Mutated TP53 in Circulating Tumor DNA as a Risk Level Biomarker in Head and Neck Squamous Cell Carcinoma Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Clinical and Histopathological Data and Outcome Measures
2.3. Tumor DNA Extraction
2.4. TP53 Library Generation and Determining the Fraction of Mutated Copies
2.5. Plasma Sample Collection and ctDNA Detection
2.6. Statistical Analysis
3. Results
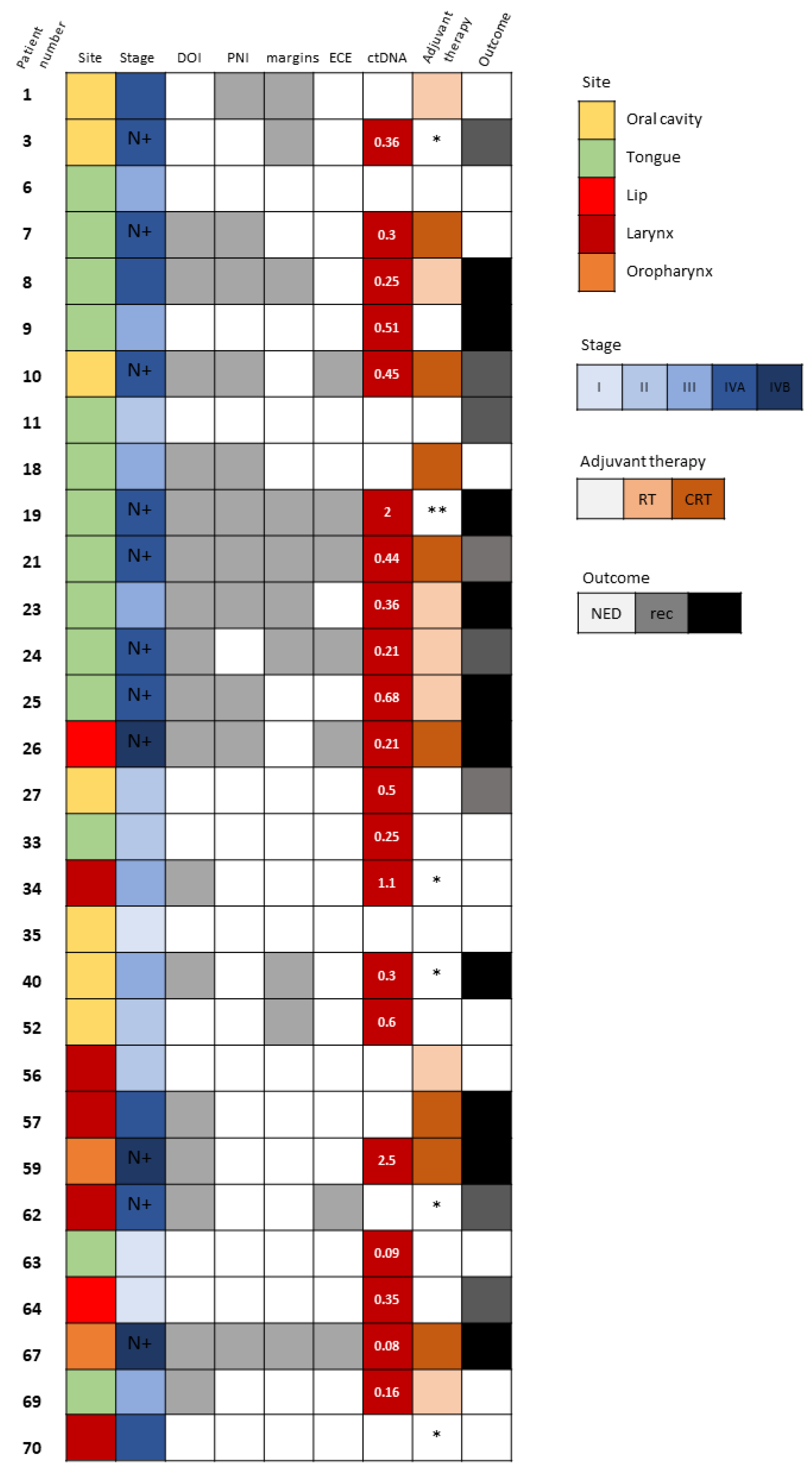
3.1. Patient Characteristics
3.2. TP53 Genetic Alterations in Tumor Specimens
3.3. Tumor-Specific TP53 Mutations Detected in Circulating Cell-Free DNA
3.4. The Prognostic Value of Detectable ctDNA
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siegel, R.; Miller, K.D.; Ahmedin, J. Cáncer Statistics. CA Cáncer J. 2017, 67, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.; Xia, P.; Fischbein, N.J.; Akazawa, P.; Akazawa, C.; Quivey, J.M. Intensity-modulated radiation therapy for head-and-neck cancer: The UCSF experience focusing on target volume delineation. Int. J. Radiat. Oncol. Biol. Phys. 2003, 57, 49–60. [Google Scholar] [CrossRef] [PubMed]
- Gatta, G.; Botta, L.; Sánchez, M.J.; Anderson, L.A.; Pierannunzio, D.; Licitra, L. Prognoses and improvement for head and neck cancers diagnosed in Europe in early 2000s: The EUROCARE-5 population-based study. Eur. J. Cancer 2015, 51, 2130–2143. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.M.; Khuri, F.R. Advances in the management of recurrent or metastatic squamous cell carcinoma of the head and neck. Head Neck 2013, 35, 443–453. [Google Scholar] [CrossRef]
- Haddad, R.; O’Neill, A.; Rabinowits, G.; Tishler, R.; Khuri, F.; Adkins, D.; Clark, J.; Sarlis, N.; Lorch, J.; Beitler, J.J.; et al. Induction chemotherapy followed by concurrent chemoradiotherapy (sequential chemoradiotherapy) versus concurrent chemoradiotherapy alone in locally advanced head and neck cancer (PARADIGM): A randomised phase 3 trial. Lancet Oncol. 2013, 14, 257–264. [Google Scholar] [CrossRef]
- Diaz, L.A.; Bardelli, A. Liquid biopsies: Genotyping circulating tumor DNA. J. Clin. Oncol. 2014, 32, 579–586. [Google Scholar] [CrossRef]
- Volik, S.; Alcaide, M.; Morin, R.D.; Collins, C. Cell-free DNA (cfDNA): Clinical Significance and Utility in Cancer Shaped By Emerging Technologies. Mol. Cancer Res. 2016, 14, 898–908. [Google Scholar] [CrossRef]
- Diehl, F.; Schmidt, K.; Choti, M.A.; Romans, K.; Goodman, S.; Li, M.; Agrawal, N.; Sokoll, L.; Szabo, S.A.; Kinzler, K.W.; et al. Circulating mutant DNA to assess tumor dynamics. Nat. Med. 2008, 14, 985–990. [Google Scholar] [CrossRef]
- Thierry, A.R.; El Messaoudi, S.; Gahan, P.B.; Anker, P.; Stroun, M. Origins, structures, and functions of circulating DNA in oncology. Cancer Metastasis Rev. 2016, 35, 347–376. [Google Scholar] [CrossRef]
