Increase in Serum MMP-9 and TIMP-1 Concentrations during Alcohol Intoxication in Adolescents—A Preliminary Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Global Status Report on Alcohol and Health 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Hyun, J.; Han, J.; Lee, C.; Yoon, M.; Jung, Y. Pathophysiological Aspects of Alcohol Metabolism in the Liver. Int. J. Mol. Sci. 2021, 22, 5717. [Google Scholar] [CrossRef] [PubMed]
- Pohl, K.; Moodley, P.; Dhanda, A.D. Alcohol’s Impact on the Gut and Liver. Nutrients 2021, 13, 3170. [Google Scholar] [CrossRef] [PubMed]
- Crabb, D.W.; Im, G.Y.; Szabo, G.; Mellinger, J.L.; Lucey, M.R. Diagnosis and Treatment of Alcohol-Associated Liver Diseases: 2019 Practice Guidance From the American Association for the Study of Liver Diseases. Hepatology 2020, 71, 306–333. [Google Scholar] [CrossRef] [PubMed]
- Le Daré, B.; Lagente, V.; Gicquel, T. Ethanol and its metabolites: Update on toxicity, benefits, and focus on immunomodulatory effects. Drug Metab. Rev. 2019, 51, 545–561. [Google Scholar] [CrossRef]
- Lackner, C.; Stauber, R.E.; Davies, S.; Denk, H.; Dienes, H.P.; Gnemmi, V.; Guido, M.; Miquel, R.; Paradis, V.; Schirmacher, P.; et al. Development and prognostic relevance of a histologic grading and staging system for alcohol-related liver disease. J. Hepatol. 2021, 75, 810–819. [Google Scholar] [CrossRef]
- Enomoto, H.; Bando, Y.; Nakamura, H.; Nishiguchi, S.; Koga, M. Liver fibrosis markers of nonalcoholic steatohepatitis. World J. Gastroenterol. 2015, 21, 7427–7435. [Google Scholar] [CrossRef]
- Charzewski, Ł.; Krzyśko, K.A.; Lesyng, B. Structural characterisation of inhibitory and non-inhibitory MMP-9-TIMP-1 complexes and implications for regulatory mechanisms of MMP-9. Sci. Rep. 2021, 11, 13376. [Google Scholar] [CrossRef]
