Role of Urinary Kidney Stress Biomarkers for Early Recognition of Subclinical Acute Kidney Injury in Critically Ill COVID-19 Patients
Abstract
:1. Introduction
2. Methods
2.1. Study Population
2.2. Definition of Acute Kidney Injury
2.3. Biomarker Determinations
2.4. Statistical Analysis
3. Results
3.1. Characteristics of Study Population
3.2. Performance of Biomarkers as AKI Predictors
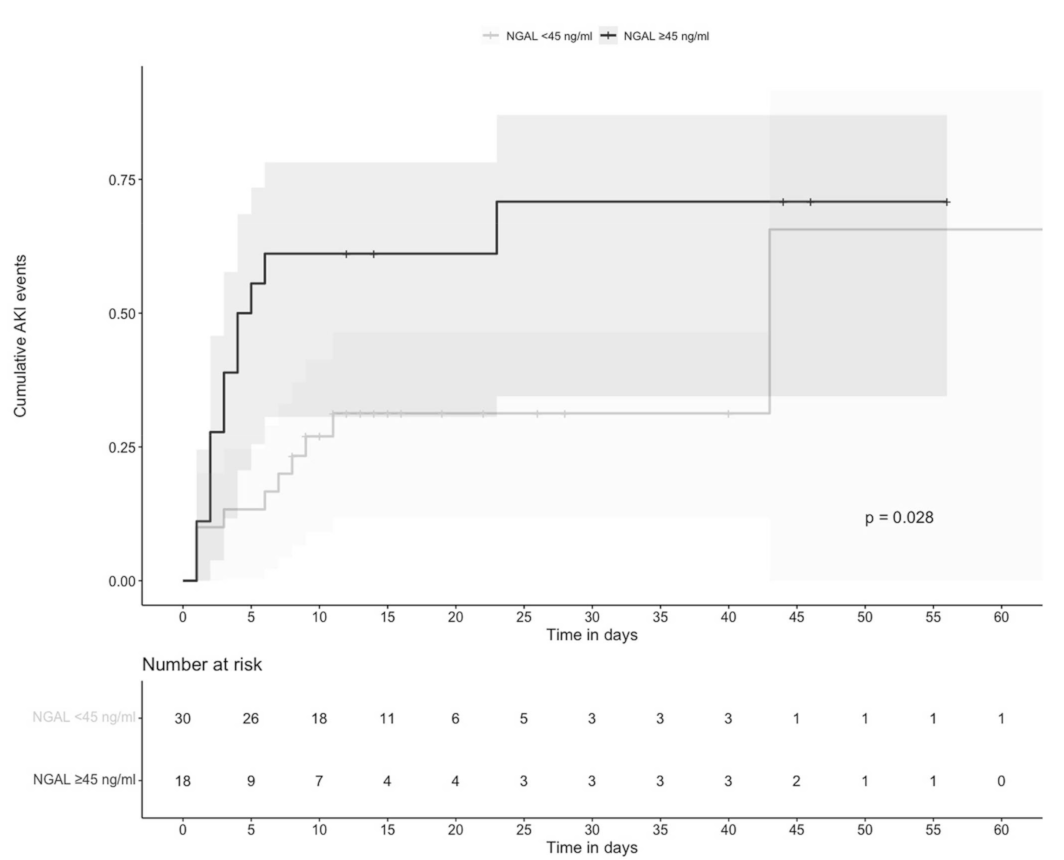
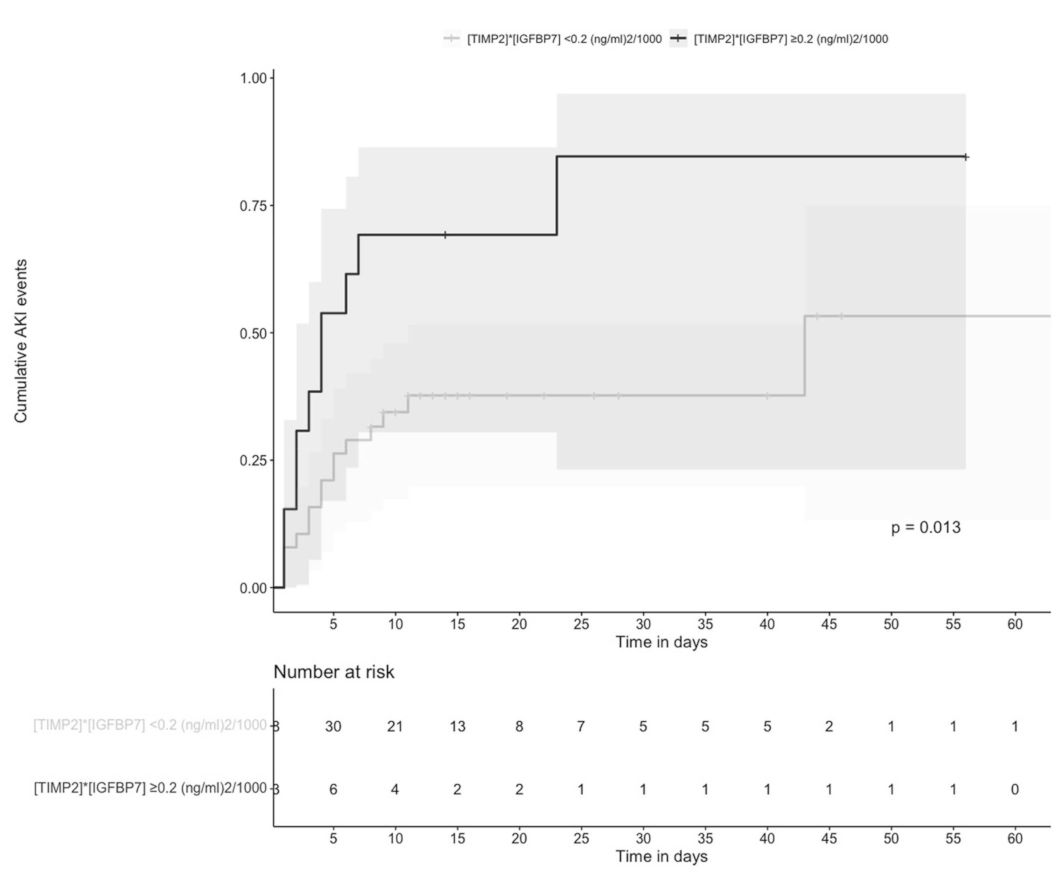
3.3. Time to AKI Was Significantly Shorter in Individuals with Higher Values of Urinary NGAL and [TIMP-2] × [IGFBP7]
3.4. Elevated Values of Urinary [TIMP-2] × [IGFBP7] were Risk Factors for AKI
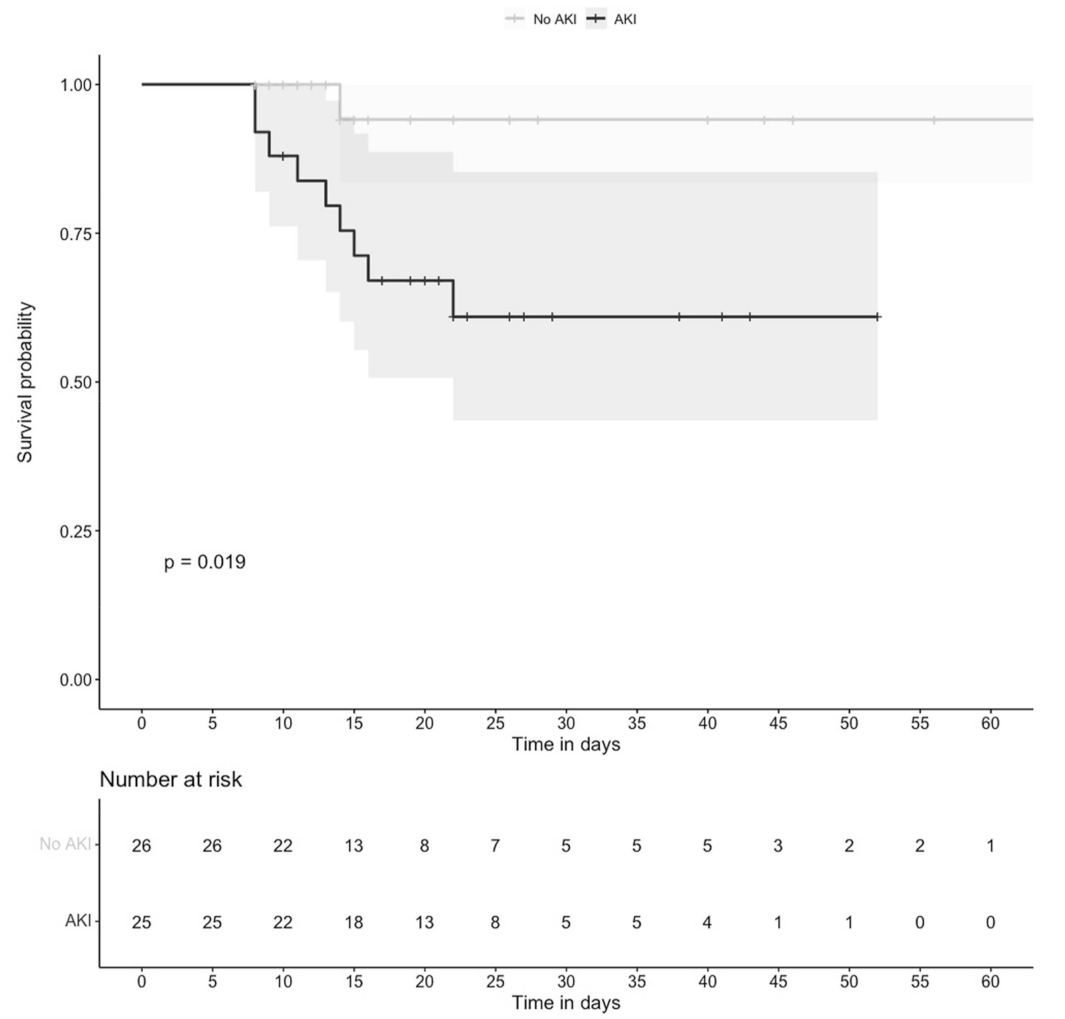
3.5. Mortality was Higher in Individuals with AKI
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- García, L.F. Immune Response, Inflammation, and the Clinical Spectrum of COVID-19. Front. Immunol. 2020, 11, 1441. [Google Scholar] [CrossRef] [PubMed]
