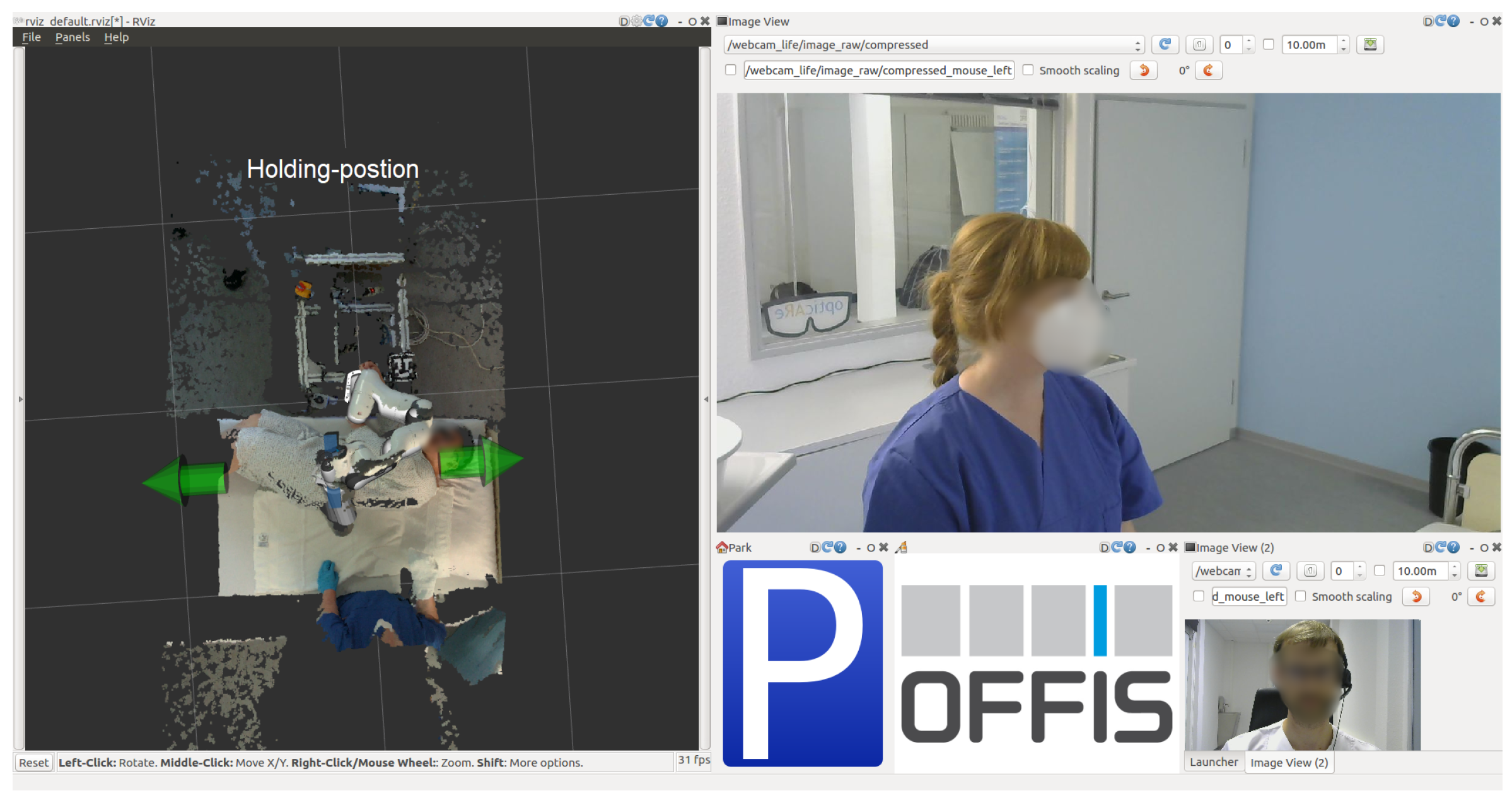
2.2.4. User Interface
- Three-dimensional viewer displaying point clouds of the on-site scene;
- Webcam interface.
