Unveiling the Hidden Burden: A Systematic Review on the Prevalence and Clinical Implications of Calcified Brain Metastases
Abstract
1. Introduction
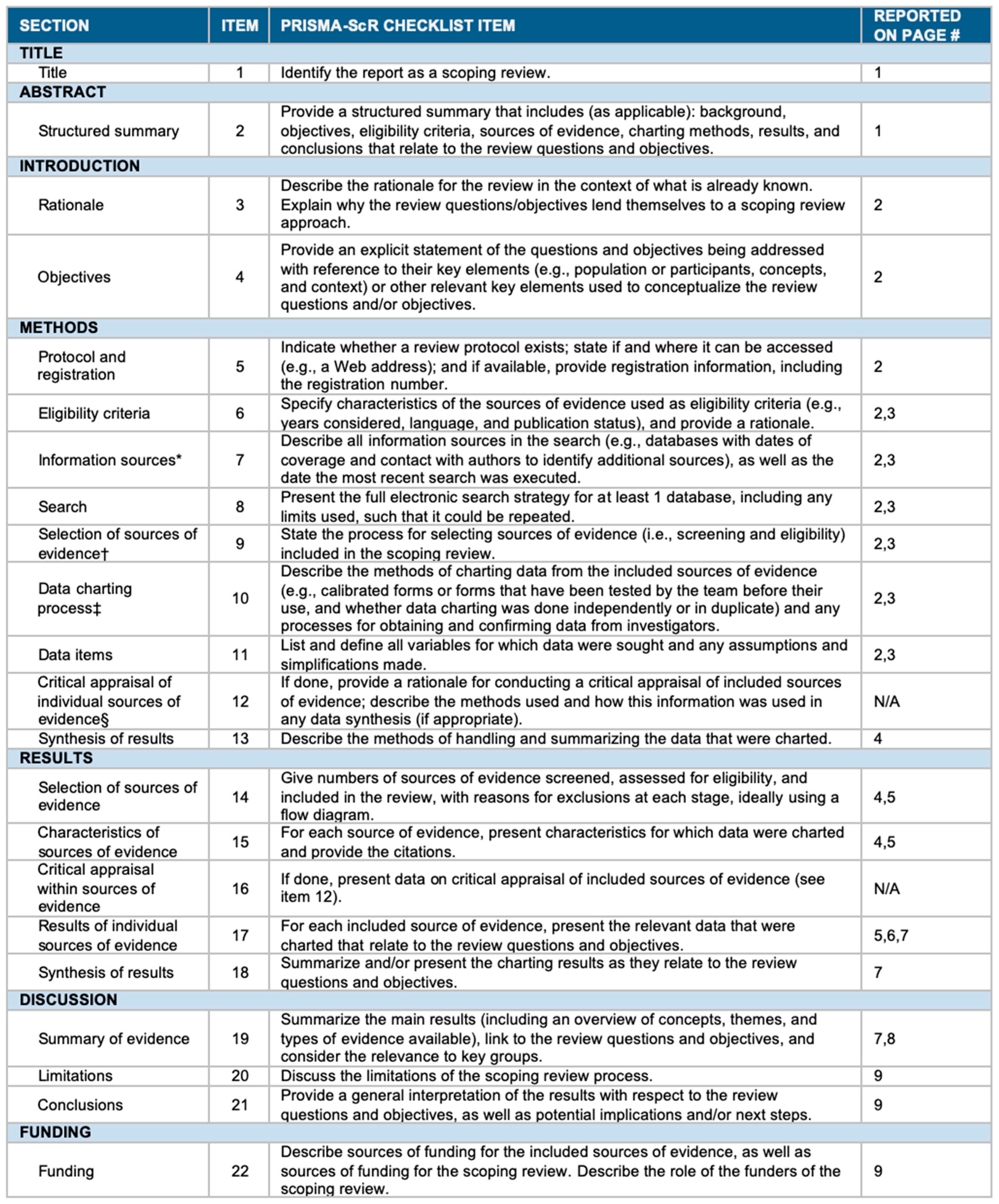
2. Materials and Methods
2.1. Literature Review
2.2. Data Extraction
2.3. Outcomes
2.4. Risk of Bias Assessment
2.5. Statistical Analysis
3. Results
3.1. Literature Review Results
3.2. Data Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
Appendix A

Appendix B
References
- Grech, R.; Grech, S.; Mizzi, A. Intracranial calcifications. A pictorial review. Neuroradiol. J. 2012, 25, 427–451. [Google Scholar] [CrossRef]
- Bertolini, F.; Spallanzani, A.; Fontana, A.; Depenni, R.; Luppi, G. Brain metastases: An overview. CNS Oncol. 2015, 4, 37–46. [Google Scholar] [CrossRef]
- Tashiro, Y.; Kondo, A.; Aoyama, I.; Nin, K.; Shimotake, K.; Tashiro, H.; Nishioka, T. Calcified metastatic brain tumor. Neurosurgery 1990, 26, 1065–1070. [Google Scholar] [CrossRef]
- Lee, K.F.; Suh, J.H. CT evidence of grey matter calcification secondary to radiation therapy. Comput. Tomogr. 1977, 1, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Inomata, M.; Hayashi, R.; Kambara, K.; Okazawa, S.; Imanishi, S.; Ichikawa, T.; Suzuki, K.; Yamada, T.; Miwa, T.; Kashii, T.; et al. Miliary brain metastasis presenting with calcification in a patient with lung cancer: A case report. J. Med. Case Rep. 2012, 6, 279. [Google Scholar] [CrossRef] [PubMed]
- Fatehi, F.; Basiri, K.; Mehr, G.K. Calcified brain metastasis of breast cancer. Acta Neurol. Belg. 2010, 110, 124–125. [Google Scholar] [PubMed]
- Kokkali, S.; Andriotis, E.; Katsarou, E.; Theocharis, A.; Drizou, M.; Magou, E.; Tzovaras, A.; Ardavanis, A. Cerebral metastasis from osteosarcoma: “Bone” in the brain. Radiol. Case Rep. 2020, 15, 780–783. [Google Scholar] [CrossRef] [PubMed]