- Nadim, M.K.; Forni, L.G.; Mehta, R.L.; Connor, M.J., Jr.; Liu, K.D.; Ostermann, M.; Rimmelé, T.; Zarbock, A.; Bell, S.; Bihorac, A.; et al. COVID-19-associated acute kidney injury: Consensus report of the 25th Acute Disease Quality Initiative (ADQI) Workgroup. Nat. Rev. Nephrol. 2020, 16, 747–764. [Google Scholar] [CrossRef] [PubMed]
- Ronco, C.; Bellomo, R.; Kellum, J.A. Acute kidney injury. Lancet 2019, 394, 1949–1964. [Google Scholar] [CrossRef]
- MacLeod, A. NCEPOD report on acute kidney injury—must do better. Lancet 2009, 374, 1405–1406. [Google Scholar] [CrossRef]
- Haase, M.; Kellum, J.A.; Ronco, C. Subclinical AKI: An emerging syndrome with important consequences. Nat Rev Nephrol. 2012, 8, 735–739. [Google Scholar] [CrossRef]
- Kashani, K.; Al-Khafaji, A.; Ardiles, T.; Artigas, A.; Bagshaw, S.M.; Bell, M.; Bihorac, A.; Birkhahn, R.; Cely, C.M.; Chawla, L.S.; et al. Discovery and validation of cell cycle arrest biomarkers in human acute kidney injury. Crit. Care. 2013, 17, R25. [Google Scholar] [CrossRef] [Green Version]
- Hoste, E.A.; McCullough, P.A.; Kashani, K.; Chawla, L.S.; Joannidis, M.; Shaw, A.D.; Feldkamp, T.; Uettwiller-Geiger, D.L.; McCarthy, P.; Shi, J.; et al. Derivation and validation of cutoffs for clinical use of cell cycle arrest biomarkers. Nephrol. Dial. Transplant. 2014, 29, 2054–2061. [Google Scholar] [CrossRef]
- Bihorac, A.; Chawla, L.S.; Shaw, A.D.; Al-Khafaji, A.; Davison, D.L.; Demuth, G.E.; Fitzgerald, R.; Gong, M.N.; Graham, D.D.; Gunnerson, K.; et al. Validation of cell-cycle arrest biomarkers for acute kidney injury using clinical adjudication. Am. J. Respir. Crit. Care. Med. 2014, 189, 932–939. [Google Scholar] [CrossRef]
- Mishra, J.; Ma, Q.; Prada, A.; Mitsnefes, M.; Zahedi, K.; Barasch, J.; Devarajan, P. Identification of neutrophil gelatinase-associated lipocalin as a novel early urinary biomarker for ischemic renal injury. J. Am. Soc. Nephrol. 2003, 14, 2534–2543. [Google Scholar] [CrossRef] [Green Version]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- World Health Organization. Clinical Management of Severe Acute Respiratory Infection When Novel Coronavirus (nCoV) Infection Is Suspected: Interim Guidance. Published 13 March 2020. Available online: https://pesquisa.bvsalud.org/portal/resource/pt/biblio-1053426 (accessed on 12 August 2021).
