Repurposable Drugs That Interact with Steroid Responsive Gene Targets for Inner Ear Disease
Abstract
1. Introduction
2. Materials and Methods
2.1. Identification of Steroid-Responsive Genes in the Mammalian Spiral Ganglion Neurons and Stria Vascularis Cell Types
2.2. Identification of Druggable Gene Targets Amongst Spiral Ganglion Neurons and Stria Vascularis Cell Types
3. Results
3.1. Overview
3.2. FDA-Approved Drugs with Repurposing Potential for Sudden Sensorineural Hearing Loss Organized by Class
3.2.1. Antidepressants
| Gene | Drug | Drug Class | MOA | SGN: SS > Control | SGN: TTS > Control | SV: SS > Control | SV: TTS > Control |
|---|---|---|---|---|---|---|---|
| Kcnh2 | Amitriptyline | TCA | Inhibitor | Y | Y | Y | Y |
| Kcnh2 | Doxepin | TCA | Inhibitor | Y | Y | Y | Y |
| Kcnh2 | Fluoxetine | SSRI | Inhibitor | Y | Y | Y | Y |
| Kcnh2 | Fluvoxamine | SSRI | Unknown | Y | Y | Y | Y |
| Kcnh2 | Imipramine | TCA | Inhibitor | Y | Y | Y | Y |
| Grin1 | Milnacipran | SSNRI | Inhibitor | NC | Y | NC | Y |
| Kcnh2 | Nefazodone | SARI | Inhibitor | Y | Y | Y | Y |
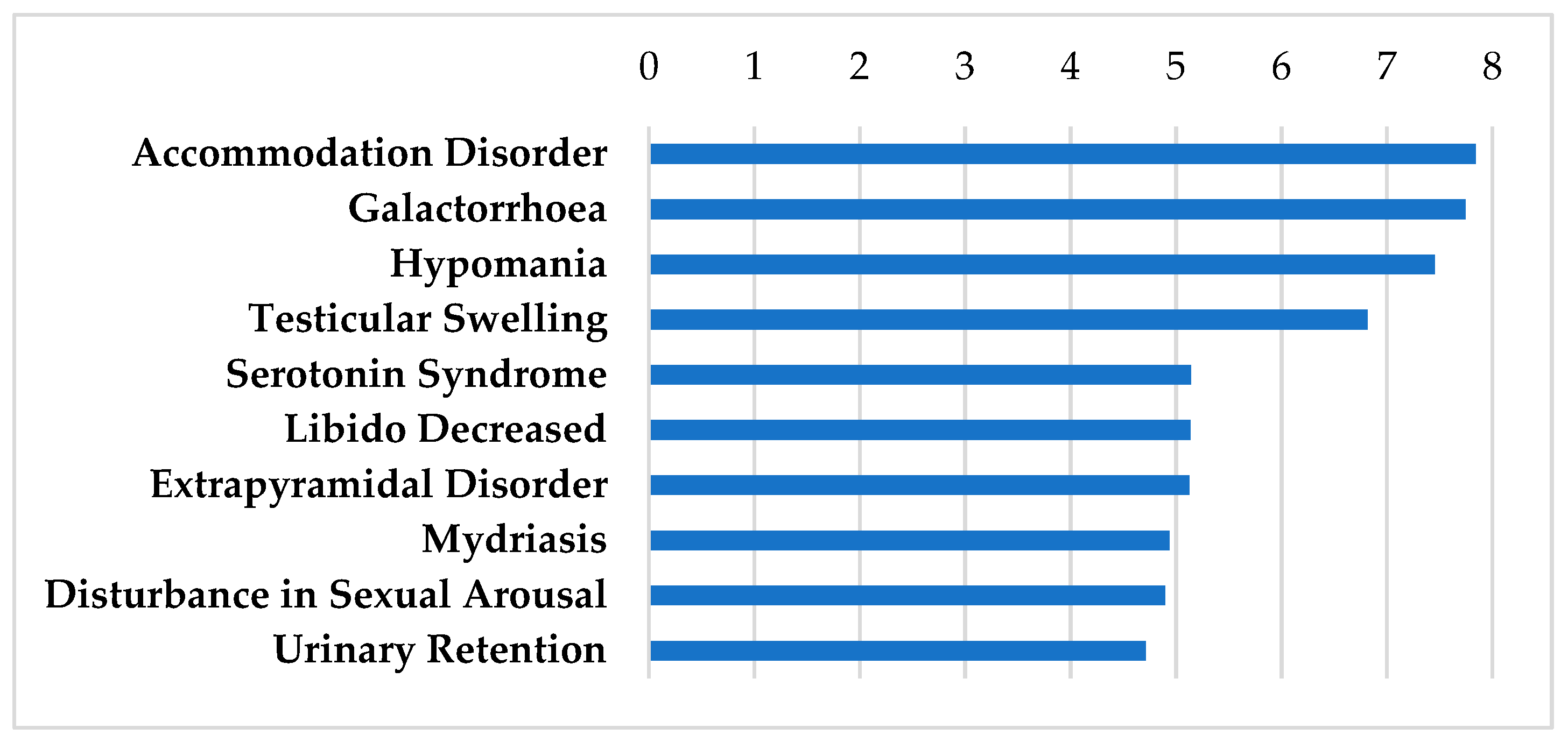
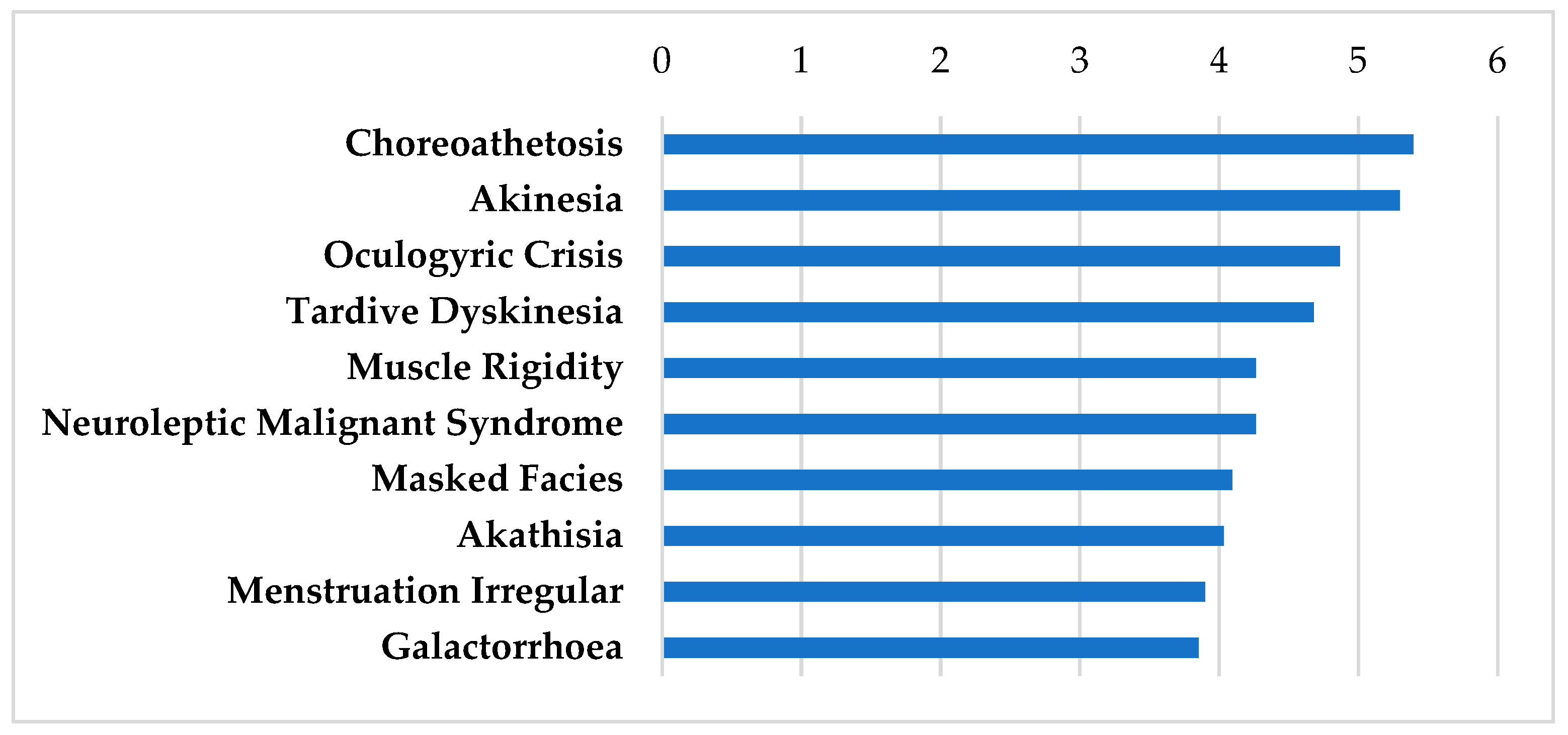
3.2.2. Antipsychotics
| Gene | Drug | MOA | SGN: SS > Control | SGN: TTS > Control | SV: SS > Control | SV: TTS > Control |
|---|---|---|---|---|---|---|
| Grin1 | Aripiprazole | Ligand | NC | Y | NC | Y |
| Kcnh2 | Thioridazine | Inhibitor | Y | Y | Y | Y |
| Kcnt1 | Loxapine | Activator | NC | Y | NC | Y |
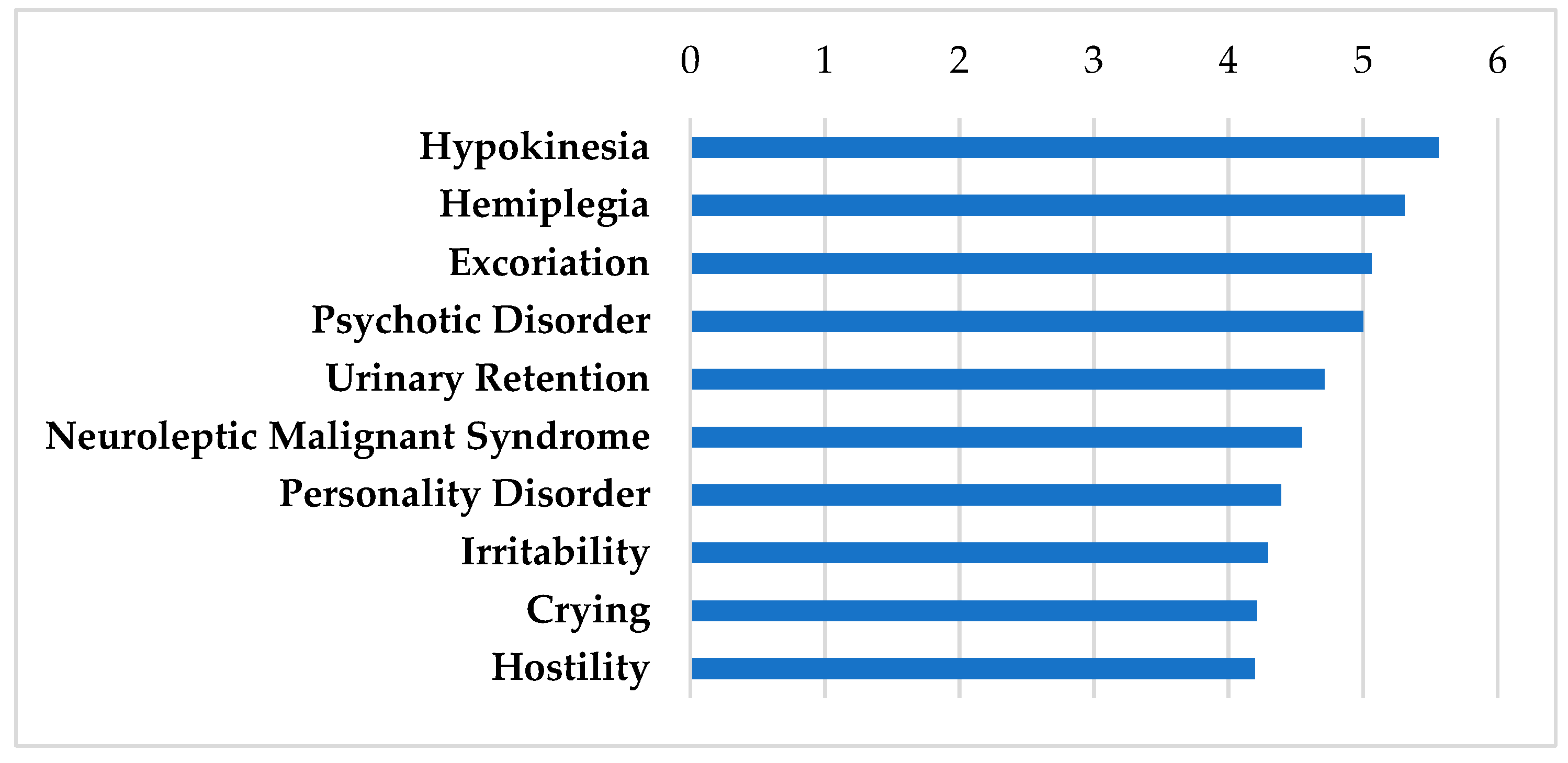
3.2.3. Central Nervous System: Other
| Gene | Drug | MOA | SGN: SS > Control | SGN: TTS > Control | SV: SS > Control | SV: TTS > Control |
|---|---|---|---|---|---|---|
| Grin1 | Donepezil | Inhibitor | NC | Y | NC | Y |
| Cacna1a | Gabapentin | Inhibitor | NC | Y | NC | Y |
| Grin1 | Gabapentin | Inhibitor | NC | Y | NC | Y |
| Grin1 | Memantine | Inhibitor | NC | Y | NC | Y |
| Kcnh2 | Phenytoin | Inhibitor | Y | Y | Y | Y |
| Grin1 | Amantadine | Inhibitor | NC | Y | NC | Y |
| Grin1 | Atomoxetine | Inhibitor | NC | Y | NC | Y |
3.2.4. Over the Counter
| Gene | Drug | MOA | SGN: SS > Control | SGN: TTS > Control | SV: SS > Control | SV: TTS > Control |
|---|---|---|---|---|---|---|
| Grin1 | Acetylcysteine | Activator | NC | Y | NC | Y |
| Nfkbia | Aspirin | Inhibitor | NC | Y | NC | Y |
| Kcnq2 | Diclofenac | Inhibitor | NC | Y | NC | Y |
| Grin1 | Guaifenesin | Inhibitor | NC | Y | NC | Y |
| Grin1 | Magnesium carbonate | Inhibitor | NC | Y | NC | Y |
| Tufm | Zinc | Unknown | Y | Y | Y | Y |
| Tufm | Zinc acetate | Unknown | Y | NC | Y | Y |
| Kcnh2 | Pentoxyverine | Inhibitor | Y | Y | Y | Y |
| Pdxk | Pyridoxine | Ligand | NC | Y | NC | NC |
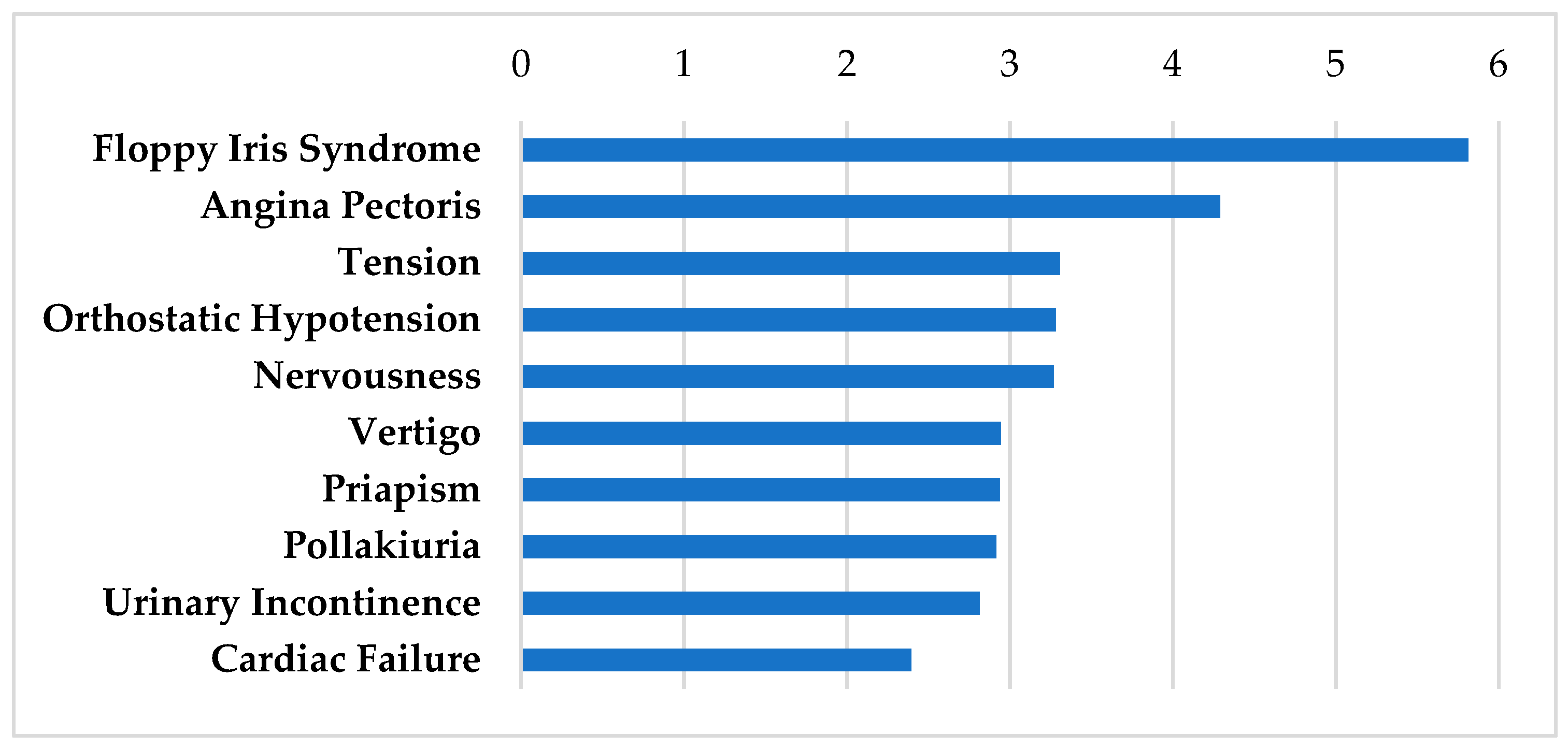
3.2.5. Adrenergic Modulators
| Gene | Drug | MOA | SGN: SS > Control | SGN: TTS > Control | SV: SS > Control | SV: TTS > Control |
|---|---|---|---|---|---|---|
| Kcnh2 | Carvedilol | Inhibitor | Y | Y | Y | Y |
| Kcnh2 | Doxazosin | Inhibitor | Y | Y | Y | Y |
| Kcnh2 | Prazosin | Inhibitor | Y | Y | Y | Y |
| Kcnh2 | Terazosin | Inhibitor | Y | Y | Y | Y |
| Atf3 | Ephedrine-(racemic) | Activator | NC | Y | NC | Y |
| Nisch | Tizanidine | Activator | NC | Y | NC | Y |
3.2.6. Calcium Channel Blockers
| Gene | Drug | MOA | SGN: SS > Control | SGN: TTS > Control | SV: SS > Control | SV: TTS > Control |
|---|---|---|---|---|---|---|
| Kcna5 | Nifedipine | Inhibitor | NC | Y | NC | Y |
| Cacna1a | Verapamil | Inhibitor | NC | Y | Y | Y |
| Kcnh2 | Verapamil | Inhibitor | Y | Y | Y | Y |
3.2.7. Ion Modulators
| Gene | Drug | MOA | SGN: SS > Control | SGN: TTS > Control | SV: SS > Control | SV: TTS > Control |
|---|---|---|---|---|---|---|
| Nrxn1 | Calcium citrate | Activator | NC | Y | NC | Y |
| Nrxn1 | Calcium phosphate | Activator | NC | Y | NC | NC |
| Cacna1a | Spironolactone | Inhibitor | NC | Y | NC | Y |
3.2.8. Antimicrobials
| Gene | Drug | MOA | SGN: SS > Control | SGN: TTS > Control | SV: SS > Control | SV: TTS > Control |
|---|---|---|---|---|---|---|
| Kcna5 | Isavuconazole | Inhibitor | NC | Y | NC | Y |
| Kcnh2 | Isavuconazole | Inhibitor | Y | Y | Y | Y |
| Kcnh2 | Erythromycin | Inhibitor | Y | Y | Y | Y |
3.2.9. Antihistamines
| Gene | Drug | MOA | SGN: SS > Control | SGN: TTS > Control | SV: SS > Control | SV: TTS > Control |
|---|---|---|---|---|---|---|
| Kcnh2 | Loratadine | Inhibitor | Y | Y | Y | Y |
| Kcnh2 | Hydroxyzine | Inhibitor | Y | Y | Y | Y |
| Grin1 | Orphenadrine | Inhibitor | NC | Y | Y | Y |
3.2.10. Fostamatinib
| Gene | Drug | MOA | SGN: SS > Control | SGN: TTS > Control | SV: SS > Control | SV: TTS > Control |
|---|---|---|---|---|---|---|
| Mast1 | Fostamatinib | Inhibitor | NC | Y | NC | Y |
