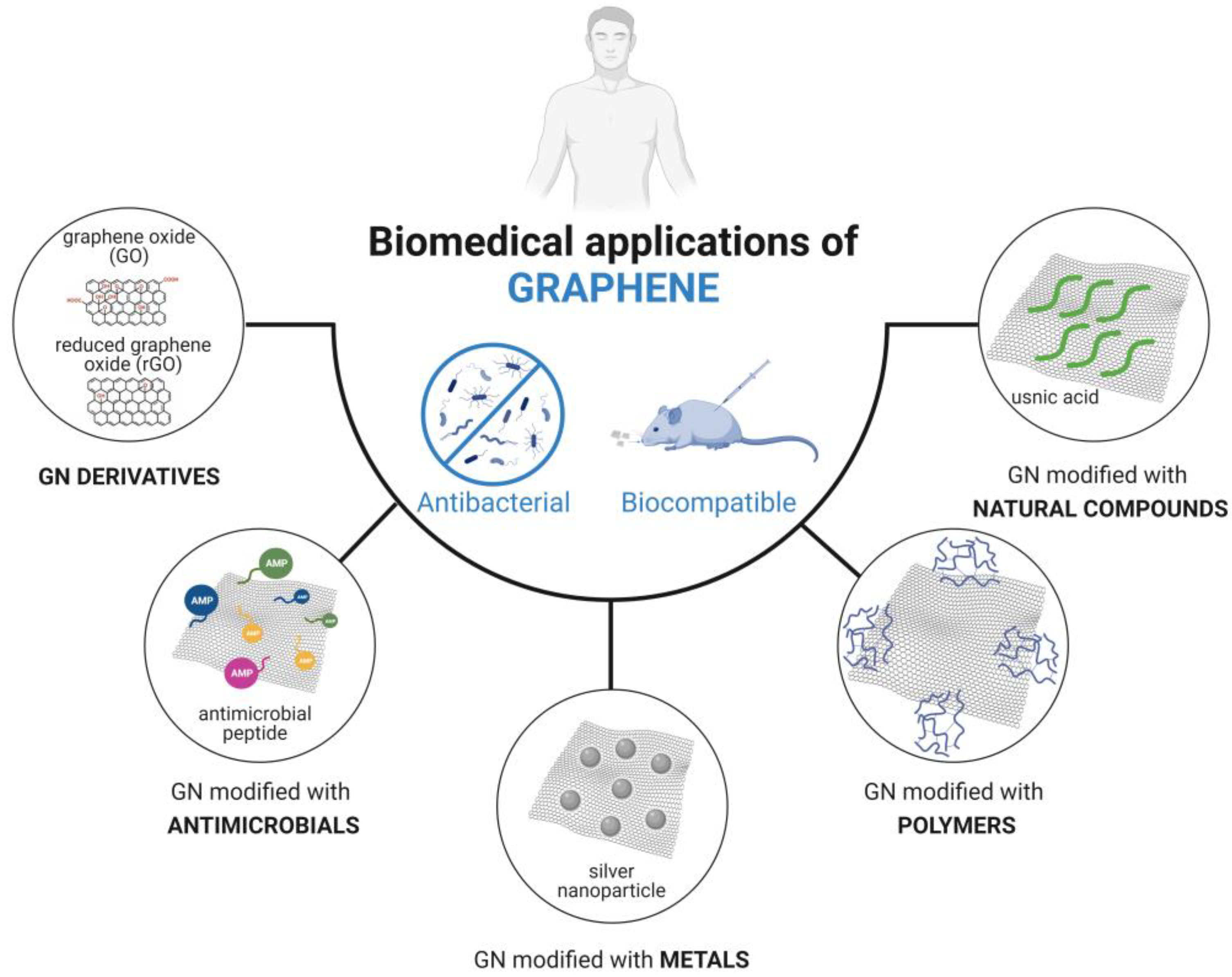
Graphene-Based Composites for Biomedical Applications: Surface Modification for Enhanced Antimicrobial Activity and Biocompatibility
Abstract
:1. Introduction
2. Graphene Modified with Antimicrobials
3. Graphene Modified with Metals
4. Graphene Modified with Polymers
| Graphene Material | Biomedical Application | Biocompatibility | Microorganism | Main Conclusions | Ref. |
|---|---|---|---|---|---|
| Non-natural polymers | |||||
| Polyoxyalkyleneamine (POAA)-graphene oxide (GO) | Surface coatings | NP | Bacillus subtilis Escherichia coli | After 3 h, bacteria exposed to POAA-GO decreased their viability to at least 75%. | [67] |
| Poly(ε-caprolactone) (PCL)-GO | Tissue engineering | Human fibroblasts kept their culturability and proliferation for up to 14 days. | E. coli Staphylococcus epidermidis | PCL-GO composites inactivated S. epidermidis and E. coli adhered cells by 80% after 24 h. | [68] |
| PCL-graphene (GN) | Nasal implants | NP | E. coli Staphylococcus aureus | The efficacy of PCL-GN against S. aureus was about 90%. In contrast, this composite did not exhibit activity against E. coli. | [64] |
| Epoxy-rich-GO (er-GO) | Wound dressing | Human cells exposed to er-GO exhibited viability ratios greater than 100%. | E. coli S. aureus | er-GO composite decreased in vitro E. coli and S. aureus viability by up to 57 and 97%, respectively. In vivo data indicated that E. coli and S. aureus viability was reduced by 47 and 68%, respectively, in presence of er-GO. | [69] * |
| Poly(Lactic-co-Glycolic Acid) (PLGA)-graphene nanoplatelets (GNP) | NE | NP | E. coli | At 15 MHz, PLGA-GNP composites reduced E. coli viability by 33%, while at lower frequencies (10 and 5 MHz), these films decreased bacteria viability by up to 60%. | [9] |
| Polydimethylsiloxane (PDMS)-GNP | Implantable medical devices | NP | Pseudomonas aeruginosa S. aureus | The PDMS-GNP reduced the number of total (57%), viable (69%), culturable (55%), and VBNC cells (85%) of S. aureus biofilms. A decrease of 25% in total cells and about 52% in viable, culturable, and VBNC cells was observed for P. aeruginosa biofilms. | [66] |
| Natural polymers | |||||
| Chitosan (CS)-graphene oxide (GO) | Surface coatings | NP | B. subtilis E. coli | After 3 h, bacteria exposed to CS-GO composite decreased their viability to less than 10%. | [67] |
| CS/poly(vinyl alcohol) (PVA)-GO nanocomposites | Tissue engineering | After 30 days of film implantation, the absence of injuries in the intervened areas with normal healing was observed. | Bacillus cereus S. aureus E. coli Salmonella spp. | Biocomposites containing 0.75 and 1 wt.% GO completely inhibited pathogen growth. | [70] * |
| CS/PVA-GO | Wound healing | CS/PVA-GO hydrogels showed nontoxicity towards pre-osteoblast cells (>70% cell viability). | E. coli S. aureus | Hydrogels exhibited high antimicrobial activity against E. coli and S. aureus (up to 35 and 32 mm inhibition halo, respectively). | [10] |
| CS/polyethylene glycol (PEG)-decorated GO biocomposite | Wound healing | Cell survival on CS/PEG-GO was 95.4%. | E. coli S. aureus | CS, 1 wt% CS/GO and 1 wt% CS/PEG-GO were able to inactivate S. aureus by 80, 85, and 100% and E. coli by 65, 85, and 95%, respectively. | [42] |
| Carboxymethyl Chitosan (CC)-GO-based Sponge | Wound healing | CC/L-cysteine-GO sponge showed a high cell viability rate, as demonstrated by Live/Dead staining. | E. coli S. aureus | In vivo data indicated that the CC/L-cysteine-GO sponge had a faster wound-healing rate than CC/GO. In vitro tests revealed that the addition of L-cysteine-GO and GO to CC increased sponges’ antimicrobial activity. | [43] * |