- Jotwani, R.; Eswaran, S.V.; Moonga, S.; Cutler, C.W. MMP-9/TIMP-1 imbalance induced in human dendritic cells by Porphyromonas gingivalis. FEMS Immunol. Med. Microbiol. 2010, 58, 314–321. [Google Scholar] [CrossRef]
- Schuppan, D.; Surabattula, R.; Wang, X.Y. Determinants of fibrosis progression and regression in NASH. J. Hepatol. 2018, 68, 238–250. [Google Scholar] [CrossRef]
- Cicoira, M.; Rossi, A.; Bonapace, S.; Zanolla, L.; Golia, G.; Franceschini, L.; Caruso, B.; Marino, P.N.; Zardini, P. Independent and additional prognostic value of aminoterminal propeptide of type III procollagen circulating levels in patients with chronic heart failure. J. Card. Fail. 2004, 10, 403–411. [Google Scholar] [CrossRef]
- Lachowski, D.; Cortes, E.; Rice, A.; Pinato, D.; Rombouts, K.; Del Rio Hernandez, A. Matrix stiffness modulates the activity of MMP-9 and TIMP-1 in hepatic stellate cells to perpetuate fibrosis. Sci. Rep. 2019, 9, 7299. [Google Scholar] [CrossRef] [PubMed]
- Mukamal, K.J. A safe level of alcohol consumption: The right answer demands the right question. J. Intern. Med. 2020, 288, 550–559. [Google Scholar] [CrossRef] [PubMed]
- Torp, N.; Israelsen, M.; Nielsen, M.J.; Åstrand, C.P.; Juhl, P.; Johansen, S.; Hansen, C.D.; Madsen, B.; Villesen, I.F.; Leeming, D.J.; et al. Binge drinking induces an acute burst of markers of hepatic fibrogenesis (PRO-C3). Liver Int. 2022, 42, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Zdanowicz, K.; Olanski, W.; Kowalczuk-Kryston, M.; Bobrus-Chociej, A.; Werpachowska, I.; Lebensztejn, D.M. Total Keratin-18 (M65) as a Potential, Early, Non-Invasive Biomarker of Hepatocyte Injury in Alcohol Intoxicated Adolescents-A Preliminary Study. Biomolecules 2021, 11, 911. [Google Scholar] [CrossRef]