2.2.5. Position Recognition and Measuring Dimensions
2.3. User Study
2.3.1. Conditions
- Washing the back without robotic assistance;
- Washing the back with robotic assistance;
- Remotely controlling the robot.
- H1: Nurses’ working posture improves;
- H2: Execution times increase;
- H3: The system is helpful and collaboration-fluent;
- H4: The remote control is easy to use;
- H5: The system is pleasant from the patient’s point of view.
2.3.2. Tasks
- Task 1 (baseline measurement): Position and anchor the patient manikin on its side with one hand while washing the patient manikin’s back with the other.
- Task 2 (intervention measurement): Request support from subject_2, who selects a suitable position for the robot contact on the patient manikin and sends the control command to the robot. Subject_1 now has both hands free and washes the back of the patient manikin. Subject_2 then asks for the robot to let go of the patient manikin. In both cases, the patient is now mobilized back into the supine position.
- Optional self-experience: Instead of the patient manikin, the participant lies down in the bed and is held on their side by the robot.
2.3.3. Scenario Selection
2.3.4. Participants
2.3.5. Procedure
2.3.6. Study Limitations
3. Results
3.1. Remote Control Usability Rating
“So, it recognizes the person, but maybe that would be quite good again if you can still correct it manually a bit.” (hospital nurse, orthopedic care)
3.2. Posture Change
3.2.1. Posture Improvements
3.2.2. Posture Aggravations
3.3. Execution Times
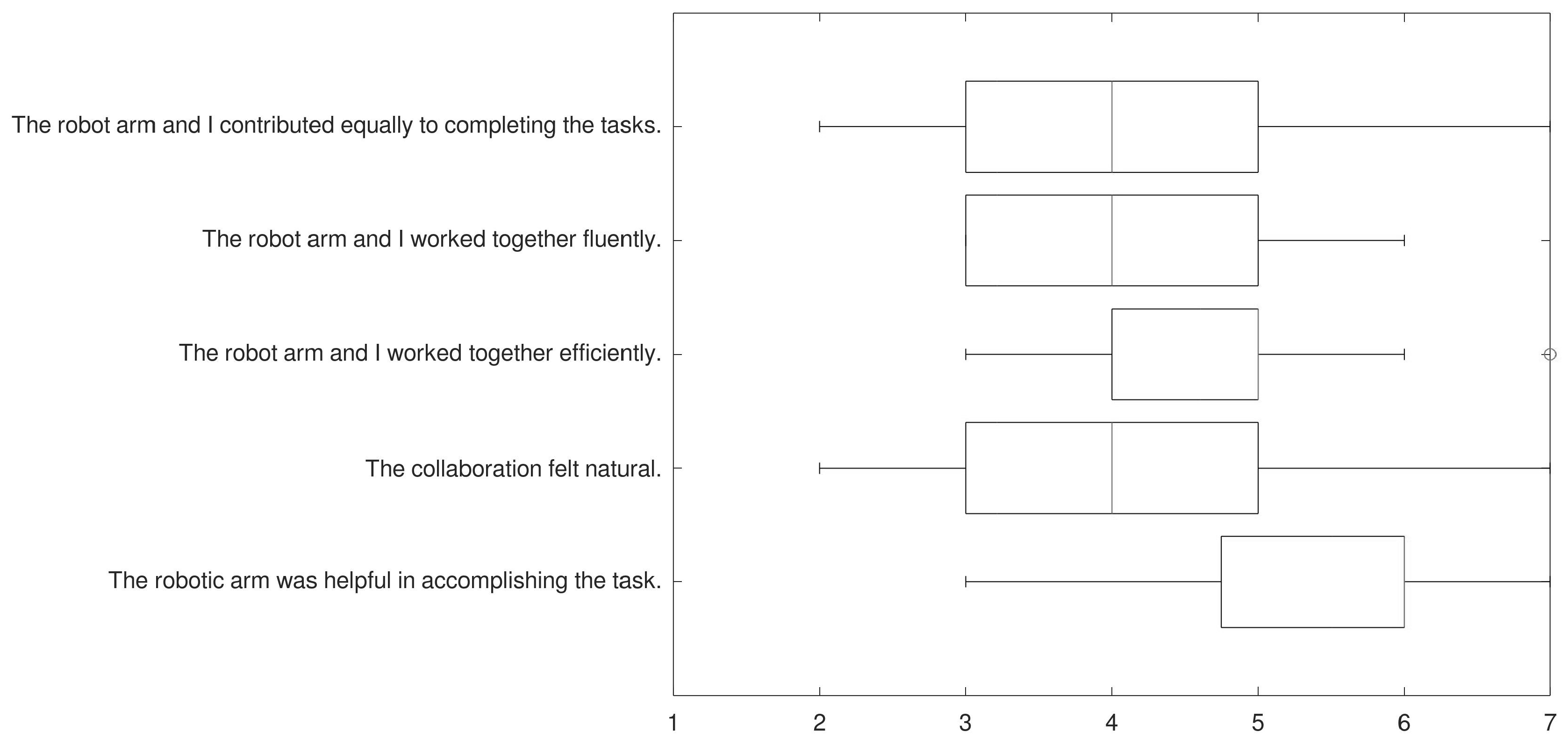
3.4. Collaboration Rating
“I had to check first ‘Is it holding?’ and then [thought] ‘Okay, now I can let go of my hands. So, you first have to check whether it really holds [the patient]”(hospital nurse in training)
“But I also had the feeling, at the PC [remote control], after I got to know the robot, that I can trust it to make the movement, because my colleague is also standing there and can intervene if necessary. But I didn’t really have the fear that anything could happen. I had the impression that it didn’t involve so much force, but rather precision.”(hospital nurse, emergency care)
“[the robot] also stopped immediately when it touched the patient. There was no fear that it would crush the patient or push them out of the bed.”(hospital nurse in training)
“And I actually noticed that when I [held the patient] myself, you bend forward and use a lot of force. But the thing, the robot, has already taken this force away from you. So that you were no longer standing so strenuously.”(long-term care nurse)
“That was totally noticeable: This pressure on the wrist the first time, when you did it alone, and then the second time you just put your hand on [the patient] very lightly. I think that was really good.”(long-term care nurse)
