Thyrotropin-Releasing Hormone and Food Intake in Mammals: An Update
Abstract
1. Introduction
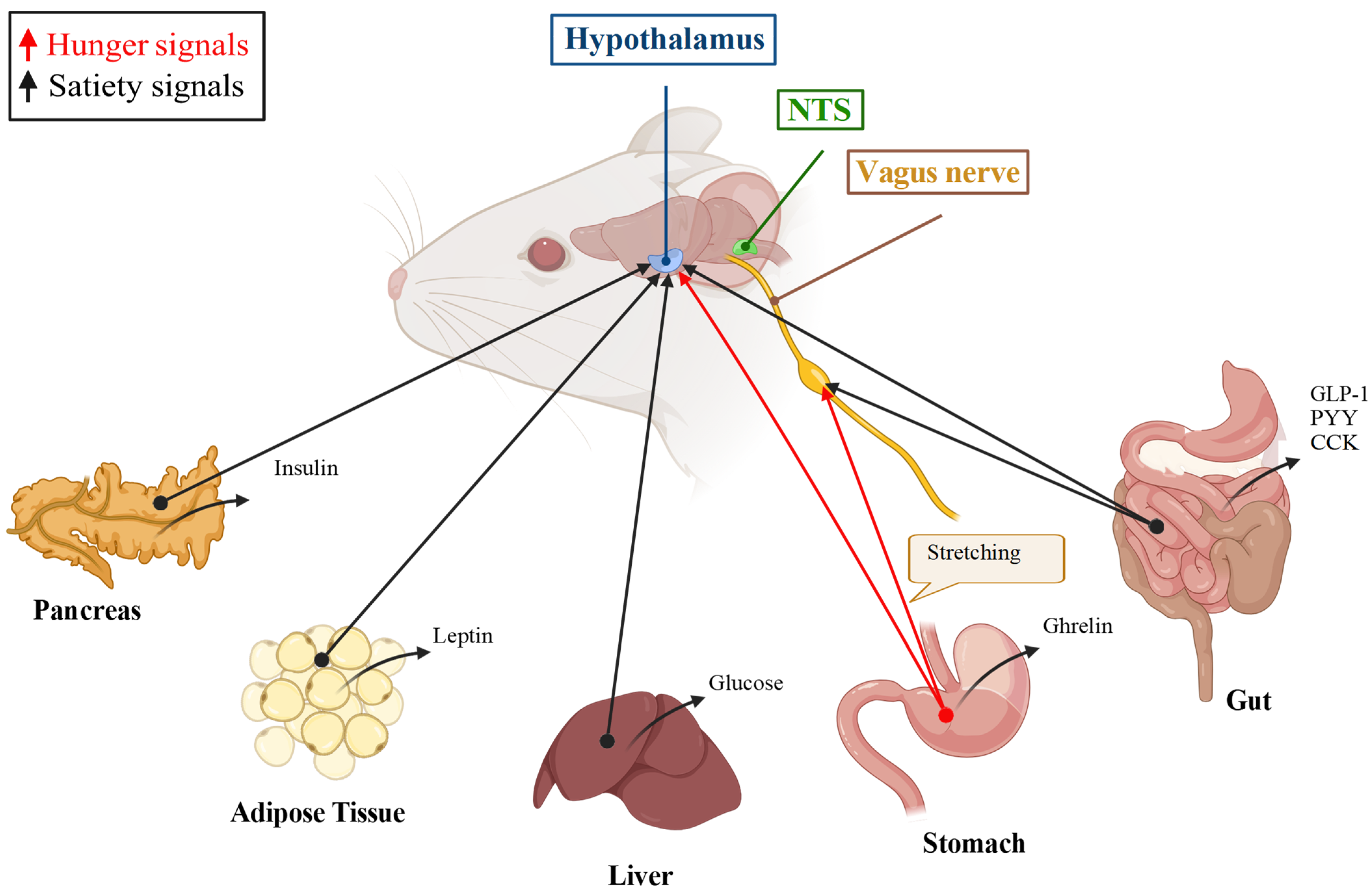
2. Food Appetite, Foraging, Intake, Satiation, and Satiety
3. Discovery of the Effects of TRH, a TRH Analogue, and TRH Catabolites on Food Intake
3.1. The Peripheral Administration of TRH Modifies Food Intake in Mammals, According to the Route of Administration
3.2. TRH Acts through TRH Receptor-1 (TRH-R1) and TRH Receptor-2 (TRH-R2) in Mammals
3.3. Peripheral TRH Is Hydrolyzed by a Metallopeptidase That Likely Limits Its Effect on Food Intake
3.4. The Anorexic Effect of Peripheral TRH on Food Intake Is Independent of the Control of the Pituitary–Thyroid Axis
3.5. Peripheral TRH Effect on Food Intake and Vagus Nerve or Other Sensory Nerve Inputs
3.6. Peripherally Injected TRH Can Enter the Brain through the BBB
3.7. TRH Inactivation In, and Transport Out Of, the CNS Parenchyma
3.8. The Injection of TRH or of RX77368 in Rat, Hamster, or Mouse Cerebral Ventricles Increases or Reduces Food Intake According to Ventricular Localization
3.9. Is the Central TRH Effect on Food Intake Dependent on TRH Receptors, or on a TRH Catabolite?
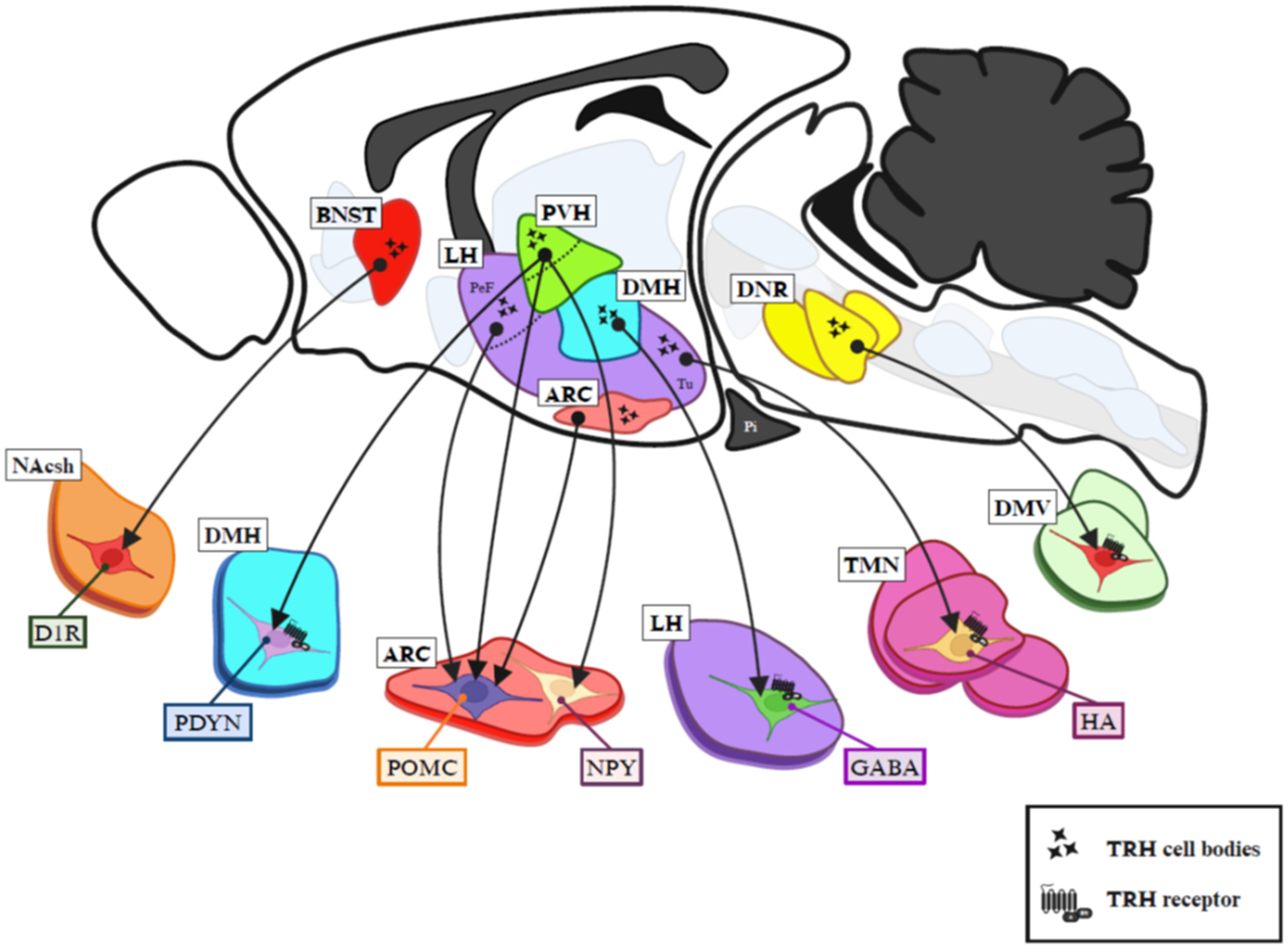
4. In Search of the Central Circuits Involved in TRH Action on Food Intake Behavior
4.1. Putative Hypothalamic TRH Neurons and Targets Sustaining Effect of TRH on Food Intake
4.1.1. Sim1PVH Neurons
4.1.2. Hypophysiotropic TRHPVH Neurons
4.1.3. TRHanterior PVH Neurons