| Folic acid (FA)/silk fibroin (SF)-GO | Wound healing Tissue engineering | The viability of fibroblast cells exposed to FA/SF-GO for 24 h was 97%. | P. aeruginosa | After 24 h, FA/SF-GO film reduced biofilm formation by 80% compared to control (polystyrene). | [73] |
5. Graphene Modified with Natural Compounds
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wang, J.; Ma, F.; Sun, M. Graphene, hexagonal boron nitride, and their heterostructures: Properties and applications. RSC Adv. 2017, 7, 16801–16822. [Google Scholar] [CrossRef]
- Novoselov, K.S.; Fal’ko, V.I.; Colombo, L.; Gellert, P.R.; Schwab, M.G.; Kim, K. A roadmap for graphene. Nature 2012, 490, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Novoselov, K.S. Nobel Lecture: Graphene: Materials in the Flatland. Rev. Mod. Phys. 2011, 83, 837–849. [Google Scholar] [CrossRef]
- Yang, S.; Feng, X.; Wang, L.; Tang, K.; Maier, J.; Müllen, K. Graphene-Based Nanosheets with a Sandwich Structure. Angew. Chem. Int. Ed. 2010, 49, 4795–4799. [Google Scholar] [CrossRef] [PubMed]
- Magne, T.M.; de Oliveira Vieira, T.; Alencar, L.M.R.; Junior, F.F.M.; Gemini-Piperni, S.; Carneiro, S.V.; Fechine, L.M.U.D.; Freire, R.M.; Golokhvast, K.; Metrangolo, P.; et al. Graphene and its derivatives: Understanding the main chemical and medicinal chemistry roles for biomedical applications. J. Nanostructure Chem. 2022, 12, 693–727. [Google Scholar] [CrossRef] [PubMed]
- Dideikin, A.T.; Vul’, A.Y. Graphene Oxide and Derivatives: The Place in Graphene Family. Front. Phys. 2019, 6, 149. [Google Scholar] [CrossRef]
- Kichukova, D.; Spassova, I.; Kostadinova, A.; Staneva, A.; Kovacheva, D. Facile Synthesized Cu-RGO and Ag-RGO Nanocomposites with Potential Biomedical Applications. Nanomaterials 2022, 12, 2096. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhou, S.; Zhang, Y.; Wu, D.; Yang, X. The dual delivery of growth factors and antimicrobial peptide by PLGA/GO composite biofilms to promote skin-wound healing. New J. Chem. 2020, 44, 1463–1476. [Google Scholar] [CrossRef]
- Zamora-Ledezma, C.; Chicaiza-Zambrano, A.; Santiago Vispo, N.; Debut, A.; Vizuete, K.; Guerrero, V.H.; Almeida, C.E.; Alexis, F. Frequency Based Control of Antifouling Properties Using Graphene Nanoplatelet/Poly(Lactic-co-Glycolic Acid) Composite Films. Compos. Interfaces 2021, 28, 1137–1153. [Google Scholar] [CrossRef]
- Khan, M.U.A.; Yaqoob, Z.; Ansari, M.N.M.; Razak, S.I.A.; Raza, M.A.; Sajjad, A.; Haider, S.; Busra, F.M. Chitosan/Poly Vinyl Alcohol/Graphene Oxide Based pH-Responsive Composite Hydrogel Films: Drug Release, Anti-Microbial and Cell Viability Studies. Polymers 2021, 13, 3124. [Google Scholar] [CrossRef]
- Ji, X.; Xu, Y.; Zhang, W.; Cui, L.; Liu, J. Review of functionalization, structure and properties of graphene/polymer composite fibers. Compos. A Appl. Sci. 2016, 87, 29–45. [Google Scholar] [CrossRef]
- Perumal, S.; Atchudan, R.; Cheong, I.W. Recent Studies on Dispersion of Graphene–Polymer Composites. Polymers 2021, 13, 2375. [Google Scholar] [CrossRef] [PubMed]
- Nanda, S.S.; Papaefthymiou, G.C.; Yi, D.K. Functionalization of Graphene Oxide and its Biomedical Applications. Crit. Rev. Solid. State Mater. Sci. 2015, 40, 291–315. [Google Scholar] [CrossRef]
- Asim, N.; Badiei, M.; Samsudin, N.A.; Mohammad, M.; Razali, H.; Soltani, S.; Amin, N. Application of graphene-based materials in developing sustainable infrastructure: An overview. Compos. B Eng. 2022, 245, 110188. [Google Scholar] [CrossRef]
- Chabot, V.; Higgins, D.; Yu, A.; Xiao, X.; Chen, Z.; Zhang, J. A review of graphene and graphene oxide sponge: Material synthesis and applications to energy and the environment. Energy Environ. Sci. 2014, 7, 1564–1596. [Google Scholar] [CrossRef]
- Sundramoorthy, A.K.; Gunasekaran, S. Applications of graphene in quality assurance and safety of food. TrAC Trends Anal. Chem. 2014, 60, 36–53. [Google Scholar] [CrossRef]