3.5. Participants’ Self-Experience and Perspectives on Implementation in Nursing Practice
“That it worked so well the first time, too. I was pretty convinced then. Well, overwhelmed actually. That was good.”(hospital nurse, emergency care)
“I liked the on-site control. You’re a bit faster. That also worked well and it was spot on.”(hospital nurse, geriatric care)
“The video connection was very helpful. The fact that you can see each other and that you’re not talking to someone without a face, so to speak, but to someone who is there and whom you can trust in the situation.”(hospital nurse, emergency care)
“Of course, you’re a bit uncertain at the beginning. But of course, you quickly learned that and, well, I was quite impressed by the robot then.”(hospital nurse, orthopedic care)
“I think that will also become the trend. Nursing care, everyone knows, will really need something like that later on.”(ambulatory care nurse, occupational therapy)
“Due to the fact that there is also an increased shortage of personnel, I think it’s good that you can replace one person with this robot, so to speak. That the other worker is no longer as physically stressed as if they had to do it alone”(long-term care nurse)
“It is questionable at the moment, how it can be implemented and how it can be accepted. Because where is [the person needed to operate the robot] going to come from? What training does this person need? To be able to put themselves into such aspects as the safety of the patient and so on? So, does it really have to be a nurse or not? I think that if it has to be a nurse, then it will be even more difficult to ensure acceptance, because then you’re more likely to say, “No, they should rather work at the bedside”.(hospital nurse, emergency care)
“Because when this is controlled by others, you can’t really say yourself, even as a caregiver at the bedside, what will happen. And you can’t really give the patient a proper warning.”(hospital nurse in training)
“If I had a patient in the practice now, maybe an older patient, who can’t quite process it cognitively anymore, if I were to somehow explain to this patient that the robot is about to come close and I myself can’t explain where it’s coming from, that panic might break out in the patient at that moment. And of course, I can’t control that very well if I don’t know what will happen next with the robot when it goes its own way.”(hospital nurse in training)
4. Discussion
- The greatest improvement is seen in the left shoulder, the arm with which the patient is held in the manually conducted version of the task. This arm no longer has to be stretched forward and upward to hold the patient. This reduces the time spent at critical joint angles.
