Salivary Osteocalcin as Potential Diagnostic Marker of Periodontal Bone Destruction among Smokers
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sampling Strategy
2.2. Collection of Salivary Samples For Estimation of Bone Biomarkers
2.3. Periodontal Clinical Examination
2.4. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Offenbacher, S. Periodontal diseases: Pathogenesis. Ann. Periodontol. 1996, 1, 821–878. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Alibrandi, A.; Indelicato, F.; Ferlito, S. Analysis of Endothelin-1 Concentrations in Individuals with Periodontitis. Sci. Rep. 2020, 10, 1652. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Muraglie, S.; Leonardi, R.; Lo Giudice, A. Assessment of Vitamin C and Antioxidant Profiles in Saliva and Serum in Patients with Periodontitis and Ischemic Heart Disease. Nutrients 2019, 11, 2956. [Google Scholar] [CrossRef] [PubMed]
- Barbato, L.; Francioni, E.; Bianchi, M.; Mascitelli, E.; Marco, L.B.; Tonelli, D.P. Periodontitis and bone metabolism. Clin. Cases Miner. Bone Metab. 2015, 12, 174. [Google Scholar] [CrossRef] [PubMed]
- Delmas, P.D. Bone marker nomenclature. Bone 2001, 28, 575–576. [Google Scholar] [CrossRef]
- Tatullo, M.; Codispoti, B.; Pacifici, A.; Palmieri, F.; Marrelli, M.; Pacifici, L.; Paduano, F. Potential use of human periapical cyst-mesenchymal stem cells (hpcy-mscs) as a novel stem cell source for regenerative medicine applications. Front. Cell. Dev. Biol. 2017, 5, 103. [Google Scholar] [CrossRef]
- Kerativitayanan, P.; Tatullo, M.; Khariton, M.; Joshi, P.; Perniconi, B.; Gaharwar, A.K. Nanoengineered Osteoinductive and Elastomeric Scaffolds for Bone Tissue Engineering. ACS Biomater. Sci. Eng. 2017, 3, 590–600. [Google Scholar] [CrossRef]
- Barry, M.; Pearce, H.; Cross, L.; Tatullo, M.; Gaharwar, A.K. Advances in Nanotechnology for the Treatment of Osteoporosis. Curr. Osteoporos Rep. 2016, 14, 87–94. [Google Scholar] [CrossRef]
- Scannapieco, F.A.; Ng, P.B.Y.; Hovey, K.; Hausmann, E.; Hutson, A.; WactawskiWende, J. Salivary biomarkers associated with alveolar bone loss. Ann. NY Acad. Sci. 2007, 1098, 496–497. [Google Scholar] [CrossRef]
- Gürsoy, U.K.; Könönen, E.; Tervahartiala, T.; Gürsoy, M.; Pitkänen, J.; Torvi, P.; Suominen, A.L.; Pussinen, P.; Sorsa, T. Molecular forms and fragments of salivary MMP8 in relation to periodontitis. J. Clin. Periodontol. 2018, 45, 1421–1428. [Google Scholar] [CrossRef]
