Multidirectional Overground Robotic Training Leads to Improvements in Balance in Older Adults
Abstract
1. Introduction
2. Materials and Methods
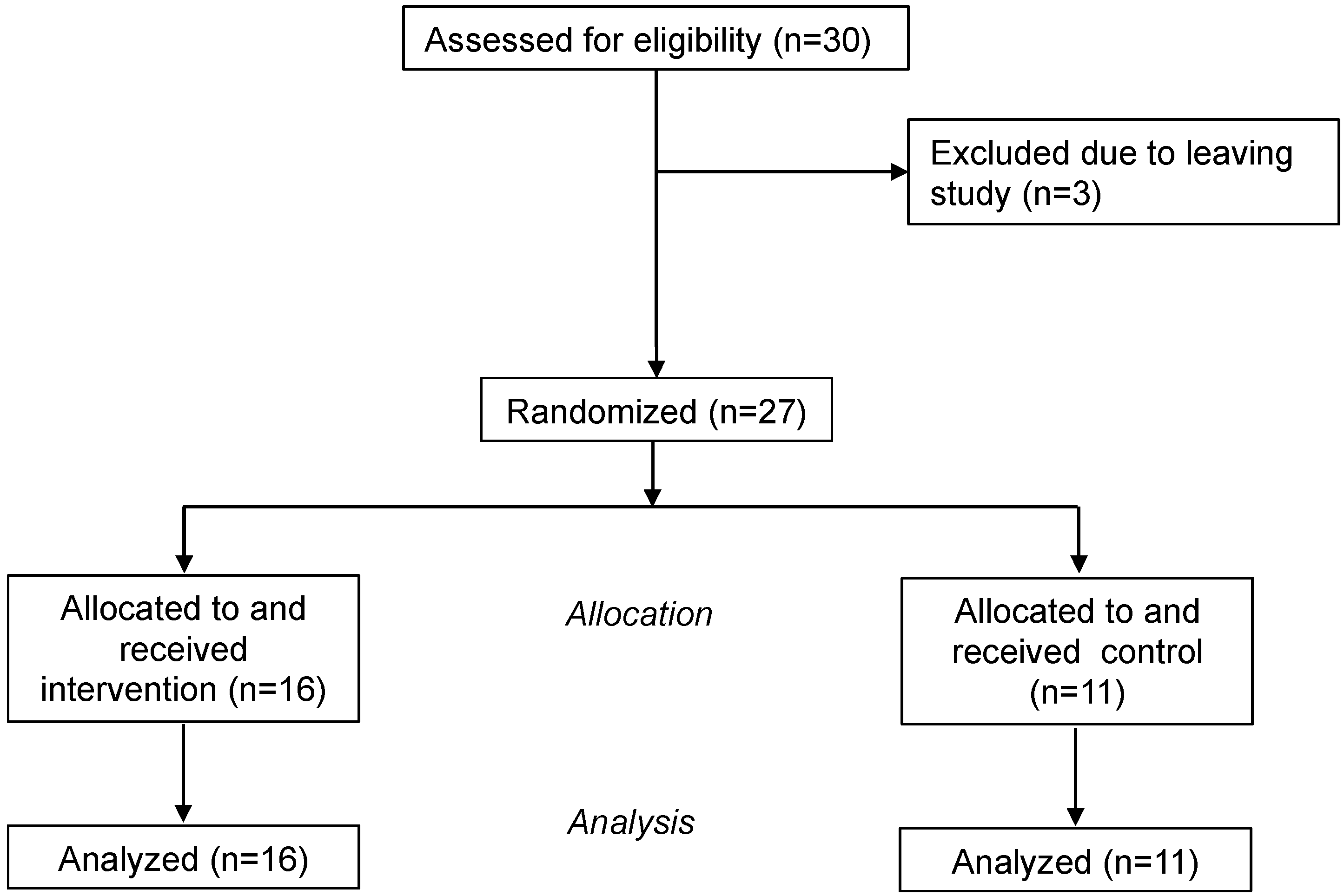
2.1. Participants
2.2. Training Protocol
2.2.1. NaviGAITor System (Used for Experimental (Intervention) Group)
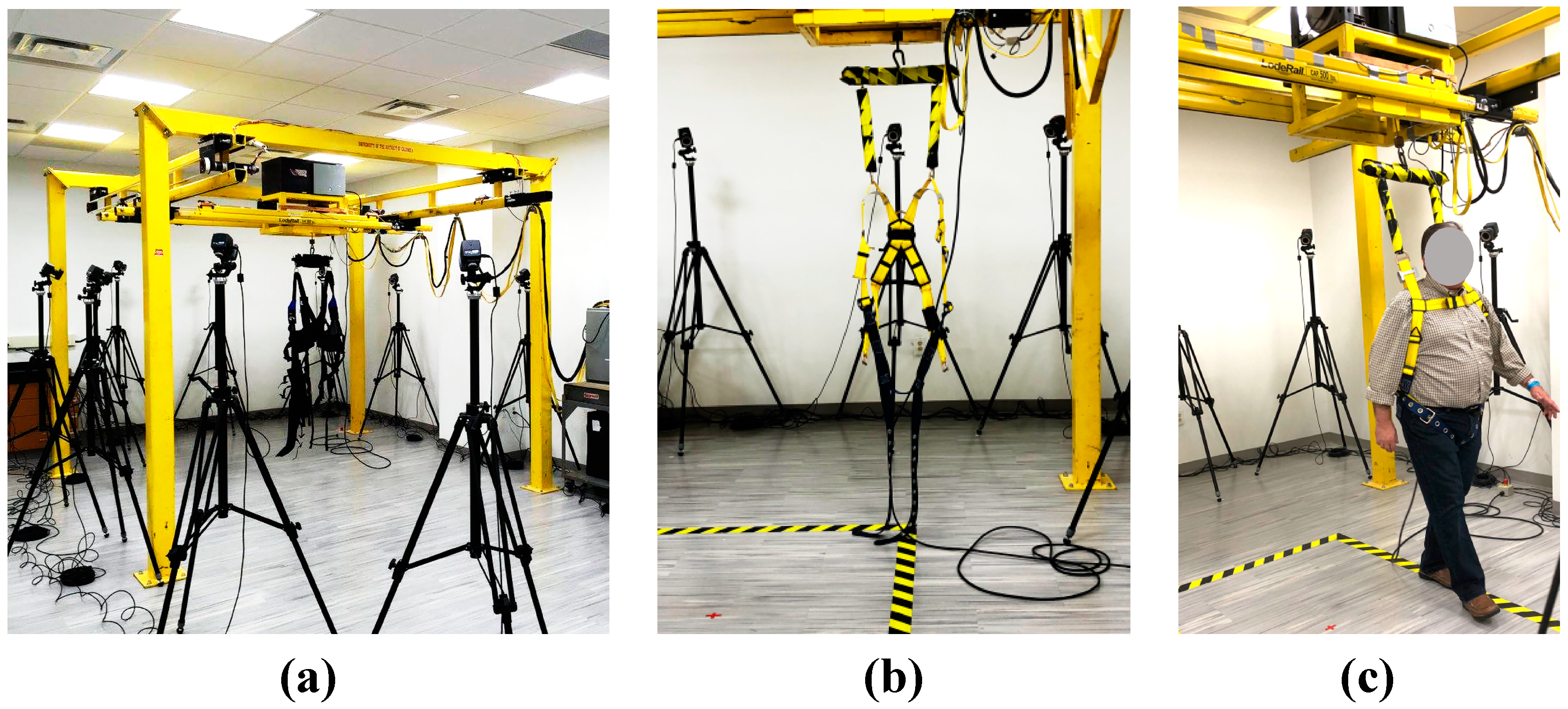
- Rather than straight path walking which is facilitated by other existing systems (e.g., ZeroG, Lokomat, and Biodex), the NaviGAITor helps the individual to perform overground movements and walking in the horizontal plane. Motorized XY motion is used so that the individual can start, walk, and stop with minimal effort and maximum safety. While the participant donned the NaviGAITor harness, the gantry system allowed them to move within the horizontal plane.
- Although it was not used in this study, the overhead harness had the capacity to provide unweighing via vertical support (BWS) of the participant while they did overground walking exercises and training. Participants in this study did not receive BWS but had experienced nBWS secure walking attributed to the robotic device.
- Although here we only utilized movements in the horizontal plane for training, the NaviGAITor has the capacity to enable movement training in along three axes of motion without risk of falls and injuries. The system provides the ability for an individual to, for example, go up and down stairs. Further, the motorized Z-axis motion with self-locking allows vertical displacement under constant or variable tension and will prevent a fall. Automation prevents falls and allows emergency stops.
- The lead-lag controller algorithm and leading offset algorithm helps the individual’s movement. The individual does not have to exert additional pressure on the cable as the control algorithm guarantees a smooth movement.
- The apparatus can be configured to accommodate different therapy facilities that may require adjustments in the mechanical and computer systems to maintain uniform and consistent operation.