4.1.4. TRHrostral perifornical LH Neurons
4.1.5. TRHtuberal LH Neurons Projecting to Histaminergic Neurons of the Tuberomammillary Nucleus (TMN)
4.1.6. TRHDMH Neurons Projecting onto LH GABA Neurons That Control MCH Neurons
4.1.7. TRHARC Neurons Projecting Locally
4.2. Putative Extrahypothalamic TRH Neurons and Targets Sustaining Effect of TRH on Food Intake
4.2.1. TRHperifornical LH and/or TRHbed nuclei of the stria terminalis Neurons That Project to the NAc
4.2.2. TRHNAcsh Neurons with Unknown Projections
4.2.3. TRHcaudal raphe nuclei Neurons Innervating the DMV
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lechan, R.M.; Wu, P.; Jackson, I.M.D.; Wolf, H.; Cooperman, S.; Mandel, G.; Goodman, R.H. Thyrotropin-Releasing Hormone Precursor: Characterization in Rat Brain. Science 1986, 231, 159–161. [Google Scholar] [CrossRef] [PubMed]
- Perello, M.; Nillni, E. The Biosynthesis and Processing of Neuropeptides: Lessons from Prothyrotropin Releasing Hormone (proTRH). Front. Biosci. 2007, 12, 3554. [Google Scholar] [CrossRef] [PubMed]
- Fekete, C.; Lechan, R.M. Central Regulation of Hypothalamic-Pituitary-Thyroid Axis Under Physiological and Pathophysiological Conditions. Endocr. Rev. 2014, 35, 159–194. [Google Scholar] [CrossRef] [PubMed]
- Joseph-Bravo, P.; Jaimes-Hoy, L.; Charli, J.-L. Regulation of TRH Neurons and Energy Homeostasis-Related Signals under Stress. J. Endocrinol. 2015, 224, R139–R159. [Google Scholar] [CrossRef]
