Quantitative Assessment of 3D Printed Model Accuracy in Delineating Congenital Heart Disease
Abstract
1. Introduction
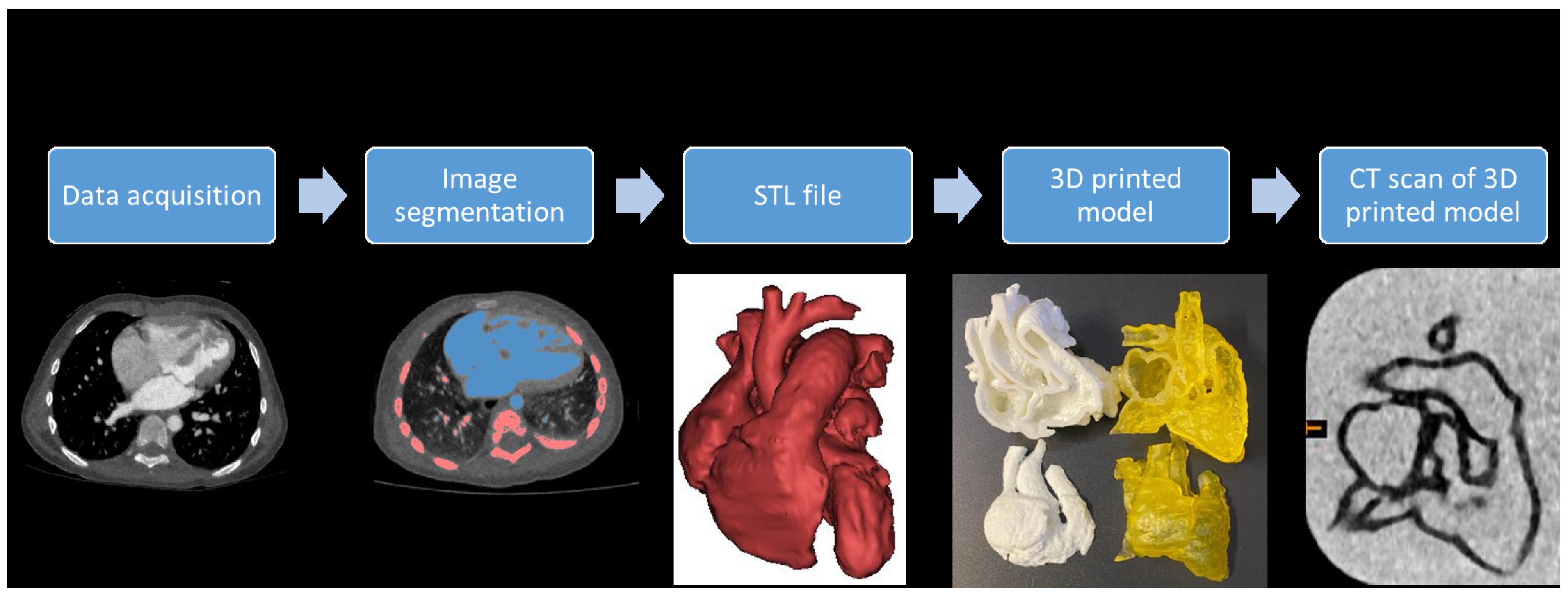
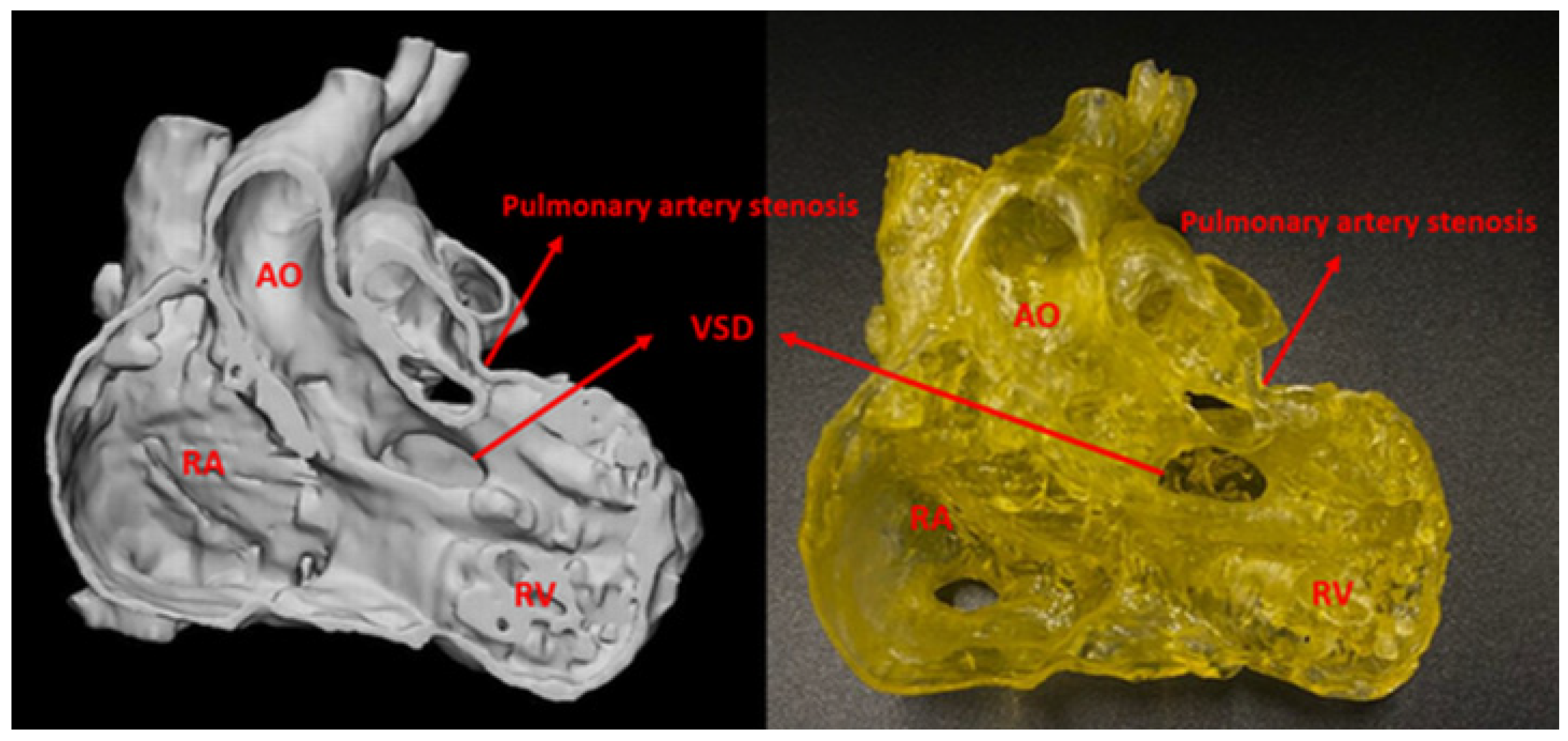
2. Materials and Methods
2.1. CT Data Collection
2.2. Image Segmentation and Post-Processing
2.3. 3D Printing of Heart Models
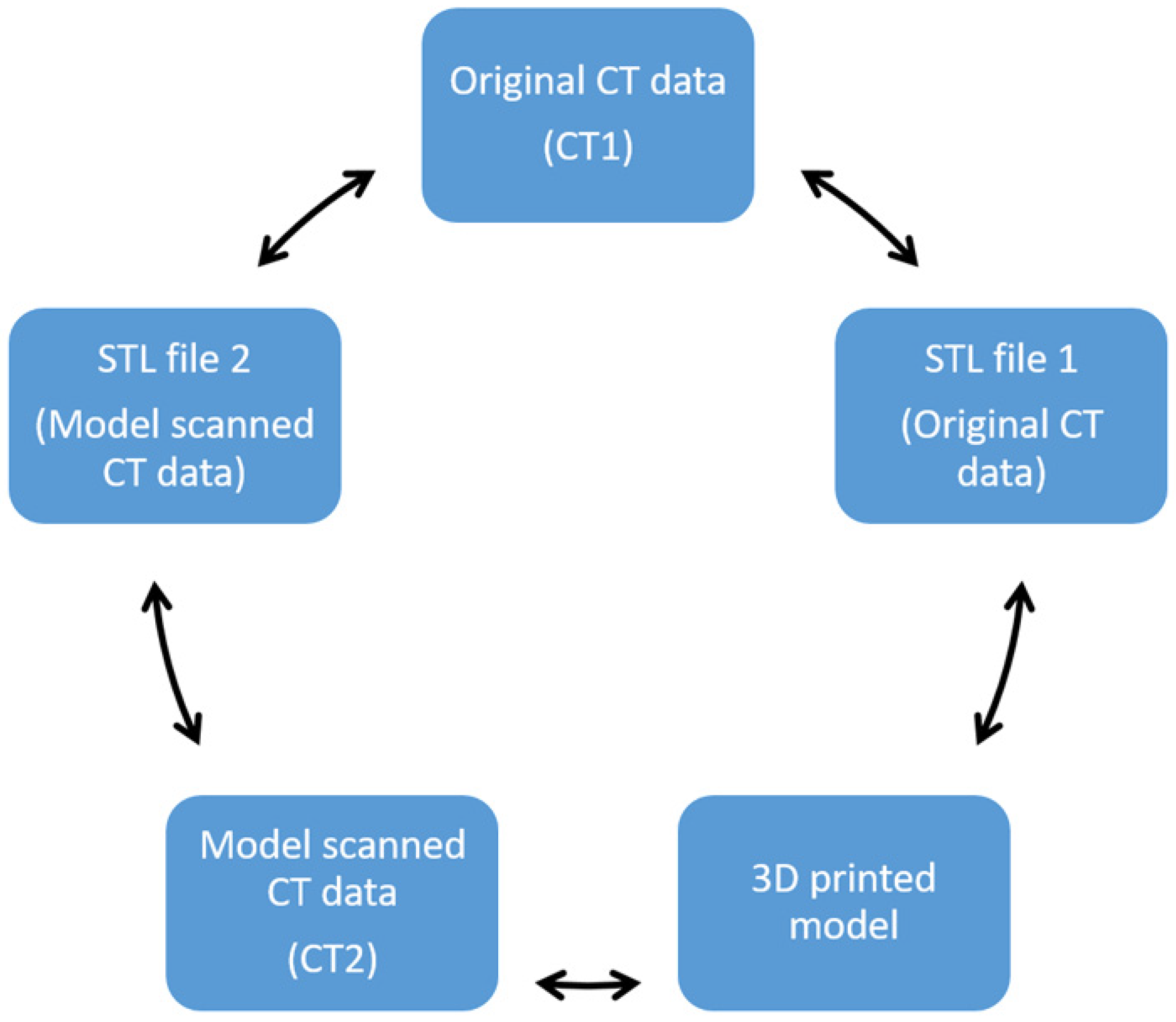
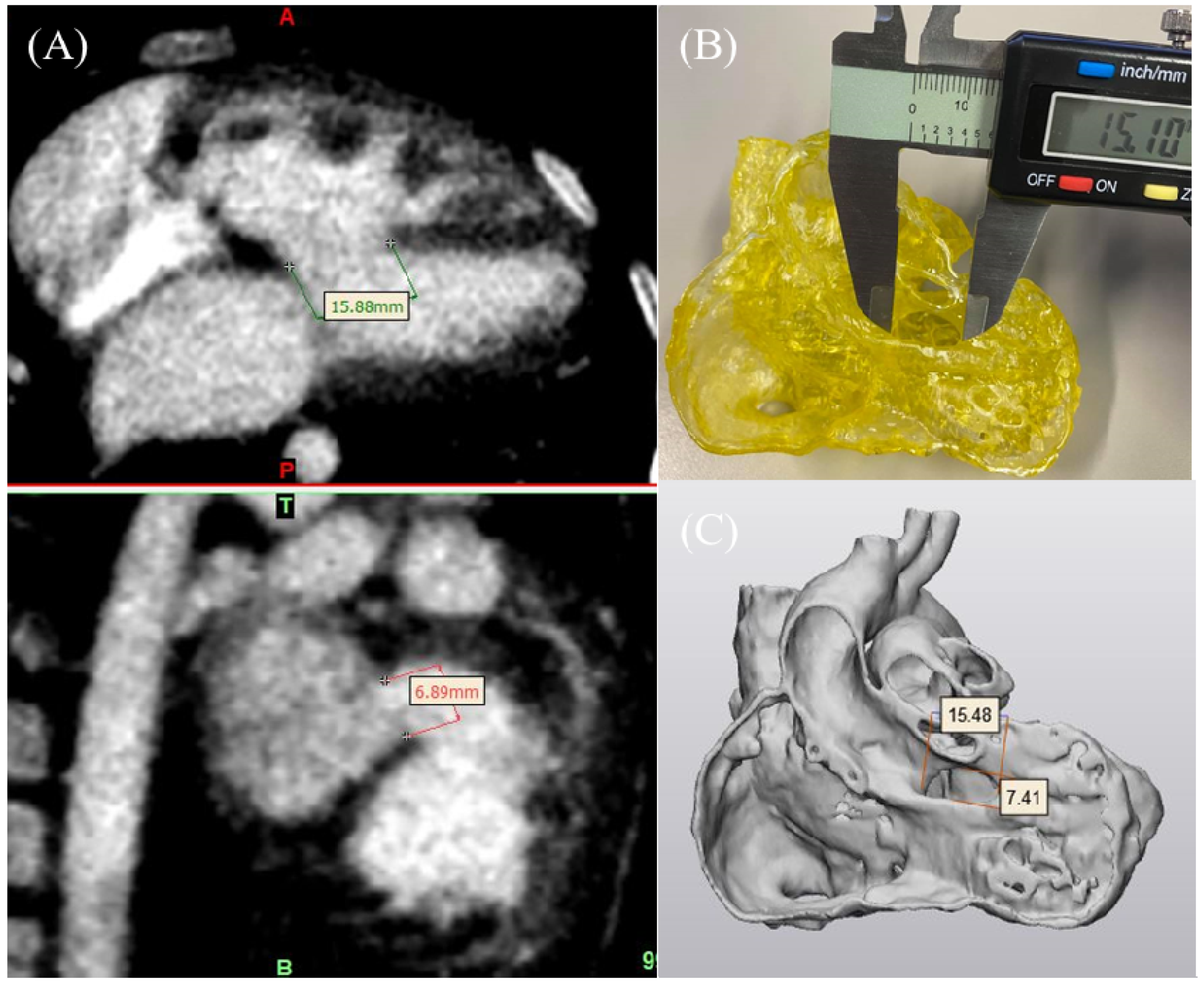
2.4. 3D Model Accuracy Assessment
2.5. Statistical Analysis
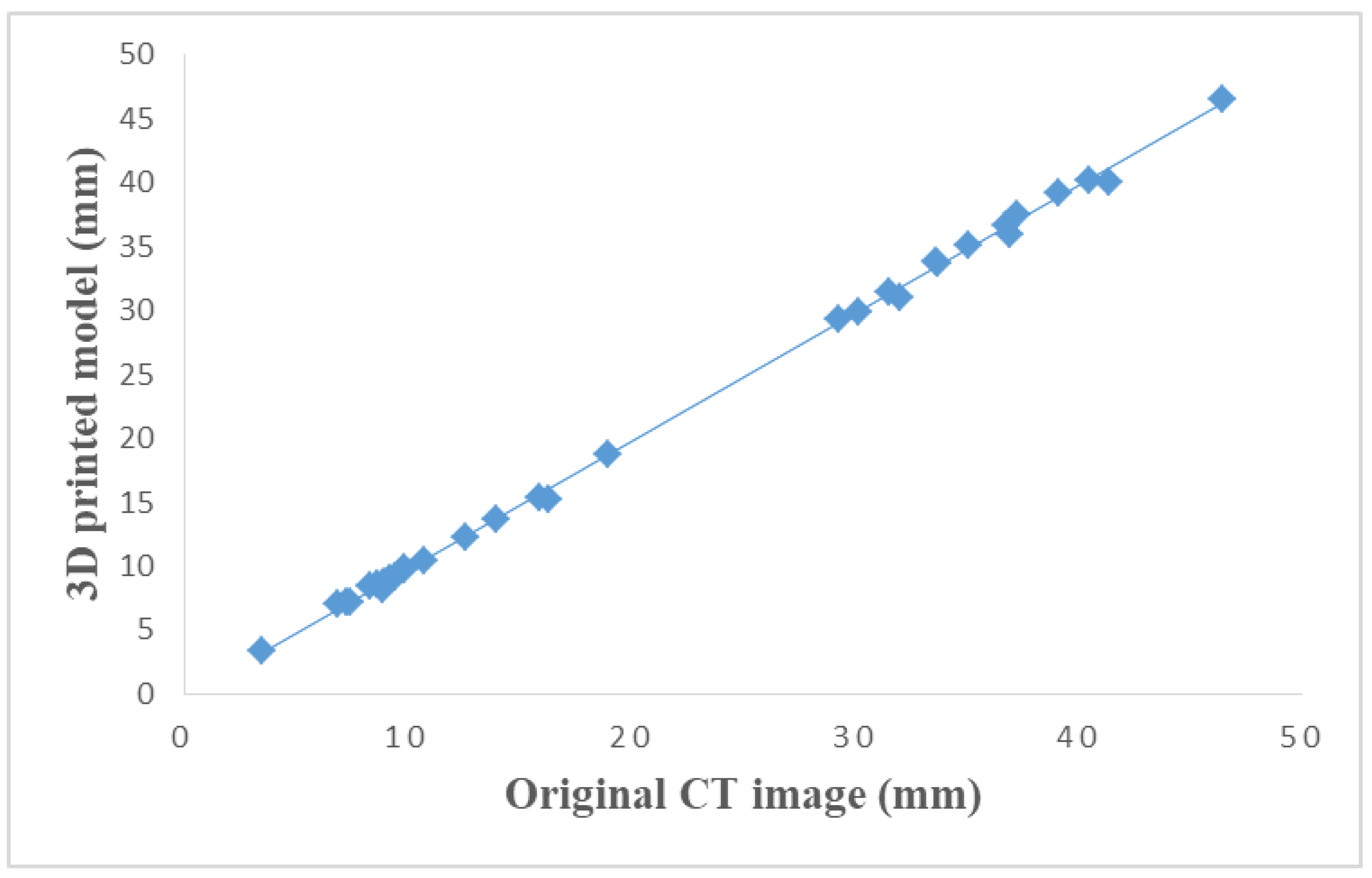
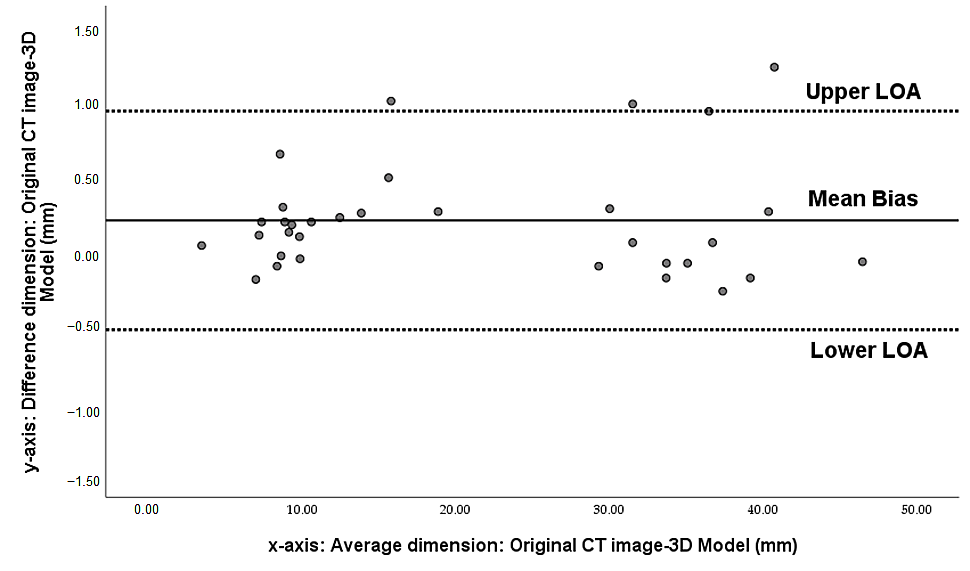
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zimmerman, M.S.; Smith, A.G.C.; Sable, C.A.; Echko, M.M.; Wilner, L.B.; Olsen, H.E.; Atalay, H.T.; Awasthi, A.; Bhutta, Z.A.; Boucher, J.L. Global, regional, and national burden of congenital heart disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Child Adolesc. Health 2020, 4, 185–200. [Google Scholar] [CrossRef]
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R. Heart disease and stroke Statistics-2019 update a report from the American Heart Association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef] [PubMed]
- Bhatla, P.; Tretter, J.T.; Ludomirsky, A.; Argilla, M.; Latson, L.A.; Chakravarti, S.; Barker, P.C.; Yoo, S.-J.; McElhinney, D.B.; Wake, N. Utility and scope of rapid prototyping in patients with complex muscular ventricular septal defects or double-outlet right ventricle: Does it alter management decisions? Pediatr. Cardiol. 