2.2.2. Control Group
2.2.3. Training
2.3. Assessment Protocol
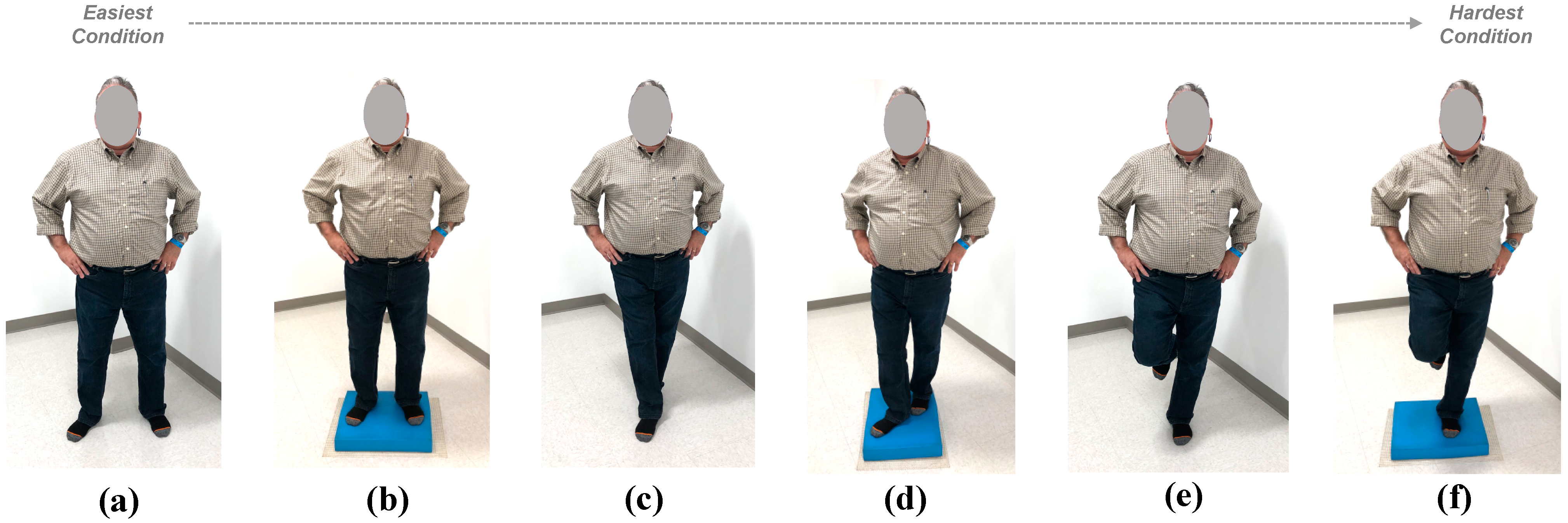
2.3.1. Measures of Balance Performance
2.3.2. Measures of Balance Confidence
2.4. Analysis
3. Results
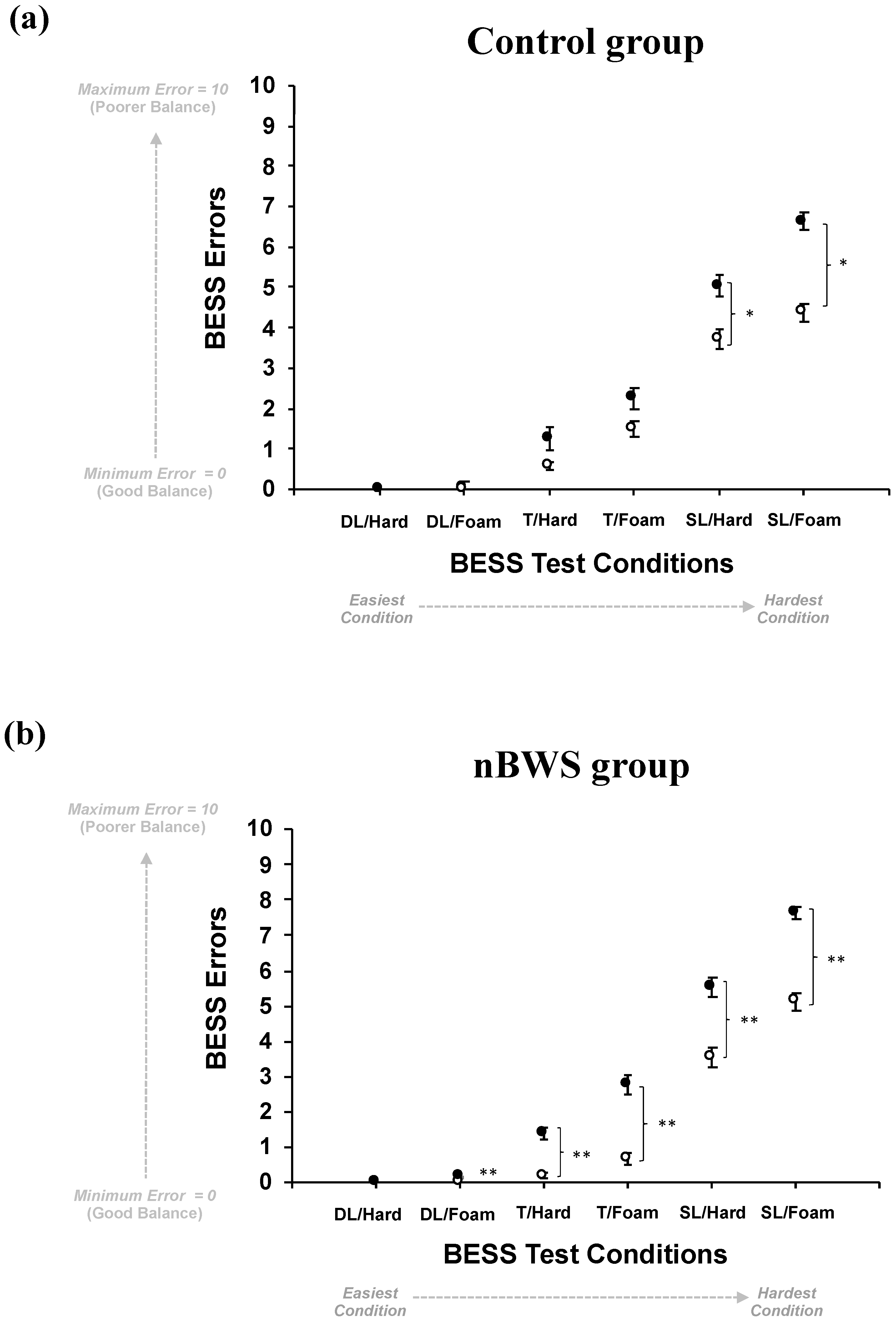
3.1. Measures of Balance Performance Results
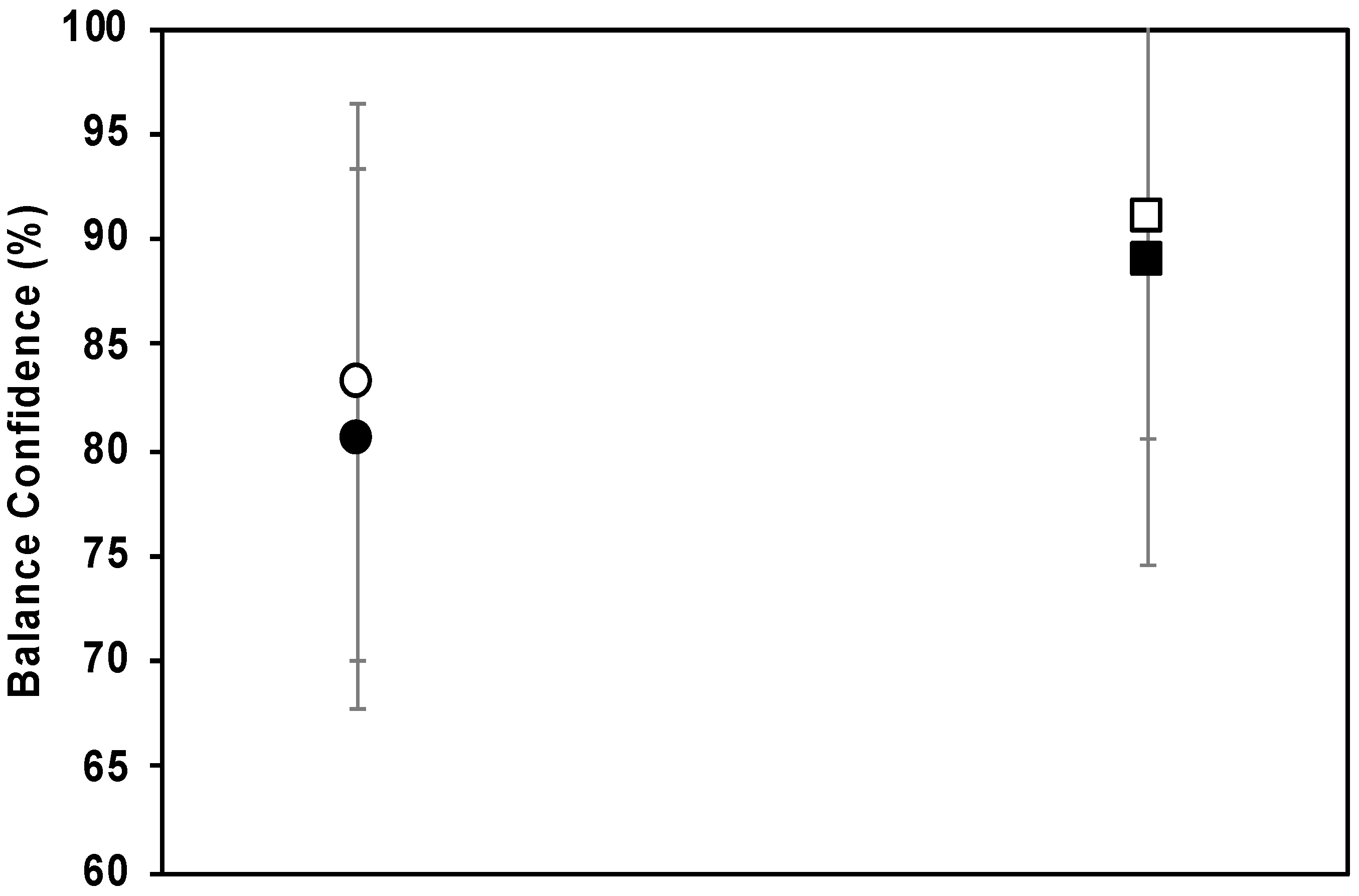
3.2. Measures of Balance Confidence—ABC Assessment Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- NIA Strategic Directions 2016. Aging Well in the 21st Century: Strategic Directions for Research on Aging. Available online: https://www.nia.nih.gov/about/aging-well-21st-century-strategic-directions-research-aging (accessed on 1 August 2020).