- Cordell, R.L.; Pandya, H.; Hubbard, M.; Turner, M.A.; Monks, P.S. GC-MS analysis of ethanol and other volatile compounds in micro-volume blood samples--quantifying neonatal exposure. Anal. Bioanal. Chem. 2013, 405, 4139–4147. [Google Scholar] [CrossRef]
- Liangpunsakul, S.; Qi, R.; Crabb, D.W.; Witzmann, F. Relationship between alcohol drinking and aspartate aminotransferase:alanine aminotransferase (AST:ALT) ratio, mean corpuscular volume (MCV), gamma-glutamyl transpeptidase (GGT), and apolipoprotein A1 and B in the U.S. population. J. Stud. Alcohol. Drugs 2010, 71, 249–252. [Google Scholar] [CrossRef]
- Ohashi, K.; Pimienta, M.; Seki, E. Alcoholic liver disease: A current molecular and clinical perspective. Liver Res. 2018, 2, 161–172. [Google Scholar] [CrossRef]
- Cabral-Pacheco, G.A.; Garza-Veloz, I.; Castruita-De la Rosa, C.; Ramirez-Acuña, J.M.; Perez-Romero, B.A.; Guerrero-Rodriguez, J.F.; Martinez-Avila, N.; Martinez-Fierro, M.L. The Roles of Matrix Metalloproteinases and Their Inhibitors in Human Diseases. Int. J. Mol. Sci. 2020, 21, 9739. [Google Scholar] [CrossRef]
- Aiken, A.; Clare, P.J.; Wadolowski, M.; Hutchinson, D.; Najman, J.M.; Slade, T.; Bruno, R.; McBride, N.; Kypri, K.; Mattick, R.P. Age of Alcohol Initiation and Progression to Binge Drinking in Adolescence: A Prospective Cohort Study. Alcohol. Clin. Exp. Res. 2018, 42, 100–110. [Google Scholar] [CrossRef]
- Center for Behaviora Health, Statistics. 2016 National Survey on Drug Use and Health Public Use File Codebook. Substance. Abuse and Mental Health Services Administration 2017. Available online: http://www.samhsa.gov/ (accessed on 1 February 2022).
- Lees, B.; Meredith, L.R.; Kirkland, A.E.; Bryant, B.E.; Squeglia, L.M. Effect of alcohol use on the adolescent brain and behavior. Pharmacol. Biochem. Behav. 2020, 192, 172906. [Google Scholar] [CrossRef]