2017, 38, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Schmauss, D.; Haeberle, S.; Hagl, C.; Sodian, R. Three-dimensional printing in cardiac surgery and interventional cardiology: A single-centre experience. Eur. J. Cardiothorac. Surg. 2015, 47, 1044–1052. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z. 3D printing in medicine: Current applications and future directions. Quant. Imaging Med. Surg. 2018, 8, 1069–1077. [Google Scholar] [CrossRef]
- Sun, Z. Clinical applications of patient-specific 3D printed models in cardiovascular disease: Current status and clinical applications. Biomolecules 2020, 10, 1577. [Google Scholar] [CrossRef]
- Sun, Z. Insights into 3D printing in medical applications. Quant. Imaging Med. Surg. 2019, 9, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Jones, T.W.; Seckeler, M.D. Use of 3D models of vascular rings and slings to improve resident education. Congenit. Heart Dis. 2017, 12, 578–582. [Google Scholar] [CrossRef] [PubMed]
- Smerling, J.; Marboe, C.C.; Lefkowitch, J.H.; Pavlicova, M.; Bacha, E.; Einstein, A.J.; Naka, Y.; Glickstein, J.; Farooqi, K.M. Utility of 3D printed cardiac models for medical student education in congenital heart disease: Across a Spectrum of disease severity. Pediatr. Cardiol. 2019, 40, 1258–1265. [Google Scholar] [CrossRef]
- White, S.C.; Sedler, J.; Jones, T.W.; Seckeler, M. Utility of three-dimensional models in resident education on simple and complex intracardiac congenital heart defects. Congenit. Heart Dis. 2018, 13, 1045–1049. [Google Scholar] [CrossRef] [PubMed]