- Sousa-Cardoso, F.; Teixeira-Santos, R.; Campos, A.F.; Lima, M.; Gomes, L.C.; Soares, O.S.G.P.; Mergulhão, F.J. Graphene-Based Coating to Mitigate Biofilm Development in Marine Environments. Nanomaterials 2023, 13, 381. [Google Scholar] [CrossRef]
- Bai, R.G.; Tuvikene, R. Chapter 12—Biomedical Applications of Graphene. In Handbook of Carbon-Based Nanomaterials; Thomas, S., Sarathchandran, C., Ilangovan, S.A., Moreno-Pirajan, J.C., Eds.; Elsevier: Amsterdam, The Netherlands, 2021; pp. 551–571. [Google Scholar]
- Yang, Y.; Asiri, A.M.; Tang, Z.; Du, D.; Lin, Y. Graphene based materials for biomedical applications. Mater. Today 2013, 16, 365–373. [Google Scholar] [CrossRef]
- Shariati, A.; Hosseini, S.M.; Chegini, Z.; Seifalian, A.; Arabestani, M.R. Graphene-Based Materials for Inhibition of Wound Infection and Accelerating Wound Healing. Biomed. Pharmacother. 2023, 158, 114184. [Google Scholar] [CrossRef]
- Arkowski, J.; Obremska, M.; Kędzierski, K.; Sławuta, A.; Wawrzyńska, M. Applications for graphene and its derivatives in medical devices: Current knowledge and future applications. Adv. Clin. Exp. Med. 2020, 29, 1497–1504. [Google Scholar] [CrossRef]
- Yaragalla, S.; Bhavitha, K.B.; Athanassiou, A. A Review on Graphene Based Materials and Their Antimicrobial Properties. Coatings 2021, 11, 1197. [Google Scholar] [CrossRef]
- Akhavan, O.; Ghaderi, E. Toxicity of Graphene and Graphene Oxide Nanowalls Against Bacteria. ACS Nano 2010, 4, 5731–5736. [Google Scholar] [CrossRef] [PubMed]
- Ng, I.M.J.; Shamsi, S. Graphene Oxide (GO): A Promising Nanomaterial against Infectious Diseases Caused by Multidrug-Resistant Bacteria. Int. J. Mol. Sci. 2022, 23, 9096. [Google Scholar] [CrossRef]
- Liu, S.; Zeng, T.H.; Hofmann, M.; Burcombe, E.; Wei, J.; Jiang, R.; Kong, J.; Chen, Y. Antibacterial Activity of Graphite, Graphite Oxide, Graphene Oxide, and Reduced Graphene Oxide: Membrane and Oxidative Stress. ACS Nano 2011, 5, 6971–6980. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, H.; Kumar, A.; Bekyarova, E.; Al-Hadeethi, Y.; Zhang, X.; Chen, M.; Ansari, M.S.; Cochis, A.; Rimondini, L. Antimicrobial Mechanisms and Effectiveness of Graphene and Graphene-Functionalized Biomaterials. A Scope Review. Front. Bioeng. Biotechnol. 2020, 8, 465. [Google Scholar] [CrossRef] [PubMed]
- Mejías Carpio, I.E.; Santos, C.M.; Wei, X.; Rodrigues, D.F. Toxicity of a polymer–graphene oxide composite against bacterial planktonic cells, biofilms, and mammalian cells. Nanoscale 2012, 4, 4746–4756. [Google Scholar] [CrossRef]
- Chen, J.; Peng, H.; Wang, X.; Shao, F.; Yuan, Z.; Han, H. Graphene oxide exhibits broad-spectrum antimicrobial activity against bacterial phytopathogens and fungal conidia by intertwining and membrane perturbation. Nanoscale 2014, 6, 1879–1889. [Google Scholar] [CrossRef]
- Staneva, A.D.; Dimitrov, D.K.; Gospodinova, D.N.; Vladkova, T.G. Antibiofouling Activity of Graphene Materials and Graphene-Based Antimicrobial Coatings. Microorganisms 2021, 9, 1839. [Google Scholar] [CrossRef]
- Deokar Archana, R.; Sinha, M.; Gollavelli, G.; Ling, Y.-C. Antimicrobial Perspectives for Graphene-Based Nanomaterials. In Graphene Science Handbook; CRC Press: Boca Raton, FL, USA, 2016. [Google Scholar]
- Shree, P.; Singh, C.K.; Sodhi, K.K.; Surya, J.N.; Singh, D.K. Biofilms: Understanding the structure and contribution towards bacterial resistance in antibiotics. Med. Microecol. 2023, 16, 100084. [Google Scholar] [CrossRef]
- Zou, X.; Zhang, L.; Wang, Z.; Luo, Y. Mechanisms of the Antimicrobial Activities of Graphene Materials. J. Am. Chem. Soc. 2016, 138, 2064–2077. [Google Scholar] [CrossRef]
- Guo, Z.; Chakraborty, S.; Monikh, F.A.; Varsou, D.-D.; Chetwynd, A.J.; Afantitis, A.; Lynch, I.; Zhang, P. Surface Functionalization of Graphene-Based Materials: Biological Behavior, Toxicology, and Safe-By-Design Aspects. Adv. Biol. 2021, 5, 2100637. [Google Scholar] [CrossRef]