- Gursoy, U.K.; Könönen, E.; Huumonen, S.; Tervahartiala, T.; Pussinen, P.J.; Suominen, A.L.; Sorsa, T. Salivary type I collagen degradation end-products and related matrix metalloproteinases in periodontitis. J. Clin. Periodontol. 2013, 40, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Betsy, J.; Ahmed, J.M.; Mohasin, A.K.; Mohammed, A.; AlQahtani, N.A. Diagnostic accuracy of salivary biomarkers of bone turnover in identifying patients with periodontitis in a Saudi Arabian population. J. Dent. Sci. 2019, 40, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Karsdal, M.A.; Genovese, F.; Madsen, E.A.; Manon-Jensen, T.; Schuppan, D. Collagen and tissue turnover as a function of age: Implications for fibrosis. J. Hepatol. 2016, 64, 103–109. [Google Scholar] [CrossRef]
- Frodge, B.D.; Ebersole, J.L.; Kryscio, R.J.; Thomas, M.V.; Miller, C.S. Bone remodeling biomarkers of periodontal disease in saliva. J. Periodontol. 2008, 79, 1913–1919. [Google Scholar] [CrossRef] [PubMed]
- Miricescu, D.; Totan, A.; Calenic, B.; Mocanu, B.; Didilescu, A.; Mohora, M.; Spinu, T.; Greabu, M. Salivary biomarkers: Relationship between oxidative stress and alveolar bone loss in chronic periodontitis. Acta Odontol. Scand. 2014, 72, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Zoch, M.L.; Clemens, T.L.; Riddle, R.C. New insights into the biology of osteocalcin. Bone 2016, 82, 42–49. [Google Scholar] [CrossRef]
- Giannobile, W.V.; Beikler, T.; Kinney, J.S.; Ramseier, C.A.; Morelli, T.; Wong, D.T. Saliva as a diagnostic tool for periodontal disease: Current state and future directions. Periodontol. 2000 2009, 50, 52–64. [Google Scholar] [CrossRef]
- Cakal, O.T.; Efeoglu, C.; Bozkurt, E. The evaluation of peri-implant sulcus fluid osteocalcin, osteopontin, and osteonectin levels in peri-implant diseases. J. Periodontol. 2018, 89, 418–423. [Google Scholar] [CrossRef]
- Payne, J.B.; Stoner, J.A.; Lee, H.M.; Nummikoski, P.V.; Reinhardt, R.A.; Golub, L.M. Serum bone biomarkers and oral/systemic bone loss in humans. J. Dent. Res. 2011, 90, 747–751. [Google Scholar] [CrossRef]
- Rosset, E.M.; Trombetta-eSilva, J.; Hepfer, G.; Yao, H.; Bradshaw, A.D. SPARC and the N-propeptide of collagen I influence fibroblast proliferation and collagen assembly in the periodontal ligament. PLoS ONE 2017, 12, e0173209. [Google Scholar] [CrossRef]