- Biglino, G.; Koniordou, D.; Gasparini, M.; Capelli, C.; Leaver, L.-K.; Khambadkone, S.; Schievano, S.; Taylor, A.M.; Wray, J. Piloting the use of patient-specific cardiac models as a novel tool to facilitate communication during clinical consultations. Pediatr. Cardiol. 2017, 38, 813–818. [Google Scholar] [CrossRef]
- Valverde, I.; Gomez-Ciriza, G.; Hussain, T.; Suarez-Mejias, C.; Velasco-Forte, M.N.; Byrne, N.; Ordoñez, A.; Gonzalez-Calle, A.; Anderson, D.; Hazekamp, M.G. Three-dimensional printed models for surgical planning of complex congenital heart defects: An international multicentre study. Eur. J. Cardiothorac. Surg. 2017, 52, 1139–1148. [Google Scholar] [CrossRef] [PubMed]
- Biglino, G.; Capelli, C.; Koniordou, D.; Robertshaw, D.; Leaver, L.K.; Schievano, S.; Taylor, A.M.; Wray, J. Use of 3D models of congenital heart disease as an education tool for cardiac nurses. Congenit. Heart Dis. 2017, 12, 113–118. [Google Scholar] [CrossRef]
- Kappanayil, M.; Koneti, N.R.; Kannan, R.R.; Kottayil, B.P.; Kumar, K. Three-dimensional-printed cardiac prototypes aid surgical decision-making and preoperative planning in selected cases of complex congenital heart diseases: Early experience and proof of concept in a resource-limited environment. Ann. Pediatr. Cardiol. 2017, 10, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Kiraly, L.; Tofeig, M.; Jha, N.K.; Talo, H. Three-dimensional printed prototypes refine the anatomy of post-modified Norwood-1 complex aortic arch obstruction and allow presurgical simulation of the repair. Interact. Cardiovasc. Thorac. Surg. 2016, 22, 238–240. [Google Scholar] [CrossRef]