- Centers for Disease Control and Prevention (CDC) (Last Updated 24 March 2015). Stroke Frequently Asked Questions (FAQs). Available online: http://www.cdc.gov/stroke/faqs.htm (accessed on 1 August 2020).
- Jørgensen, L.; Engstad, T.; Jacobsen, B.K. Higher incidence of falls in long-term stroke survivors than in population controls depressive symptoms predict falls after stroke. Stroke 2002, 33, 542–547. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, Y. Fear of falling among stroke survivors after discharge from inpatient rehabilitation. Int. J. Rehabil. Res. 2005, 28, 149–152. [Google Scholar] [CrossRef] [PubMed]
- Legters, K. Fear of Falling. Phys. Ther. 2002, 82, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Vellas, B.J.; Wayne, S.J.; Romero, L.J.; Baumgartner, R.N.; Garry, P.J. Fear of falling and restriction of mobility in elderly fallers. Age Ageing 1997, 26, 189–193. [Google Scholar] [CrossRef]
- Kalron, A.; Fonkatz, I.; Frid, L.; Baransi, H.; Achiron, A. The effect of balance training on postural control in people with multiple sclerosis using the CAREN virtual reality system: A pilot randomized controlled trial. J. Neuroeng. Rehabil. 2016, 13, 13. [Google Scholar] [CrossRef] [PubMed]
- Sloot, L.H.; van den Noort, J.C.; van der Krogt, M.M.; Bruijn, S.M.; Harlaar, J. Can treadmill perturbations evoke stretch reflexes in the calf muscles? PLoS ONE 2015, 10, e0144815. [Google Scholar] [CrossRef] [PubMed]
- Vlutters, M.; Van Asseldonk, E.H.F.; Van der Kooij, H. Center of mass velocity-based predictions in balance recovery following pelvis perturbations during human walking. J. Exp. Biol. 2016, 219, 1514–1523. [Google Scholar] [CrossRef]
- Olenšek, A.; Zadrave, M.; Matjačićc, Z. A novel robot for imposing perturbations during overground walking: Mechanism, control and normative stepping responses. J. Neuroeng. Rehabil. 2016, 13, 55. [Google Scholar] [CrossRef]
- Frey, M.; Colombo, G.; Vaglio, M.; Bucher, R.; Jorg, M.; Riener, R. A novel mechatronic body weight support system. IEEE Trans. Neural Syst. Rehabil. Eng. 2006, 14, 311–321. [Google Scholar] [CrossRef]
- Wyss, D.; Bartenbach, V.; Pennycott, A.; Riener, R.; Vallery, H. A body weight support system extension to control lateral forces: Realization and validation. In IEEE International Conference on Robotics and Automation (ICRA), Proceedings of the 2014 IEEE International Conference on Robotics and Automation (ICRA), Hong Kong, China, 31 May–7 June 2014; IEEE: Piscataway, NJ, USA, 2014; pp. 328–332. [Google Scholar]
- Hidler, J.; Brennan, D.; Black, I.; Nichols, D.; Brady, K.; Nef, T. ZeroG: Overground gait and balance training system. J. Rehabil. Res. Dev. 2011, 48, 287–298. [Google Scholar] [CrossRef] [PubMed]
- Johnson Space Center Engineering. Active Response Gravity Offload System. 2013. Available online: https://www.nasa.gov/centers/johnson/engineering/integrated_environments/active_response_gravity/index.html (accessed on 1 August 2020).