- Moore, P.K.; Hsu, R.K.; Liu, K.D. Management of Acute Kidney Injury: Core Curriculum 2018. Am. J. Kidney. Dis. 2018, 72, 136–148; [Google Scholar] [CrossRef] [PubMed]
- KDIGO Clinical Practice Guideline for Acute Kidney Injury. Published March 2012. Available online: https://kdigo.org/wp-content/uploads/2016/10/KDIGO-2012-AKI-Guideline-English.pdf (accessed on 12 August 2021).
- Chawla, L.S.; Bellomo, R.; Bihorac, A.; Goldstein, S.L.; Siew, E.D.; Bagshaw, S.M.; Bittleman, D.; Cruz, D.; Endre, Z.; Fitzgerald, R.L.; et al. Acute kidney disease and renal recovery: Consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup. Nat. Rev. Nephrol. 2017, 13, 241–257; [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Legrand, M.; Bell, S.; Forni, L.; Joannidis, M.; Koyner, J.L.; Liu, K.; Cantaluppi, V. Pathophysiology of COVID-19-associated acute kidney injury. Nat. Rev. Nephrol. 2021, 17, 751–764. [Google Scholar] [CrossRef]
- Husain-Syed, F.; Wilhelm, J.; Kassoumeh, S.; Birk, H.W.; Herold, S.; Vadász, I.; Walmrath, H.D.; A Kellum, J.; Ronco, C.; Seeger, W. Acute kidney injury and urinary biomarkers in hospitalized patients with coronavirus disease-2019. Nephrol. Dial. Transplant. 2020, 35, 1271–1274. [Google Scholar] [CrossRef] [PubMed]
- Fiorentino, M.; Xu, Z.; Smith, A.; Singbartl, K.; Palevsky, P.M.; Chawla, L.S.; Huang, D.T.; Yealy, D.M.; Angus, D.C.; Kellum, J.A.; et al. Serial Measurement of cell-cycle arrest biomarkers [TIMP-2]•[IGFBP7] and risk for progression to death, dialysis or severe acute kidney injury in patients with septic shock. Am. J. Respir. Crit. Care. Med. 2020, 202, 1262–1270. [Google Scholar] [CrossRef]
- Gocze, I.; Koch, M.; Renner, P.; Zeman, F.; Graf, B.M.; Dahlke, M.H.; Nerlich, M.; Schlitt, H.J.; Kellum, J.A.; Bein, T. Urinary biomarkers TIMP-2 and IGFBP7 early predict acute kidney injury after major surgery. PLoS ONE 2015, 10, e0120863. [Google Scholar] [CrossRef] [Green Version]
- Pajenda, S.; Ilhan-Mutlu, A.; Preusser, M.; Roka, S.; Druml, W.; Wagner, L. NephroCheck data compared to serum creatinine in various clinical settings. BMC Nephrol. 2015, 16, 206. [Google Scholar] [CrossRef] [Green Version]
- Emlet, D.R.; Pastor-Soler, N.; Marciszyn, A.; Wen, X.; Gomez, H.; Humphries, W.H.; Morrisroe, S.; Volpe, J.K.; Kellum, J.A. Insulin-like growth factor binding protein 7 and tissue inhibitor of metalloproteinases-2: Differential expression and secretion in human kidney tubule cells. Am. J. Physiol. Renal. Physiol. 2017, 312, F284–F296. [Google Scholar] [CrossRef] [Green Version]
- Johnson, A.C.M.; Zager, R.A. Mechanisms underlying increased TIMP-2 and IGFBP7 urinary excretion in experimental AKI. J. Am. Soc. Nephrol. 2018, 29, 2157–2167. [Google Scholar] [CrossRef]