- Vukicevic, M.; Mosadegh, B.; Min, J.K.; Little, S.H. Cardiac 3D printing and its future directions. JACC Cardiovasc. Imaging 2017, 10, 171–184. [Google Scholar] [CrossRef]
- Loke, Y.-H.; Harahsheh, A.S.; Krieger, A.; Olivieri, L.J. Usage of 3D models of tetralogy of Fallot for medical education: Impact on learning congenital heart disease. BMC Med. Educ. 2017, 17, 54. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.; McGuinness, J.; O’Reilly, M.; Nolke, L.; Murray, J.; Jones, J. The role of 3D printing in preoperative planning for heart transplantation in complex congenital heart disease. Ir. J. Med. Sci. 2017, 186, 753–756. [Google Scholar] [CrossRef]
- Farooqi, K.M.; Gonzalez-Lengua, C.; Shenoy, R.; Sanz, J.; Nguyen, K. Use of a three dimensional printed cardiac model to assess suitability for biventricular repair. World J. Pediatr. Congenit. Heart Surg. 2016, 7, 414–416. [Google Scholar] [CrossRef]
- Shiraishi, I.; Yamagishi, M.; Hamaoka, K.; Fukuzawa, M.; Yagihara, T. Simulative operation on congenital heart disease using rubber-like urethane stereolithographic biomodels based on 3D datasets of multislice computed tomography. Eur. J. Cardiothorac. Surg. 2010, 37, 302–306. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Lau, I.; Wong, Y.H.; Yeong, C.H. Personalized three-dimensional printed models in congenital heart disease. J. Clin. Med. 2019, 8, 522. [Google Scholar] [CrossRef] [PubMed]