- Ram, V.S.; Parthiban, U.S.; Mithradas, N.; Prabhakar, R. Bone biomarkers in periodontal disease: A review article. J. Clin. Diagn. Res. 2015, 9, ZE07. [Google Scholar] [PubMed]
- Ng, P.Y.; Donley, M.; Hausmann, E.; Hutson, A.D.; Rossomando, E.F.; Scannapieco, F.A. Candidate salivary biomarkers associated with alveolar bone loss: Cross-sectional and in vitro studies. FEMS Immunol. Med. Microbiol. 2007, 49, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Moradi-Lakeh, M.; El Bcheraoui, C.; Tuffaha, M.; Daoud, F.; Al Saeedi, M.; Basulaiman, M.; Memish, Z.A.; AlMazroa, M.A.; Rabeeah, A.A.; Mokdad, A.H. Tobacco consumption in the Kingdom of Saudi Arabia, 2013: Findings from a national survey. BMC Public Health. 2015, 15, 611. [Google Scholar] [CrossRef]
- Algabbani, A.M.; Almubark, R.; Althumiri, N.; Alqahtani, A.; BinDhim, N. The Prevalence of Cigarette Smoking in Saudi Arabia in 2018. Food Drug Regul. Sci. J. 2018, 1, 1–4. [Google Scholar] [CrossRef]
- Tatullo, M.; Marrelli, M.; Scacco, S.; Lorusso, M.; Doria, S.; Sabatini, R.; Auteri, P.; Cagiano, R.; Inchingolo, F. Relationship between oxidative stress and “burning mouth syndrome” in female patients: A scientific hypothesis. Eur. Rev. Med. Pharmacol. Sci. 2012, 16, 1218–1221. [Google Scholar]
- Caton, J.; Armitage, G.; Berglundh, T.; Chapple, I.L.; Jepsen, S.; Kornman, K.S.; Mealey, B.L.; Papapanou, P.N.; Sanz, M.; Tonetti, M.S. A new classification scheme for periodontal and peri-implant diseases and conditions–Introduction and key changes from the 1999 classification. J. Periodontol. 2018, 89, S1–S8. [Google Scholar] [CrossRef] [PubMed]
- Colby, S.M.; Clark, M.A.; Rogers, M.L.; Ramsey, S.; Graham, A.L.; Boergers, J.; Kahler, C.W.; Papandonatos, G.D.; Buka, S.L.; Niaura, R.S.; et al. Development and reliability of the lifetime interview on smoking trajectories. Nicotine Tob. Res. 2011, 14, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Navazesh, M.; Kumar, S.K. Measuring salivary flow: Challenges and opportunities. J. Am. Dent. Assoc. 2008, 139, 35S–40S. [Google Scholar] [CrossRef]
- Papapanou, P.N.; Sanz, M.; Buduneli, N.; Dietrich, T.; Feres, M.; Fine, D.H.; Flemmig, T.F.; Garcia, R.; Giannobile, W.V.; Graziani, F.; et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89, 173–182. [Google Scholar] [CrossRef]