- Vallery, H.; Lutz, P.; Von Zitzewitz, J.; Rauter, G.; Fritschi, M.; Everarts, C.; Ronsse, R.; Curt, A.; Bolliger, M. Multidirectional transparent support for overground gait training. In IEEE International Conference on Rehabilitation Robotics (ICORR), Proceedings of the 2013 IEEE 13th International Conference on Rehabilitation Robotics (ICORR), Seattle, WA, USA, 24–26 June 2013; IEEE: Piscataway, NJ, USA, 2013; pp. 1–7. [Google Scholar]
- Olenšek, A.; Oblak, J.; Cikajlo, I.; Novak, P.; Jere, K.; Matjačićc, Z. Adaptive dynamic balance training during overground walking with assistive device. In IEEE/RAS-EMBS International Conference on Biomedical Robotics and Biomechatronics (BioRob), Proceedings of the 2012 4th IEEE RAS & EMBS International Conference on Biomedical Robotics and Biomechatronics (BioRob), Rome, Italy, 24–27 June 2012; IEEE: Piscataway, NJ, USA, 2012; pp. 1066–1070. [Google Scholar]
- Patton, J.; Brown, D.A.; Peshkin, M.; Santos-Munné, J.J.; Makhlin, A.; Lewis, E.; Colgate, E.J.; Schwandt, D. KineAssist: Design and development of a robotic overground gait and balance therapy device. Top. Stroke Rehabil. 2008, 15, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Veneman, J.F.; Kruidhof, R.; Hekman, E.E.; Ekkelenkamp, R.; Van Asseldonk, E.H.; Van Der Kooij, H. Design and evaluation of the LOPES exoskeleton robot for interactive gait rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2007, 15, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Meuleman, J.; van Asseldonk, E.; van Oort, G.; Rietman, J.; van der Kooij, H. LOPES II—Design and evaluation of an admittance controlled gait training robot with shadow-leg approach. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 24, 352–363. [Google Scholar] [CrossRef] [PubMed]
- Young, A.J.; Ferris, D.P. State-of-the-art and future directions for robotic lower limb exoskeletons. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 25, 171–182. [Google Scholar] [CrossRef]
- Esquenazi, A.; Talaty, M.; Jayaraman, A. Powered exoskeletons for walking assistance in persons with central nervous system injuries: A narrative review. PM R 2017, 9, 46–62. [Google Scholar]
- Wang, S.; Wang, L.; Meijneke, C.; van Asseldonk, E.; Hoellinger, T.; Cheron, G.; Ivanenko, Y.; La Scaleia, V.; Sylos-Labini, F.; Molinari, M.; et al. Design and control of the MINDWALKER exoskeleton. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 23, 277–286. [Google Scholar] [CrossRef]
- Visintin, M.; Barbeau, H.; Korner-Bitensky, N.; Mayo, N.E. A New Approach to Retrain Gait in Stroke Patients Through Body Weight Support and Treadmill Stimulation. Stroke 1998, 29, 1122–1128. [Google Scholar] [CrossRef]
- Hesse, S.A.; Bertelt, C.; Jahnke, M.T.; Schaffrin, A.; Baake, P.; Malezic, M.; Mauritz, K.H. Treadmill training with partial body weight support compared with physiotherapy in nonambulatory hemiparetic patients. Stroke 1995, 26, 976–981. [Google Scholar] [CrossRef]
- Visintin, M.; Finch, L.; Barbeau, H. Progressive weight bearing and treadmill stimulation during gait retraining of hemiplegics: A case study. Phys. Ther. 1987, 68, 807. [Google Scholar]
- Hesse, S.A.; Bertlet, C.M.; Schaffrin, A.; Malezic, M.; Mauritz, K.H. Restoration of gait in nonambulatory hemiparetic patients by treadmill training with partial body weight support. Arch. Phys. Med. Rehabil. 1994, 75, 1087–1093. [Google Scholar] [CrossRef]
- Wernig, A.; Müller, S. Laufband locomotion with body weight support improved walking in persons with severe spinal cord injuries. Spinal Cord 1992, 30, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Wernig, A.; Müller, S.; Nanassy, A.; Cagol, E. Laufband therapy based on ‘rules of spinal locomotion’ is effective in spinal cord injured persons. Eur. J. Neurosci. 1995, 7, 823–829. [Google Scholar] [CrossRef]
- Labruyère, R.; van Hedel, H.J.A. Strength training versus robot-assisted gait training after incomplete spinal cord injury: A randomized pilot study in patients depending on walking assistance. J. Neuroeng. Rehabil. 2014, 11, 4. [Google Scholar] [CrossRef] [PubMed]
- Colombo, G.; Wirz, M.; Dietz, V. Driven gait orthosis for improvement of locomotor training in paraplegic patients. Spinal Cord 2001, 39, 252–255. [Google Scholar] [CrossRef] [PubMed]
