A Synergistic Effect between Plasma Dickkopf-1 and Obstructive Coronary Artery Disease on the Prediction of Major Adverse Cardiac Events in Patients with Angina: An Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Procedures
2.3. Laboratory Assessments
2.4. Statistical Analysis
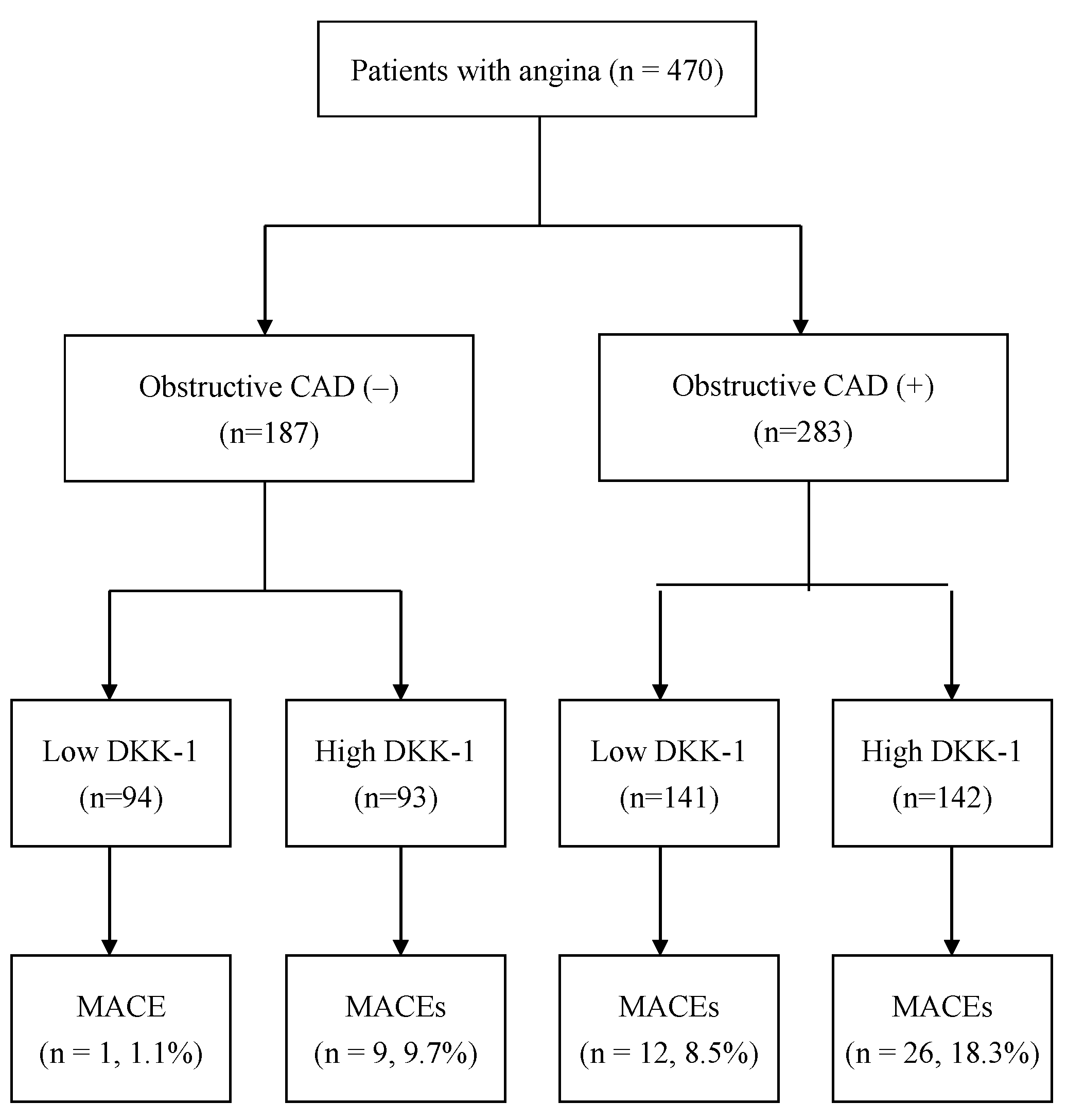
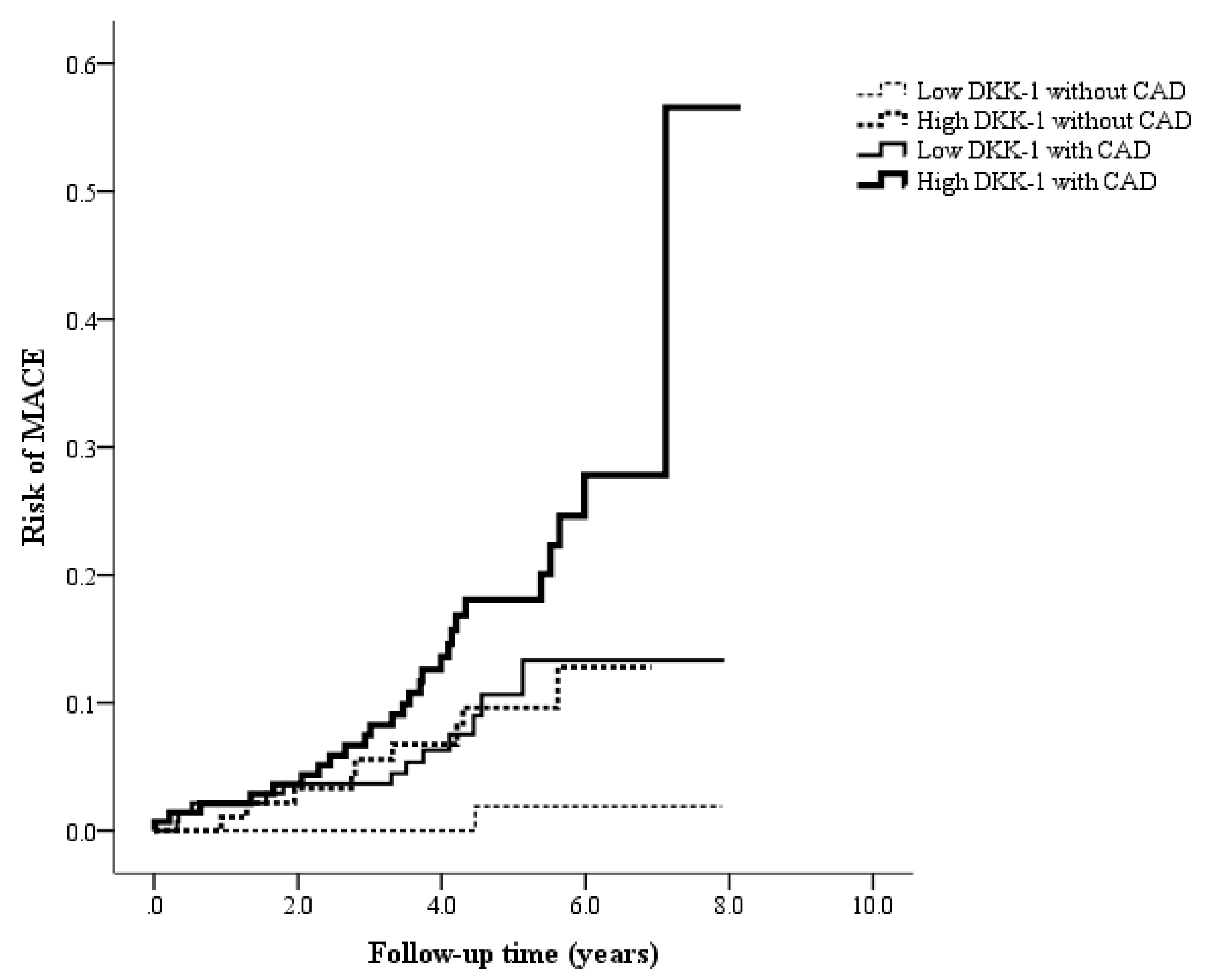
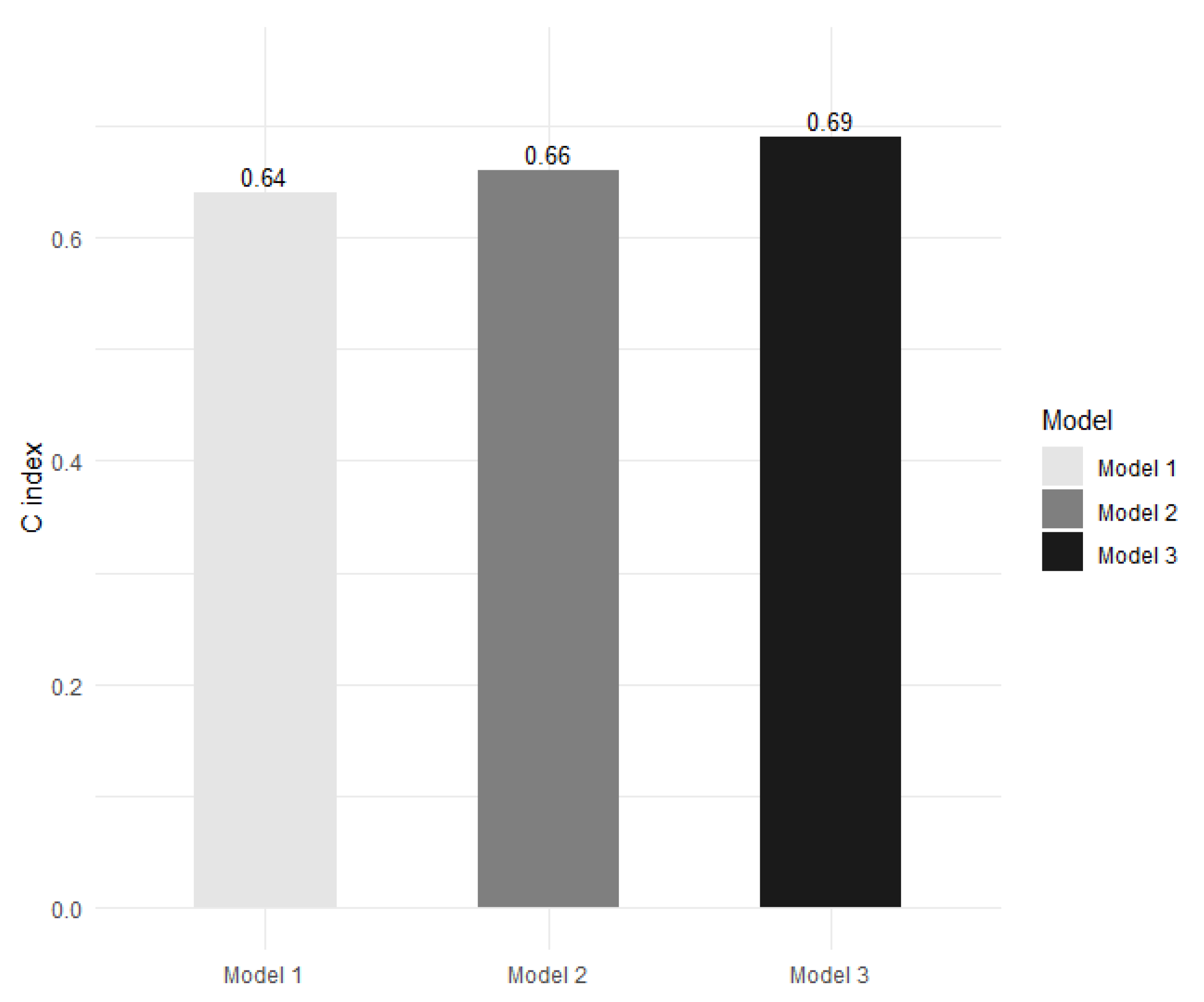
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Khan, M.A.; Hashim, M.J.; Mustafa, H.; Baniyas, M.Y.; Al Suwaidi, S.; AlKatheeri, R.; Alblooshi, F.M.K.; Almatrooshi, M.; Alzaabi, M.E.H.; Al Darmaki, R.S.; et al. Global Epidemiology of Ischemic Heart Disease: Results from the Global Burden of Disease Study. Cureus 2020, 12, e9349. [Google Scholar] [CrossRef] [PubMed]
- Dai, H.; Much, A.A.; Maor, E.; Asher, E.; Younis, A.; Xu, Y.; Lu, Y.; Liu, X.; Shu, J.; Bragazzi, N.L. Global, regional, and national burden of ischemic heart disease and its attributable risk factors, 1990–2017: Results from the global Burden of Disease Study 2017. Eur. Heart J. Qual. Care Clin. Outcomes 2022, 8, 50–60. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Traghella, I.; Mastorci, F.; Pepe, A.; Pingitore, A.; Vassalle, C. Nontraditional Cardiovascular Biomarkers and Risk Factors: Rationale and Future Perspectives. Biomolecules 2018, 8, 40. [Google Scholar] [CrossRef]
- Glinka, A.; Wu, W.; Delius, H.; Monaghan, A.P.; Blumenstock, C.; Niehrs, C. Dickkopf-1 is a member of a new family of secreted proteins and functions in head induction. Nature 1998, 391, 357–362. [Google Scholar] [CrossRef]
- MacDonald, B.T.; Tamai, K.; He, X. Wnt/beta-catenin signaling: Components, mechanisms, and diseases. Dev. Cell 2009, 17, 9–26. [Google Scholar] [CrossRef]
- Foulquier, S.; Daskalopoulos, E.P.; Lluri, G.; Hermans, K.C.M.; Deb, A.; Blankesteijn, W.M. WNT Signaling in Cardiac and Vascular Disease. Pharmacol. Rev. 2018, 70, 68–141. [Google Scholar] [CrossRef]