- Kellum, J.A.; van Till, J.W.O.; Mulligan, G. Targeting acute kidney injury in COVID-19. Nephrol. Dial. Transplant. 2020, 35, 1652–1662. [Google Scholar] [CrossRef] [PubMed]
- Borregaard, N.; Cowland, J.B. Granules of the human neutrophilic polymorphonuclear leukocyte. Blood 1997, 89, 3503–3521. [Google Scholar] [CrossRef] [PubMed]
- Xu, K.; Shang, N.; Levitman, A.; Corker, A.; Kudose, S.; Yaeh, A.; Neupane, A.; Stevens, J.; Mohan, S.; Sampogna, R.; et al. Urine test predicts kidney injury and death in COVID-19. medRxiv 2021. [Google Scholar] [CrossRef]
- He, L.; Zhang, Q.; Li, Z.; Shen, L.; Zhang, J.; Wang, P.; Wu, S.; Zhou, T.; Xu, Q.; Chen, X.; et al. Incorporation of Urinary Neutrophil Gelatinase-Associated Lipocalin and Computed Tomography Quantification to Predict Acute Kidney Injury and In-Hospital Death in COVID-19 Patients. Kidney. Dis. 2021, 7, 120–130; [Google Scholar] [CrossRef] [PubMed]
- Xu, K.; Shang, N.; Levitman, A.; Corker, A.; Kudose, S.; Yaeh, A.; Neupane, U.; Stevens, J.; Sampogna, R.; Mills, A.M.; et al. Elevated neutrophil gelatinase-associated lipocalin is associated with the severity of kidney injury and poor prognosis of patients with COVID-19. Kidney. Int. Rep. 2021, 12, 2979–2992; [Google Scholar] [CrossRef]
- Jo, S.K.; Yang, J.; Hwang, S.M.; Lee, M.S.; Park, S.H. Role of biomarkers as predictors of acute kidney injury and mortality in decompensated cirrhosis. Sci. Rep. 2019, 9, 14508. [Google Scholar] [CrossRef]
- Coca, S.G.; King, J.T., Jr.; Rosenthal, R.A.; Perkal, M.F.; Parikh, C.R. The duration of postoperative acute kidney injury is an additional parameter predicting long-term survival in diabetic veterans. Kidney Int. 2010, 78, 926–933. [Google Scholar] [CrossRef] [Green Version]
- Vanmassenhove, J.; Glorieux, G.; Hoste, E.; Dhondt, A.; Vanholder, R.; Van Biesen, W. AKI in early sepsis is a continuum from transient AKI without tubular damage over transient AKI with minor tubular damage to intrinsic AKI with severe tubular damage. Int. Urol. Nephrol. 2014, 4610, 2003–2008. [Google Scholar] [CrossRef]
- Gameiro, J.; Duarte, I.; Marques, F.; Fonseca, J.A.; Jorge, S.; Rosa, R.; Lopes, J.A. Transient and Persistent AKI and Outcomes in Patients Undergoing Major Abdominal Surgery. Nephron. 2020, 144, 236–244. [Google Scholar] [CrossRef]
- de Geus, H.R.H.; Meersch, M.; Zarbock, A. Discussion on “Prevention of cardiac surgery-associated AKI by implementing the KDIGO guidelines in high-risk patients identified by biomarkers: The PrevAKI randomized controlled trial”. Intensive. Care. Med. 2018, 44, 273–274. [Google Scholar] [CrossRef]