| Sbk1 | Fostamatinib | Inhibitor | NC | Y | NC | Y |
4. Discussion
4.1. Overview
4.2. Repurposing Studies as an Approach Forward
4.3. Existing Knowledge of Identified Drugs in Hearing Disorders
4.4. Limitations
4.5. Implications and Future Directions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chandrasekhar, S.S.; Tsai Do, B.S.; Schwartz, S.R.; Bontempo, L.J.; Faucett, E.A.; Finestone, S.A.; Hollingsworth, D.B.; Kelley, D.M.; Kmucha, S.T.; Moonis, G.; et al. Clinical Practice Guideline: Sudden Hearing Loss (Update). Otolaryngol. Head Neck Surg. 2019, 161, S1–S45. [Google Scholar] [CrossRef]
- Basura, G.J.; Adams, M.E.; Monfared, A.; Schwartz, S.R.; Antonelli, P.J.; Burkard, R.; Bush, M.L.; Bykowski, J.; Colandrea, M.; Derebery, J.; et al. Clinical Practice Guideline: Meniere’s Disease. Otolaryngol. Head Neck Surg. 2020, 162, S1–S55. [Google Scholar] [CrossRef]
- Vambutas, A.; Pathak, S. AAO: Autoimmune and Autoinflammatory (Disease) in Otology: What is New in Immune-Mediated Hearing Loss. Laryngoscope Investig. Otolaryngol. 2016, 1, 110–115. [Google Scholar] [CrossRef]
- Breslin, N.K.; Varadarajan, V.V.; Sobel, E.S.; Haberman, R.S. Autoimmune inner ear disease: A systematic review of management. Laryngoscope Investig. Otolaryngol. 2020, 5, 1217–1226. [Google Scholar] [CrossRef]
- Brant, J.A.; Eliades, S.J.; Ruckenstein, M.J. Systematic Review of Treatments for Autoimmune Inner Ear Disease. Otol. Neurotol. 2015, 36, 1585–1592. [Google Scholar] [CrossRef]
- Vambutas, A.; Lesser, M.; Mullooly, V.; Pathak, S.; Zahtz, G.; Rosen, L.; Goldofsky, E. Early efficacy trial of anakinra in corticosteroid-resistant autoimmune inner ear disease. J. Clin. Invest. 2014, 124, 4115–4122. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.P.; Weisman, M.H.; Derebery, J.M.; Espeland, M.A.; Gantz, B.J.; Gulya, A.J.; Hammerschlag, P.E.; Hannley, M.; Hughes, G.B.; Moscicki, R.; et al. Treatment of corticosteroid-responsive autoimmune inner ear disease with methotrexate: A randomized controlled trial. JAMA 2003, 290, 1875–1883. [Google Scholar] [CrossRef] [PubMed]
- Broughton, S.S.; Meyerhoff, W.E.; Cohen, S.B. Immune-mediated inner ear disease: 10-year experience. Semin. Arthritis Rheum. 2004, 34, 544–548. [Google Scholar] [CrossRef] [PubMed]
- Alexander, T.H.; Harris, J.P. Incidence of sudden sensorineural hearing loss. Otol. Neurotol. 2013, 34, 1586–1589. [Google Scholar] [CrossRef] [PubMed]
- Byl, F.M., Jr. Sudden hearing loss: Eight years’ experience and suggested prognostic table. Laryngoscope 1984, 94, 647–661. [Google Scholar] [CrossRef] [PubMed]
- Klemm, E.; Deutscher, A.; Mosges, R. [A present investigation of the epidemiology in idiopathic sudden sensorineural hearing loss]. Laryngorhinootologie 2009, 88, 524–527. [Google Scholar] [CrossRef]
- Ciorba, A.; Corazzi, V.; Bianchini, C.; Aimoni, C.; Pelucchi, S.; Skarzynski, P.H.; Hatzopoulos, S. Autoimmune inner ear disease (AIED): A diagnostic challenge. Int. J. Immunopathol. Pharmacol. 2018, 32, 2058738418808680. [Google Scholar] [CrossRef]
- Carlsson, P.I.; Hall, M.; Lind, K.J.; Danermark, B. Quality of life, psychosocial consequences, and audiological rehabilitation after sudden sensorineural hearing loss. Int. J. Audiol. 2011, 50, 139–144. [Google Scholar] [CrossRef]
- Shaia, F.T.; Sheehy, J.L. Sudden sensori-neural hearing impairment: A report of 1,220 cases. Laryngoscope 1976, 86, 389–398. [Google Scholar] [CrossRef]
- Wie, O.B.; Pripp, A.H.; Tvete, O. Unilateral deafness in adults: Effects on communication and social interaction. Ann. Otol. Rhinol. Laryngol. 2010, 119, 772–781. [Google Scholar]
- Chiossoine-Kerdel, J.A.; Baguley, D.M.; Stoddart, R.L.; Moffat, D.A. An investigation of the audiologic handicap associated with unilateral sudden sensorineural hearing loss. Am. J. Otol. 2000, 21, 645–651. [Google Scholar]
- Chen, J.; Liang, J.; Ou, J.; Cai, W. Mental health in adults with sudden sensorineural hearing loss: An assessment of depressive symptoms and its correlates. J. Psychosom. Res. 2013, 75, 72–74. [Google Scholar] [CrossRef]
- Jung, D.; Bhattacharyya, N. Association of hearing loss with decreased employment and income among adults in the United States. Ann. Otol. Rhinol. Laryngol. 2012, 121, 771–775. [Google Scholar] [CrossRef]
- Shan, A.; Ting, J.S.; Price, C.; Goman, A.M.; Willink, A.; Reed, N.S.; Nieman, C.L. Hearing loss and employment: A systematic review of the association between hearing loss and employment among adults. J. Laryngol. Otol. 2020, 134, 387–397. [Google Scholar] [CrossRef]
- Chao, P.Z.; Huang, S.W.; Escorpizo, R.; Chi, W.C.; Yen, C.F.; Liao, H.F.; Chen, Y.W.; Liou, T.H. Effects of Hearing Disability on the Employment Status Using WHODAS 2.0 in Taiwan. Int. J. Environ. Res. Public Health 2020, 17, 9374. [Google Scholar] [CrossRef]