- Zhang, Y.; Hudson-Smith, N.V.; Frand, S.D.; Cahill, M.S.; Davis, L.S.; Feng, Z.V.; Haynes, C.L.; Hamers, R.J. Influence of the Spatial Distribution of Cationic Functional Groups at Nanoparticle Surfaces on Bacterial Viability and Membrane Interactions. J. Am. Chem. Soc. 2020, 142, 10814–10823. [Google Scholar] [CrossRef] [PubMed]
- Peng, C.; Zhang, X. Chemical Functionalization of Graphene Nanoplatelets with Hydroxyl, Amino, and Carboxylic Terminal Groups. Chemistry 2021, 3, 873–888. [Google Scholar] [CrossRef]
- Lan, S.; Zhang, J.; Li, J.; Guo, Y.; Sheng, X.; Dong, A. An N-Halamine/Graphene Oxide-Functionalized Electrospun Polymer Membrane That Inactivates Bacteria on Contact and by Releasing Active Chlorine. Polymers 2021, 13, 2784. [Google Scholar] [CrossRef] [PubMed]
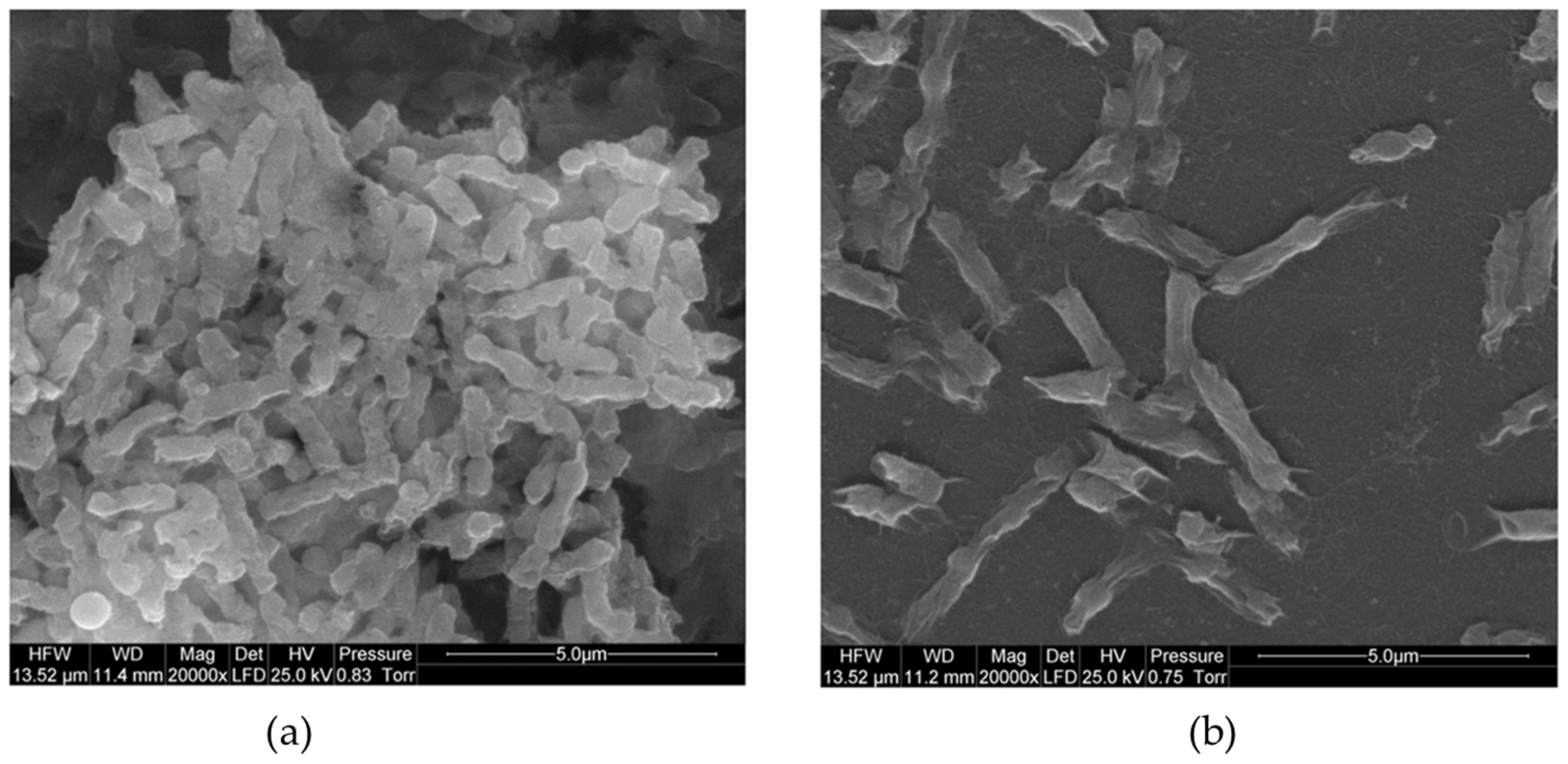
- Sengupta, I.; Bhattacharya, P.; Talukdar, M.; Neogi, S.; Pal, S.K.; Chakraborty, S. Bactericidal effect of graphene oxide and reduced graphene oxide: Influence of shape of bacteria. Colloids Interface Sci. Commun. 2019, 28, 60–68. [Google Scholar] [CrossRef]
- Belo, S.; Sousa-Cardoso, F.; Teixeira-Santos, R.; Gomes, L.C.; Vieira, R.; Sjollema, J.; Soares, O.S.G.P.; Mergulhão, F.J. Production and Characterization of Graphene Oxide Surfaces against Uropathogens. Coatings 2023, 13, 1324. [Google Scholar] [CrossRef]
- Di Giulio, M.; Zappacosta, R.; Di Lodovico, S.; Di Campli, E.; Siani, G.; Fontana, A.; Cellini, L. Antimicrobial and Antibiofilm Efficacy of Graphene Oxide against Chronic Wound Microorganisms. Antimicrob. Agents Chemother. 2018, 62, e00547-18. [Google Scholar] [CrossRef]
- Mai-Prochnow, A.; Clauson, M.; Hong, J.; Murphy, A.B. Gram positive and Gram negative bacteria differ in their sensitivity to cold plasma. Sci. Rep. 2016, 6, 38610. [Google Scholar] [CrossRef]
- Aunkor, M.T.H.; Raihan, T.; Prodhan, S.H.; Metselaar, H.S.C.; Malik, S.U.F.; Azad, A.K. Antibacterial activity of graphene oxide nanosheet against multidrug resistant superbugs isolated from infected patients. R. Soc. Open Sci. 2020, 7, 200640. [Google Scholar] [CrossRef]
- Mohammadi, S.; Babaei, A.; Arab-Bafrani, Z. Polyethylene Glycol-decorated GO Nanosheets as a Well-Organized Nanohybrid to Enhance the Performance of Chitosan Biopolymer. J. Polym. Environ. 2022, 30, 5130–5147. [Google Scholar] [CrossRef]
- Xu, Z.; Zou, L.; Xie, F.; Zhang, X.; Ou, X.; Gao, G. Biocompatible Carboxymethyl Chitosan/GO-Based Sponge to Improve the Efficiency of Hemostasis and Wound Healing. ACS Appl. Mater. Interfaces 2022, 14, 44799–44808. [Google Scholar] [CrossRef] [PubMed]
- Patarroyo, J.L.; Cifuentes, J.; Muñoz, L.N.; Cruz, J.C.; Reyes, L.H. Novel antibacterial hydrogels based on gelatin/polyvinyl-alcohol and graphene oxide/silver nanoconjugates: Formulation, characterization, and preliminary biocompatibility evaluation. Heliyon 2022, 8, e09145. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Pang, Y.X.; Yan, Y.; Qian, P.; Zhao, H.; Manickam, S.; Wu, T.; Pang, C.H. Synthesis and Functionalization of Graphene Materials for Biomedical Applications: Recent Advances, Challenges, and Perspectives. Adv. Sci. 2023, 10, 2205292. [Google Scholar] [CrossRef] [PubMed]
- Liao, C.; Li, Y.; Tjong, S.C. Graphene Nanomaterials: Synthesis, Biocompatibility, and Cytotoxicity. Int. J. Mol. Sci. 2018, 19, 3564. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Kong, H.; Yang, G.; Zhu, D.; Luan, X.; He, P.; Wei, G. Graphene-Based Functional Hybrid Membranes for Antimicrobial Applications: A Review. Appl. Sci. 2022, 12, 4834. [Google Scholar] [CrossRef]
- Tran, D.L.; Le Thi, P.; Hoang Thi, T.T.; Park, K.D. Graphene oxide immobilized surfaces facilitate the sustained release of doxycycline for the prevention of implant related infection. Colloids Surf. B 2019, 181, 576–584. [Google Scholar] [CrossRef]