- Hagström, H.; Hemmingsson, T.; Discacciati, A.; Andreasson, A. Alcohol consumption in late adolescence is associated with an increased risk of severe liver disease later in life. J. Hepatol. 2018, 68, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Hagström, H.; Hemmingsson, T.; Discacciati, A.; Andreasson, A. Risk Behaviors Associated with Alcohol Consumption Predict Future Severe Liver Disease. Dig. Dis. Sci. 2019, 64, 2014–2023. [Google Scholar] [CrossRef] [PubMed]
- Roderfeld, M. Matrix metalloproteinase functions in hepatic injury and fibrosis. Matrix Biol. 2018, 68–69, 452–462. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Liu, X.; Zhang, J.; Lu, L.; Feng, M.; Wang, J. Dynamic features of liver fibrogenesis and fibrosis resolution in the absence of matrix metalloproteinase-9. Mol. Med. Rep. 2019, 20, 5239–5248. [Google Scholar] [CrossRef]
- Li, Y.; Liu, H.; Xu, L. Expression of MMP-9 in different degrees of chronic hepatitis B and its correlation with inflammation. Exp. Ther. Med. 2018, 16, 4136–4140. [Google Scholar] [CrossRef]
- D’Amico, F.; Consolo, M.; Amoroso, A.; Skarmoutsou, E.; Mauceri, B.; Stivala, F.; Stivala, F.; Malaponte, G.; Bertino, G.; Neri, S.; et al. Liver immunolocalization and plasma levels of MMP-9 in non-alcoholic steatohepatitis (NASH) and hepatitis C infection. Acta Histochem. 2010, 112, 474–481. [Google Scholar] [CrossRef]
- Lebensztejn, D.M.; Sobaniec-Lotowska, M.E.; Kaczmarski, M.; Voelker, M.; Schuppan, D. Matrix-derived serum markers in monitoring liver fibrosis in children with chronic hepatitis B treated with interferon alpha. World J. Gastroenterol. 2006, 12, 3338–3343. [Google Scholar] [CrossRef]
- Wei, L.; Shao, C.; Luo, L.; He, H.; Xv, S.; Shi, L.; Qiu, S.; Gu, H.; Zhu, C.; Chen, J.; et al. Predictive Value of the Serum Matrix Metalloproteinase-9 Level on Hepatic Encephalopathy in Patients with Chronic Liver Disease. Ann. Clin. Lab. Sci. 2021, 51, 713–720. [Google Scholar]