- Lee, D.K.; Nathan Grantham, R.; Trachte, A.L.; Mannion, J.D.; Wilson, C.L. Activation of the canonical Wnt/beta-catenin pathway enhances monocyte adhesion to endothelial cells. Biochem. Biophys. Res. Commun. 2006, 347, 109–116. [Google Scholar] [CrossRef]
- Li, M.; Liu, X.; Zhang, Y.; Di, M.; Wang, H.; Wang, L.; Chen, Y.; Liu, X.; Cao, X.; Zeng, R.; et al. Upregulation of Dickkopf1 by oscillatory shear stress accelerates atherogenesis. J. Mol. Med. 2016, 94, 431–441. [Google Scholar] [CrossRef]
- Ueland, T.; Akerblom, A.; Ghukasyan, T.; Michelsen, A.E.; Becker, R.C.; Bertilsson, M.; Himmelmann, A.; James, S.K.; Siegbahn, A.; Storey, R.F.; et al. Admission Levels of DKK1 (Dickkopf-1) Are Associated with Future Cardiovascular Death in Patients with Acute Coronary Syndromes. Arterioscler. Thromb. Vasc. Biol. 2019, 39, 294–302. [Google Scholar] [CrossRef] [PubMed]
- Ueland, T.; Otterdal, K.; Lekva, T.; Halvorsen, B.; Gabrielsen, A.; Sandberg, W.J.; Paulsson-Berne, G.; Pedersen, T.M.; Folkersen, L.; Gullestad, L.; et al. Dickkopf-1 enhances inflammatory interaction between platelets and endothelial cells and shows increased expression in atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2009, 29, 1228–1234. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; Das, S.R.; de Ferranti, S.; Despres, J.P.; Fullerton, H.J.; et al. Heart Disease and Stroke Statistics-2016 Update: A Report from the American Heart Association. Circulation 2016, 133, e38–e360. [Google Scholar] [CrossRef]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef]
- Inker, L.A.; Astor, B.C.; Fox, C.H.; Isakova, T.; Lash, J.P.; Peralta, C.A.; Kurella Tamura, M.; Feldman, H.I. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am. J. Kidney Dis. 2014, 63, 713–735. [Google Scholar] [CrossRef] [PubMed]
- D’Agostino, R.B., Sr.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation 2008, 117, 743–753. [Google Scholar] [CrossRef]