- Riener, R.; Lünenburger, L.; Maier, I.C.; Colombo, G.; Dietz, V. Locomotor training in subjects with sensori-motor deficits: An overview of the robotic gait orthosis lokomat. J. Healthc. Eng. 2010, 1, 197–216. [Google Scholar] [CrossRef]
- Hesse, S.; Schmidt, H.; Werner, C.; Bardeleben, A. Upper and lower extremity robotic devices for rehabilitation and for studying motor control. Curr. Opin. Neurol. 2003, 16, 705–710. [Google Scholar] [CrossRef]
- Vallery, H.; Duschau-Wicke, A.; Riener, R. Generalized elasticities improve patient-cooperative control of rehabilitation robots. In IEEE International Conference on Rehabilitation Robotics (ICORR), Proceedings of the 2009 IEEE International Conference on Rehabilitation Robotics, Kyoto, Japan, 23–26 June 2009; IEEE: Piscataway, NJ, USA, 2009; pp. 535–541. [Google Scholar]
- Vallery, H.; Duschau-Wicke, A.; Riener, R. Optimized passive dynamics improve transparency of haptic devices. In IEEE International Conference on Robotics and Automation (ICRA), Proceedings of the 2009 IEEE International Conference on Robotics and Automation, Kobe, Japan, 12–17 May 2009; IEEE: Piscataway, NJ, USA, 2009; pp. 301–306. [Google Scholar]
- Harvey, L.; Wyndaele, J.J. Are we jumping too early with locomotor training programs? Spinal Cord 2011, 49, 947. [Google Scholar] [CrossRef]
- Sullivan, K.J.; Brown, D.A.; Klassen, T.; Mulroy, S.; Ge, T.; Azen, S.P.; Winstein, C.J. Effects of task-specific locomotor and strength training in adults who were ambulatory after stroke: Results of the STEPS randomized clinical trial. Phys. Ther. 2007, 87, 1580–1602. [Google Scholar] [CrossRef]
- Duncan, P.W.; Sullivan, K.J.; Behrman, A.L.; Azen, S.P.; Wu, S.S.; Nadeau, S.E.; Dobkin, B.H.; Rose, D.K.; Tilson, J.K.; Cen, S.; et al. Body-weight-supported treadmill rehabilitation after stroke. N. Engl. J. Med. 2011, 364, 2026–2036. [Google Scholar] [CrossRef]
- Graham, S.A.; Roth, E.J.; Brown, D.A. Walking and balance outcomes for stroke survivors: A randomized clinical trial comparing body-weight-supported treadmill training with versus without challenging mobility skills. J. Neuroeng. Rehabil. 2018, 15, 91. [Google Scholar] [CrossRef]
- Dobkin, B.H.; Duncan, P.W. Should body weight-supported treadmill training and robotic-assistive steppers for locomotor training trot back to the starting gate? Neurorehabilit. Neural Repair 2012, 26, 308–317. [Google Scholar] [CrossRef]
- Barbeau, H. Locomotor training in neurorehabilitation: Emerging rehabilitation concepts. Neurorehabilit. Neural Repair 2003, 17, 3–11. [Google Scholar] [CrossRef]
- Dobkin, B.H. An overview of treadmill locomotor training with partial body weight support: A neurophysiologically sound approach whose time has come for randomized clinical trials. Neurorehabilit. Neural Repair 1999, 13, 157–165. [Google Scholar] [CrossRef]
- Bouyer, L.J. Animal models for studying potential training strategies in persons with spinal cord injury. J. Neurol. Phys. Ther. 2005, 29, 117–125. [Google Scholar] [CrossRef]
- Richards, C.L.; Olney, S.J. Hemiparetic gait following stroke. Part II: Recovery and physical therapy. Gait Posture 1996, 4, 149–162. [Google Scholar] [CrossRef]
- Mehrholz, J.; Pohl, M.; Elsner, B. Treadmill training and body weight support for walking after stroke. Cochrane Database Syst. Rev. 2014, 2014, CD002840. [Google Scholar]
- Drużbicki, M.; Przysada, G.; Guzik, A.; Brzozowska-Magoń, A.; Kołodziej, K.; Wolan-Nieroda, A.; Majewska, J.; Kwolek, A. The Efficacy of Gait Training Using a Body Weight Support Treadmill and Visual Biofeedback in Patients with Subacute Stroke: A Randomized Controlled Trial. BioMed Res. Int. 2018, 2018, 3812602. [Google Scholar] [CrossRef]
- Gama, G.L.; Celestino, M.L.; Barela, J.A.; Forrester, L.; Whitall, J.; Barela, A.M. Effects of Gait Training With Body Weight Support on a Treadmill Versus Overground in Individuals With Stroke. Arch. Phys. Med. Rehabil. 2017, 98, 738–745. [Google Scholar] [CrossRef]
- Roerdink, M.; Lamoth, C.J.C.; Kwakkel, G.; Van Wieringen, P.C.W.; Beek, P.J. Gait coordination after stroke: Benefits of acoustically paced treadmill walking. Phys. Ther. Sport 2007, 87, 1009–1022. [Google Scholar] [CrossRef] [PubMed]