- Bhatoe, H.S.; Gill, H.S. Calcified brain metastasis in non-Hodgkin’s lymphoma. Postgrad. Med. J. 1994, 70, 384–385. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Michail, P.; Amith, I.; George, S.; George, M.K. A case of calcified metastatic colorectal adenocarcinoma mimicking a benign lesion: Pitfalls in diagnosis. Case Rep. Oncol. Med. 2015, 2015, 936260. [Google Scholar] [CrossRef] [PubMed]
- Callizo, J.A.; Gimenez-Mas, J.A.; Martin, J.; Lacasa, J. Calcified brain metastases from acinar-cell carcinoma of pancreas. Neuroradiology 1989, 31, 200. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef]
- Tomita, T.; Larsen, M.B. Calcified metastases to the brain in a child: Case report. Neurosurgery 1983, 13, 435–437. [Google Scholar] [CrossRef]
- Kelly, R.B.; Mahoney, P.D.; Johnson, J.F. A calcified carcinoma of the lung and intracerebral metastasis. J. Comput. Tomogr. 1987, 11, 389–391. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, Y.; Homma, T.; Kohga, H.; Uki, J.; Shisa, H. A lung cancer case with numerous calcified metastatic nodules of the brain. Neuroradiology 1988, 30, 265–268. [Google Scholar] [CrossRef] [PubMed]
- Gaze, M.N.; Gregor, A.; Whittle, I.R.; Sellar, R.J. Calcified cerebral metastasis from cervical carcinoma. Neuroradiology 1989, 31, 291. [Google Scholar] [CrossRef] [PubMed]
- Yamada, I.; Suzuki, S. Calcification in cerebral non-Hodgkin’s lymphoma: CT demonstration. Neuroradiology 1989, 31, 372. [Google Scholar] [CrossRef]
- Nakase, H.; Sakaki, T.; Fujita, T.; Tsunoda, S.; Nakamura, M.; Imai, T.; Hiasa, Y. Multiple calcified metastatic brain tumor--case report. Neurol. Med. Chir. 1991, 31, 787–791. [Google Scholar] [CrossRef] [PubMed]
- Kincaid, W. Case report: Calcified brain metastases from an osteogenic sarcoma. Clin. Radiol. 1992, 45, 139–140. [Google Scholar] [CrossRef]
- Yamazaki, T.; Harigaya, Y.; Noguchi, O.; Okamoto, K.; Hirai, S. Calcified miliary brain metastases with mitochondrial inclusion bodies. J. Neurol. Neurosurg. Psychiatry 1993, 56, 110–111. [Google Scholar] [CrossRef] [PubMed]