- Uno, H.; Cai, T.; Pencina, M.J.; D’Agostino, R.B.; Wei, L.J. On the C-statistics for evaluating overall adequacy of risk prediction procedures with censored survival data. Stat. Med. 2011, 30, 1105–1117. [Google Scholar] [CrossRef]
- Pencina, M.J.; D’Agostino, R.B., Sr.; Steyerberg, E.W. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat. Med. 2011, 30, 11–21. [Google Scholar] [CrossRef]
- Klingenschmid, G.; Tschiderer, L.; Himmler, G.; Rungger, G.; Brugger, S.; Santer, P.; Willeit, J.; Kiechl, S.; Willeit, P. Associations of Serum Dickkopf-1 and Sclerostin with Cardiovascular Events: Results from the Prospective Bruneck Study. J. Am. Heart Assoc. 2020, 9, e014816. [Google Scholar] [CrossRef]
- Seifert-Held, T.; Pekar, T.; Gattringer, T.; Simmet, N.E.; Scharnagl, H.; Stojakovic, T.; Fazekas, F.; Storch, M.K. Circulating Dickkopf-1 in acute ischemic stroke and clinically stable cerebrovascular disease. Atherosclerosis 2011, 218, 233–237. [Google Scholar] [CrossRef]
- Register, T.C.; Hruska, K.A.; Divers, J.; Bowden, D.W.; Palmer, N.D.; Carr, J.J.; Wagenknecht, L.E.; Hightower, R.C.; Xu, J.; Smith, S.C.; et al. Plasma Dickkopf1 (DKK1) concentrations negatively associate with atherosclerotic calcified plaque in African-Americans with type 2 diabetes. J. Clin. Endocrinol. Metab. 2013, 98, E60–E65. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Hu, X.B.; Zhang, W.; Wu, L.D.; Liu, Y.S.; Hu, B.; Bi, C.L.; Chen, Y.F.; Liu, X.X.; Ge, C.; et al. Dickkopf-1 as a novel predictor is associated with risk stratification by GRACE risk scores for predictive value in patients with acute coronary syndrome: A retrospective research. PLoS ONE 2013, 8, e54731. [Google Scholar] [CrossRef] [PubMed]
- Cohen, E.D.; Tian, Y.; Morrisey, E.E. Wnt signaling: An essential regulator of cardiovascular differentiation, morphogenesis and progenitor self-renewal. Development 2008, 135, 789–798. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Neogi, A.; Mani, A. The role of Wnt signalling in development of coronary artery disease and its risk factors. Open Biol. 2020, 10, 200128. [Google Scholar] [CrossRef]