- Joshi, S.; Siddiqui, R.; Sharma, P.; Kumar, R.; Verma, G.; Saini, A. Green synthesis of peptide functionalized reduced graphene oxide (rGO) nano bioconjugate with enhanced antibacterial activity. Sci. Rep. 2020, 10, 9441. [Google Scholar] [CrossRef]
- Mei, D.; Guo, X.; Wang, Y.; Huang, X.; Guo, L.; Zou, P.; Ge, D.; Wang, X.; Lee, W.; Sun, T.; et al. PEGylated Graphene Oxide Carried OH-CATH30 to Accelerate the Healing of Infected Skin Wounds. Int. J. Nanomed. 2021, 16, 4769–4780. [Google Scholar] [CrossRef]
- Peyriere, H.; Makinson, A.; Marchandin, H.; Reynes, J. Doxycycline in the management of sexually transmitted infections. J. Antimicrob. Chemother. 2018, 73, 553–563. [Google Scholar] [CrossRef]
- Xie, Y.-Y.; Hu, X.-H.; Zhang, Y.-W.; Wahid, F.; Chu, L.-Q.; Jia, S.-R.; Zhong, C. Development and antibacterial activities of bacterial cellulose/graphene oxide-CuO nanocomposite films. Carbohydr. Polym. 2020, 229, 115456. [Google Scholar] [CrossRef]
- Alayande, A.B.; Obaid, M.; Kim, I.S. Antimicrobial mechanism of reduced graphene oxide-copper oxide (rGO-CuO) nanocomposite films: The case of Pseudomonas aeruginosa PAO1. Mater. Sci. Eng. C 2020, 109, 110596. [Google Scholar] [CrossRef] [PubMed]
- Vasilopoulos, V.; Pitou, M.; Fekas, I.; Papi, R.; Ouranidis, A.; Pavlidou, E.; Patsalas, P.; Choli-Papadopoulou, Τ. Graphene-Wrapped Copper Nanoparticles: An Antimicrobial and Biocompatible Nanomaterial with Valuable Properties for Medical Uses. ACS Omega 2020, 5, 26329–26334. [Google Scholar] [CrossRef] [PubMed]
- Wierzbicki, M.; Jaworski, S.; Sawosz, E.; Jung, A.; Gielerak, G.; Jaremek, H.; Łojkowski, W.; Woźniak, B.; Stobiński, L.; Małolepszy, A.; et al. Graphene Oxide in a Composite with Silver Nanoparticles Reduces the Fibroblast and Endothelial Cell Cytotoxicity of an Antibacterial Nanoplatform. Nanoscale Res. Lett. 2019, 14, 320. [Google Scholar] [CrossRef] [PubMed]
- Pipattanachat, S.; Qin, J.; Rokaya, D.; Thanyasrisung, P.; Srimaneepong, V. Biofilm inhibition and bactericidal activity of NiTi alloy coated with graphene oxide/silver nanoparticles via electrophoretic deposition. Sci. Rep. 2021, 11, 14008. [Google Scholar] [CrossRef]
- Noor, N.; Mutalik, S.; Younas, M.W.; Chan, C.Y.; Thakur, S.; Wang, F.; Yao, M.Z.; Mou, Q.; Leung, P.H.-M. Durable Antimicrobial Behaviour from Silver-Graphene Coated Medical Textile Composites. Polymers 2019, 11, 2000. [Google Scholar] [CrossRef]
- Esmaeili, E.; Eslami-Arshaghi, T.; Hosseinzadeh, S.; Elahirad, E.; Jamalpoor, Z.; Hatamie, S.; Soleimani, M. The biomedical potential of cellulose acetate/polyurethane nanofibrous mats containing reduced graphene oxide/silver nanocomposites and curcumin: Antimicrobial performance and cutaneous wound healing. Int. J. Biol. Macromol. 2020, 152, 418–427. [Google Scholar] [CrossRef]
- Li, X.; Li, S.; Bai, Q.; Sui, N.; Zhu, Z. Gold nanoclusters decorated amine-functionalized graphene oxide nanosheets for capture, oxidative stress, and photothermal destruction of bacteria. Colloids Surf. B 2020, 196, 111313. [Google Scholar] [CrossRef]
- Murugesan, B.; Pandiyan, N.; Arumugam, M.; Sonamuthu, J.; Samayanan, S.; Yurong, C.; Juming, Y.; Mahalingam, S. Fabrication of palladium nanoparticles anchored polypyrrole functionalized reduced graphene oxide nanocomposite for antibiofilm associated orthopedic tissue engineering. Appl. Surf. Sci. 2020, 510, 145403. [Google Scholar] [CrossRef]
- Sharma, G.; Prema, D.; Venkataprasanna, K.S.; Prakash, J.; Sahabuddin, S.; Devanand Venkatasubbu, G. Photo induced antibacterial activity of CeO2/GO against wound pathogens. Arab. J. Chem. 2020, 13, 7680–7694. [Google Scholar] [CrossRef]
- Lee, S.J.; Yoon, S.J.; Jeon, I.-Y. Graphene/Polymer Nanocomposites: Preparation, Mechanical Properties, and Application. Polymers 2022, 14, 4733. [Google Scholar] [CrossRef]