- Ricke, J.; Baum, K.; Hosten, N. Calcified brain metastases from ovarian carcinoma. Neuroradiology 1996, 38, 460–461. [Google Scholar] [CrossRef] [PubMed]
- Cacho, J.; Guerrero, A.L.; Arcaya, J.; Gomez, J.C.; Marcos, M.M.; Adeva, T. Calcified brain metastases from lung carcinoma. J. Neurol. 1996, 243, 487–488. [Google Scholar] [CrossRef] [PubMed]
- Duval, L.; Defebvre, L.; Durieu, J.; Destee, A. Multiple calcified brain metastases revealing a lung carcinoma. Acta Neurol. Belg. 1996, 96, 312–315. [Google Scholar]
- Stadnik, T.; Deroover, J.; Gosens, A.; Michotte, A.; Freson, M.; Osteaux, M. Calcified, cystic brain metastases. Eur. J. Radiol. 1997, 25, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Dibiane, A.; Amrar, F.; Abdelmoumni, A.; Jourdain, C.; Poquet, E.; Serre, I.; Escure, M.N. Multiple calcified cerebral metastases revealing bronchial adenocarcinoma. Apropos of a case. J Radiol. 1998, 79, 563–565. [Google Scholar] [PubMed]
- Henríquez, I.; Castro, C.; Berenguer, J.; Biete, A. Calcification of presumed ovarian carcinoma brain metastases following radiotherapy. Br. J. Radiol. 1999, 72, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Teksam, M.; Cevik, B.; Coskun, M. Calcified brain metastasis of osteosarcoma: CT findings. Eur. J. Radiol. Extra 2004, 52, 47–49. [Google Scholar] [CrossRef]
- Graña, L.; Santamaría, N.; Yus, M.; Méndez, R. Metástasis cerebral calcificada. Radiología 2007, 49, 335–337. [Google Scholar] [CrossRef] [PubMed]
- Pugnet, G.; Arista, S.; Martin-Blondel, G.; Roche, H.; Arlet-Suau, E.; Astudillo, L. Métastase choroïdienne révélant un cancer du sein. Rev. Médecine Interne 2007, 28, 790–792. [Google Scholar] [CrossRef]
- Eom, K.S.; Kim, T.Y. Cystic and Calcified Brain Tumor Metastasized From Non-Small Cell Carcinoma: A Case Report. J. Neurol. Sci. 2012, 29, 611. Available online: https://openurl.ebsco.com/contentitem/gcd:82481237?sid=ebsco:plink:crawler&id=ebsco:gcd:82481237 (accessed on 12 September 2024).