- Zhou, X.; Hu, X.; Xie, J.; Xu, C.; Xu, W.; Jiang, H. Exogenous high-mobility group box 1 protein injection improves cardiac function after myocardial infarction: Involvement of Wnt signaling activation. J. Biomed. Biotechnol. 2012, 2012, 743879. [Google Scholar] [CrossRef]
- Baetta, R.; Banfi, C. Dkk (Dickkopf) Proteins. Arterioscler. Thromb. Vasc. Biol. 2019, 39, 1330–1342. [Google Scholar] [CrossRef]
- Di, M.; Wang, L.; Li, M.; Zhang, Y.; Liu, X.; Zeng, R.; Wang, H.; Chen, Y.; Chen, W.; Zhang, Y.; et al. Dickkopf1 destabilizes atherosclerotic plaques and promotes plaque formation by inducing apoptosis of endothelial cells through activation of ER stress. Cell Death Dis. 2017, 8, e2917. [Google Scholar] [CrossRef]
- Guo, Y.; Mishra, A.; Howland, E.; Zhao, C.; Shukla, D.; Weng, T.; Liu, L. Platelet-derived Wnt antagonist Dickkopf-1 is implicated in ICAM-1/VCAM-1-mediated neutrophilic acute lung inflammation. Blood 2015, 126, 2220–2229. [Google Scholar] [CrossRef]
- Lattanzio, S.; Santilli, F.; Liani, R.; Vazzana, N.; Ueland, T.; Di Fulvio, P.; Formoso, G.; Consoli, A.; Aukrust, P.; Davi, G. Circulating dickkopf-1 in diabetes mellitus: Association with platelet activation and effects of improved metabolic control and low-dose aspirin. J. Am. Heart Assoc. 2014, 3, e001000. [Google Scholar] [CrossRef]
- Ford, T.J.; Berry, C. How to Diagnose and Manage Angina without Obstructive Coronary Artery Disease: Lessons from the British Heart Foundation CorMicA Trial. Interv. Cardiol. 2019, 14, 76–82. [Google Scholar] [CrossRef]
- Marzilli, M.; Crea, F.; Morrone, D.; Bonow, R.O.; Brown, D.L.; Camici, P.G.; Chilian, W.M.; DeMaria, A.; Guarini, G.; Huqi, A.; et al. Myocardial ischemia: From disease to syndrome. Int. J. Cardiol. 2020, 314, 32–35. [Google Scholar] [CrossRef] [PubMed]