- Chapple, I.L.; Mealey, B.L.; Van Dyke, T.E.; Bartold, P.M.; Dommisch, H.; Eickholz, P.; Geisinger, M.L.; Genco, R.J.; Glogauer, M.; Goldstein, M.; et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45, 68–77. [Google Scholar] [CrossRef]
- Habibzadeh, F.; Habibzadeh, P.; Yadollahie, M. On determining the most appropriate test cut-off value: The case of tests with continuous results. Biochem. Med.: Biochem. Med. 2016, 26, 297–307. [Google Scholar] [CrossRef] [PubMed]
- Özçaka, O.; Nalbantsoy, A.; Buduneli, N. Salivary osteocalcin levels are decreased in smoker chronic periodontitis patients. Oral Dis. 2011, 17, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Gürlek, Ö.; Lappin, D.F.; Buduneli, N. Effects of smoking on salivary C-telopeptide pyridinoline cross-links of type I collagen and osteocalcin levels. Arch. Oral Biol. 2009, 54, 1099–1104. [Google Scholar] [CrossRef] [PubMed]
- Petrušić, N.; Posavac, M.; Sabol, I.; Mravak-Stipetić, M. The effect of tobacco smoking on salivation. Acta Stomatol. Croatica. 2015, 49, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.; Ingle, N.A.; Kaur, N.; Yadav, P.; Ingle, E. Effect of long-term smoking on salivary flow rate and salivary pH. J. Indian Assoc. Public Health Dent. 2015, 13, 11–13. [Google Scholar] [CrossRef]
- Chang, C.H.; Han, M.L.; Teng, N.C.; Lee, C.Y.; Huang, W.T.; Lin, C.T.; Huang, Y.K. Cigarette Smoking Aggravates the Activity of Periodontal Disease by Disrupting Redox Homeostasis-An Observational Study. Sci. Rep. 2018, 8, 11055. [Google Scholar] [CrossRef]
- Stanescu, I.I.; Totan, A.; Rus, F.; Miricescu, D.; Mocanu, B.; Calenic, B.; Greabu, M. Salivary Diagnosis-Clinical Uses in Assessing Oral Inflammation. Rev. Chim. 2017, 68, 1201–1204. [Google Scholar] [CrossRef]
- Kinney, J.S.; Morelli, T.; Braun, T.; Ramseier, C.A.; Herr, A.E.; Sugai, J.V.; Shelburne, C.E.; Rayburn, L.A.; Singh, A.K.; Giannobile, W.V. Saliva/pathogen biomarker signatures and periodontal disease progression. J. Dent. Res. 2011, 90, 752–758. [Google Scholar] [CrossRef]
- Delany, A.M.; Hankenson, K.D. Thrombospondin-2 and SPARC/osteonectin are critical regulators of bone remodelling. J. Cell. Commun. Signal. 2009, 3, 227–238. [Google Scholar] [CrossRef]