- Kawamura, D.; Tanaka, T.; Fuga, M.; Yanagisawa, T.; Tochigi, S.; Irie, K.; Hasegawa, Y.; Abe, T. Slow progression of calcified cerebellar metastasis from ovarian cancer: A case report and review of the literature. Neurol. Med. Chir. 2013, 53, 722–726. [Google Scholar] [CrossRef] [PubMed]
- De Pablo-Fernández, E.; Gómez-Herrera, J.J.; Sierra-Hidalgo, F.; Sanchez-Ferro, A. Calcified brain metastases from osteosarcoma. Can. J. Neurol. Sci. J. Can. Sci. Neurol. 2013, 40, 247–248. [Google Scholar] [CrossRef] [PubMed]
- Ressl, N.; Oberndorfer, S. Multiple calcified brain metastases in a man with invasive ductal breast cancer. Case Rep. 2015, 2015, bcr2015211777. [Google Scholar] [CrossRef] [PubMed]
- Bahrami, E.; Taheri, M.; Benam, M. Calcified brain metastatic adenocarcinoma: A case report and review of the literature. Neuroradiol. J. 2019, 32, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Santos Vázquez, G.; Garcia Cázarez, R.; Moreno Pizarro, E.; Serrano Padilla, A.E.; Plascencia Salcedo, J.C. Central Nervous System Miliary Brain Metastasis Secondary to Breast Cancer. Cureus 2020, 12, e9649. [Google Scholar] [CrossRef]
- Ananthashayana, V.H.; Jana, M.; Malapure, S.S.; Gupta, A.K. Unusual cause of seizure in a child: Intracranial calcified metastasis of osteosarcoma. Indian J. Cancer 2020, 57, 209. [Google Scholar] [CrossRef]
- Divya, K.P.; Cherian, A.; Prabhakaran, P.K.; Thomas, B.; Shetty, K. Calcific Miliary Brain Metastasis in Adenocarcinoma Lung Treated with Gefitinib. Neurol. India 2022, 70, 1197. [Google Scholar] [CrossRef]
- Mo, Y.; Zhang, Y.; Zhuang, L.; Wang, J.; Yan, S.; Li, Y.; Qiao, S.; Lai, Q. Stroke-like onset of calcified brain metastases with Wallerian degeneration: A case report and review of the literature. Int. J. Neurosci. 2023, 134, 1288–1292. [Google Scholar] [CrossRef] [PubMed]
- Anand, A.K.; Potts, D.G. Calcified brain metastases: Demonstration by computed tomography. AJNR Am. J. Neuroradiol. 1982, 3, 527–529. [Google Scholar]
- Hwang, T.L.; Valdivieso, J.G.; Yang, C.H.; Wolin, M.J. Calcified brain metastasis. Neurosurgery 1993, 32, 451–454. [Google Scholar] [CrossRef] [PubMed]
- Ohmoto, Y.; Nishizaki, T.; Kajiwara, K.; Nomura, S.; Kameda, H.; Suzuki, M. Calcified metastatic brain tumor--two case reports. Neurol. Med. Chir. 2002, 42, 264–267. [Google Scholar] [CrossRef] [PubMed]
- Hwang, K.-E.; Oh, S.-J.; Park, C.; Jeon, S.-J.; Lee, J.-M.; Cha, B.-K.; Yoon, K.-H.; Jeong, E.-T.; Kim, H.-R. Computed tomography morphologic features of pulmonary adenocarcinoma with brain/bone metastasis. Korean J. Intern. Med. 2016, 33, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Kuo, Y.-H.; Chang, Y.-C.; Hu, F.-C.; Lin, Z.-Z.; Yang, J.C.-H. Calcified brain metastasis after systemic treatment predict long survival in advanced non-small cell lung cancer patients. Ann. Oncol. 2017, 28, x139. [Google Scholar] [CrossRef]
- Rebella, G.; Romano, N.; Silvestri, G.; Ravetti, J.L.; Gaggero, G.; Belgioia, L.; Lupidi, F.; Signori, A.; Roccatagliata, L.; Saitta, L.; et al. Calcified brain metastases may be more frequent than normally considered. Eur. Radiol. 2021, 31, 650–657. [Google Scholar] [CrossRef]