- Wood, L.D.; Parsons, D.W.; Jones, S.; Lin, J.; Sjöblom, T.; Leary, R.J.; Shen, D.; Boca, S.M.; Barber, T.; Ptak, J.; et al. The genomic landscapes of human breast and colorectal cancers. Science 2007, 318, 1108–1113. [Google Scholar] [CrossRef]
- Diehl, F.; Li, M.; Dressman, D.; He, Y.; Shen, D.; Szabo, S.; Diaz, L.A.; Goodman, S.N.; David, K.A.; Juhl, H.; et al. Detection and quantification of mutations in the plasma of patients with colorectal tumors. Proc. Natl. Acad. Sci. USA 2005, 102, 16368–16373. [Google Scholar] [CrossRef] [PubMed]
- Postel, M.; Roosen, A.; Laurent-Puig, P.; Taly, V.; Wang-Renault, S.-F. Droplet-based digital PCR and next generation sequencing for monitoring circulating tumor DNA: A cancer diagnostic perspective. Expert Rev. Mol. Diagn. 2017, 18, 7–17. [Google Scholar] [CrossRef] [PubMed]
- Van Ginkel, J.H.; Huibers, M.M.H.; Noorlag, R.; De Bree, R.; Van Es, R.J.J.; Willems, S.M. Liquid biopsy: A future tool for posttreatment surveillance in head and neck cancer? Pathobiology 2017, 84, 115–120. [Google Scholar] [CrossRef]
- Cohen, J.D.; Li, L.; Wang, Y.; Thoburn, C.; Afsari, B.; Danilova, L.; Douville, C.; Javed, A.A.; Wong, F.; Mattox, A.; et al. Detection and localization of surgically resectable cancers with a multi-analyte blood test. Science 2018, 359, 926–930. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Zhao, Q.; Wei, W.; Zheng, L.; Yi, S.; Li, G.; Wang, W.; Sheng, H.; Pu, H.; Mo, H.; et al. Circulating tumor DNA methylation profiles enable early diagnosis, prognosis prediction, and screening for colorectal cancer. Sci. Transl. Med. 2020, 12, eaax7533. [Google Scholar] [CrossRef] [PubMed]
- Dawson, S.J.; Tsui, D.W.; Murtaza, M.; Biggs, H.; Rueda, O.M.; Chin, S.F.; Dunning, M.J.; Gale, D.; Forshew, T.; Mahler-Araujo, B.; et al. Analysis of Circulating Tumor DNA to Monitor Metastatic Breast Cancer. N. Engl. J. Med. 2013, 368, 1199–1209. [Google Scholar] [CrossRef] [PubMed]
- Guo, N.; Lou, F.; Ma, Y.; Li, J.; Yang, B.; Chen, W.; Ye, H.; Zhang, J.; Zhao, M.; Wu, W.; et al. Circulating tumor DNA detection in lung cancer patients before and after surgery. Nat. Publ. Gr. 2016, 6, 1–8. [Google Scholar] [CrossRef]
- Tie, J.; Cohen, J.D.; Wang, Y.; Christie, M.; Simons, K.; Lee, M.; Wong, R.; Kosmider, S.; Ananda, S.; McKendrick, J.; et al. Circulating tumor dna analyses as markers of recurrence risk and benefit of adjuvant therapy for stage III colon cancer. JAMA Oncol. 2019, 5, 1710–1717. [Google Scholar] [CrossRef]