- Daniluk, U.; Daniluk, J.; Guzinska-Ustymowicz, K.; Pryczynicz, A.; Lebensztejn, D. Usefulness of metalloproteinase-9 and tissue inhibitor of metalloproteinase-1 in clinical characterisation of children with newly diagnosed Crohn’s disease. J. Paediatr. Child. Health 2020, 56, 1233–1241. [Google Scholar] [CrossRef]
- Prystupa, A.; Boguszewska-Czubara, A.; Bojarska-Junak, A.; Toruń-Jurkowska, A.; Roliński, J.; Załuska, W. Activity of MMP-2, MMP-8 and MMP-9 in serum as a marker of progression of alcoholic liver disease in people from Lublin Region, eastern Poland. Ann. Agric. Environ. Med. 2015, 22, 325–328. [Google Scholar] [CrossRef]
- Roeb, E. Matrix metalloproteinases and liver fibrosis (translational aspects). Matrix Biol. 2018, 68–69, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Latronico, T.; Mascia, C.; Pati, I.; Zuccala, P.; Mengoni, F.; Marocco, R.; Tieghi, T.; Belvisi, V.; Lichtner, M.; Vullo, V.; et al. Liver Fibrosis in HCV Monoinfected and HIV/HCV Coinfected Patients: Dysregulation of Matrix Metalloproteinases (MMPs) and Their Tissue Inhibitors TIMPs and Effect of HCV Protease Inhibitors. Int. J. Mol. Sci. 2016, 17, 455. [Google Scholar] [CrossRef] [PubMed]
- Karsdal, M.A.; Daniels, S.J.; Holm Nielsen, S.; Bager, C.; Rasmussen, D.G.K.; Loomba, R.; Surabattula, R.; Villesen, I.F.; Luo, Y.; Shevell, D.; et al. Collagen biology and non-invasive biomarkers of liver fibrosis. Liver Int. 2020, 40, 736–750. [Google Scholar] [CrossRef] [PubMed]
- Israelsen, M.; Kim, M.; Suvitaival, T.; Madsen, B.S.; Hansen, C.D.; Torp, N.; Trost, K.; Thiele, M.; Hansen, T.; Legido-Quigley, C.; et al. Comprehensive lipidomics reveals phenotypic differences in hepatic lipid turnover in ALD and NAFLD during alcohol intoxication. JHEP Rep. 2021, 3, 100325. [Google Scholar] [CrossRef]