- The fact that the arms no longer need to be extended means that the nurses work more with bent elbows when working positioned above the bed and also when handling the wash bowl. This explains the deterioration in this joint.
- Another significant improvement affects the lower back, as the nurses can perform their work more upright with robotic support and no longer have to twist their backs when reaching for the wash bowl.
- This new upright working position also relieves the strain on the neck, as the head no longer has to be placed at the nape of the neck to see the patient’s back while working on the patient.
- The free physical mobility gained by the nurse in front of the bed leads to an improvement in adduction and abduction in the left hip. This is because the nurse can now walk to the wash bowl and does not have to stay with one leg by the bed to still reach and hold the patient while taking a step toward the wash bowl with the other.
- The deterioration in hip flexion and extension can be attributed to a measurement error. When reviewing the video material, it was noticed that the participating nurses touched the bed with an upper leg sensor during postprocessing in the round without robotic assistance and moved the sensor in the process.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| DOF | Degrees of freedom |
| D-P-HRI | Ddirect physical human–robot interaction |
| GUIs | Graphical user interfaces |
| HRI | Human–robot interaction |
| LIFE | Laboratory for Intensive Care Facility Experience |
| NARS | Negative attitudes toward robots scale |
| NASSS | Non-adoption, abandonment, scale-up, spread, and sustainability |
| OWAS | Ovako Working Posture Analysing System |
| AC | OWAS action category |
| RGBD | Red green blue depth |
| SDK | Doftware development kit |
| SD | Standard Deviation |
| SUS | System Usability Scale |
Appendix A
| Mean | ||||||||
|---|---|---|---|---|---|---|---|---|
| Joint | Direction | With Robot | Without Robot | Test Type | Test Statistics | p-Value | Change | Comparison |
| Left shoulder | Vertical rotation | 1.364975641 | 1.791717388 | T | −4.54 | 0.000 | 23.82% | Better |
| Lower back | Lateral right flexion/Lateral Left flexion | 1.477045997 | 1.741157908 | T | −3.82 | 0.001 | 15.17% | Better |
| Lower back | Right Rotation/Left Rotation | 1.178020113 | 1.375876848 | T | −2.93 | 0.005 | 14.38% | Better |
| Neck | Lateral right flexion/Lateral Left flexion | 1.845710155 | 2.0750751 | T | −2.73 | 0.008 | 11.05% | Better |
| Right elbow | External rotation/Internal rotation | 1.434272794 | 1.608729251 | T | −2.77 | 0.007 | 10.84% | Better |
| Left hip | Abduction/Adduction | 1.154333162 | 1.255075487 | T | −2.22 | 0.021 | 8.03% | Better |
| Left shoulder | External rotation/Internal rotation | 1.58502534 | 1.719954897 | T | −1.29 | 0.108 | 7.84% | No Difference |
| Right shoulder | External rotation/Internal rotation | 1.32089116 | 1.426196202 | T | −2.21 | 0.021 | 7.38% | Better |
| Neck | Right Rotation/Left Rotation | 2.189780824 | 2.354638786 | T | −2.48 | 0.013 | 7.00% | Better |