- Jackson, I.M.D.; Reichlin, S. Thyrotropin Releasing Hormone (TRH): Distribution in the Brain, Blood and Urine of the Rat. Life Sci. 1974, 14, 2259–2266. [Google Scholar] [CrossRef]
- Morley, J.E. Extrahypothalamic Thyrotropin Releasing Hormone (TRH)—Its Distribution and Its Functions. Life Sci. 1979, 25, 1539–1550. [Google Scholar] [CrossRef]
- Lechan, R.M.; Wu, P.; Jackson, I.M.D. Immunolocalization of the Thyrotropin-Releasing Hormone Prohormone in the Rat Central Nervous System. Endocrinology 1986, 119, 1210–1216. [Google Scholar] [CrossRef] [PubMed]
- Segerson, T.P.; Hoefler, H.; Childers, H.; Wolfe, H.J.; Wu, P.; Jackson, I.M.D.; Lechan, R.M. Localization of Thyrotropin-Releasing Hormone Prohormone Messenger Ribonucleic Acid in Rat Brain by in Situ Hybridization. Endocrinology 1987, 121, 98–107. [Google Scholar] [CrossRef]
- Hökfelt, T.; Tsuruo, Y.; Ulfhake, B.; Cullheim, S.; Arvidsson, U.; Foster, G.A.; Schultzberg, M.; Schalling, M.; Arborelius, L.; Freedman, J.; et al. Distribution of TRH-like Immunoreactivity with Special Reference to Coexistence with Other Neuroactive Compounds. Ann. N. Y. Acad. Sci. 1989, 553, 76–105. [Google Scholar] [CrossRef]
- Satoh, T.; Yamada, M.; Monden, T.; Iizuka, M.; Mori, M. Cloning of the Mouse Hypothalamic Preprothyrotropin-Releasing Hormone (TRH) cDNA and Tissue Distribution of Its mRNA. Brain Res. Mol. Brain Res. 1992, 14, 131–135. [Google Scholar] [CrossRef]
- Hall, K.D. Did the Food Environment Cause the Obesity Epidemic? Obesity 2018, 26, 11–13. [Google Scholar] [CrossRef] [PubMed]