- Pinto, A.M.; Moreira, J.A.; Magalhães, F.D.; Gonçalves, I.C. Polymer surface adsorption as a strategy to improve the biocompatibility of graphene nanoplatelets. Colloids Surf. B 2016, 146, 818–824. [Google Scholar] [CrossRef] [PubMed]
- Hajduga, M.B.; Bobiński, R.; Dutka, M.; Ulman-Włodarz, I.; Bujok, J.; Pająk, C.; Ćwiertnia, M.; Kurowska, A.; Dziadek, M.; Rajzer, I. Analysis of the antibacterial properties of polycaprolactone modified with graphene, bioglass and zinc-doped bioglass. Acta Bioeng. Biomech. 2021, 23, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Song, W.; Zhang, Y.; Yu, D.-G.; Tran, C.H.; Wang, M.; Varyambath, A.; Kim, J.; Kim, I. Efficient Synthesis of Folate-Conjugated Hollow Polymeric Capsules for Accurate Drug Delivery to Cancer Cells. Biomacromolecules 2021, 22, 732–742. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, I.M.; Gomes, M.; Gomes, L.C.; Pereira, M.F.R.; Soares, O.S.G.P.; Mergulhão, F.J. Performance of Graphene/Polydimethylsiloxane Surfaces against S. aureus and P. aeruginosa Single- and Dual-Species Biofilms. Nanomaterials 2022, 12, 355. [Google Scholar] [CrossRef]
- Wu, P.-C.; Chen, H.-H.; Chen, S.-Y.; Wang, W.-L.; Yang, K.-L.; Huang, C.-H.; Kao, H.-F.; Chang, J.-C.; Hsu, C.-L.L.; Wang, J.-Y.; et al. Graphene oxide conjugated with polymers: A study of culture condition to determine whether a bacterial growth stimulant or an antimicrobial agent? J. Nanobiotechnol. 2018, 16, 1. [Google Scholar] [CrossRef]
- Melo, S.F.; Neves, S.C.; Pereira, A.T.; Borges, I.; Granja, P.L.; Magalhães, F.D.; Gonçalves, I.C. Incorporation of graphene oxide into poly(ɛ-caprolactone) 3D printed fibrous scaffolds improves their antimicrobial properties. Mater. Sci. Eng. C 2020, 109, 110537. [Google Scholar] [CrossRef]
- Zheng, Y.; Li, S.; Han, D.; Kong, L.; Wang, J.; Zhao, M.; Cheng, W.; Ju, H.; Yang, Z.; Ding, S. Eco-Friendly Preparation of Epoxy-Rich Graphene Oxide for Wound Healing. ACS Biomater. Sci. Eng. 2021, 7, 752–763. [Google Scholar] [CrossRef]
- Ruiz, S.; Tamayo, J.A.; Delgado Ospina, J.; Navia Porras, D.P.; Valencia Zapata, M.E.; Mina Hernandez, J.H.; Valencia, C.H.; Zuluaga, F.; Grande Tovar, C.D. Antimicrobial Films Based on Nanocomposites of Chitosan/Poly(vinyl alcohol)/Graphene Oxide for Biomedical Applications. Biomolecules 2019, 9, 109. [Google Scholar] [CrossRef]
- Yilmaz Atay, H. Antibacterial Activity of Chitosan-Based Systems. In Functional Chitosan: Drug Delivery and Biomedical Applications; Springer: Berlin/Heidelberg, Germany, 2020; pp. 457–489. [Google Scholar]
- Song, W.; Zhang, M.; Huang, X.; Chen, B.; Ding, Y.; Zhang, Y.; Yu, D.G.; Kim, I. Smart l-borneol-loaded hierarchical hollow polymer nanospheres with antipollution and antibacterial capabilities. Mater. Today Chem. 2022, 26, 101252. [Google Scholar] [CrossRef]
- Eivazzadeh-Keihan, R.; Alimirzaloo, F.; Aghamirza Moghim Aliabadi, H.; Bahojb Noruzi, E.; Akbarzadeh, A.R.; Maleki, A.; Madanchi, H.; Mahdavi, M. Functionalized graphene oxide nanosheets with folic acid and silk fibroin as a novel nanobiocomposite for biomedical applications. Sci. Rep. 2022, 12, 6205. [Google Scholar] [CrossRef]
- El-Naggar, M.E.; Abu Ali, O.A.; Saleh, D.I.; Abu-Saied, M.A.; Ahmed, M.K.; Abdel-Fattah, E.; Mansour, S.F. Microstructure, morphology and physicochemical properties of nanocomposites containing hydroxyapatite/vivianite/graphene oxide for biomedical applications. Luminescence 2022, 37, 290–301. [Google Scholar] [CrossRef] [PubMed]
- Pandit, S.; Rahimi, S.; Derouiche, A.; Boulaoued, A.; Mijakovic, I. Sustained release of usnic acid from graphene coatings ensures long term antibiofilm protection. Sci. Rep. 2021, 11, 9956. [Google Scholar] [CrossRef] [PubMed]