- Laroche, M.; Lasne, Y.; Felez, A.; Moulinier, L.; Bon, E.; Cantagrel, A.; Leophonte, P.; Mazières, B. Osteocalcin and smoking. Rev. du Rhum. 1994, 61, 433–436. [Google Scholar]
- AL-Bashaireh, A.M.; Haddad, L.G.; Weaver, M.; Kelly, D.L.; Chengguo, X.; Yoon, S. The effect of tobacco smoking on musculoskeletal health: A systematic review. J. Environ. Res. Public Health 2018, 2018, 1–106. [Google Scholar] [CrossRef] [PubMed]
- De Campos, J.M.; Prati, A.J.; Cirano, F.R.; Pimentel, S.P.; Pastore, G.P.; Pecorari, V.G.; Ribeiro, F.V.; Casati, M.Z.; Casarin, R.C. Smoking modulates gene expression of type I collagen, bone sialoprotein, and osteocalcin in human alveolar bone. J. Oral Maxillofac. Surg. 2015, 73, 2123–2131. [Google Scholar] [CrossRef] [PubMed]
- Hogg, R.V.; Tanis, E.A.; Zimmerman, D.L. Probability and Statistical Inference; Pearson/Prentice Hall: Upper Saddle River, NJ, USA, 2010. [Google Scholar]
- Christie, J.J.; Osborne, R.H.; Kantor, S.; Nowson, C.A.; Seibel, M.J.; Wark, J.D. Mechanisms of bone loss in twins discordant for cigarette smoking. In Proceedings of the 2nd Joint Meeting of the International Bone & Mineral Society and the Australian & New Zealand Bone & Mineral Society, Sydney, NSW, Australia, 21–25 March 2009. [Google Scholar]
- Alqassem, M.Y.; SBFM, A. Risk factors for failure to quit cigarette smoking among male Saudi’s in Abha City. J. Med. Med. Sci. 2013, 1, 18–27. [Google Scholar]



| Variables | Group I (n = 30) | Group II (n = 30) | Group III (n = 30) | Total | p-Value | |
|---|---|---|---|---|---|---|
| Gender | Male | 18 (60.0) | 14 (46.7) | 22 (73.3) | 54 (60.0) | 0.11 ns |
| Female | 12 (40.0) | 16 (53.3) | 8 (26.7) | 36 (40.0) | ||
| Age | Mean ± SD | 32.70 ± 7.09 | 34.93 ± 7.31 | 35.13 ± 7.40 | - | 0.35 ns |
| Smoking Status | Absent | 30 | 30 | 0 | 60 (66.7) | 0.000 ** |
| Present | 0 | 0 | 30 | 30 (33.3) | ||
| Teeth Present | Mean ± SD | 28.93 ± 2.33 | 29.67±1.93 | 29.13 ± 2.08 | - | 0.38 ns |
| Oral Hygiene Tool | No oral hygiene | 7 (23.3) | 8 (26.7) | 12 (40.0) | 27 (30.0) | 0.429 ns |
| Toothbrush | 15 (50.0) | 16 (53.3) | 15 (50.0) | 46 (51.1) | ||
| Miswak twig | 8 (26.7) | 6 (20.0) | 3 (10.0) | 17 (18.9) | ||
| Frequency of Brushing | Once daily | 16 (53.3) | 16 (53.3) | 13 (43.3) | 45 (50.0) | 0.298 ns |
| Twice daily | 10 (33.3) | 7 (23.3) | 6 (20.0) | 23 (25.6) | ||