- De Rosa, S.; Samoni, S.; Ronco, C. Creatinine-based definitions: From baseline creatinine to serum creatinine adjustment in intensive care. Crit. Care 2016, 20, 69. [Google Scholar] [CrossRef] [Green Version]

| Variable | Overall (n = 51) | AKI (n = 25) | Non-AKI (n = 26) | p Value |
|---|---|---|---|---|
| Age, years * | 53 (40–61) | 57 (47–65) | 49 (37–56) | 0.029 |
| Male [n (%)] | 30 (58.8) | 18 (72) | 12 (46.1) | 0.061 |
| BMI, kg/m2 * | 29.3 (25.9–31.6) | 29.4 (26.7–34.1) | 29.1 (25.9–30.3) | 0.522 |
| Comorbidities | ||||
| Obesity [n (%)] | 21 (41.2) | 11 (44.0) | 10 (38.5) | 0.688 |
| Diabetes [n (%)] | 16 (31.4) | 7 (28.0) | 9 (34.6) | 0.611 |
| Hypertension [n (%)] | 14 (27.5) | 11 (44.0) | 3 (11.5) | 0.009 |
| Two or more comorbidities [n (%)] | 21 (41.2) | 12 (48.0) | 9 (34.6) | 0.332 |
| Critical Care Variables | ||||
| IMV [n (%)] | 32 (62.7) | 18 (72.0) | 14 (53.8) | 0.180 |
| PaO₂/FiO₂ ratio, mmHg * | 141 (108–187) | 140 (120–174.5) | 148 (103–198.5) | 0.733 |
| PEEP, cm H₂O * | 10 (9.5–14) | 10 (8–12) | 12 (10–14) | 0.125 |
| pH * | 7.4 (7.3–7.4) | 7.3 (7.3–7.4) | 7.4 (7.3–7.4) | 0.556 |
| pCO₂, mmHg * | 38.0 (32.3–51.9) | 46.3 (33.0–52.2) | 35.9 (33–50.9) | 0.378 |
| SOFA score, points * | 4 (2–6) | 4 (3–6) | 3 (2–6) | 0.076 |
| Vasoactive drugs [n (%)] | 16 (31.4) | 8 (32.0) | 8 (30.8) | 0.925 |
| Inotropic drug [n (%)] | 2 (3.9) | 0 (0.0) | 2 (7.7) | 0.157 |
| Treatment | ||||
| Systemic steroids [n (%)] | 25 (49) | 14 (56.0) | 11 (42.3) | 0.328 |
| Tocilizumab [n (%)] | 25 (49) | 11 (44.0) | 14 (53.8) | 0.355 |
| Hydroxychloroquine [n (%)] | 7 (13.7) | 4 (16.0) | 3 (11.5) | 0.643 |
| Lopinavir/Ritonavir [n (%)] | 12 (23.5) | 2 (8.0) | 10 (38.5) | 0.010 |
| Nephrotoxic drugs [n (%)] | 1 (2) | 0 (0.0) | 1 (3.8) | 0.322 |
| Renal Function Indicators | ||||
| Serum creatinine, mg/dL, Day 1 * | 0.6 (0.5–0.7) | 0.6 (0.5–0.8) | 0.6 (0.4–0.7) | 0.039 |
| eGFR, mL/min, Day 1* | 112.3 (98.4–121.4) | 107.0 (92.5–114.9) | 113.3 (108.7–125.1) | 0.026 |
| Laboratories | ||||
| Hemoglobin, g/dL, Day 1 * | 13.3 (12.6–14.9) | 13.1 (12.5–15.0) | 13.4 (12.8–14.4) | 0.850 |
| Leucocytes, 10×3 mm3, Day 1 * | 8.9 (6.3–13.4) | 9.4 (7.8–13.4) | 8.3 (5.8–11.6) | 0.239 |
| Lymphocytes, 10×3 mm3, Day 1 * | 0.8 (0.6–1.0) | 0.7 (0.5–1.0) | 0.85 (0.6–1.1) | 0.219 |
| Platelets, 10x3 mm3, Day 1 * | 272 (219–329) | 283 (228–363) | 259 (219–308) | 0.323 |
| Blood urea nitrogen, mg/dL, Day 1 * | 22 (13–35) | 32 (27–45) | 13.5 (11–21) | 0.001 |
| Lactate dehydrogenase, U/mL, Day 1 * | 387 (299–557) | 421 (327–557) | 364.5 (249–541) | 0.118 |
| Total bilirrubines, mg/dL, Day 1 * | 0.5 (0.4–0.6) | 0.5 (0.4–0.6) | 0.4 (0.4–0.8) | 0.651 |