- Tran, P.; Tran, L. National, Regional, and State Employment Rates of U.S. Adults Who Are Deaf or Hard of Hearing. Am. Ann. Deaf. 2021, 166, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Deal, J.A.; Reed, N.S.; Kravetz, A.D.; Weinreich, H.; Yeh, C.; Lin, F.R.; Altan, A. Incident Hearing Loss and Comorbidity: A Longitudinal Administrative Claims Study. JAMA Otolaryngol. Head Neck Surg. 2019, 145, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Lacey Nelson, B.L.; Dixon Johns, J.; Choi, D.; Trune, D.; Hoa, M. In silico Single-Cell Analysis of Steroid-Responsive Gene Targets in the Mammalian Cochlea. Front. Neurol. 2022. [Google Scholar]
- Trune, D.R.; Shives, K.D.; Hausman, F.; Kempton, J.B.; MacArthur, C.J.; Choi, D. Intratympanically Delivered Steroids Impact Thousands More Inner Ear Genes Than Systemic Delivery. Ann. Otol. Rhinol. Laryngol. 2019, 128, 134S–138S. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, B.R.; Chia, C.; Wu, L.; Kujawa, S.G.; Liberman, M.C.; Goodrich, L.V. Sensory Neuron Diversity in the Inner Ear Is Shaped by Activity. Cell 2018, 174, 1229–1246.e1217. [Google Scholar] [CrossRef]
- Korrapati, S.; Taukulis, I.; Olszewski, R.; Pyle, M.; Gu, S.; Singh, R.; Griffiths, C.; Martin, D.; Boger, E.; Morell, R.J.; et al. Single Cell and Single Nucleus RNA-Seq Reveal Cellular Heterogeneity and Homeostatic Regulatory Networks in Adult Mouse Stria Vascularis. Front. Mol. Neurosci. 2019, 12, 316. [Google Scholar] [CrossRef]
- Gu, S.; Olszewski, R.; Taukulis, I.; Wei, Z.; Martin, D.; Morell, R.J.; Hoa, M. Characterization of rare spindle and root cell transcriptional profiles in the stria vascularis of the adult mouse cochlea. Sci. Rep. 2020, 10, 18100. [Google Scholar] [CrossRef]
- Wishart, D.S.; Feunang, Y.D.; Guo, A.C.; Lo, E.J.; Marcu, A.; Grant, J.R.; Sajed, T.; Johnson, D.; Li, C.; Sayeeda, Z.; et al. DrugBank 5.0: A major update to the DrugBank database for 2018. Nucleic Acids Res. 2018, 46, D1074–D1082. [Google Scholar] [CrossRef]
- Nguyen, D.T.; Mathias, S.; Bologa, C.; Brunak, S.; Fernandez, N.; Gaulton, A.; Hersey, A.; Holmes, J.; Jensen, L.J.; Karlsson, A.; et al. Pharos: Collating protein information to shed light on the druggable genome. Nucleic Acids Res. 2017, 45, D995–D1002. [Google Scholar] [CrossRef]
- Stathias, V.; Turner, J.; Koleti, A.; Vidovic, D.; Cooper, D.; Fazel-Najafabadi, M.; Pilarczyk, M.; Terryn, R.; Chung, C.; Umeano, A.; et al. LINCS Data Portal 2.0: Next generation access point for perturbation-response signatures. Nucleic Acids Res. 2020, 48, D431–D439. [Google Scholar] [CrossRef]
- Sheils, T.K.; Mathias, S.L.; Kelleher, K.J.; Siramshetty, V.B.; Nguyen, D.T.; Bologa, C.G.; Jensen, L.J.; Vidovic, D.; Koleti, A.; Schurer, S.C.; et al. TCRD and Pharos 2021: Mining the human proteome for disease biology. Nucleic Acids Res. 2021, 49, D1334–D1346. [Google Scholar] [CrossRef]
- Taukulis, I.A.; Olszewski, R.T.; Korrapati, S.; Fernandez, K.A.; Boger, E.T.; Fitzgerald, T.S.; Morell, R.J.; Cunningham, L.L.; Hoa, M. Single-Cell RNA-Seq of Cisplatin-Treated Adult Stria Vascularis Identifies Cell Type-Specific Regulatory Networks and Novel Therapeutic Gene Targets. Front. Mol. Neurosci. 2021, 14, 718241. [Google Scholar] [CrossRef] [PubMed]
- Hescheler, D.A.; Riemann, B.; Hartmann, M.J.M.; Michel, M.; Faust, M.; Bruns, C.J.; Alakus, H.; Chiapponi, C. Targeted Therapy of Papillary Thyroid Cancer: A Comprehensive Genomic Analysis. Front. Endocrinol. 2021, 12, 748941. [Google Scholar] [CrossRef]
- Advani, D.; Kumar, P. Therapeutic Targeting of Repurposed Anticancer Drugs in Alzheimer’s Disease: Using the Multiomics Approach. ACS Omega 2021, 6, 13870–13887. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.; Wang, G.; Yarmus, L.B.; Wan, Y. Combined Methylome and Transcriptome Analyses Reveals Potential Therapeutic Targets for EGFR Wild Type Lung Cancers with Low PD-L1 Expression. Cancers 2020, 12, 2496. [Google Scholar] [CrossRef]
- Gelemanovic, A.; Vidovic, T.; Stepanic, V.; Trajkovic, K. Identification of 37 Heterogeneous Drug Candidates for Treatment of COVID-19 via a Rational Transcriptomics-Based Drug Repurposing Approach. Pharmaceuticals 2021, 14, 87. [Google Scholar] [CrossRef] [PubMed]
- Kropiwnicki, E.; Evangelista, J.E.; Stein, D.J.; Clarke, D.J.B.; Lachmann, A.; Kuleshov, M.V.; Jeon, M.; Jagodnik, K.M.; Ma’ayan, A. Drugmonizome and Drugmonizome-ML: Integration and abstraction of small molecule attributes for drug enrichment analysis and machine learning. Database 2021, 2021. [Google Scholar] [CrossRef]