| Infrequent | 4 (13.3) | 7 (23.3) | 11 (36.7) | 22 (24.4) | ||
| Time Taken for Brushing | 0–1 min | 1 (3.3) | 0 | 2 (6.7) | 3 (3.3) | 0.637 ns |
| 1–2 min | 18 (60.0) | 23 (76.7) | 20 (66.7) | 61 (67.8) | ||
| 2–5 min | 11 (36.7) | 7 (23.3) | 8 (26.6) | 27 (28.9) | ||
| BOP | <10% | 30 (100.0) | 0 | 0 | 30 (33.33) | 0.000 ** |
| ≥10% | 0 | 30 (100.0) | 30 (100.0) | 60 (66.7) | ||
| PPD | <4.0 mm | 30 (100.0) | 0 | 0 | 30 (33.33) | 0.000 ** |
| ≥4.0 mm | 0 | 30 (100.0) | 30 (100.0) | 60 (66.7) | ||
| Bone Loss | <15% | 30 (100.0) | 0 | 0 | 30 (33.33) | 0.000 ** |
| ≥15% | 0 | 30 (100.0) | 30 (100.0) | 60 (66.7) |
| Variable | Periodontal Variables (Mean ± SD) | p Value | ||
|---|---|---|---|---|
| Group I | Group II | Group III | ||
| BOP | 7.20 ± 2.26 | 56.99 ± 18.44 | 64.02 ± 15.70 | 0.000 ¶ |
| PPD (mm) | 2.53 ± 0.62 | 5.2 ± 0.67 | 5.3 ± 0.84 | 0.000 ¶ |
| Bone Loss (mm) | 1.2 ± 0.61 | 3.9 ± 0.59 | 4.17 ± 0.68 | 0.000 ¶ |
| Bone Loss (%) | 9.65 ± 4.51 | 29.33 ± 6.9 | 31.69 ± 7.25 | 0.000 ¶ |
| Salivary Biomarkers of Bone Turnover (Mean ± SD) | ||||
| Group I | Group II | Group III | ||
| Osteocalcin (ng/mL) | 10.97 ± 5.80 | 24.99 ± 8.97 | 23.11 ± 8.63 | 0.000 ¶ |
| Osteonectin (ng/mL) | 59.47 ± 21.26 | 109 ± 20.48 | 82.53 ± 31.17 | 0.000 ¶ |
| CTX (ng/mL) | 21.08 ± 17.75 | 61.90 ± 11.57 | 39.21 ± 10.28 | 0.000 ¶ |
| Variable | BOP | PPD | Bone Loss | CTX | Osteocalcin | Osteonectin |
|---|---|---|---|---|---|---|
| Osteocalcin | 0.000 ¶ (0.60) | 0.001 € (0.40) | 0.000 ¶ (0.58) | 0.000 ¶ (0.51) | - | 0.000 ¶ (0.50) |
| Osteonectin | 0.010 * (0.46) | 0.012 * (0.32) | 0.000 € (0.38) | 0.000 € (0.48) | 0.000 ¶ (0.50) | - |
| CTX | 0.001 € (0.48) | 0.004 € (0.36) | 0.000 ¶ (0.51) | - | 0.000 ¶ (0.51) | 0.000 € (0.48) |
| Cut-off (ng/mL) | Se (%) | Sp (%) | AUC | 95% CI | P | YI | ||
|---|---|---|---|---|---|---|---|---|
| Healthy vs. Total Periodontitis (BOP: 10% BL: 15%; PPD: 4 mm) | CTX | 18.3 | 91.67 | 70.00 | 0.873 | 0.787–0.934 | 0.001 | 0.783 |
| 20.19 | 91.67 | 86.67 | ||||||
| 22.14 | 88.33 | 86.67 | ||||||
| OC | 9.21 | 100 | 56.67 | 0.871 | 0.783–0.932 | 0.001 | 0.667 | |
| 15.25 | 90.00 | 76.67 | ||||||
| 25.99 | 41.67 | 100.0 | ||||||
| ON | 55.0 | 93.33 | 53.33 | 0.833 | 0.739–0.903 | 0.001 | 0.667 | |
| 68.2 | 80.00 | 86.67 | ||||||
| 98.2 | 45.0 | 90.0 | ||||||
| Cut-off (ng/mL) | Se (%) | Sp (%) | AUC | 95% CI | P | YI | ||