- Lau, I.W.W.; Sun, Z. Dimensional accuracy and clinical value of 3D printed models in congenital heart disease: A systematic review and meta-analysis. J. Clin. Med. 2019, 8, 1483. [Google Scholar] [CrossRef] [PubMed]
- Olejník, P.; Nosal, M.; Havran, T.; Furdova, A.; Cizmar, M.; Slabej, M.; Thurzo, A.; Vitovic, P.; Klvac, M.; Acel, T. Utilisation of three-dimensional printed heart models for operative planning of complex congenital heart defects. Kardiol. Pol. 2017, 75, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Olivieri, L.J.; Krieger, A.; Loke, Y.-H.; Nath, D.S.; Kim, P.C.; Sable, C.A. Three-dimensional printing of intracardiac defects from three-dimensional echocardiographic images: Feasibility and relative accuracy. J. Am. Soc. Echocardiogr. 2015, 28, 392–397. [Google Scholar] [CrossRef]
- Lau, I.W.W.; Liu, D.; Xu, L.; Fan, Z.; Sun, Z. Clinical value of patient-specific three-dimensional printing of congenital heart disease: Quantitative and qualitative assessments. PLoS ONE 2018, 13, e0194333. [Google Scholar] [CrossRef]
- Mowers, K.L.; Fullerton, J.B.; Hicks, D.; Singh, G.K.; Johnson, M.C.; Anwar, S. 3D echocardiography provides highly accurate 3D printed models in congenital heart disease. Pediatr. Cardiol. 2021, 42, 131–141. [Google Scholar] [CrossRef]
- Zhao, L.; Zhou, S.; Fan, T.; Li, B.; Liang, W.; Dong, H. Three-dimensional printing enhances preparation for repair of double outlet right ventricular surgery. J. Card. Surg. 2018, 33, 24–27. [Google Scholar] [CrossRef]