- Kuhn, M.; Letunic, I.; Jensen, L.J.; Bork, P. The SIDER database of drugs and side effects. Nucleic Acids Res 2016, 44, D1075–D1079. [Google Scholar] [CrossRef] [PubMed]
- Masoudi-Sobhanzadeh, Y.; Omidi, Y.; Amanlou, M.; Masoudi-Nejad, A. Drug databases and their contributions to drug repurposing. Genomics 2020, 112, 1087–1095. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Qiu, Y.; Hou, W.; Cheng, X.; Yim, M.Y.; Ching, W.K. Drug Side-Effect Profiles Prediction: From Empirical to Structural Risk Minimization. IEEE/ACM Trans. Comput. Biol. Bioinform. 2020, 17, 402–410. [Google Scholar] [CrossRef]
- Uhr, M.; Grauer, M.T.; Yassouridis, A.; Ebinger, M. Blood-brain barrier penetration and pharmacokinetics of amitriptyline and its metabolites in p-glycoprotein (abcb1ab) knock-out mice and controls. J. Psychiatr. Res. 2007, 41, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Hendset, M.; Haslemo, T.; Rudberg, I.; Refsum, H.; Molden, E. The complexity of active metabolites in therapeutic drug monitoring of psychotropic drugs. Pharmacopsychiatry 2006, 39, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Sun, Y.; Hu, B.; He, Z.; Chen, S.; Qi, D.; An, H.; Wei, Y. Organic Cation Transporters are Involved in Fluoxetine Transport Across the Blood-Brain Barrier in Vivo and in Vitro. Curr Drug Deliv 2021. [Google Scholar] [CrossRef]
- Geldof, M.; Freijer, J.; van Beijsterveldt, L.; Danhof, M. Pharmacokinetic modeling of non-linear brain distribution of fluvoxamine in the rat. Pharm. Res. 2008, 25, 792–804. [Google Scholar] [CrossRef] [PubMed]
- Akanuma, S.I.; Han, M.; Murayama, Y.; Kubo, Y.; Hosoya, K.I. Differences in Cerebral Distribution between Imipramine and Paroxetine via Membrane Transporters at the Rat Blood-Brain Barrier. Pharm. Res. 2022, 39, 223–237. [Google Scholar] [CrossRef]
- Nacca, A.; Guiso, G.; Fracasso, C.; Cervo, L.; Caccia, S. Brain-to-blood partition and in vivo inhibition of 5-hydroxytryptamine reuptake and quipazine-mediated behaviour of nefazodone and its main active metabolites in rodents. Br. J. Pharmacol. 1998, 125, 1617–1623. [Google Scholar] [CrossRef] [PubMed]
- Gelenberg, A.J. A review of the current guidelines for depression treatment. J. Clin. Psychiatry 2010, 71, e15. [Google Scholar] [CrossRef] [PubMed]
- Gautam, S.; Jain, A.; Gautam, M.; Vahia, V.N.; Gautam, A. Clinical Practice Guidelines for the Management of Generalised Anxiety Disorder (GAD) and Panic Disorder (PD). Indian J. Psychiatry 2017, 59, S67–S73. [Google Scholar] [CrossRef]
- Koran, L.M.; Hanna, G.L.; Hollander, E.; Nestadt, G.; Simpson, H.B.; American Psychiatric, A. Practice guideline for the treatment of patients with obsessive-compulsive disorder. Am. J. Psychiatry 2007, 164, 5–53. [Google Scholar] [PubMed]
- Martin, A.; Naunton, M.; Kosari, S.; Peterson, G.; Thomas, J.; Christenson, J.K. Treatment Guidelines for PTSD: A Systematic Review. J. Clin. Med. 2021, 10, 4175. [Google Scholar] [CrossRef]
- McCain, J.A. Antidepressants and suicide in adolescents and adults: A public health experiment with unintended consequences? P T 2009, 34, 355–378. [Google Scholar] [PubMed]
- Spielmans, G.I.; Spence-Sing, T.; Parry, P. Duty to Warn: Antidepressant Black Box Suicidality Warning Is Empirically Justified. Front. Psychiatry 2020, 11, 18. [Google Scholar] [CrossRef] [PubMed]
- Thanacoody, H.K.; Thomas, S.H. Tricyclic antidepressant poisoning: Cardiovascular toxicity. Toxicol. Rev. 2005, 24, 205–214. [Google Scholar] [CrossRef]
- Schneider, J.; Patterson, M.; Jimenez, X.F. Beyond depression: Other uses for tricyclic antidepressants. Cleve. Clin. J. Med. 2019, 86, 807–814. [Google Scholar] [CrossRef] [PubMed]
- Abouzari, M.; Goshtasbi, K.; Chua, J.T.; Tan, D.; Sarna, B.; Saber, T.; Lin, H.W.; Djalilian, H.R. Adjuvant Migraine Medications in the Treatment of Sudden Sensorineural Hearing Loss. Laryngoscope 2021, 131, E283–E288. [Google Scholar] [CrossRef]
- Goshtasbi, K.; Chua, J.T.; Risbud, A.; Sarna, B.; Jamshidi, S.; Abouzari, M.; Djalilian, H.R. Treatment of Long-term Sudden Sensorineural Hearing Loss as an Otologic Migraine Phenomenon. Otol. Neurotol. 2021, 42, 1001–1007. [Google Scholar] [CrossRef]
- Oskotsky, T.; Maric, I.; Tang, A.; Oskotsky, B.; Wong, R.J.; Aghaeepour, N.; Sirota, M.; Stevenson, D.K. Mortality Risk Among Patients With COVID-19 Prescribed Selective Serotonin Reuptake Inhibitor Antidepressants. JAMA Netw. Open. 2021, 4, e2133090. [Google Scholar] [CrossRef]
- Lenze, E.J.; Mattar, C.; Zorumski, C.F.; Stevens, A.; Schweiger, J.; Nicol, G.E.; Miller, J.P.; Yang, L.; Yingling, M.; Avidan, M.S.; et al. Fluvoxamine vs Placebo and Clinical Deterioration in Outpatients With Symptomatic COVID-19: A Randomized Clinical Trial. JAMA 2020, 324, 2292–2300. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Snyder, G.L.; Vanover, K.E. Dopamine Targeting Drugs for the Treatment of Schizophrenia: Past, Present and Future. Curr. Top. Med. Chem. 2016, 16, 3385–3403. [Google Scholar] [CrossRef] [PubMed]