- Croitoru, A.-M.; Moroșan, A.; Tihăuan, B.; Oprea, O.; Motelică, L.; Trușcă, R.; Nicoară, A.I.; Popescu, R.-C.; Savu, D.; Mihăiescu, D.E.; et al. Novel Graphene Oxide/Quercetin and Graphene Oxide/Juglone Nanostructured Platforms as Effective Drug Delivery Systems with Biomedical Applications. Nanomaterials 2022, 12, 1943. [Google Scholar] [CrossRef] [PubMed]


| Graphene Material | Biomedical Application | Biocompatibility | Microorganism | Main Conclusions | Ref. |
|---|---|---|---|---|---|
| Doxycycline (Dox)-graphene oxide (GO) immobilized on titanium (TiO2) | Medical devices | Dox-GO/TiO2 did not affect the viability of human fibroblasts (over 80% cell viability). | Escherichia coli Staphylococcus aureus | Dox-GO/TiO2 reduced the viability of adhered bacteria by over 90%, whereas the GO/TiO2 surface inactivated adhered bacteria by 40%. | [48] |
| Antimicrobial peptide (CATH-2)–reduced graphene oxide (rGO) | Medical devices | Functionalized rGO induced low cytotoxicity towards erythrocytes in comparison to rGO alone. | E. coli | Peptide-functionalized rGO exhibited higher antimicrobial activity compared to rGO (13.3- and 21.8-mm inhibition halo). | [49] |
| Antimicrobial peptide (ponericin G1)/growth factor (bFGF)/poly(lactide-co-glycolide (PLGA)-GO composite | Wound healing | Produced composite increased cell proliferation compared to PLGA (p < 0.05). | E. coli S. aureus | Ponericin G1/PLGA-GO reduced bacteria growth compared to PLGA or PLGA-GO composite (p < 0.05). | [8] |
| Antimicrobial peptide (OH30)/polyethylene glycol (PEG)-GO | Wound healing | OH30/PEG-GO had high cell viability (over 80%) and low toxicity. | S. aureus | In vitro data demonstrated that OH30 released by the synthesized composite inhibited S. aureus growth by up to 95% after 3 h. In vivo data indicated that, on day 7, the number of S. aureus in wounds containing the composite was 6 times less than OH30 or PEG-GO (p < 0.05). | [50] * |
| N-halamine-GO fibrous membrane | NS | NP | E. coli | Synthesized composite exhibited high biocidal activity against E. coli (>90%). | [36] |
| Graphene Material | Biomedical Application | Biocompatibility | Microorganism | Main Conclusions | Ref. |
|---|---|---|---|---|---|
| Silver nanoparticles (AgNPs)-reduced graphene oxide (rGO) | Medical textiles | NP | Escherichia coli | AgNPs-rGO composites exhibited enhanced activity against E. coli (100% inactivation) compared to rGO (82.5% inactivation). | [57] |
| AgNPs-graphene oxide (GO) | NE | The viability of human cells was not changed when incubated on nanoplatforms coated with AgNPs-GO. | Salmonella enteritidis | AgNPs-GO nanoplatform significantly inhibited S. enteritidis growth (over 50% cell inactivation). | [55] |
| AgNPs-rGO immobilized into polyurethane/cellulose acetate matrix | Wound healing | In vivo data demonstrated that AgNPs-rGO-based film significantly promoted the wound healing process. | Pseudomonas aeruginosa Staphylococcus aureus | The produced film exhibited an inactivation rate of 100% for Gram-negative bacteria and 95% against Gram-positive bacteria. | [58] * |
| AgNPs-GO deposited on nickel-titanium alloy | Medical devices | NP | Streptococcus mutans | AgNPs-GO reduced the number of S. mutans viable cells by up to 5 Log. | [56] |
| Gold (Au)-decorated amine-functionalized graphene oxide (NH2-GO) | Implant devices | Au-NH2-GO did not affect the viability of human cells (approximately 100% viability). | Bacillus subtilis E. coli P. aeruginosa S. aureus | The synthesized material exhibited a higher (5-fold more) antibacterial activity against Gram-positive and Gram-negative bacteria than bare Au or NH2-GO material. | [59] |