- Parimi, M.; Buelter, J.; Thanugundla, V.; Condoor, S.; Parkar, N.; Danon, S.; King, W. Feasibility and validity of printing 3D heart models from rotational angiography. Pediatr. Cardiol. 2018, 39, 653–658. [Google Scholar] [CrossRef]
- Huang, J.; Shi, H.; Chen, Q.; Hu, J.; Zhang, Y.; Song, H.; Zhou, Q. Three-dimensional printed model fabrication and effectiveness evaluation in fetuses with congenital heart disease or with a normal heart. J. Ultrasound Med. 2021, 40, 15–28. [Google Scholar] [CrossRef]
- Ma, X.; Tao, L.; Chen, X.; Li, W.; Peng, Z.; Chen, Y.; Jin, J.; Zhang, X.; Xiong, Q.; Zhong, Z. Clinical application of three-dimensional reconstruction and rapid prototyping technology of multislice spiral computed tomography angiography for the repair of ventricular septal defect of tetralogy of Fallot. Genet. Mol. Res. 2015, 14, 1301–1309. [Google Scholar] [CrossRef]
- Illmann, C.F.; Ghadiry-Tavi, R.; Hosking, M.; Harris, K.C. Utility of 3D printed cardiac models in congenital heart disease: A scoping review. Heart 2020, 106, 1631–1637. [Google Scholar] [CrossRef]
- Lau, I.; Sun, Z. Three-dimensional printing in congenital heart disease: A systematic review. J. Med. Radiat. Sci. 2018, 65, 226–236. [Google Scholar] [CrossRef]
- Batteux, C.; Haidar, M.A.; Bonnet, D. 3D-printed models for surgical planning in complex congenital heart diseases: A systematic review. Front. Pediatr. 2019, 7, 23. [Google Scholar] [CrossRef] [PubMed]
- Lau, I.; Squelch, A.; Wan, Y.L.; Wong, A.M.C.; Ducke, W.; Sun, Z. Patient-specific 3D printed model in delineating brain glioma and surrounding structures in a pediatric patient. Digit. Med. 2017, 3, 86–92. [Google Scholar]