- Saha, A.; Ghosh, S.K.; Roy, C.; Choudhury, K.B.; Chakrabarty, B.; Sarkar, R. Demographic and clinical profile of patients with brain metastases: A retrospective study. Asian J. Neurosurg. 2013, 8, 157–161. [Google Scholar] [CrossRef]
- Chiesa, A.M.; Spinnato, P.; Miceli, M.; Facchini, G. Radiologic Assessment of Osteosarcoma Lung Metastases: State of the Art and Recent Advances. Cells 2021, 10, 553. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMAScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]

| Author | Year | Primary Tumor Type | Location of CBM | Type of CBM | Radiotherapy | Overall Survival (OS) |
|---|---|---|---|---|---|---|
| Tomita and Larsen [13] | 1983 | Metastatic undifferentiated sarcoma | Parietal/cerebellum | - | Yes | 3 mo |
| Kelly et al. [14] | 1987 | Lung large cell undifferentiated carcinoma | Left cerebral hemisphere | - | No | 9 mo |
| Fukuda et al. [15] | 1988 | Lung papillary adenocarcinoma | Disseminate | Nodular | No | - |
| Callizo et al. [10] | 1989 | Acinar cell carcinoma of the pancreas | Disseminate | Punctate/curvilinear comma-like scattered | Yes | - |
| Gaze et al. [16] | 1989 | Squamous carcinoma of cervix | Temporoparietal | Punctate | Yes | 10 mo |
| Yamada and Suzuki [17] | 1989 | Diffuse, large cell non-Hodgkin’s lymphoma | Thalamic region | Nodular | No | 12 mo |
| Tashiro et al. [3] | 1990 | Metastatic squamous cell carcinoma/unknown origin | Corpus callosum | Conglomerate | No | 12 mo |
| Nakase et al. [18] | 1991 | Small cell carcinoma of lung | Disseminate | - | - | - |
| Kincaid [19] | 1992 | Osteosarcoma | Occipital lobe | - | No | 8 mo |
| Yamazaki et al. [20] | 1993 | Metastatic adenocarcinoma of the lung | Disseminate | Scattered punctate | No | 12 d |
| Bhatoe and Gill [8] | 1994 | Non-Hodgkin’s lymphoma | Frontal lobe | - | No | - |
| Ricke et al. [21] | 1996 | Papillary carcinoma of the ovaries | Disseminate | Circular/irregular | - | 1 mo |
| Cacho et al. [22] | 1996 | Lung carcinoma | Right lateral ventricle, right paramedian region, left frontoparietal cortical region | - | - | 12 mo |
| Duval et al. [23] | 1996 | Lung carcinoma | - | - | No | - |
| Stadnik et al. [24] | 1997 | Papillary cystadenocarcinoma | Posterior fossa | Peripheral calcification | - | - |
| Dibiane et al. [25] | 1998 | Bronchial adenocarcinoma | - | - | Yes | - |
| Henriquez et al. [26] | 1999 | Ovarian carcinoma | - | - | No | 20 d |
| Teksam et al. [27] | 2004 | Osteosarcoma | Temporoparieto-occipital | - | - | 2 mo |
| Graña et al. [28] | 2007 | Adenocarcinoma of colorectal | Frontal lobe | - | - | 24 mo |
| Pugnet et al. [29] | 2007 | Breast carcinoma | Supra/infratentorial | - | No | - |
| Fatehi et al. [6] | 2010 | Breast cancer | Disseminate | - | No | 12 mo |
| Inomata et al. [5] | 2012 | Lung adenocarcinoma/leptomeningeal adenocarcinoma | Disseminate | Scattered | - | - |
| Eom and Kim [30] | 2012 | Non-small cell carcinoma of lung | Frontal lobe | - | No | - |
| Kawamura et al. [31] | 2013 | Serous mucinous adenocarcinoma | Cerebellar hemisphere | - | No | Few d |
| Fernandez et al. [32] | 2013 | Osteosarcoma of the mandible | Centrum semiovale | Round | No | - |
| Michail et al. [9] | 2015 | Adenocarcinoma of colorectal | Frontoparietal | - | Yes | - |