| Right shoulder | Vertical rotation | 1.449327956 | 1.526522768 | T | −1.32 | 0.103 | 5.06% | No Difference |
| Right shoulder | Horizontal external rotation/Horizontal internal rotation | 1.998104448 | 2.010122367 | T | −0.17 | 0.434 | 0.60% | No Difference |
| Left knee | Flexion/Extension | 1 | 1 | T | − | 0.000 | 0.00% | No Difference |
| Right knee | Flexion/Extension | 1.000019072 | 1 | W | 1.00 | 0.159 | 0.00% | No Difference |
| Left elbow | External rotation/Internal rotation | 1.301889842 | 1.285519853 | T | 0.26 | 0.400 | −1.27% | No Difference |
| Right hip | Abduction/Adduction | 1.175635105 | 1.159614799 | W | 48.00 | 0.752 | −1.38% | No Difference |
| Right hip | External rotation/Internal rotation | 1.930877977 | 1.864066544 | W | 69.00 | 0.490 | −3.58% | No Difference |
| Left hip | External rotation/Internal rotation | 1.394146207 | 1.322021907 | T | 0.75 | 0.232 | −5.46% | No Difference |
| Neck | Flexion/Extension | 1.721764675 | 1.61007867 | W | 88.00 | 0.161 | −6.94% | No Difference |
| Lower back | Flexion/Extension | 1.173362187 | 1.087390638 | W | 35.00 | 0.069 | −7.91% | No Difference |
| Left shoulder | Horizontal external rotation/Horizontal internal rotation | 2.11592065 | 1.944331763 | T | 1.53 | 0.073 | −8.83% | No Difference |
| Right knee | External rotation/Internal rotation | 1.575774722 | 1.421327385 | W | 98.00 | 0.065 | −10.87% | No Difference |
| Right hip | Flexion/Extension | 1.123942992 | 1.011559561 | W | 36.00 | 0.006 | −11.11% | Worse |
| Right elbow | Flexion/Extension | 1.393919137 | 1.253911445 | T | 2.23 | 0.021 | −11.17% | Worse |
| Left hip | Flexion/Extension | 1.134343948 | 1.020327317 | W | 45.00 | 0.004 | −11.17% | Worse |
| Left elbow | Flexion/Extension | 1.337373204 | 1.060275391 | T | 4.62 | 0.000 | −26.13% | Worse |
Appendix B
| Characteristic | N (%) |
|---|---|
| If Not Stated Otherwise | |
| Age in years (mean, SD) | 28.8 (8.4) |
| Work experience in years (mean, SD) | 7.0 (6.4) |
| Qualification | |
| registered nurse | 9 (56.3) |
| nurse assistant | 2 (12.5) |
| other | 5 (31.3) |
| Place of work | |
| home care | 1 (6.3) |
| nursing home | 4 (25.0) |
| hospital | 11 (68.8) |
| Frequency of positioning or mobilizing patients | |
| several times daily/very frequently | 9 (56.3) |
| occasional daily/rather frequently | 0 |
| not daily but weekly/rather rarely | 6 (37.5) |
| only on special occasions/very rarely | 1 (6.3) |
| Time spent using a computer during work hours | |
| more than half of working time/more than 4 h | 2 (12.5) |
| a quarter to a half of working time/2 to 4 h | 2 (12.5) |
| less than a quarter of working time/less than 2 h | 12 (75.0) |
| Gaming leisure activity | |
| yes, mainly using a keyboard and mouse | 1 (6.3) |
| yes, mainly using a controller | 2 (12.5) |
| no | 13 (81.3) |
| Cooperation in everyday work as a real team | |
| yes | 12 (75.0) |
| no | 4 (25.0) |
| NARS-Score (mean, SD) | |
| S1: Negative attitudes toward situations of interaction with robots | 4.3 (0.8) |
| S2: Negative attitudes toward the social influence of robots | 3.2 (1.0) |
| S3: Negative attitudes toward emotions in interaction with robots | 2.9 (1.0) |