- Garcia-Murillas, I.; Schiavon, G.; Weigelt, B.; Ng, C.; Hrebien, S.; Cutts, R.J.; Cheang, M.; Osin, P.; Nerurkar, A.; Kozarewa, I.; et al. Mutation tracking in circulating tumor DNA predicts relapse in early breast cancer. Sci. Transl. Med. 2015, 7, 302ra133. [Google Scholar] [CrossRef]
- Sausen, M.; Phallen, J.; Adleff, V.; Jones, S.; Leary, R.J.; Barrett, M.T.; Anagnostou, V.; Parpart-Li, S.; Murphy, D.; Li, Q.K.; et al. Clinical implications of genomic alterations in the tumour and circulation of pancreatic cancer patients. Nat. Commun. 2015, 6, 7686. [Google Scholar] [CrossRef]
- Wang, Y.; Springer, S.; Mulvey, C.L.; Silliman, N.; Schaefer, J.; Sausen, M.; James, N.; Rettig, E.M.; Guo, T.; Pickering, C.R.; et al. Detection of somatic mutations and HPV in the saliva and plasma of patients with head and neck squamous cell carcinomas. Sci. Transl. Med. 2015, 7, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Perdomo, S.; Avogbe, P.H.; Foll, M.; Abedi-Ardekani, B.; Lescher Facciolla, V.; Anantharaman, D.; Chopard, P.; Le Calvez-Kelm, F.; Vilensky, M.; Polesel, J.; et al. Circulating tumor DNA detection in head and neck cancer: Evaluation of two different detection approaches. Oncotarget 2017, 8, 72621–72632. [Google Scholar] [CrossRef] [PubMed]
- Egyud, M.; Sridhar, P.; Devaiah, A.; Yamada, E.; Saunders, S.; Ståhlberg, A.; Filges, S.; Krzyzanowski, P.M.; Kalatskaya, I.; Jiao, W.; et al. Plasma circulating tumor DNA as a potential tool for disease monitoring in head and neck cancer. Head Neck 2019, 41, 1351–1358. [Google Scholar] [CrossRef] [PubMed]
- van Ginkel, J.H.; de Leng, W.W.J.; de Bree, R.; van Es, R.J.J.; Willems, S.M. Targeted sequencing reveals TP53 as a potential diagnostic biomarker in the post-treatment surveillance of head and neck cancer. Oncotarget 2016, 7, 61575–61586. [Google Scholar] [CrossRef]
- Chan, K.C.A.; Woo, J.K.S.; King, A.; Zee, B.C.Y.; Lam, W.K.J.; Chan, S.L.; Chu, S.W.I.; Mak, C.; Tse, I.O.L.; Leung, S.Y.M.; et al. Analysis of Plasma Epstein–Barr Virus DNA to Screen for Nasopharyngeal Cancer. N. Engl. J. Med. 2017, 377, 513–522. [Google Scholar] [CrossRef]
- Chera, B.S.; Kumar, S.; Shen, C.; Amdur, R.; Dagan, R.; Green, R.; Goldman, E.; Weiss, J.; Grilley-Olson, J.; Patel, S.; et al. Plasma circulating tumor HPV DNA for the surveillance of cancer recurrence in HPV-associated oropharyngeal cancer. J. Clin. Oncol. 2020, 38, 1050–1058. [Google Scholar] [CrossRef]
- Flach, S.; Howarth, K.; Hackinger, S.; Pipinikas, C.; Ellis, P.; McLay, K.; Marsico, G.; Forshew, T.; Walz, C.; Reichel, C.A.; et al. Liquid biopsy for minimal residual disease detection in head and neck squamous cell carcinoma (LIONESS)—A personalised circulating tumour DNA analysis in head and neck squamous cell carcinoma. Br. J. Cancer 2022, 126, 1186–1195. [Google Scholar] [CrossRef]