| Ressl and Oberdornfer [33] | 2015 | Breast invasive ductal carcinoma | - | - | No | - |
| Bahrami et al. [34] | 2018 | Adenocarcinoma, probably from colon origin | Parietal lobe | Amorphous | - | - |
| Vazquez et al. [35] | 2020 | Breast cancer | Disseminate | - | No | 2 mo |
| Kokkali et al. [7] | 2020 | Osteosarcoma | Cerebellum | - | - | - |
| Ananthashayana et al. [36] | 2020 | Osteosarcoma | Left frontal lobe | - | - | 3 mo |
| Divya et al. [37] | 2022 | Adenocarcinoma of lung | Parieto-occipital region | - | - | - |
| Mo et al. [38] | 2023 | Pulmonary adenocarcinoma | Left periventricular white matter, basal ganglia | - | - | - |
| Author | Year | Primary Tumor Type | Location of CBM | Type of CBM | Radiotherapy | Overall Survival (OS) |
|---|---|---|---|---|---|---|
| Anand and Potts [39] | 1982 | Lung, breast | Temporal lobe | Punctate | No | - |
| Lung | Supra/infratentorial | Punctate | No | - | ||
| Esophagus | Cerebellum | Curvilinear | No | - | ||
| Lung | Cerebellum | Curvilinear | No | - | ||
| Colon | Frontal lobe | Amorphous | No | - | ||
| Breast | Supratentorial | Punctate | No | - | ||
| Colon | Frontoparietal | Amorphous | No | - | ||
| Hwang et al. [40] | 1993 | Metastatic adenocarcinoma | Parietal/temporal lobe, corpus callosum | - | No | 27 mo |
| Lung squamous cell carcinoma | Temporal lobe | - | No | 45 mo | ||
| Ohmoto et al. [41] | 2002 | Lung adenocarcinoma | Frontal lobe | - | No | 33 mo |
| Adenocarcinoma | Frontal lobe | Linear | No | 12 mo |
| Author | Year | Primary Tumor Type | Sample Size | Patients with CBM | Incidence of CBM (%) | Radiotherapy | Overall Survival (OS) |
|---|---|---|---|---|---|---|---|
| Hwang et al. [42] | 2016 | Lung adenocarcinoma | 19 | 5 | 26.3 | No | - |
| Kuo et al. [43] | 2017 | NSCLC | 943 | 49 | 5.2 | No | 462 d |
| Rebella et al. [44] | 2020 | Lung, breast, ovaries | 153 | 34 | 22.2 | 16 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garaba, A.; Panciani, P.P.; Da’ana, A.; Ius, T.; Tel, A.; Fontanella, M.M.; Zeppieri, M.; Ortolani, F.; Agosti, E. Unveiling the Hidden Burden: A Systematic Review on the Prevalence and Clinical Implications of Calcified Brain Metastases. Biomolecules 2024, 14, 1585. https://doi.org/10.3390/biom14121585
Garaba A, Panciani PP, Da’ana A, Ius T, Tel A, Fontanella MM, Zeppieri M, Ortolani F, Agosti E. Unveiling the Hidden Burden: A Systematic Review on the Prevalence and Clinical Implications of Calcified Brain Metastases. Biomolecules. 2024; 14(12):1585. https://doi.org/10.3390/biom14121585
Chicago/Turabian StyleGaraba, Alexandru, Pier Paolo Panciani, Aida Da’ana, Tamara Ius, Alessandro Tel, Marco Maria Fontanella, Marco Zeppieri, Fulvia Ortolani, and Edoardo Agosti. 2024. "Unveiling the Hidden Burden: A Systematic Review on the Prevalence and Clinical Implications of Calcified Brain Metastases" Biomolecules 14, no. 12: 1585. https://doi.org/10.3390/biom14121585
APA StyleGaraba, A., Panciani, P. P., Da’ana, A., Ius, T., Tel, A., Fontanella, M. M., Zeppieri, M., Ortolani, F., & Agosti, E. (2024). Unveiling the Hidden Burden: A Systematic Review on the Prevalence and Clinical Implications of Calcified Brain Metastases. Biomolecules, 14(12), 1585. https://doi.org/10.3390/biom14121585