| total | 3.6 (1.1) |
References
- Chen, T.L.; Kemp, C.C. A Direct Physical Interface for Navigation and Positioning of a Robotic Nursing Assistant. Adv. Robot. 2011, 25, 605–627. [Google Scholar] [CrossRef]
- Baum, F.; Beck, B.B.; Fischer, B.; Glüsing, R.; Graupner, I.; Kuhn, S.; Müller, A.; Stabel, S.; Wortmann, N. Prävention von Rückenbeschwerden; Berufsgenossenschaft für Gesundheitsdienst und Wohlfahrtspflege (BGW): Hamburg, Germany, 2018. [Google Scholar]
- Jäger, M.; Jordan, C.; Theilmeier, A.; Wortmann, N.; Kuhn, S.; Nienhaus, A.; Luttmann, A. Analyse der Lumbalbelastung beim manuellen Bewegen von Patienten zur Prävention biomechanischer Überlastungen von Beschäftigten im Gesundheitswesen. Zentralblatt Für Arbeitsmedizin Arbeitsschutz Ergon. 2014, 64, 98–112. [Google Scholar] [CrossRef]
- Iblasi, A.S.; Aungsuroch, Y.; Gunawan, J.; Gede Juanamasta, I.; Carver, C. Repositioning Practice of Bedridden Patients: An Evolutionary Concept Analysis. SAGE Open Nurs. 2022, 8, 237796082211064. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, K.; Kuhlmey, A.; Greß, S.; Klauber, J.; Schwinger, A. (Eds.) Pflege-Report 2019; Springer: Berlin/Heidelberg, Germany, 2020; pp. 283–294. [Google Scholar] [CrossRef]
- World Health Organization. State of the World’s Nursing 2020: Investing in Education, Jobs and Leadership; Technical Report; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Hülsken-Giesler, M. Technische Assistenzsysteme in der Pflege in pragmatischer Perspektive der Pflegewissenschaft. In Technisierung Des Alltags; Franz Steiner Verlag: Stuttgart, Germany, 2015; Volume 117. [Google Scholar] [CrossRef]
- Fifelski-von Böhlen, C.; Brinkmann, A.; Kowalski, C.; Meyer, O.; Hellmers, S.; Hein, A. Reducing Caregiver’s Physical Strain in Manual Patient Transfer with Robot Support. In Proceedings of the 2020 5th International Conference on Automation, Control and Robotics Engineering (CACRE), Dalian, China, 19–20 September 2020; Liu, L., Wu, Q., Eds.; IEEE: Piscataway, NJ, USA, 2020; pp. 189–194. [Google Scholar]
- Seibert, K.; Domhoff, D.; Huter, K.; Krick, T.; Rothgang, H.; Wolf-Ostermann, K. Application of digital technologies in nursing practice: Results of a mixed methods study on nurses’ experiences, needs and perspectives. Z. Für Evidenz Fortbild. Und Qual. Gesundheitswesen 2020, 158–159, 94–106. [Google Scholar] [CrossRef]
- Sparrow, R.; Sparrow, L. In the hands of machines? The future of aged care. Minds Mach. 2006, 16, 141–161. [Google Scholar] [CrossRef]
- Langensiepen, S.; Nielsen, S.; Madi, M.; Siebert, M.; Körner, D.; Elissen, M.; Meyer, G.; Stephan, A. Nutzerorientierte Bedarfsanalyse zum potenziellen Einsatz von Assistenzrobotern in der direkten Pflege. Pflege 2022. [Google Scholar] [CrossRef]
- Deutscher Ethikrat. Robotik für Gute Pflege; Deutschen Ethikrat: Berlin, Germany, 2020; pp. 1–60. [Google Scholar]
- Nieto Agraz, C.; Pfingsthorn, M.; Gliesche, P.; Eichelberg, M.; Hein, A. A Survey of Robotic Systems for Nursing Care. Front. Robot. AI 2022, 9, 832248. [Google Scholar] [CrossRef]