- TCGA Network Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature 2015, 517, 576–582. [CrossRef]
- Zhou, G.; Liu, Z.; Myers, J.N. TP53 Mutations in Head and Neck Squamous Cell Carcinoma and Their Impact on Disease Progression and Treatment Response. J. Cell. Biochem. 2016, 117, 2682–2692. [Google Scholar] [CrossRef]
- Stransky, N.; Egloff, A.M.; Tward, A.D.; Kostic, A.D.; Cibulskis, K.; Sivachenko, A.; Kryukov, G.V.; Lawrence, M.S.; Sougnez, C.; McKenna, A.; et al. The Mutational Landscape of Head and Neck Squamous Cell Carcinoma. Science 2011, 333, 1157–1160. [Google Scholar] [CrossRef]
- Brandwein-Gensler, M.; Teixeira, M.S.; Lewis, C.M.; Lee, B. Oral Squamous Cell Carcinoma (OSCC). Am. J. Surg. Pathol. 2005, 29, 140–146. [Google Scholar]
- Bryne, M.; Koppang, H.S.; Lilleng, R.; Stene, T.; Bang, G.; Dabelsteen, E. New malignancy grading is a better prognostic indicator than Broders’ grading in oral squamous cell carcinomas. J. Oral Pathol. Med. 1989, 18, 432–437. [Google Scholar] [CrossRef] [PubMed]
- Pfister, D.G.; Spencer, S.; Adelstein, D.; Al, E. NCCN Guidelines Version 2.2018: Head and Neck Cancers; National Comprehensive Cancer Network: Plymouth Meeting, PA, USA, 2018; 227p. [Google Scholar]
- Bernier, J.; Domenge, C.; Ozsahin, M.; Matuszewska, K.; Lefèbvre, J.L.; Greiner, R.H.; Giralt, J.; Maingon, P.; Rolland, F.; Bolla, M.; et al. Postoperative Irradiation with or without Concomitant Chemotherapy for Locally Advanced Head and Neck Cancer. N. Engl. J. Med. 2004, 350, 1945–1952. [Google Scholar] [CrossRef] [PubMed]
- Cooper, J.S.; Pajak, T.F.; Forastiere, A.A.; Jacobs, J.; Campbell, B.H.; Saxman, S.B.; Kish, J.A.; Kim, H.E.; Cmelak, A.J.; Rotman, M.; et al. Postoperative Concurrent Radiotherapy and Chemotherapy for High-Risk Squamous-Cell Carcinoma of the Head and Neck. N. Engl. J. Med. 2004, 350, 1937–1944. [Google Scholar] [CrossRef]
- Biezuner, T.; Spiro, A.; Raz, O.; Amir, S.; Milo, L.; Adar, R.; Chapal-Ilani, N.; Berman, V.; Fried, Y.; Ainbinder, E.; et al. A generic, cost-effective, and scalable cell lineage analysis platform. Genome Res. 2016, 26, 1588–1599. [Google Scholar] [CrossRef]
- Yang, H.; Wang, K. Genomic variant annotation and prioritization with ANNOVAR and wANNOVAR. Nat. Protoc. 2015, 10, 1556–1566. [Google Scholar] [CrossRef]
- Bettegowda, C.; Sausen, M.; Leary, R.J.; Kinde, I.; Wang, Y.; Agrawal, N.; Bartlett, B.R.; Wang, H.; Luber, B.; Alani, R.M.; et al. Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci. Transl. Med. 2014, 6, 224ra24. [Google Scholar] [CrossRef]