- Meeks, T.W.; Jeste, D.V. Beyond the Black Box: What is The Role for Antipsychotics in Dementia? Curr. Psychiatr. 2008, 7, 50–65. [Google Scholar] [PubMed]
- Duma, S.R.; Fung, V.S. Drug-induced movement disorders. Aust. Prescr. 2019, 42, 56–61. [Google Scholar] [CrossRef]
- Long, J.M.; Holtzman, D.M. Alzheimer Disease: An Update on Pathobiology and Treatment Strategies. Cell 2019, 179, 312–339. [Google Scholar] [CrossRef] [PubMed]
- Runde, T.J.; Nappe, T.M. Salicylates Toxicity; StatPearls: Treasure Island, FL, USA, 2022. [Google Scholar]
- Enright, J.M.; Karacal, H.; Tsai, L.M. Floppy iris syndrome and cataract surgery. Curr. Opin. Ophthalmol. 2017, 28, 29–34. [Google Scholar] [CrossRef]
- Lapierre, Y.; Bouchard, S.; Tansey, C.; Gendron, D.; Barkas, W.J.; Francis, G.S. Treatment of spasticity with tizanidine in multiple sclerosis. Can. J. Neurol. Sci. 1987, 14, 513–517. [Google Scholar] [CrossRef][Green Version]
- Li, K.; Wang, X.F.; Li, D.Y.; Chen, Y.C.; Zhao, L.J.; Liu, X.G.; Guo, Y.F.; Shen, J.; Lin, X.; Deng, J.; et al. The good, the bad, and the ugly of calcium supplementation: A review of calcium intake on human health. Clin. Interv. Aging 2018, 13, 2443–2452. [Google Scholar] [CrossRef]
- Xiao, Q.; Murphy, R.A.; Houston, D.K.; Harris, T.B.; Chow, W.H.; Park, Y. Dietary and supplemental calcium intake and cardiovascular disease mortality: The National Institutes of Health-AARP diet and health study. JAMA Intern. Med. 2013, 173, 639–646. [Google Scholar] [CrossRef]
- Roberts, E.E.; Nowsheen, S.; Davis, D.M.R.; Hand, J.L.; Tollefson, M.M.; Wetter, D.A. Use of spironolactone to treat acne in adolescent females. Pediatr. Dermatol. 2021, 38, 72–76. [Google Scholar] [CrossRef]
- Lainscak, M.; Pelliccia, F.; Rosano, G.; Vitale, C.; Schiariti, M.; Greco, C.; Speziale, G.; Gaudio, C. Safety profile of mineralocorticoid receptor antagonists: Spironolactone and eplerenone. Int. J. Cardiol. 2015, 200, 25–29. [Google Scholar] [CrossRef]
- Struthers, A.; Krum, H.; Williams, G.H. A comparison of the aldosterone-blocking agents eplerenone and spironolactone. Clin. Cardiol. 2008, 31, 153–158. [Google Scholar] [CrossRef]
- Keirns, J.; Desai, A.; Kowalski, D.; Lademacher, C.; Mujais, S.; Parker, B.; Schneidkraut, M.J.; Townsend, R.; Wojtkowski, T.; Yamazaki, T.; et al. QT Interval Shortening With Isavuconazole: In Vitro and In Vivo Effects on Cardiac Repolarization. Clin. Pharmacol. Ther. 2017, 101, 782–790. [Google Scholar] [CrossRef]
- Ellsworth, M.; Ostrosky-Zeichner, L. Isavuconazole: Mechanism of Action, Clinical Efficacy, and Resistance. J. Fungi. 2020, 6, 324. [Google Scholar] [CrossRef] [PubMed]
- Graham, E.M. Erythromycin. Obstet. Gynecol. Clin. North Am. 1992, 19, 539–549. [Google Scholar] [CrossRef]
- Weber, F.H., Jr.; Richards, R.D.; McCallum, R.W. Erythromycin: A motilin agonist and gastrointestinal prokinetic agent. Am. J. Gastroenterol. 1993, 88, 485–490. [Google Scholar] [PubMed]
- Simons, F.E.; Simons, K.J. The pharmacology and use of H1-receptor-antagonist drugs. N. Engl. J. Med. 1994, 330, 1663–1670. [Google Scholar] [CrossRef] [PubMed]
- Drugs for allergic rhinitis and allergic conjunctivitis. Med. Lett. Drugs Ther. 2021, 63, 57–64.
- Reznikov, L.R.; Norris, M.H.; Vashisht, R.; Bluhm, A.P.; Li, D.; Liao, Y.J.; Brown, A.; Butte, A.J.; Ostrov, D.A. Identification of antiviral antihistamines for COVID-19 repurposing. Biochem. Biophys. Res. Commun. 2021, 538, 173–179. [Google Scholar] [CrossRef]
- Katzenschlager, R.; Sampaio, C.; Costa, J.; Lees, A. Anticholinergics for symptomatic management of Parkinson’s disease. Cochrane Database Syst. Rev. 2003, CD003735. [Google Scholar] [CrossRef]
- Pasko, P.; Rodacki, T.; Domagala-Rodacka, R.; Palimonka, K.; Marcinkowska, M.; Owczarek, D. Second generation H1 - antihistamines interaction with food and alcohol-A systematic review. Biomed. Pharmacother. 2017, 93, 27–39. [Google Scholar] [CrossRef]
- Paik, J. Fostamatinib: A Review in Chronic Immune Thrombocytopenia. Drugs 2021, 81, 935–943. [Google Scholar] [CrossRef]
- Connell, N.T.; Berliner, N. Fostamatinib for the treatment of chronic immune thrombocytopenia. Blood 2019, 133, 2027–2030. [Google Scholar] [CrossRef]
- Hoepel, W.; Chen, H.J.; Geyer, C.E.; Allahverdiyeva, S.; Manz, X.D.; de Taeye, S.W.; Aman, J.; Mes, L.; Steenhuis, M.; Griffith, G.R.; et al. High titers and low fucosylation of early human anti-SARS-CoV-2 IgG promote inflammation by alveolar macrophages. Sci. Transl. Med. 2021, 13. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, M.; Heman-Ackah, S.E.; Shaikh, J.A.; Roehm, P.C. Sudden sensorineural hearing loss: A review of diagnosis, treatment, and prognosis. Trends Amplif. 2011, 15, 91–105. [Google Scholar] [CrossRef] [PubMed]