- Sørensen, M.D.; Thiele, M.; Krag, A.; Daniels, S.J.; Leeming, D.J.; Karsdal, M.; Detlefsen, S. Stage-dependent expression of fibrogenic markers in alcohol-related liver disease. Pathol. Res. Pract. 2022, 231, 153798. [Google Scholar] [CrossRef]
- Mak, A.L.; Lee, J.; van Dijk, A.M.; Vali, Y.; Aithal, G.P.; Schattenberg, J.M.; Anstee, Q.M.; Brosnan, M.J.; Zafarmand, M.H.; Ramsoekh, D.; et al. Systematic Review with Meta-Analysis: Diagnostic Accuracy of Pro-C3 for Hepatic Fibrosis in Patients with Non-Alcoholic Fatty Liver Disease. Biomedicines 2021, 9, 1920. [Google Scholar] [CrossRef]
- Madsen, B.S.; Thiele, M.; Detlefsen, S.; Kjaergaard, M.; Møller, L.S.; Trebicka, J.; Nielsen, M.J.; Gudmann, N.S.; Leeming, D.J.; Karsdal, M.A.; et al. PRO-C3 and ADAPT algorithm accurately identify patients with advanced fibrosis due to alcohol-related liver disease. Aliment. Pharmacol. Ther. 2021, 54, 699–708. [Google Scholar] [CrossRef]
- Sorva, R.; Anttila, R.; Siimes, M.A.; Sorva, A.; Tähtelä, R.; Turpeinen, M. Serum markers of collagen metabolism and serum osteocalcin in relation to pubertal development in 57 boys at 14 years of age. Pediatr. Res. 1997, 42, 528–532. [Google Scholar] [CrossRef][Green Version]
| Parameter | Study Group (n = 57) | Control Group (n = 24) | p |
|---|---|---|---|
| Alcohol (g/L) | 1.78 (0.48–3.26) | - | NA |
| Age (years) | 15 (12–17) | 16 (12–17) | NS |
| ALT (IU/L) | 13 (7–48) | 13 (11–15) | NS |
| AST (IU/L) | 22 (14–45) | 20 (14–29) | NS |
| PIIINP (ng/mL) | 25.66 (14.34–48.42) | 24.67 (12.96–40.82) | NS |
| Collagen IV (ng/mL) | 68.11 (40.72–121.1) | 70.79 (43.16–108.1) | NS |
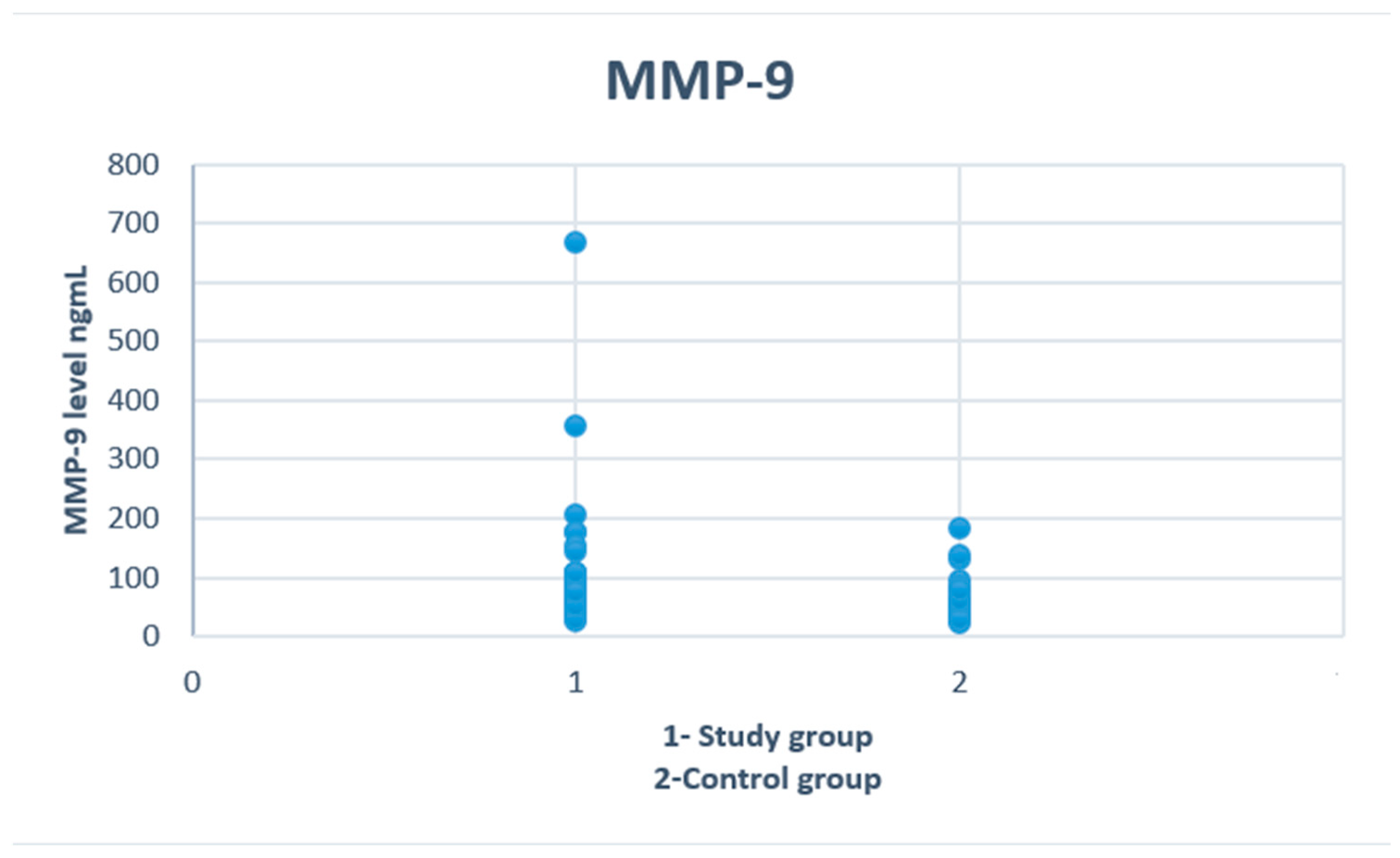
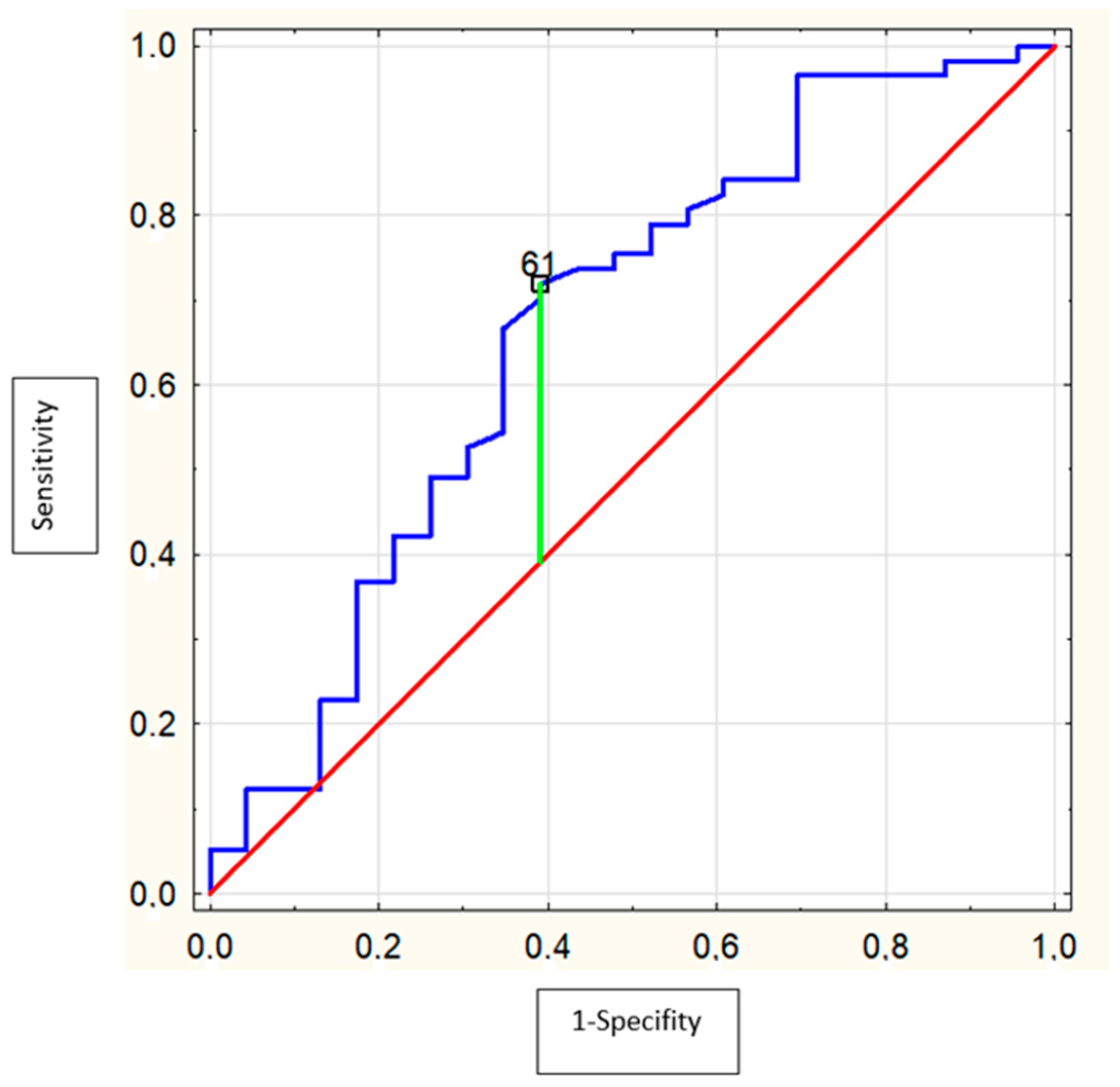
| MMP-9 (ng/mL) | 72.4 (26.4–667.4) | 58 (22.8–183.0) | 0.02 * |
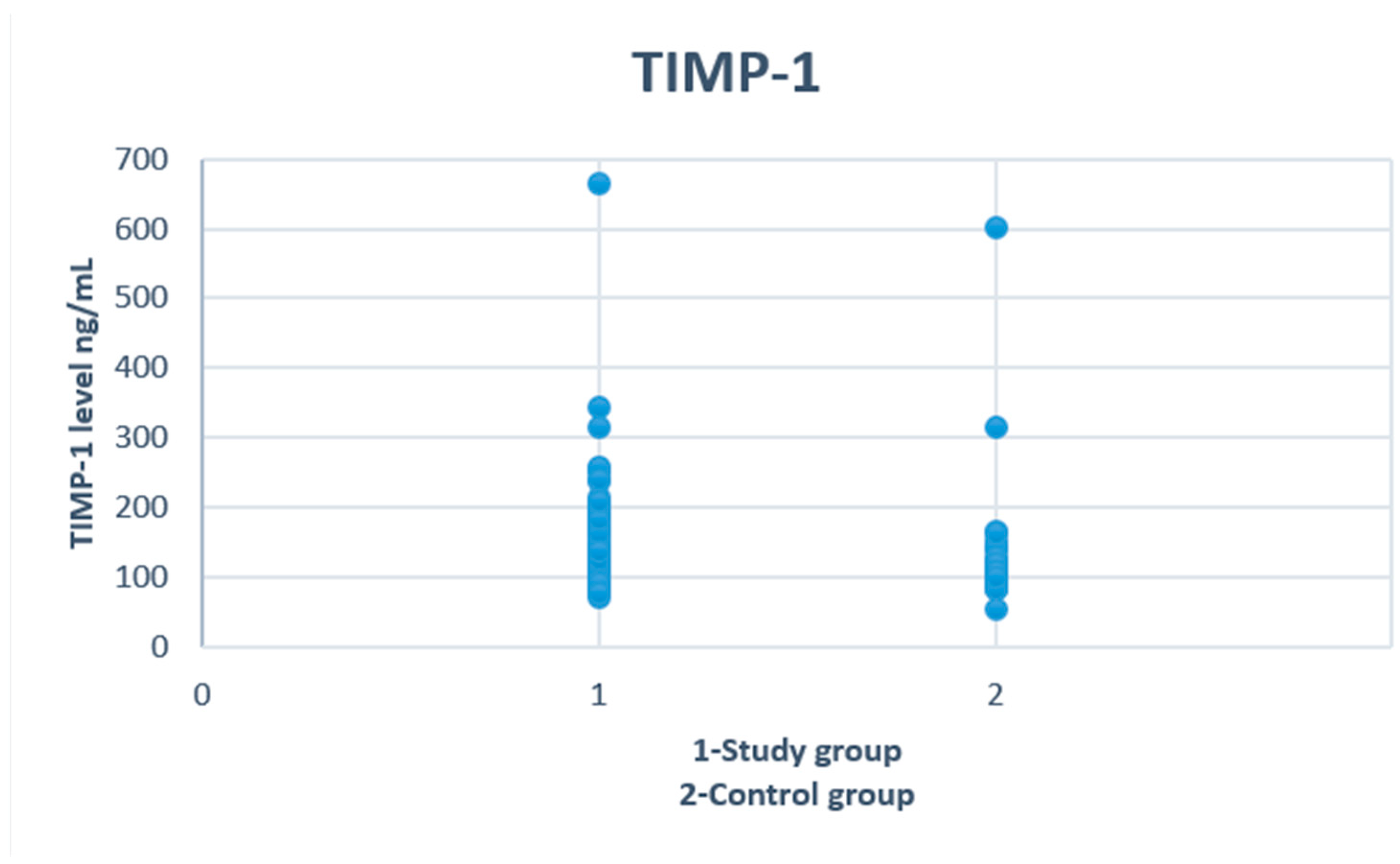