- Perets, R.; Greenberg, O.; Shentzer, T.; Semenisty, V.; Epelbaum, R.; Bick, T.; Sarji, S.; Ben-Izhak, O.; Sabo, E.; Hershkovitz, D. Mutant KRAS Circulating Tumor DNA Is an Accurate Tool for Pancreatic Cancer Monitoring. Oncologist 2018, 23, 566–572. [Google Scholar] [CrossRef]
- Diaz, L.A.; Williams, R.T.; Wu, J.; Kinde, I.; Hecht, J.R.; Berlin, J.; Allen, B.; Bozic, I.; Reiter, J.G.; Nowak, M.A.; et al. The molecular evolution of acquired resistance to targeted EGFR blockade in colorectal cancers. Nature 2012, 486, 537–540. [Google Scholar] [CrossRef]
- Oxnard, G.R.; Paweletz, C.P.; Kuang, Y.; Mach, S.L.; O’Connell, A.; Messineo, M.M.; Luke, J.J.; Butaney, M.; Kirschmeier, P.; Jackman, D.M.; et al. Noninvasive detection of response and resistance in egfrmutant lung cancer using quantitative next-generation genotyping of cell-free plasma DNA. Clin. Cancer Res. 2014, 20, 1698–1705. [Google Scholar] [CrossRef]
- Schirmer, M.A.; Beck, J.; Leu, M.; Oellerich, M.; Rave-Fränk, M.; Walson, P.D.; Schütz, E.; Canis, M. Cell-Free plasma DNA for disease stratification and prognosis in head and neck cancer. Clin. Chem. 2018, 64, 959–970. [Google Scholar] [CrossRef] [PubMed]
- Mes, S.W.; Brink, A.; Sistermans, E.A.; Straver, R.; Oudejans, C.B.; Poell, J.B.; Leemans, C.R.; Brakenhoff, R.H. Comprehensive multiparameter genetic analysis improves circulating tumor DNA detection in head and neck cancer patients. Oral Oncol. 2020, 109, 104852. [Google Scholar] [CrossRef] [PubMed]
- Burgener, J.M.; Zou, J.; Zhao, Z.; Zheng, Y.; Shen, S.Y.; Huang, S.H.; Keshavarzi, S.; Xu, W.; Liu, F.F.; Liu, G.; et al. Tumor-Naïve Multimodal Profiling of Circulating Tumor DNA in Head and Neck Squamous Cell Carcinoma. Clin. Cancer Res. 2021, 27, 4230–4244. [Google Scholar] [CrossRef]
- Wilson, H.L.; D’Agostino, R.B.; Meegalla, N.; Petro, R.; Commander, S.; Topaloglu, U.; Zhang, W.; Porosnicu, M. The Prognostic and Therapeutic Value of the Mutational Profile of Blood and Tumor Tissue in Head and Neck Squamous Cell Carcinoma. Oncologist 2021, 26, e279–e289. [Google Scholar] [CrossRef]
- Muhanna, N.; Di Grappa, M.A.; Chan, H.H.L.; Khan, T.; Jin, C.S.; Zheng, Y.; Irish, J.C.; Bratman, S. V Cell-Free DNA Kinetics in a Pre- Clinical Model of Head and Neck Cancer. Sci. Rep. 2017, 7, 16723. [Google Scholar] [CrossRef]
- Kamat, A.A.; Bischoff, F.Z.; Dang, D.; Baldwin, M.F.; Han, L.Y.; Lin, Y.G.; Merritt, W.M.; Landen, C.N.; Lu, C.; Gershenson, D.M.; et al. Circulating cell-free DNA: A novel biomarker for response to therapy in ovarian carcinoma. Cancer Biol. Ther. 2006, 5, 1369–1374. [Google Scholar] [CrossRef]