- Aribas, E.; van Lennep, J.E.R.; Elias-Smale, S.E.; Piek, J.J.; Roos, M.; Ahmadizar, F.; Arshi, B.; Duncker, D.J.; Appelman, Y.; Kavousi, M. Prevalence of microvascular angina among patients with stable symptoms in the absence of obstructive coronary artery disease: A systematic review. Cardiovasc. Res. 2022, 118, 763–771. [Google Scholar] [CrossRef] [PubMed]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 2020, 41, 407–477. [Google Scholar] [CrossRef] [PubMed]
- Jespersen, L.; Hvelplund, A.; Abildstrom, S.Z.; Pedersen, F.; Galatius, S.; Madsen, J.K.; Jorgensen, E.; Kelbaek, H.; Prescott, E. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur. Heart J. 2012, 33, 734–744. [Google Scholar] [CrossRef]
- Rahman, H.; Corcoran, D.; Aetesam-Ur-Rahman, M.; Hoole, S.P.; Berry, C.; Perera, D. Diagnosis of patients with angina and non-obstructive coronary disease in the catheter laboratory. Heart 2019, 105, 1536–1542. [Google Scholar] [CrossRef]
- Qiu, F.; He, J.; Zhou, Y.; Bai, X.; Wu, G.; Wang, X.; Liu, Z.; Chen, Y.; Ma, J.X.; Liu, Z. Plasma and vitreous fluid levels of Dickkopf-1 in patients with diabetic retinopathy. Eye 2014, 28, 402–409. [Google Scholar] [CrossRef]
- Ali, H.; Zmuda, J.M.; Cvejkus, R.K.; Kershaw, E.E.; Kuipers, A.L.; Oczypok, E.A.; Wheeler, V.; Bunker, C.H.; Miljkovic, I. Wnt Pathway Inhibitor DKK1: A Potential Novel Biomarker for Adiposity. J. Endocr. Soc. 2019, 3, 488–495. [Google Scholar] [CrossRef]

| Low DKK-1 without CAD (n = 94) | High DKK-1 without CAD (n = 93) | Low DKK-1 with CAD (n = 141) | High DKK-1 with CAD (n = 142) | p | ||
|---|---|---|---|---|---|---|
| Age (years) | 56.9 ± 11.3 | 60.4 ± 11.9 | 60.6 ± 10.9 | 63.4 ± 11.5 | <0.001 | a |
| Male, n (%) | 64 (68.1%) | 62 (66.7%) | 129 (91.5%) | 125 (88.0%) | <0.001 | |
| Current smoker, n (%) | 21 (22.3%) | 35 (37.6%) | 40 (28.4%) | 53 (37.3%) | 0.044 | |
| BMI (kg/m2) | 26.5 ± 3.9 | 25.6 ± 3.7 | 26.4 ± 3.7 | 26.1 ± 3.9 | 0.104 | k |
| Hypertension, n (%) | 82 (87.2%) | 83 (89.2%) | 134 (95.0%) | 136 (95.8%) | 0.033 | |
| Systolic BP (mmHg) | 126.5 ± 18.4 | 127.4 ± 17.5 | 127.8 ± 16.3 | 128.5 ± 19.3 | 0.868 | a |
| Diastolic BP (mmHg) | 74.8 ± 11.0 | 74.4 ± 10.0 | 75.1 ± 11.1 | 73.8 ± 9.8 | 0.760 | a |