- Fetterman, B.L.; Saunders, J.E.; Luxford, W.M. Prognosis and treatment of sudden sensorineural hearing loss. Am. J. Otol. 1996, 17, 529–536. [Google Scholar] [PubMed]
- Battaglia, A.; Lualhati, A.; Lin, H.; Burchette, R.; Cueva, R. A prospective, multi-centered study of the treatment of idiopathic sudden sensorineural hearing loss with combination therapy versus high-dose prednisone alone: A 139 patient follow-up. Otol. Neurotol. 2014, 35, 1091–1098. [Google Scholar] [CrossRef]
- Chandrasekhar, S.S. Intratympanic dexamethasone for sudden sensorineural hearing loss: Clinical and laboratory evaluation. Otol. Neurotol. 2001, 22, 18–23. [Google Scholar] [CrossRef]
- Rauch, S.D.; Halpin, C.F.; Antonelli, P.J.; Babu, S.; Carey, J.P.; Gantz, B.J.; Goebel, J.A.; Hammerschlag, P.E.; Harris, J.P.; Isaacson, B.; et al. Oral vs intratympanic corticosteroid therapy for idiopathic sudden sensorineural hearing loss: A randomized trial. JAMA 2011, 305, 2071–2079. [Google Scholar] [CrossRef]
- Bird, P.A.; Begg, E.J.; Zhang, M.; Keast, A.T.; Murray, D.P.; Balkany, T.J. Intratympanic versus intravenous delivery of methylprednisolone to cochlear perilymph. Otol. Neurotol. 2007, 28, 1124–1130. [Google Scholar] [CrossRef]
- Merchant, S.N.; Durand, M.L.; Adams, J.C. Sudden deafness: Is it viral? ORL J. Otorhinolaryngol. Relat. Spec. 2008, 70, 52–60. [Google Scholar] [CrossRef]
- Froehlich, M.H.; Lambert, P.R. The Physiologic Role of Corticosteroids in Meniere’s Disease: An Update on Glucocorticoid-mediated Pathophysiology and Corticosteroid Inner Ear Distribution. Otol. Neurotol. 2020, 41, 271–276. [Google Scholar] [CrossRef]
- Trune, D.R. Ion homeostasis in the ear: Mechanisms, maladies, and management. Curr. Opin. Otolaryngol. Head Neck Surg. 2010, 18, 413–419. [Google Scholar] [CrossRef]
- Wei, B.P.; Stathopoulos, D.; O’Leary, S. Steroids for idiopathic sudden sensorineural hearing loss. Cochrane Database Syst. Rev. 2013, CD003998. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.H.; Kim, M.E.; Kim, H.Y.; Lee, J.S.; Jang, C.H. Inflammatory cytokines and mononuclear cells in sudden sensorineural hearing loss. J. Laryngol. Otol. 2019, 133, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.W.; Kim, M.G.; Kim, S.S.; Im, H.I.; Dong, S.H.; Kim, S.H.; Yeo, S.G. Neutrophil-lymphocyte ratio as a valuable prognostic marker in idiopathic sudden sensorineural hearing loss. Acta Otolaryngol. 2020, 140, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Bayoumy, A.B.; van der Veen, E.L.; Alexander de Ru, J. Assessment of Spontaneous Recovery Rates in Patients With Idiopathic Sudden Sensorineural Hearing Loss. JAMA Otolaryngol. Head Neck Surg. 2018, 144, 655–656. [Google Scholar] [CrossRef] [PubMed]
- Labus, J.; Breil, J.; Stutzer, H.; Michel, O. Meta-analysis for the effect of medical therapy vs. placebo on recovery of idiopathic sudden hearing loss. Laryngoscope 2010, 120, 1863–1871. [Google Scholar] [CrossRef] [PubMed]
- Cinamon, U.; Bendet, E.; Kronenberg, J. Steroids, carbogen or placebo for sudden hearing loss: A prospective double-blind study. Eur. Arch. Otorhinolaryngol. 2001, 258, 477–480. [Google Scholar] [CrossRef] [PubMed]
- Nosrati-Zarenoe, R.; Hultcrantz, E. Corticosteroid treatment of idiopathic sudden sensorineural hearing loss: Randomized triple-blind placebo-controlled trial. Otol. Neurotol. 2012, 33, 523–531. [Google Scholar] [CrossRef]
- Casani, A.P.; Piaggi, P.; Cerchiai, N.; Seccia, V.; Franceschini, S.S.; Dallan, I. Intratympanic treatment of intractable unilateral Meniere disease: Gentamicin or dexamethasone? A randomized controlled trial. Otolaryngol. Head Neck Surg. 2012, 146, 430–437. [Google Scholar] [CrossRef]
- Patel, M.; Agarwal, K.; Arshad, Q.; Hariri, M.; Rea, P.; Seemungal, B.M.; Golding, J.F.; Harcourt, J.P.; Bronstein, A.M. Intratympanic methylprednisolone versus gentamicin in patients with unilateral Meniere’s disease: A randomised, double-blind, comparative effectiveness trial. Lancet 2016, 388, 2753–2762. [Google Scholar] [CrossRef]
- Silverstein, H.; Isaacson, J.E.; Olds, M.J.; Rowan, P.T.; Rosenberg, S. Dexamethasone inner ear perfusion for the treatment of Meniere's disease: A prospective, randomized, double-blind, crossover trial. Am. J. Otol. 1998, 19, 196–201. [Google Scholar]
- Lavigne, P.; Lavigne, F.; Saliba, I. Intratympanic corticosteroids injections: A systematic review of literature. Eur. Arch. Otorhinolaryngol. 2016, 273, 2271–2278. [Google Scholar] [CrossRef] [PubMed]