- Mazurek, A.M.; Rutkowski, T.; Fiszer-Kierzkowska, A.; Małusecka, E.; Składowski, K. Assessment of the total cfDNA and HPV16/18 detection in plasma samples of head and neck squamous cell carcinoma patients. Oral Oncol. 2016, 54, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Parkinson, C.A.; Gale, D.; Piskorz, A.M.; Biggs, H.; Hodgkin, C.; Addley, H.; Freeman, S.; Moyle, P.; Sala, E.; Sayal, K.; et al. Exploratory Analysis of TP53 Mutations in Circulating Tumour DNA as Biomarkers of Treatment Response for Patients with Relapsed High-Grade Serous Ovarian Carcinoma: A Retrospective Study. PLoS Med. 2016, 13, e1002198. [Google Scholar] [CrossRef]
- Pessoa, L.S.; Heringer, M.; Ferrer, V.P. ctDNA as a cancer biomarker: A broad overview. Crit. Rev. Oncol. Hematol. 2020, 155, 103–109. [Google Scholar] [CrossRef]
- Cortese, R.; Almendros, I.; Wang, Y.; Gozal, D. Tumor circulating DNA profiling in xenografted mice exposed to intermittent hypoxia. Oncotarget 2015, 6, 556–569. [Google Scholar] [CrossRef]
- Kustanovich, A.; Schwartz, R.; Peretz, T.; Grinshpun, A. Life and death of circulating cell-free DNA. Cancer Biol. Ther. 2019, 20, 1057–1067. [Google Scholar] [CrossRef] [PubMed]
- Lipson, E.J.; Velculescu, V.E.; Pritchard, T.S.; Sausen, M.; Pardoll, D.M.; Topalian, S.L.; Diaz, L.A. Circulating tumor DNA analysis as a real-time method for monitoring tumor burden in melanoma patients undergoing treatment with immune checkpoint blockade. J. Immunother. Cancer 2014, 2, 42. [Google Scholar] [CrossRef] [PubMed]
- Lecomte, T.; Berger, A.; Zinzindohoué, F.; Micard, S.; Landi, B.; Blons, H.; Beaune, P.; Cugnenc, P.H.; Laurent-Puig, P. Detection of free-circulating tumor-associated DNA in plasma of colorectal cancer patients and its association with prognosis. Int. J. Cancer 2002, 100, 542–548. [Google Scholar] [CrossRef] [PubMed]


| Characteristic | n (%) |
|---|---|
| Age (median, range) (y) | 65 (35–89) |
| Male sex | 41 (59) |
| Active/past smoker | 39 (56) |
| Tumor site | |
| Oral cavity | 53 (76) |
| Oropharynx | 5 (7) |
| Larynx | 12 (17) |
| T stage | |
| T1 | 12 (17) |
| T2 | 27 (39) |
| T3 | 16 (23) |
| T4 | 15 (21) |
| N stage | |
| N0 | 39 (56) |
| N1 | 6 (9) |
| N2 | 17 (24) |
| N3 | 8 (11) |
| Stage (TNM) | |
| I | 10 (14) |
| II | 17 (24) |
| III | 5 (7) |
| IV | 38 (54) |
| Patient | NA Change | Protein Change | Mutation Type | Circulating cfDNA Concentration (ng/μL) | AF (%) | Noise in WT DNA (%) |
|---|---|---|---|---|---|---|
| 1 | G811C | E271Q | Missense | 0.438 | - | 0.002 |
| 3 | G524A | R175H | Missense | 0.596 | 0.36 | 0.000 |
| 6 | G856A | E286K | Missense | 0.376 | - | 0.019 |
| 7 | 625_626del | R209Kfs*5 | Frameshift del | 0.672 | 0.30 | 0.031 |
| 8 | Splicing | 0.394 | 0.25 | 0.023 | ||
| 9 | C742T | R248W | Missense | 0.610 | 0.51 | 0.000 |
| 10 | C637T | R213X | Nonsense | 0.676 | 0.45 | 0.031 |
| 11 | G473A | R158H | Missense | 0.622 | - | 0.000 |