- Lee, J.Y.; Song, Y.A.; Jung, J.Y.; Kim, H.J.; Kim, B.R.; Do, H.K.; Lim, J.Y. Nurses’ needs for care robots in integrated nursing care services. J. Adv. Nurs. 2018, 74, 2094–2105. [Google Scholar] [CrossRef]
- Al-Abtah, J.; Ammann, A.; Bensch, S.; Dörr, B.; Elbert-Maschke, D. I Care Pflege; Thieme: New York, NY, USA, 2015. [Google Scholar]
- Hignett, S. Postural analysis of nursing work. Appl. Ergon. 1996, 27, 171–176. [Google Scholar] [CrossRef]
- Gliesche, P.; Kowalski, C.; Pfingsthorn, M.; Hein, A. Commanding a Whole-Arm Manipulation Grasp Configuration with One Click: Interaction Concept and Analytic IK Method. In Proceedings of the 2021 30th IEEE International Conference on Robot and Human Interactive Communication (RO-MAN), Vancouver, BC, Canada, 8–12 August 2021; Rossi, S., Soh, H., Eds.; IEEE: Piscataway, NJ, USA, 2021; pp. 573–579. [Google Scholar] [CrossRef]
- Quigley, M.; Conley, K.; Gerkey, B.; Faust, J.; Foote, T.; Leibs, J.; Wheeler, R.; Ng, A.Y. ROS: An open-source Robot Operating System. In Proceedings of the ICRA Workshop on Open Source Software, Kobe, Japan, 12–17 May 2009; Volume 3. [Google Scholar]
- Coleman, D.; Sucan, I.; Chitta, S.; Correll, N. Reducing the Barrier to Entry of Complex Robotic Software: A MoveIt! Case Study. J. Softw. Eng. Robot. 2014, 5, 3–16. [Google Scholar] [CrossRef]
- Romero-Ramirez, F.J.; Muñoz-Salinas, R.; Medina-Carnicer, R. Speeded up detection of squared fiducial markers. Image Vis. Comput. 2018, 76, 38–47. [Google Scholar] [CrossRef]
- Albert, J.A.; Owolabi, V.; Gebel, A.; Brahms, C.M.; Granacher, U.; Arnrich, B. Evaluation of the pose tracking performance of the azure kinect and kinect v2 for gait analysis in comparison with a gold standard: A pilot study. Sensors 2020, 20, 5104. [Google Scholar] [CrossRef] [PubMed]
- Karhu, O.; Kansi, P.; Kuorinka, I. Correcting working postures in industry: A practical method for analysis. Appl. Ergon. 1977, 8, 199–201. [Google Scholar] [CrossRef]
- Monod, H.H.; Kapitaniak, B. Ergonomie; Masson: Paris, France, 2003; p. 286. [Google Scholar]
- Brooke, J. SUS—A quick and dirty usability scale. In Usability Evaluation in Industry; Jordan, P.W., Thomas, B., McClelland, I.L., Weerdmeester, B., Eds.; CRC Press: Boca Raton, FL, USA, 1996; Chapter 21; pp. 189–194. [Google Scholar]
- Hoffman, G. Evaluating Fluency in Human-Robot Collaboration. IEEE Trans. Hum. Mach. Syst. 2019, 49, 209–218. [Google Scholar] [CrossRef]
- Nomura, T.; Suzuki, T.; Kanda, T.; Kato, K. Measurement of negative attitudes toward robots. Interact. Stud. Soc. Behav. Commun. Biol. Artif. Syst. 2006, 7, 437–454. [Google Scholar] [CrossRef]
- Beaton, D.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Recommendations for the Cross-Cultural Adaptation of Health Status Measures; American Academy of Orthopaedic Surgeons: New York, NY, USA, 2002; Volume 12, pp. 1–9. [Google Scholar]
- Charalambous, G.; Fletcher, S.; Webb, P. The Development of a Scale to Evaluate Trust in Industrial Human–robot Collaboration. Int. J. Soc. Robot. 2016, 8, 193–209. [Google Scholar] [CrossRef]
- Lin, T.C.; Krishnan, A.U.; Li, Z. Intuitive, Efficient and Ergonomic Tele-Nursing Robot Interfaces: Design Evaluation and Evolution. ACM Trans. Hum. Robot. Interact. 2022, 11, 1–41. [Google Scholar] [CrossRef]