- Patel, M. Intratympanic corticosteroids in Meniere’s disease: A mini-review. J. Otol. 2017, 12, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Garduno-Anaya, M.A.; Couthino De Toledo, H.; Hinojosa-Gonzalez, R.; Pane-Pianese, C.; Rios-Castaneda, L.C. Dexamethasone inner ear perfusion by intratympanic injection in unilateral Meniere’s disease: A two-year prospective, placebo-controlled, double-blind, randomized trial. Otolaryngol. Head Neck Surg. 2005, 133, 285–294. [Google Scholar] [CrossRef] [PubMed]
- Morales-Luckie, E.; Cornejo-Suarez, A.; Zaragoza-Contreras, M.A.; Gonzalez-Perez, O. Oral administration of prednisone to control refractory vertigo in Meniere’s disease: A pilot study. Otol. Neurotol. 2005, 26, 1022–1026. [Google Scholar] [CrossRef]
- Salt, A.N.; Plontke, S.K. Pharmacokinetic principles in the inner ear: Influence of drug properties on intratympanic applications. Hear Res. 2018, 368, 28–40. [Google Scholar] [CrossRef]
- Schubert, N.M.A.; van Tuinen, M.; Pyott, S.J. Transcriptome-Guided Identification of Drugs for Repurposing to Treat Age-Related Hearing Loss. Biomolecules 2022, 12, 498. [Google Scholar] [CrossRef]
- Chakraborty, C.; Sharma, A.R.; Bhattacharya, M.; Agoramoorthy, G.; Lee, S.S. The Drug Repurposing for COVID-19 Clinical Trials Provide Very Effective Therapeutic Combinations: Lessons Learned From Major Clinical Studies. Front. Pharmacol. 2021, 12, 704205. [Google Scholar] [CrossRef]
- Fernandez, K.A.; Watabe, T.; Tong, M.; Meng, X.; Tani, K.; Kujawa, S.G.; Edge, A.S. Trk agonist drugs rescue noise-induced hidden hearing loss. JCI Insight 2021, 6. [Google Scholar] [CrossRef]
- Shibata, S.B.; Osumi, Y.; Yagi, M.; Kanda, S.; Kawamoto, K.; Kuriyama, H.; Nishiyama, T.; Yamashita, T. Administration of amitriptyline attenuates noise-induced hearing loss via glial cell line-derived neurotrophic factor (GDNF) induction. Brain Res. 2007, 1144, 74–81. [Google Scholar] [CrossRef]
- Numakawa, T.; Yokomaku, D.; Richards, M.; Hori, H.; Adachi, N.; Kunugi, H. Functional interactions between steroid hormones and neurotrophin BDNF. World J. Biol. Chem. 2010, 1, 133–143. [Google Scholar] [CrossRef]
- Nicholson, R.I.; McClelland, R.A.; Robertson, J.F.; Gee, J.M. Involvement of steroid hormone and growth factor cross-talk in endocrine response in breast cancer. Endocr. Relat. Cancer 1999, 6, 373–387. [Google Scholar] [CrossRef][Green Version]
- Podoshin, L.; Ben-David, Y.; Fradis, M.; Malatskey, S.; Hafner, H. Idiopathic Subjective Tinnitus Treated by Amitriptyline Hydrochloride/Biofeedback. Int. Tinnitus. J. 1995, 1, 54–60. [Google Scholar]
- Lauritsen, C.G.; Marmura, M.J. Current Treatment Options: Vestibular Migraine. Curr. Treat Options Neurol. 2017, 19, 38. [Google Scholar] [CrossRef]
- Han, J.J.; Jung, J.Y.; Park, K.H.; Lee, H.Y.; Lee, B.D.; Choi, S.J.; Lee, C.K. Nimodipine and Steroid Combination Therapy for Idiopathic Sudden Sensorineural Hearing Loss. Otol. Neurotol. 2020, 41, e783–e789. [Google Scholar] [CrossRef]
- Lenarz, T. [Treatment of sudden deafness with the calcium antagonist nimodipine. Results of a comparative study]. Laryngorhinootologie 1989, 68, 634–637. [Google Scholar] [CrossRef]
- Mann, W.; Beck, C.; Beck, C. Calcium antagonists in the treatment of sudden deafness. Arch Otorhinolaryngol. 1986, 243, 170–173. [Google Scholar] [CrossRef]
- Monzani, D.; Genovese, E.; Pini, L.A.; Di Berardino, F.; Alicandri Ciufelli, M.; Galeazzi, G.M.; Presutti, L. Nimodipine in otolaryngology: From past evidence to clinical perspectives. Acta Otorhinolaryngol. Ital. 2015, 35, 135–145. [Google Scholar]
- Coleman, J.K.; Dengerink, H.A.; Wright, J.W. Effects of hydroxyethyl starch, nimodipine, and propylene glycol on cochlear blood flow. Otolaryngol. Head Neck Surg. 1991, 105, 840–844. [Google Scholar] [CrossRef]
- Tomassoni, D.; Lanari, A.; Silvestrelli, G.; Traini, E.; Amenta, F. Nimodipine and its use in cerebrovascular disease: Evidence from recent preclinical and controlled clinical studies. Clin. Exp. Hypertens. 2008, 30, 744–766. [Google Scholar] [CrossRef]
- Duan, M.; Qiu, J.; Laurell, G.; Olofsson, A.; Counter, S.A.; Borg, E. Dose and time-dependent protection of the antioxidant N-L-acetylcysteine against impulse noise trauma. Hear Res. 2004, 192, 1–9. [Google Scholar] [CrossRef]