| Copper oxide (CuO)-GO nanohybrids into bacterial cellulose (BC) matrix | NS | CuO-GO/BC film exhibited excellent biocompatibility towards fibroblast cells (>100%). | B. subtilis E. coli P. aeruginosa S. aureus | After 3 h, CuO-GO/BC films completely inactivated Gram-positive bacteria while only reducing the viability of Gram-negative bacteria by 20%. | [52] |
| CuO-rGO | NS | NP | P. aeruginosa | CuO-rGO composites led to complete bacterial inactivation (7 Log reduction). | [53] |
| Copper nanoparticles (CuNPs)-graphene (GN) supported on silicon (Si) wafers | NS | CuNPs-GN/Si showed slight toxicity for human cells (15% reduction in cell viability). | E. coli S. aureus | In the presence of CuNPs-GN/Si films, S. aureus growth was completely inhibited, and E. coli viability was reduced by 87%. | [54] |
| Palladium (Pd)/polypyrrole (PPy)-rGO composite | Tissue engineering | Pd/PPy-rGO (<100 µg/mL) did not substantially affect osteoblast viability (>80%). | B. subtilis E. coli Klebsiella pneumoniae P. aeruginosa | Pd/PPy-rGO nanocomposite significantly inhibited the biofilm formation of B. subtilis (72%), E. coli (90%), K. pneumoniae (89%), and P. aeruginosa (83%). | [60] |
| Cerium oxide (CeO2)-GO | Wound healing | NP | E. coli P. aeruginosa S. aureus Salmonella typhi | CeO2-GO nanocomposite inhibited E. coli, P. aeruginosa, S. aureus, and S. typhi biofilms by 38, 40, 31, and 35%, respectively. | [61] |
| Graphene Material | Biomedical Application | Biocompatibility | Microorganism | Main Conclusions | Ref. |
|---|---|---|---|---|---|
| Hydroxyapatite/Vivianite-GO | NS | Cell viability of osteoblasts in the presence of this composite was 98%. | E. coli S. aureus | Composite exhibited activity against E. coli and S. aureus after 24 h (14.5 and 13.4 mm inhibition halo, respectively). | [74] |
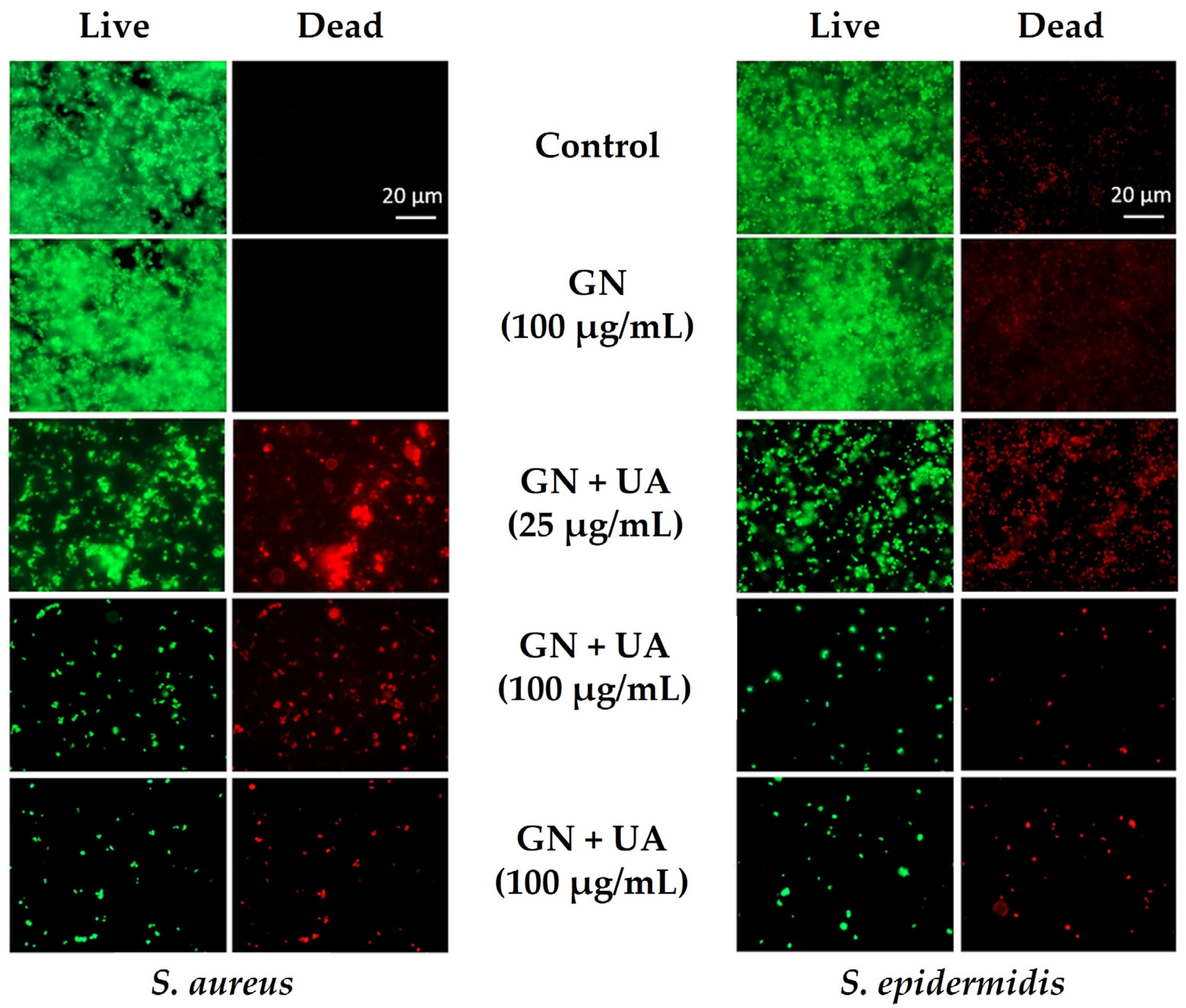
| Usnic acid (UA)-GN | Medical devices | NP | S. aureus Staphylococcus epidermidis | After 24 h, UA-GN inhibited S. aureus and S. epidermidis biofilms by 3 Log at 25, 50, 100, and 200 µg/mL AU/GO compared to GN films and glass, except for S. aureus growing on 25 µg/mL AU-GN. After 96 h, staphylococcal biofilms were reduced by 5 Log compared to the control (glass). | [75] |
| Quercetin-GO | Drug delivery systems | GO-based materials showed a biocompatible behavior at lower concentrations (>70% cell viability). | E. coli S. aureus | Quercetin/GO composites reduced S. aureus culturability by 1 Log and E. coli culturability by 5 Log. | [76] |
| Juglone-GO | Drug delivery systems | Materials showed a biocompatible behavior at lower concentrations (>70% cell viability). | E. coli S. aureus | Juglone/GO composites reduced S. aureus culturability by 3 Log and E. coli culturability by 5 Log. | [76] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Teixeira-Santos, R.; Belo, S.; Vieira, R.; Mergulhão, F.J.M.; Gomes, L.C. Graphene-Based Composites for Biomedical Applications: Surface Modification for Enhanced Antimicrobial Activity and Biocompatibility. Biomolecules 2023, 13, 1571. https://doi.org/10.3390/biom13111571
Teixeira-Santos R, Belo S, Vieira R, Mergulhão FJM, Gomes LC. Graphene-Based Composites for Biomedical Applications: Surface Modification for Enhanced Antimicrobial Activity and Biocompatibility. Biomolecules. 2023; 13(11):1571. https://doi.org/10.3390/biom13111571
Chicago/Turabian StyleTeixeira-Santos, Rita, Samuel Belo, Rita Vieira, Filipe J. M. Mergulhão, and Luciana C. Gomes. 2023. "Graphene-Based Composites for Biomedical Applications: Surface Modification for Enhanced Antimicrobial Activity and Biocompatibility" Biomolecules 13, no. 11: 1571. https://doi.org/10.3390/biom13111571
APA StyleTeixeira-Santos, R., Belo, S., Vieira, R., Mergulhão, F. J. M., & Gomes, L. C. (2023). Graphene-Based Composites for Biomedical Applications: Surface Modification for Enhanced Antimicrobial Activity and Biocompatibility. Biomolecules, 13(11), 1571. https://doi.org/10.3390/biom13111571