- Fehling, P.; Dassen, T. Motive und Hürden bei der Etablierung technischer Assistenzsysteme in Pflegeheimen: Eine qualitative Studie. Klin. Pflegeforschung 2017, 3, 61–71. [Google Scholar] [CrossRef]
- Bangor, A.; Kortum, P.; Miller, J. Determining what individual SUS scores mean: Adding an adjective rating scale. J. Usability Stud. 2009, 4, 114–123. [Google Scholar]
- Knibbe, N.E.; Knibbe, H.J.J. Postural load of nurses during bathing and showering of patients: Results of a laboratory study. Prof. Saf. 1996, 41, 37. [Google Scholar]
- Krick, T.; Huter, K.; Domhoff, D.; Schmidt, A.; Rothgang, H.; Wolf-Ostermann, K. Digital technology and nursing care: A scoping review on acceptance, effectiveness and efficiency studies of informal and formal care technologies. BMC Health Serv. Res. 2019, 19, 400. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, T.; Abimbola, S. The NASSS Framework—A Synthesis of Multiple Theories of Technology Implementation. Stud. Health Technol. Inform. 2019, 263, 193–204. [Google Scholar] [CrossRef] [PubMed]
- Langer, S.L.; Castro, F.G.; Chen, A.C.C.; Davis, K.C.; Joseph, R.P.; Kim, W.; Larkey, L.; Lee, R.E.; Petrov, M.E.; Reifsnider, E.; et al. Recruitment and retention of underrepresented and vulnerable populations to research. Public Health Nurs. 2021, 38, 1102–1115. [Google Scholar] [CrossRef] [PubMed]



| Max. [N] | ||||
|---|---|---|---|---|
| Joint | p | d | Movement | Anchoring |
| 1 | 500 | 50 | 20 | 20 |
| 2 | 500 | 50 | 20 | 35 |
| 3 | 500 | 50 | 18 | 20 |
| 4 | 500 | 20 | 18 | 45 |
| 5 | 500 | 20 | 16 | 25 |
| 6 | 500 | 20 | 14 | 45 |
| 7 | 10 | 10 | 13 | 25 |
| Scale Component | Mean (Standard Deviation) |
|---|---|
| Perceived robot motion and speed 1 | 5.4 (1.3) |
| Perceived safe cooperation 2 | 13.3 (1.7) |
| Perceived robot reliability 2 | 11.8 (1.1) |
| Total score 3 (mean, SD) | 30.5 (2.7) |
| Study | AC 1 | AC 2 | AC 3 | AC 4 |
|---|---|---|---|---|
| Our | 42.2 | 48.0 | 9.2 | 0.6 |
| Knibbe et al. [32] | 39.4 | 41.7 | 17.3 | 1.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hinrichs, P.; Seibert, K.; Arizpe Gómez, P.; Pfingsthorn, M.; Hein, A. A Robotic System to Anchor a Patient in a Lateral Position and Reduce Nurses’ Physical Strain. Robotics 2023, 12, 144. https://doi.org/10.3390/robotics12050144
Hinrichs P, Seibert K, Arizpe Gómez P, Pfingsthorn M, Hein A. A Robotic System to Anchor a Patient in a Lateral Position and Reduce Nurses’ Physical Strain. Robotics. 2023; 12(5):144. https://doi.org/10.3390/robotics12050144
Chicago/Turabian StyleHinrichs, Pascal, Kathrin Seibert, Pedro Arizpe Gómez, Max Pfingsthorn, and Andreas Hein. 2023. "A Robotic System to Anchor a Patient in a Lateral Position and Reduce Nurses’ Physical Strain" Robotics 12, no. 5: 144. https://doi.org/10.3390/robotics12050144
APA StyleHinrichs, P., Seibert, K., Arizpe Gómez, P., Pfingsthorn, M., & Hein, A. (2023). A Robotic System to Anchor a Patient in a Lateral Position and Reduce Nurses’ Physical Strain. Robotics, 12(5), 144. https://doi.org/10.3390/robotics12050144