- Ogden, K.M.; Aslan, C.; Ordway, N.; Diallo, D.; Tillapaugh-Fay, G.; Soman, P. Factors affecting dimensional accuracy of 3-D printed anatomical structures derived from CT data. J. Digit. Imaging 2015, 28, 654–663. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, V.; Rodrigues, N.; Ribeiro, R.; Costa, P.F.; Lima, R.A.; Teixeira, S.F.C.F. 3D printed biomodels for flow visualiszation in stenotic vessels: An experimental and numerical study. Micromachines 2020, 11, 549. [Google Scholar] [CrossRef] [PubMed]
| Anatomical Locations | |
|---|---|
| 1 | Right atrium |
| 2 | Right ventricle |
| 3 | Left atrium |
| 4 | Left ventricle |
| 5 | Aortic arch |
| 6 | Ascending aorta |
| 7 | Descending aorta |
| 8 | Pulmonary trunk |
| 9 | Superior vena cava |
| 10 | Ventricular septal defect |
| Comparison | Difference (mm) (mean ± SD) | Percentage Difference (%) |
|---|---|---|
| CT1 vs. STL1 | 0.12 ± 0.23 | 0.5 ± 1.06 |
| STL1 vs. 3D model | 0.1 ± 0.28 | 0.4 ± 1.32 |
| 3D model vs. CT2 | −0.11 ± 0.47 | 0.5 ± 2.24 |
| CT2 vs. STL2 | 0.12 ± 0.25 | 0.6 ± 1.18 |
| STL2 vs. CT1 | −0.23 ± 0.47 | 0.9 ± 2.24 |
| CT1 vs. 3D model | 0.21 ± 0.37 | 0.9 ± 1.7 |
| CT1 vs. CT2 | 0.1 ± 0.40 | 0.5 ± 1.8 |
| STL1 vs. CT2 | −0.12 ± 0.42 | 0.5 ± 1.9 |
| STL1 vs. STL2 | 0.1 ± 0.45 | 0.4 ± 2.13 |
| 3D model vs. STL2 | 0.17 ± 0.48 | 0.8 ± 2.28 |
| Studies Reporting Accuracy | No. of Models Printed | Comparisons | Mean Difference (mm) | Analysis Method |
|---|---|---|---|---|