|---|---|---|---|---|---|---|---|---|
| Healthy vs. Periodontitis (BOP: 10% BL: 15%; PPD: 4 mm) | CTX | 17.37 | 90.0 | 68.97 | 0.844 | 0.726–0.925 | <0.0001 | 0.729 |
| 20.19 | 83.33 | 89.66 | ||||||
| 22.14 | 76.67 | 89.66 | ||||||
| OC | 9.21 | 100 | 58.62 | 0.870 | 0.757–0.943 | <0.0001 | 0.693 | |
| 15.25 | 90.00 | 79.31 | ||||||
| 25.99 | 41.67 | 100.0 | ||||||
| ON | 55.0 | 83.33 | 58.62 | 0.754 | 0.625–0.857 | <0.0001 | 0.496 | |
| 68.2 | 60.00 | 89.66 | ||||||
| 98.2 | 45.0 | 90.0 | ||||||
| Cut-off (ng/mL) | Se (%) | Sp (%) | AUC | 95% CI | P | YI | ||
|---|---|---|---|---|---|---|---|---|
| BL (33.33%) | CTX | 17.37 | 100 | 31.51 | 0.666 | 0.559–0.762 | 0.013 | 0.315 |
| 42.36 | 64.71 | 52.05 | ||||||
| 62.14 | 41.18 | 83.56 | ||||||
| OC | 16.45 | 94.12 | 46.58 | 0.708 | 0.603–0.799 | 0.001 | 0.407 | |
| 18.59 | 70.59 | 54.79 | ||||||
| 28.22 | 52.94 | 83.56 | ||||||
| ON | 88.64 | 76.47 | 56.16 | 0.645 | 0.537–0.743 | 0.032 | 0.326 | |
| 92.14 | 64.71 | 58.90 | ||||||
| 138.7 | 17.65 | 100 | ||||||
| Cut-off (ng/mL) | Se (%) | Sp (%) | AUC | 95% CI | P | YI | ||
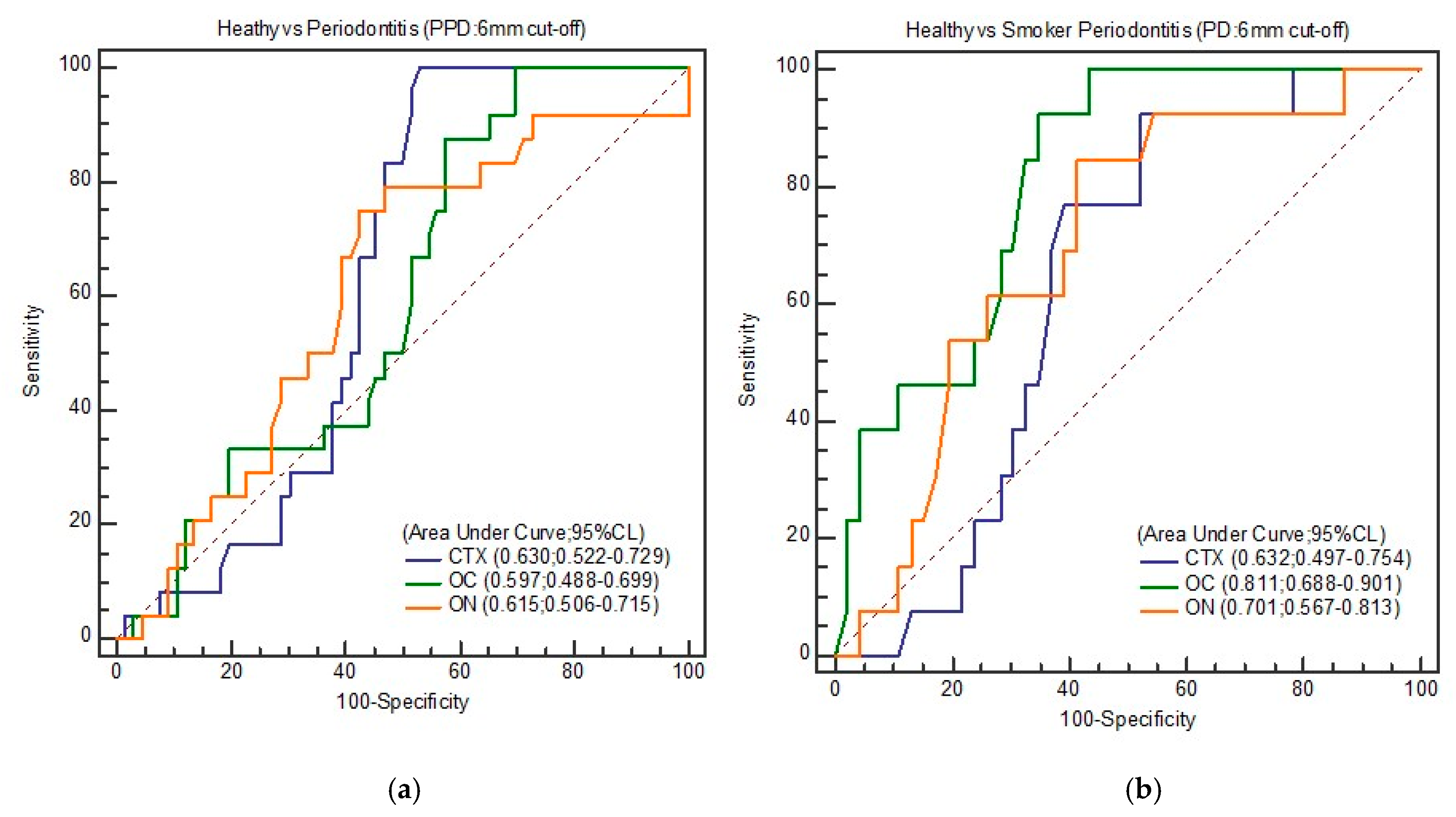
| PPD (6 mm) | CTX | 20.19 | 100 | 46.97 | 0.630 | 0.522–0.729 | 0.023 | 0.469 |
| 30.11 | 83.33 | 50.0 | ||||||
| 39.54 | 75.0 | 54.55 | ||||||
| OC | 9.45 | 100 | 30.30 | 0.597 | 0.488–0.699 | 0.117 | 0.303 | |
| 15.64 | 87.50 | 42.42 | ||||||
| 16.47 | 70.83 | 45.45 | ||||||
| ON | 77.5 | 79.17 | 53.03 | 0.615 | 0.537–0.643 | 0.084 | 0.327 | |
| 88.2 | 75.00 | 57.58 | ||||||
| 89.14 | 66.67 | 59.09 | ||||||
| Cut-off (ng/mL) | Se (%) | Sp (%) | AUC | 95% CI | P | YI | ||
|---|---|---|---|---|---|---|---|---|
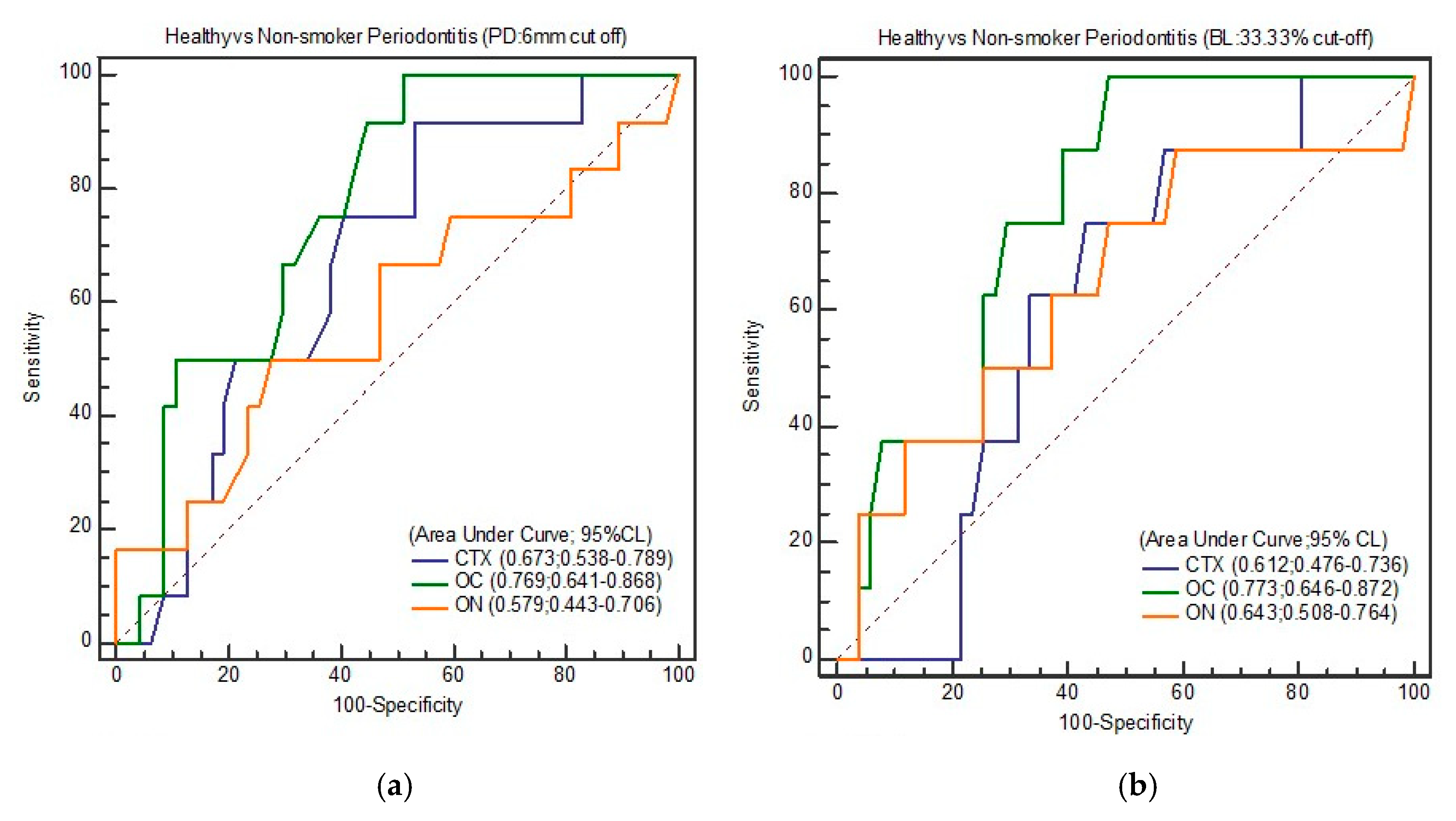
| BL (33.33%) | CTX | 17.37 | 87.50 | 43.14 | 0.612 | 0.476–0.736 | 0.211 | 0.319 |
| 20.19 | 75.00 | 56.86 | ||||||
| 71.56 | 0 | 100 | ||||||
| OC | 15.64 | 100 | 52.94 | 0.773 | 0.646–0.872 | <0.0001 | 0.529 | |
| 16.19 | 87.50 | 54.90 | ||||||
| 29.21 | 37.50 | 92.16 | ||||||
| ON | 55.6 | 87.50 | 41.18 | 0.643 | 0.508–0.764 | 0.231 | 0.287 | |
| 56.33 | 75.0 | 45.10 | ||||||
| 124.6 | 25.0 | 96.08 | ||||||
| Cut-off (ng/mL) | Se (%) | Sp (%) | AUC | 95% CI | P | YI | ||
| PPD (6 mm) | CTX | 17.37 | 91.67 | 46.81 | 0.673 | 0.538–0.789 | 0.030 | 0.384 |
| 18.15 | 75.00 | 46.81 | ||||||
| 45.21 | 50.0 | 78.72 | ||||||