- Kopke, R.; Slade, M.D.; Jackson, R.; Hammill, T.; Fausti, S.; Lonsbury-Martin, B.; Sanderson, A.; Dreisbach, L.; Rabinowitz, P.; Torre, P., 3rd; et al. Efficacy and safety of N-acetylcysteine in prevention of noise induced hearing loss: A randomized clinical trial. Hear Res. 2015, 323, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Pathak, S.; Stern, C.; Vambutas, A. N-Acetylcysteine attenuates tumor necrosis factor alpha levels in autoimmune inner ear disease patients. Immunol. Res. 2015, 63, 236–245. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Marie, A.; Meunier, J.; Brun, E.; Malmstrom, S.; Baudoux, V.; Flaszka, E.; Naert, G.; Roman, F.; Cosnier-Pucheu, S.; Gonzalez-Gonzalez, S. N-acetylcysteine Treatment Reduces Age-related Hearing Loss and Memory Impairment in the Senescence-Accelerated Prone 8 (SAMP8) Mouse Model. Aging Dis. 2018, 9, 664–673. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.P.; Hsu, C.J.; Cheng, T.J.; Guo, Y.L. N-acetylcysteine attenuates noise-induced permanent hearing loss in diabetic rats. Hear Res. 2010, 267, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Motalebi Kashani, M.; Saberi, H.; Hannani, M. Prevention of Acoustic Trauma-Induced Hearing Loss by N-acetylcysteine Administration in Rabbits. Arch. Trauma. Res. 2013, 1, 145–150. [Google Scholar] [CrossRef]
- Chen, C.H.; Young, Y.H. N-acetylcysteine as a single therapy for sudden deafness. Acta Otolaryngol. 2017, 137, 58–62. [Google Scholar] [CrossRef]
- Angeli, S.I.; Abi-Hachem, R.N.; Vivero, R.J.; Telischi, F.T.; Machado, J.J. L-N-Acetylcysteine treatment is associated with improved hearing outcome in sudden idiopathic sensorineural hearing loss. Acta Otolaryngol. 2012, 132, 369–376. [Google Scholar] [CrossRef]
- Capaccio, P.; Pignataro, L.; Gaini, L.M.; Sigismund, P.E.; Novembrino, C.; De Giuseppe, R.; Uva, V.; Tripodi, A.; Bamonti, F. Unbalanced oxidative status in idiopathic sudden sensorineural hearing loss. Eur. Arch. Otorhinolaryngol. 2012, 269, 449–453. [Google Scholar] [CrossRef]
- Eftekhari, P.; Hajizadeh, S.; Raoufy, M.R.; Masjedi, M.R.; Yang, M.; Hansbro, N.; Li, J.J.; Foster, P.S. Preventive effect of N-acetylcysteine in a mouse model of steroid resistant acute exacerbation of asthma. EXCLI J. 2013, 12, 184–192. [Google Scholar]
- Franco-Vidal, V.; Beurg, M.; Darrouzet, V.; Bebear, J.P.; Skinner, L.J.; Dulon, D. Zinc protection against pneumolysin toxicity on rat cochlear hair cells. Audiol. Neurootol. 2008, 13, 65–70. [Google Scholar] [CrossRef]
- Zirpel, L.; Parks, T.N. Zinc inhibition of group I mGluR-mediated calcium homeostasis in auditory neurons. J. Assoc. Res. Otolaryngol. 2001, 2, 180–187. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Powell, S.R. The antioxidant properties of zinc. J. Nutr. 2000, 130, 1447S–1454S. [Google Scholar] [CrossRef] [PubMed]
- Prasad, A.S.; Beck, F.W.; Bao, B.; Snell, D.; Fitzgerald, J.T. Duration and severity of symptoms and levels of plasma interleukin-1 receptor antagonist, soluble tumor necrosis factor receptor, and adhesion molecules in patients with common cold treated with zinc acetate. J. Infect. Dis. 2008, 197, 795–802. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.H.; Ko, M.T.; Peng, J.P.; Hwang, C.F. Zinc in the treatment of idiopathic sudden sensorineural hearing loss. Laryngoscope 2011, 121, 617–621. [Google Scholar] [CrossRef] [PubMed]
- Hunchaisri, N.; Chantapant, S.; Sirirattanapan, J. Effectiveness of oral zinc supplementation in the treatment of idiopathic sudden sensorineural hearing loss (ISSNHL). J. Med. Assoc. Thai. 2015, 98, 400–407. [Google Scholar]
- Panettieri, R.A.; Schaafsma, D.; Amrani, Y.; Koziol-White, C.; Ostrom, R.; Tliba, O. Non-genomic Effects of Glucocorticoids: An Updated View. Trends Pharmacol. Sci. 2019, 40, 38–49. [Google Scholar] [CrossRef]
- Hou, Y.C.; Yu, H.C.; Martin, R.; Cirulli, E.T.; Schenker-Ahmed, N.M.; Hicks, M.; Cohen, I.V.; Jonsson, T.J.; Heister, R.; Napier, L.; et al. Precision medicine integrating whole-genome sequencing, comprehensive metabolomics, and advanced imaging. Proc. Natl. Acad. Sci. USA 2020, 117, 3053–3062. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Missner, A.A.; Johns, J.D.; Gu, S.; Hoa, M. Repurposable Drugs That Interact with Steroid Responsive Gene Targets for Inner Ear Disease. Biomolecules 2022, 12, 1641. https://doi.org/10.3390/biom12111641
Missner AA, Johns JD, Gu S, Hoa M. Repurposable Drugs That Interact with Steroid Responsive Gene Targets for Inner Ear Disease. Biomolecules. 2022; 12(11):1641. https://doi.org/10.3390/biom12111641
Chicago/Turabian StyleMissner, Alexander A., James Dixon Johns, Shoujun Gu, and Michael Hoa. 2022. "Repurposable Drugs That Interact with Steroid Responsive Gene Targets for Inner Ear Disease" Biomolecules 12, no. 11: 1641. https://doi.org/10.3390/biom12111641
APA StyleMissner, A. A., Johns, J. D., Gu, S., & Hoa, M. (2022). Repurposable Drugs That Interact with Steroid Responsive Gene Targets for Inner Ear Disease. Biomolecules, 12(11), 1641. https://doi.org/10.3390/biom12111641