| Fasting glucose (mmol/L) | 5.2 ± 0.7 | 5.3 ± 0.6 | 5.4 ± 0.6 | 5.3 ± 1.0 | 0.092 | k |
| Fasting insulin (µIU/mL) | 11.7 ± 10.2 | 11.5 ± 10.6 | 13.9 ± 17.3 | 11.9 ± 16.1 | 0.215 | k |
| HOMA-IR index | 2.7 ± 2.4 | 2.8 ± 2.8 | 3.4 ± 4.3 | 3.0 ± 5.8 | 0.166 | |
| Total cholesterol (mmol/L) | 4.6 ± 0.8 | 4.8 ± 0.9 | 4.1 ± 0.9 | 4.4 ± 1.1 | <0.001 | k |
| HDL cholesterol (mmol/L) | 1.3 ± 0.3 | 1.3 ± 0.3 | 1.2 ± 0.3 | 1.2 ± 0.3 | <0.001 | k |
| Triglycerides (mmol/L) | 1.5 ± 0.9 | 1.8 ± 1.2 | 1.4 ± 0.7 | 1.6 ± 0.9 | 0.042 | k |
| Framingham Risk Score | 12 ± 4 | 14 ± 5 | 14 ± 4 | 15 ± 4 | <0.001 | k |
| eGFR (mL/min/1.73 m2) | 91.7 ± 29.1 | 82.8 ± 23.7 | 85.6 ± 24.6 | 76.2 ± 24.1 | <0.001 | k |
| Platelet count (109/L) | 207 ± 57 | 219 ± 56 | 199 ± 47 | 207 ± 53 | 0.095 | a |
| C-reactive protein (mg/L) | 1.8 ± 1.9 | 2.3 ± 2.5 | 2.2 ± 2.3 | 3.0 ± 2.7 | 0.003 | k |
| NT-proBNP (pg/mL) | 1907 ± 4654 | 1261 ± 3193 | 1214 ± 3208 | 1484 ± 3153 | 0.085 | k |
| UACR (mg/g) | 24.5 ± 84.1 | 40.8 ± 135.7 | 47.0 ± 148.7 | 44.6 ± 132.3 | 0.068 | k |
| Statins, n (%) | 10 (10.6%) | 20 (21.5%) | 81 (57.4%) | 73 (51.4%) | <0.001 |
| Group | Patient Number | DKK-1 (pg/mL) | p | |
|---|---|---|---|---|
| Age | <60 years | (n = 221) | 588 ± 194 | 0.021 |
| ≥60 years | (n = 249) | 628 ± 183 | ||
| Sex | Female | (n = 90) | 614 ± 184 | 0.775 |
| Male | (n = 380) | 608 ± 190 | ||
| Smokers | No | (n = 321) | 595 ± 190 | 0.015 |
| Yes | (n = 149) | 640 ± 184 | ||
| Hypertension | No | (n = 35) | 602 ± 201 | 0.830 |
| Yes | (n = 435) | 610 ± 188 | ||
| BMI | <27 kg/m2 | (n = 311) | 620 ± 185 | 0.089 |
| ≥27 kg/m2 | (n = 159) | 588 ± 194 | ||
| Systolic BP | <130 mmHg | (n = 260) | 599 ± 189 | 0.210 |
| ≥130 mmHg | (n = 210) | 621 ± 188 | ||
| Diastolic BP | <85 mmHg | (n = 395) | 614 ± 194 | 0.230 |
| ≥85 mmHg | (n = 75) | 585 ± 160 | ||
| Fasting glucose | <5.56 mmol/L | (n = 345) | 611 ± 188 | 0.750 |
| ≥5.56 mmol/L | (n = 125) | 604 ± 190 | ||