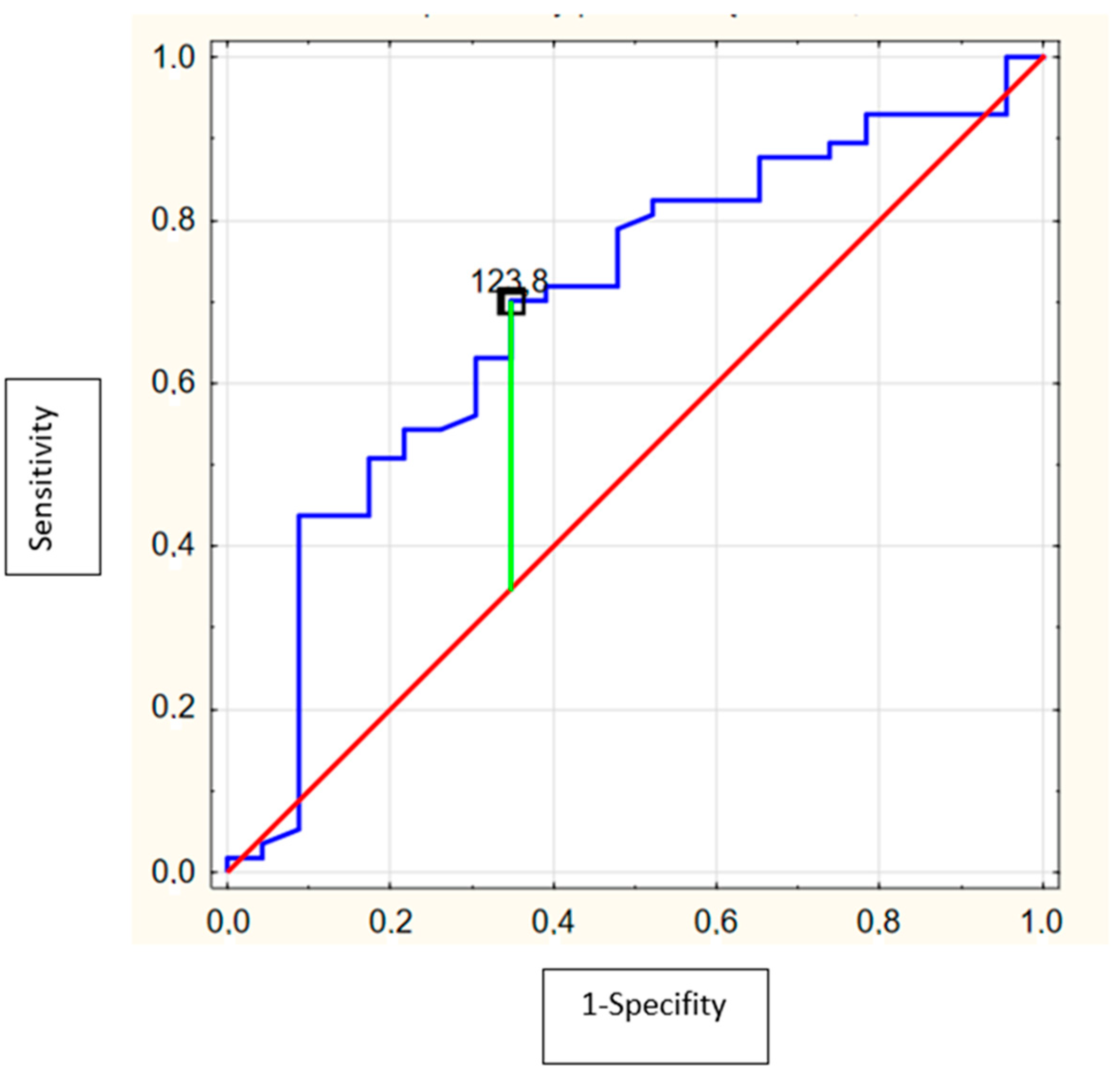
| TIMP-1 (ng/mL) | 153.4 (71.1–665.0) | 110.3 (54.0–601.0) | 0.007 * |
| MMP-9/TIMP-1 ratio | 0.5 (0.21–1.04) | 0.52 (0.22–1.15) | NS |
| Parameter | 12–15 Years (n = 30) | 16–17 Years (n = 27) | p |
|---|---|---|---|
| Alcohol (g/L) | 1.64 (0.48–3.26) | 2.06 (0.51–3.06) | 0.02 * |
| ALT (IU/L) | 13 (9–48) | 13 (7–38) | NS |
| AST (IU/L) | 21 (14–45) | 22 (15–35) | NS |
| Bilirubin (mg/dL) | 0.35 (0.15–1.49) | 0.32 (0.15–1.57) | NS |
| CK (IU/L) | 218 (88–923) | 193 (79–624) | NS |
| CK-MB (IU/L) | 21 (13–32) | 19 (11–55) | NS |
| Urea (mg/dL) | 23 (12–35) | 21 (10–36) | NS |
| PIIINP (ng/mL) | 27.74 (14,34–45.9) | 24.81 (19–48.42) | NS |
| Collagen IV (ng/mL) | 73.59 (40.72–121.1) | 67.59 (50.94–120.29) | NS |
| MMP-9 (ng/mL) | 69.2 (26.4–667.4) | 74.6 (39.8–355.4) | NS |
| TIMP-1 (ng/mL) | 134.55 (71.1–665) | 176.1 (96.6–342.8) | 0.03 * |
| MMP-9/TIMP-1 ratio | 0.57 (0.21–1) | 0.43 (0.21–1.04) | NS |
| Parameter | BAC < 1.78 (n = 28) | BAC ≥ 1.78 (n = 29) | p |
|---|---|---|---|
| Age (year) | 15 (12–17) | 16 (12–17) | NS |
| ALT (IU/L) | 13 (7–38) | 13 (8–48) | NS |
| AST (IU/L) | 22 (15–45) | 22 (14–42) | NS |
| Bilirubin (mg/dL) | 0.31 (0.15–1.49) | 0.33 (0.15–1.57) | NS |
| CK (IU/L) | 218 (88–923) | 202 (79–624) | NS |
| CK-MB (IU/L) | 20 (11–43) | 20 (13–55) | NS |
| Urea (mg/dL) | 23 (12–35) | 21 (10–36) | NS |
| PIIINP (ng/mL) | 25.66 (14.34–40.18) | 26.05 (18.3–48.42) | NS |
| Collagen IV (ng/mL) | 67.45 (40.72–104.32) | 69.77 (46.34–121.1) | NS |
| MMP-9 (ng/mL) | 69.2 (26.4–667.4) | 74.6 (39.8–205.2) | NS |
| TIMP-1 (ng/mL) | 148.8 (71.7–665) | 163.3 (83.6–253.8) | NS |
| MMP-9/TIMP-1 ratio | 0.59 (0.21–1) | 0.43 (0.21–1.04) | NS |
| PIIINP | Collagen IV | MMP-9 | TIMP-1 | MMP-9/TIMP-1 Ratio | |
|---|---|---|---|---|---|