| Creatine phosphokinase, U/L, Day 1 * | 140 (39–443) | 175 (97–992) | 58 (31–354) | 0.004 |
| D-dimer, µg/mL, Day 1 * | 0.9 (0.4–2.5) | 1.1 (0.5–3.7) | 0.7 (0.4–1.2) | 0.057 |
| C-reactive protein, mg/dL, Day 1 * | 16.5 (10.3–27.6) | 25.2 (13.6–31.9) | 13.2 (10.1–17.7) | 0.030 |
| Fibrinogen, mg/dL, Day 1 * | 733.5 (580.2–821.2) | 750 (613.5–805) | 685 (587–786) | 0.424 |
| Procalcitonin, ng/mL, Day 1 * | 0.4 (0.1–0.9) | 0.6 (0.2–1.1) | 0.1 (0.9–0.5) | 0.043 |
| Troponin, pg/mL, Day 1 * | 5.6 (3.3–37) | 12.4 (3.8–40.6) | 4.2 (2.1–9.0) | 0.039 |
| Ferritin, ng/mL, Day 1 * | 745.4 (358.3–1883.4) | 831.3 (468.2–2512) | 636.4 (337.1–1008.7) | 0.257 |
| Urinary Biomarkers | ||||
| NGAL, ng/mL, Day 1 * | 39.3 (19.2–98.5) | 50.2 (36.4–112.1) | 32.9 (13.9–44.7) | 0.015 |
| TIMP-2, ng/mL, Day 1 * | 5.5 (3.0–9.0) | 6.3 (4.2–9.1) | 5.1 (2.9–7.6) | 0.356 |
| IGFBP7, ng/mL/1000, Day 1 * | 13.4 (8.2–24.1) | 22.1 (9.9–29.0) | 11.6 (7.0–17.7) | 0.040 |
| [TIMP-2] × [IGFBP7], (ng/mL)2/1000, Day 1* | 0.08 (0.04–0.24) | 0.11 (0.05–0.27) | 0.06 (0.02–0.12) | 0.026 |
| Outcomes | ||||
| Days in hospital | 16 (12–27) | 20 (14–27) | 14.5 (12–26) | 0.304 |
| Days on IMV | 13 (10–22.2) | 15 (12.5–22) | 11 (8.5–21.5) | 0.235 |
| Days with symptoms before IMV | 10 (6–14) | 9 (5.5–12) | 11.5 (8–14) | 0.178 |
| Mortality [n (%)] | 10 (19.6) | 9 (36.0) | 1 (3.8) | 0.004 |
| Biomarker | AUC | 95% CI | p | Cutoff | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) |
|---|---|---|---|---|---|---|---|---|---|
| Prediction of AKI during the Whole Period of Hospitalization | |||||||||
| N-Gal (ng/mL) | 0.706 | 0.559–0.854 | 0.015 | 40.0 | 59.1 | 61.5 | 50.6 | 69.3 | 60.5 |
| 45.0 | 54.5 | 76.9 | 61.1 | 71.7 | 67.9 | ||||
| 50.0 | 50 | 76.9 | 59.1 | 69.7 | 66.1 | ||||
| [TIMP-2] × [IGFBP7] ((ng/mL)2/1000) | 0.682 | 0.535–0.829 | 0.026 | 0.1 | 56.0 | 69.2 | 54.8 | 70.2 | 63.9 |
| 0.2 | 40.0 | 88.4 | 69.8 | 68.8 | 69.1 | ||||
| 0.3 | 24.0 | 92.3 | 67.5 | 64.5 | 64.9 | ||||
| Prediction of AKI on Day 7 of Hospitalization | |||||||||
| N-Gal (ng/mL) | 0.771 | 0.632–0.910 | 0.002 | 40.0 | 70.5 | 64.5 | 57.0 | 76.6 | 66.9 |
| 45.0 | 64.7 | 77.4 | 65.6 | 76.6 | 72.3 | ||||
| 50.0 | 64.7 | 80.6 | 69.0 | 77.4 | 74.2 | ||||
| [TIMP-2] × [IGFBP7] ((ng/mL)2/1000) | 0.671 | 0.515–0.827 | 0.041 | 0.1 | 60.0 | 67.7 | 55.3 | 71.7 | 64.6 |
| 0.2 | 45.0 | 87.1 | 69.9 | 70.3 | 70.2 | ||||
| 0.3 | 25.0 | 90.3 | 63.2 | 64.3 | 64.1 | ||||
| Variables | Unadjusted HR (95% CI) | p Value | Adjusted HR (95% CI) | p Value |
|---|---|---|---|---|
| Age | 0.94 (0.90–0.99) | 0.034 | 0.95 (0.89–1.01) | 0.144 |
| Male | 3.0 (0.93–9.61) | 0.065 | 7.57 (1.28–44.8) | 0.026 |
| Hypertension | 6.02 (1.42–25.40) | 0.014 | 5.61 (0.84–37.22) | 0.074 |