| HOMA IR index | <2 | (n = 209) | 635 ± 174 | 0.007 |
| ≥2 | (n = 261) | 588 ± 197 | ||
| Total cholesterol | <4.14 mmol/L | (n = 198) | 608 ± 202 | 0.923 |
| ≥4.14 mmol/L | (n = 272) | 610 ± 179 | ||
| Low HDL cholesterol * | No | (n = 331) | 594 ± 184 | 0.009 |
| Yes | (n = 139) | 644 ± 197 | ||
| Triglycerides | <1.7 mmol/L | (n = 322) | 597 ± 186 | 0.041 |
| ≥1.7 mmol/L | (n = 148) | 635 ± 193 | ||
| eGFR | ≥60 mL/min/1.73 m2 | (n = 380) | 592 ± 183 | 0.001 |
| <60 mL/min/1.73 m2 | (n = 90) | 681 ± 196 | ||
| Platelet count | <203 (109/L) | (n = 235) | 582 ± 173 | 0.002 |
| ≥203 (109/L) | (n = 235) | 636 ± 200 | ||
| C-reactive protein | <1.393 mg/L | (n = 235) | 580 ± 177 | <0.001 |
| ≥1.393 mg/L | (n = 235) | 638 ± 196 | ||
| NT-proBNP | <328.7 pg/mL | (n = 235) | 588 ± 177 | 0.017 |
| ≥328.7 pg/mL | (n = 235) | 630 ± 198 | ||
| UACR | <300 mg/g | (n = 453) | 609 ± 191 | 0.778 |
| ≥300 mg/g | (n = 17) | 622 ± 133 | ||
| Use of statins | No | (n = 286) | 605 ± 189 | 0.543 |
| Yes | (n = 184) | 616 ± 189 | ||
| Use of antihypertensive drugs | No | (n = 60) | 627 ± 204 | 0.426 |
| Yes | (n = 410) | 606 ± 187 | ||
| Use of antiplatelet drugs | No | (n = 23) | 597 ± 225 | 0.749 |
| Yes | (n = 447) | 610 ± 187 |
| Crude | Multivariable | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p | |
| Low DKK-1 without CAD | 1.000 | 1.000 | 1.000 | ||||||
| High DKK-1 without CAD | 8.185 | (1.036, 64.690) | 0.046 | 6.803 | (0.857, 53.971) | 0.070 | 7.370 | (0.899, 60.408) | 0.063 |
| Low DKK-1 with CAD | 8.622 | (1.121, 66.313) | 0.038 | 7.044 | (0.913, 54.358) | 0.061 | 6.291 | (0.760, 52.056) | 0.088 |
| High DKK-1 with CAD | 16.644 | (2.257, 122.719) | 0.006 | 12.100 | (1.623, 90.182) | 0.015 | 10.640 | (1.350, 83.874) | 0.025 |
| Framingham Risk Score | 1.098 | (1.030, 1.170) | 0.004 | ||||||
| Age (≥60 years) | 3.258 | (1.525, 6.960) | 0.002 | ||||||
| Male | 1.268 | (0.497, 3.235) | 0.619 | ||||||
| Current smoker | 1.052 | (0.544, 2.033) | 0.881 | ||||||