| Valverde et al. [12] | 20 | 3D model vs. CT/MRI | 0.27 ± 0.73 mm | Pearson |
| Olejník et al. [23] | 8 | 3D model vs. DICOM | 0.19 ± 0.38 mm | Bland–Altman |
| 3D model vs. vivo | 0.13 ± 0.26 mm | |||
| Olivieri et al. [24] | 9 | 3D model vs. Echo | 0.4 ± 0.9 mm | Pearson/Bland–Altman |
| Lau et al. [25] | 1 | 3D model vs. CT | 0.23 mm | Pearson |
| Mowers et al. [26] | 5 | 2D echo vs. digital 3D | 0 mm | Pearson/Bland–Altman |
| 2D echo vs. 3D model | 0.3 mm | |||
| Our study | 3 | 3D model vs. original CT/CT of 3D model | 0.21 ± 0.37/ −0.11 ± 0.47 mm 0.1 ± 0.28/0.17 ± 0.48 mm 0.12 ± 0.23/0.12 ± 0.25 mm | Pearson/Bland–Altman |
| 3D model vs. STL files | ||||
| CT images vs. STL files |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.; Squelch, A.; Sun, Z. Quantitative Assessment of 3D Printed Model Accuracy in Delineating Congenital Heart Disease. Biomolecules 2021, 11, 270. https://doi.org/10.3390/biom11020270
Lee S, Squelch A, Sun Z. Quantitative Assessment of 3D Printed Model Accuracy in Delineating Congenital Heart Disease. Biomolecules. 2021; 11(2):270. https://doi.org/10.3390/biom11020270
Chicago/Turabian StyleLee, Shenyuan, Andrew Squelch, and Zhonghua Sun. 2021. "Quantitative Assessment of 3D Printed Model Accuracy in Delineating Congenital Heart Disease" Biomolecules 11, no. 2: 270. https://doi.org/10.3390/biom11020270
APA StyleLee, S., Squelch, A., & Sun, Z. (2021). Quantitative Assessment of 3D Printed Model Accuracy in Delineating Congenital Heart Disease. Biomolecules, 11(2), 270. https://doi.org/10.3390/biom11020270