| TIMP-2 × IGFBP7 > 2.0 (ng/mL)2/1000 | 5.11 (1.20–21.67) | 0.027 | 7.23 (0.99–52.4) | 0.050 |
| NGAL > 45 | 4.00 (1.15–13.81) | 0.028 | 1.45 (0.30–6.94) | 0.637 |
| CPK | 1.00 (0.99–1.00) | 0.192 | - | - |
| Procalcitonine > 0.25 | 2.47 (0.79–7.75) | 0.119 | 0.90 (.204.0) | 0.894 |
| Troponine | 0.99 (0.98–1.00) | 0.274 | - | - |
| Variables | Unadjusted HR (95% CI) | p Value | Adjusted HR (95% CI) | p Value |
|---|---|---|---|---|
| Age 60, years | 5.33 (1.23–23.09) | 0.025 | 3.88 (0.78–19.24) | 0.097 |
| Male | 3.45 (0.65–18.29) | 0.145 | 2.65 (0.43–16.39) | 0.293 |
| Transient AKI | 4.33 (0.62–30.24) | 0.139 | 2.47 (0.37–16.38) | 0.347 |
| Persistent AKI | 10.83 (1.67–69.91) | 0.012 | 7.42 (1.04–53.04) | 0.046 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Casas-Aparicio, G.; Alvarado-de la Barrera, C.; Escamilla-Illescas, D.; León-Rodríguez, I.; Del Río-Estrada, P.M.; Calderón-Dávila, N.; González-Navarro, M.; Olmedo-Ocampo, R.; Castillejos-López, M.; Figueroa-Hernández, L.; et al. Role of Urinary Kidney Stress Biomarkers for Early Recognition of Subclinical Acute Kidney Injury in Critically Ill COVID-19 Patients. Biomolecules 2022, 12, 275. https://doi.org/10.3390/biom12020275
Casas-Aparicio G, Alvarado-de la Barrera C, Escamilla-Illescas D, León-Rodríguez I, Del Río-Estrada PM, Calderón-Dávila N, González-Navarro M, Olmedo-Ocampo R, Castillejos-López M, Figueroa-Hernández L, et al. Role of Urinary Kidney Stress Biomarkers for Early Recognition of Subclinical Acute Kidney Injury in Critically Ill COVID-19 Patients. Biomolecules. 2022; 12(2):275. https://doi.org/10.3390/biom12020275
Chicago/Turabian StyleCasas-Aparicio, Gustavo, Claudia Alvarado-de la Barrera, David Escamilla-Illescas, Isabel León-Rodríguez, Perla Mariana Del Río-Estrada, Natalia Calderón-Dávila, Mauricio González-Navarro, Rossana Olmedo-Ocampo, Manuel Castillejos-López, Liliana Figueroa-Hernández, and et al. 2022. "Role of Urinary Kidney Stress Biomarkers for Early Recognition of Subclinical Acute Kidney Injury in Critically Ill COVID-19 Patients" Biomolecules 12, no. 2: 275. https://doi.org/10.3390/biom12020275
APA StyleCasas-Aparicio, G., Alvarado-de la Barrera, C., Escamilla-Illescas, D., León-Rodríguez, I., Del Río-Estrada, P. M., Calderón-Dávila, N., González-Navarro, M., Olmedo-Ocampo, R., Castillejos-López, M., Figueroa-Hernández, L., Peralta-Prado, A., Luna-Villalobos, Y., Piten-Isidro, E., Fernández-Campos, P., & Ávila-Ríos, S. (2022). Role of Urinary Kidney Stress Biomarkers for Early Recognition of Subclinical Acute Kidney Injury in Critically Ill COVID-19 Patients. Biomolecules, 12(2), 275. https://doi.org/10.3390/biom12020275