| Hypertension | 1.191 | (0.277, 5.125) | 0.815 | ||||||
| HOMA IR index ≥2 | 1.164 | (0.616,2.199) | 0.640 | ||||||
| Total cholesterol ≥4.14 mmol/L | 0.805 | (0.425, 1.528) | 0.508 | ||||||
| Low HDL cholesterol * | 2.095 | (1.110, 3.955) | 0.022 | ||||||
| Triglycerides ≥1.7 mmol/L | 0.728 | (0.368, 1.439) | 0.361 | ||||||
| eGFR < 60 mL/min/1.73 m2 | 1.389 | (0.719, 2.687) | 0.328 | ||||||
| Platelet ≥ 203 (109/L) | 1.149 | (0.617, 2.141) | 0.662 | ||||||
| C-reactive protein ≥ 1.393 mg/L | 1.773 | (0.932, 3.374) | 0.081 | ||||||
| NT-proBNP ≥ 328.7 pg/mL | 1.871 | (0.560, 6.254) | 0.309 | ||||||
| UACR ≥ 300 mg/g | 1.547 | (0.771, 3.104) | 0.219 | ||||||
| Use of statins | 1.181 | (0.634, 2.201) | 0.601 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.-H.; Wu, M.-H.; Lee, W.-J.; Lee, I.-T. A Synergistic Effect between Plasma Dickkopf-1 and Obstructive Coronary Artery Disease on the Prediction of Major Adverse Cardiac Events in Patients with Angina: An Observational Study. Biomolecules 2022, 12, 1408. https://doi.org/10.3390/biom12101408
Li Y-H, Wu M-H, Lee W-J, Lee I-T. A Synergistic Effect between Plasma Dickkopf-1 and Obstructive Coronary Artery Disease on the Prediction of Major Adverse Cardiac Events in Patients with Angina: An Observational Study. Biomolecules. 2022; 12(10):1408. https://doi.org/10.3390/biom12101408
Chicago/Turabian StyleLi, Yu-Hsuan, Min-Huan Wu, Wen-Jane Lee, and I-Te Lee. 2022. "A Synergistic Effect between Plasma Dickkopf-1 and Obstructive Coronary Artery Disease on the Prediction of Major Adverse Cardiac Events in Patients with Angina: An Observational Study" Biomolecules 12, no. 10: 1408. https://doi.org/10.3390/biom12101408
APA StyleLi, Y.-H., Wu, M.-H., Lee, W.-J., & Lee, I.-T. (2022). A Synergistic Effect between Plasma Dickkopf-1 and Obstructive Coronary Artery Disease on the Prediction of Major Adverse Cardiac Events in Patients with Angina: An Observational Study. Biomolecules, 12(10), 1408. https://doi.org/10.3390/biom12101408