| OC | 11.41 | 100 | 48.94 | 0.769 | 0.641–0.868 | <0.0001 | 0.489 | |
| 15.64 | 91.67 | 55.32 | ||||||
| 26.12 | 50 | 89.32 | ||||||
| ON | 58.11 | 66.67 | 53.19 | 0.579 | 0.443–0.706 | 0.450 | 0.223 | |
| 88.64 | 50.00 | 72.34 | ||||||
| 133.28 | 16.67 | 100 | ||||||
| Cut-off (ng/mL) | Se (%) | Sp (%) | AUC | 95% CI | P | YI | ||
|---|---|---|---|---|---|---|---|---|
| BL (33.33%) | CTX | 15.88 | 80.0 | 36.78 | 0.534 | 0.399–0.665 | 0.729 | 0.167 |
| 17.37 | 70.0 | 40.82 | ||||||
| 20.19 | 50.0 | 53.06 | ||||||
| OC | 11.41 | 100 | 46.94 | 0.809 | 0.686–0.900 | <0.001 | 0.534 | |
| 19.24 | 80.0 | 73.47 | ||||||
| 25.99 | 60.0 | 87.76 | ||||||
| ON | 55.6 | 80.0 | 40.82 | 0.611 | 0.475–0.735 | 0.298 | 0.238 | |
| 58.11 | 70.0 | 53.06 | ||||||
| 108.36 | 30.0 | 93.88 | ||||||
| Cut-off (ng/mL) | Se (%) | Sp (%) | AUC | 95% CI | P | YI | ||
| PPD (6 mm) | CTX | 17.37 | 92.31 | 47.31 | 0.632 | 0.497–0.754 | 0.0732 | 0.401 |
| 20.19 | 76.92 | 60.87 | ||||||
| 71.56 | 100 | 0 | ||||||
| OC | 16.45 | 92.31 | 65.22 | 0.811 | 0.688–0.901 | <0.001 | 0.575 | |
| 18.23 | 84.62 | 67.39 | ||||||
| 29.21 | 38.46 | 95.65 | ||||||
| ON | 57.65 | 84.62 | 54.35 | 0.701 | 0.567–0.813 | 0.009 | 0.433 | |
| 58.11 | 84.62 | 58.70 | ||||||
| 92.14 | 53.85 | 80.43 | ||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Joseph, B.; Javali, M.A.; Khader, M.A.; AlQahtani, S.M.; Mohammed, A. Salivary Osteocalcin as Potential Diagnostic Marker of Periodontal Bone Destruction among Smokers. Biomolecules 2020, 10, 380. https://doi.org/10.3390/biom10030380
Joseph B, Javali MA, Khader MA, AlQahtani SM, Mohammed A. Salivary Osteocalcin as Potential Diagnostic Marker of Periodontal Bone Destruction among Smokers. Biomolecules. 2020; 10(3):380. https://doi.org/10.3390/biom10030380
Chicago/Turabian StyleJoseph, Betsy, Mukhatar Ahmed Javali, Mohasin Abdul Khader, Saad M. AlQahtani, and Amanullah Mohammed. 2020. "Salivary Osteocalcin as Potential Diagnostic Marker of Periodontal Bone Destruction among Smokers" Biomolecules 10, no. 3: 380. https://doi.org/10.3390/biom10030380
APA StyleJoseph, B., Javali, M. A., Khader, M. A., AlQahtani, S. M., & Mohammed, A. (2020). Salivary Osteocalcin as Potential Diagnostic Marker of Periodontal Bone Destruction among Smokers. Biomolecules, 10(3), 380. https://doi.org/10.3390/biom10030380