- Thompson, L.A. Moderate sensory balance training leads to improvements in elderly. Phys. Ther. Rehabil. 2019, 6, 12. [Google Scholar] [CrossRef][Green Version]
- Kim, H.J.; Kwon, B.S.; Park, J.; Lee, H.J.; Yoo, A. Robot-assisted gait training (Lokomat) improves walking function and activity in people with spinal cord injury: A systematic review. J. Neuroeng. Rehabil. 2017, 14, 24. [Google Scholar]
| Robotic Device | Image | Description |
|---|---|---|
| Biodex Unweighing System 1 |  | The Biodex Unweighing system allows for partial bodyweight support (BWS) of the patient. Additionally, overground walking and movements which replicate natural ambulation are possible while using this device. This device does not allow for vertical movements. |
| Lokomat System 2 |  | The Lokomat is a robotic treadmill training device that allows for partial BWS of the patient. There is a harness and robotic (automated gait orthosis device) that attaches to the person while they walk on a treadmill. The concept behind use of this device is that, by continuous repetition of movements, it can train patients to re-learn normal walking. |
| ZeroG System 3 |  | The ZeroG is a partial BWS system that moves along a driven trolley attached to an overhead rail system. The system allows the patient to do overground walking and vertical movements. The rail system is typically attached to ceilings over 9 feet high but can be designed without ceiling integration. |
| KineAssist Walking and balance system 4 |  | This KineAssist robotic device consists of a hip brace and harness that connects to an actuation system. It provides partial BWS and postural torques on the torso while following patient’s walking motions overground in forward, rotation and sidestepping directions. |
| Autoambulator 5 |  | The Autoamblator system incorporates robotic assistance, with connectors at the lower limbs, to simulate normal walking motion. A harness provides partial BWS to the patient while they walk over a treadmill. This device does not allow for vertical movements. |
| NaviGAITor | (See Figure 2) | The NaviGAITor is an ambulatory suspension and rehabilitation apparatus system designed by D. Shetty and experimented by the authors. It is a newer device for research and clinical applications. It enables exercise and movement training in all three planes of motion. These features are made possible because of mechatronic design methodology. |
| Group | DL/Hard | DL/Foam | T/Hard | T/Foam | SL/Hard | SL/Foam |
|---|---|---|---|---|---|---|
| Control | df = 16, t = −2.46, p = 0.026 | df = 12, t = −2.72, p = 0.019 | ||||
| nBWS | df = 15, t = −11.54, p < 0.00001 | df = 29, t = −7.32, p < 0.00001 | df = 29, t = −7.32, p < 0.00001 | df = 16, t = −2.46, p < 0.00001 | df = 27, t = −8.23, p < 0.00001 |
| BESS Condition | Control | nBWS |
|---|---|---|
| DL/H | Undefined | undefined |
| DL/F | 200% | −200% |
| T/H | −69.1% | −153.8% |
| T/F | −41.1% | −122.9% |
| SL/H | −30.1% | −43.7% |
| SL/F | −40.8% | −39.2% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thompson, L.A.; Badache, M.; Brusamolin, J.A.R.; Savadkoohi, M.; Guise, J.; Paiva, G.V.d.; Suh, P.; Sanchez Guerrero, P.; Shetty, D. Multidirectional Overground Robotic Training Leads to Improvements in Balance in Older Adults. Robotics 2021, 10, 101. https://doi.org/10.3390/robotics10030101
Thompson LA, Badache M, Brusamolin JAR, Savadkoohi M, Guise J, Paiva GVd, Suh P, Sanchez Guerrero P, Shetty D. Multidirectional Overground Robotic Training Leads to Improvements in Balance in Older Adults. Robotics. 2021; 10(3):101. https://doi.org/10.3390/robotics10030101
Chicago/Turabian StyleThompson, Lara A., Mehdi Badache, Joao Augusto Renno Brusamolin, Marzieh Savadkoohi, Jelani Guise, Gabriel Velluto de Paiva, Pius Suh, Pablo Sanchez Guerrero, and Devdas Shetty. 2021. "Multidirectional Overground Robotic Training Leads to Improvements in Balance in Older Adults" Robotics 10, no. 3: 101. https://doi.org/10.3390/robotics10030101
APA StyleThompson, L. A., Badache, M., Brusamolin, J. A. R., Savadkoohi, M., Guise, J., Paiva, G. V. d., Suh, P., Sanchez Guerrero, P., & Shetty, D. (2021). Multidirectional Overground Robotic Training Leads to Improvements in Balance in Older Adults. Robotics, 10(3), 101. https://doi.org/10.3390/robotics10030101