| ALT | R = 0.28 p = 0.04 * | R = 0.34 p = 0.008 * | R = 0.38 p = 0.004 * | R = 0.47 p < 0.0001 * | R = 0.3; p = 0.02 * |
| AST | R = 0.42 p = 0.001 * | R = 0.42 p = 0.001 * | R = 0.23 p = 0.09 * | R = 0.29 p = 0.03 * | R = 0.3; p = 0.01 * |
| Total bilirubin | R = 0.44 p = 0.001 * | R = 0.44 p = 0.001 * | R = 0.39 p = 0.004 * | R = 0.32 p = 0.018 * | NS |
| CK | R = 0.3 p = 0.03 * | R = 0.3 p = 0.03 * | R = 0.24 p = 0.08 * | R = 0.28 p = 0.04 * | R = 0.38; p = 0.005 * |
| CK-MB | R = 0.33 p = 0.01 * | NS | NS | NS | R = 0.3; p = 0.03 * |
| Urea | R = 0.35 p = 0.008 * | R = 0.35 p = 0.008 * | NS | NS | R = 0.28; p = 0.04 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zdanowicz, K.; Kowalczuk-Kryston, M.; Olanski, W.; Werpachowska, I.; Mielech, W.; Lebensztejn, D.M. Increase in Serum MMP-9 and TIMP-1 Concentrations during Alcohol Intoxication in Adolescents—A Preliminary Study. Biomolecules 2022, 12, 710. https://doi.org/10.3390/biom12050710
Zdanowicz K, Kowalczuk-Kryston M, Olanski W, Werpachowska I, Mielech W, Lebensztejn DM. Increase in Serum MMP-9 and TIMP-1 Concentrations during Alcohol Intoxication in Adolescents—A Preliminary Study. Biomolecules. 2022; 12(5):710. https://doi.org/10.3390/biom12050710
Chicago/Turabian StyleZdanowicz, Katarzyna, Monika Kowalczuk-Kryston, Witold Olanski, Irena Werpachowska, Wlodzimierz Mielech, and Dariusz Marek Lebensztejn. 2022. "Increase in Serum MMP-9 and TIMP-1 Concentrations during Alcohol Intoxication in Adolescents—A Preliminary Study" Biomolecules 12, no. 5: 710. https://doi.org/10.3390/biom12050710
APA StyleZdanowicz, K., Kowalczuk-Kryston, M., Olanski, W., Werpachowska, I., Mielech, W., & Lebensztejn, D. M. (2022). Increase in Serum MMP-9 and TIMP-1 Concentrations during Alcohol Intoxication in Adolescents—A Preliminary Study. Biomolecules, 12(5), 710. https://doi.org/10.3390/biom12050710