| 18 | G524A | R175H | Missense | 0.296 | - | 0.000 |
| 19 | A583T | I195F | Missense | 0.468 | 2 | 0.002 |
| 21 | C380T | S127F | Missense | 1.800 | 0.44 | 0.001 |
| 23 | G731T | G244V | Missense | 0.416 | 0.36 | 0.000 |
| 24 | C380T | S127F | Missense | 0.830 | 0.21 | 0.001 |
| 25 | C844T | R282W | Missense | 0.638 | 0.68 | 0.019 |
| 26 | G670T | E224X | Nonsense | 1.440 | 0.21 | 0.000 |
| 27 | A138_T140 | Non-frameshift | 0.438 | 0.50 | 0.000 | |
| 33 | A578T | H193L | Missense | 0.528 | 0.25 | 0.053 |
| 34 | G730T | G244C | Missense | 0.116 | 1.10 | 0.000 |
| 35 | G814A | V272M | Missense | 0.443 | - | 0.002 |
| 40 | C404T | C135F | Missense | 0.282 | 0.30 | 0.000 |
| 52 | A659G | Y220C | Missense | 0.342 | 0.60 | 0.000 |
| 56 | C535T | H179Y | Missense | 0.345 | - | 0.000 |
| 57 | G733A | G245S | Missense | 1.200 | - | 0.000 |
| 59 | C574T | Q192X | Stopgain | 0.602 | 2.50 | 0.053 |
| 62 | C832T | P278S | Missense | 1.570 | - | 0.002 |
| 63 | C844T | R282W | Nonsense | 0.200 | 0.09 | 0.019 |
| 64 | C844T | R282W | Nonsense | 0.462 | 0.35 | 0.019 |
| 67 | A536G | H179R | Missense | 0.374 | 0.08 | 0.000 |
| 69 | G514T | V127F | Nonsense | 0.868 | 0.16 | 0.001 |
| 70 | G743A | R248Q | Missense | 0.354 | - | 0.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kampel, L.; Feldstein, S.; Tsuriel, S.; Hannes, V.; Carmel Neiderman, N.N.; Horowitz, G.; Warshavsky, A.; Leider-Trejo, L.; Hershkovitz, D.; Muhanna, N. Mutated TP53 in Circulating Tumor DNA as a Risk Level Biomarker in Head and Neck Squamous Cell Carcinoma Patients. Biomolecules 2023, 13, 1418. https://doi.org/10.3390/biom13091418
Kampel L, Feldstein S, Tsuriel S, Hannes V, Carmel Neiderman NN, Horowitz G, Warshavsky A, Leider-Trejo L, Hershkovitz D, Muhanna N. Mutated TP53 in Circulating Tumor DNA as a Risk Level Biomarker in Head and Neck Squamous Cell Carcinoma Patients. Biomolecules. 2023; 13(9):1418. https://doi.org/10.3390/biom13091418
Chicago/Turabian StyleKampel, Liyona, Sara Feldstein, Shlomo Tsuriel, Victoria Hannes, Narin N. Carmel Neiderman, Gilad Horowitz, Anton Warshavsky, Leonor Leider-Trejo, Dov Hershkovitz, and Nidal Muhanna. 2023. "Mutated TP53 in Circulating Tumor DNA as a Risk Level Biomarker in Head and Neck Squamous Cell Carcinoma Patients" Biomolecules 13, no. 9: 1418. https://doi.org/10.3390/biom13091418
APA StyleKampel, L., Feldstein, S., Tsuriel, S., Hannes, V., Carmel Neiderman, N. N., Horowitz, G., Warshavsky, A., Leider-Trejo, L., Hershkovitz, D., & Muhanna, N. (2023). Mutated TP53 in Circulating Tumor DNA as a Risk Level Biomarker in Head and Neck Squamous Cell Carcinoma Patients. Biomolecules, 13(9), 1418. https://doi.org/10.3390/biom13091418