- Horita, A.; Kalivas, P.W.; Simasko, S.M. Thyrotropin Releasing Hormone (TRH): Possible Physiological Functions Not Related to the Neuroendocrine System. Rev. Pure Appl. Pharmacol. Sci. 1983, 4, 111–137. [Google Scholar] [PubMed]
- Bowden, C.R.; Karkanias, C.D.; Bean, A.J. Re-Evaluation of Histidyl-Proline Diketopiperazine [Cyclo(His-Pro)] Effects on Food Intake in the Rat. Pharmacol. Biochem. Behav. 1988, 29, 357–363. [Google Scholar] [CrossRef]
- Karydis, I.; Tolis, G. Orexis, Anorexia, and Thyrotropin-Releasing Hormone. Thyroid 1998, 8, 947–950. [Google Scholar] [CrossRef] [PubMed]
- Tache, Y.; Adelson, D.; Yang, H. TRH/TRH-R1 Receptor Signaling in the Brain Medulla as a Pathway of Vagally Mediated Gut Responses During the Cephalic Phase. Curr. Pharm. Des. 2014, 20, 2725–2730. [Google Scholar] [CrossRef] [PubMed]
- Joseph-Bravo, P.; Jaimes-Hoy, L.; Uribe, R.-M.; Charli, J.-L. 60 YEARS OF NEUROENDOCRINOLOGY: TRH, the First Hypophysiotropic Releasing Hormone Isolated: Control of the Pituitary–Thyroid Axis. J. Endocrinol. 2015, 226, T85–T100. [Google Scholar] [CrossRef]
- Charli, J.-L.; Rodríguez-Rodríguez, A.; Hernández-Ortega, K.; Cote-Vélez, A.; Uribe, R.M.; Jaimes-Hoy, L.; Joseph-Bravo, P. The Thyrotropin-Releasing Hormone-Degrading Ectoenzyme, a Therapeutic Target? Front. Pharmacol. 2020, 11, 640. [Google Scholar] [CrossRef]
- Alvarez-Salas, E.; García-Luna, C.; Soberanes-Chávez, P.; De Gortari, P. Role of the Thyrotropin-Releasing Hormone of the Limbic System in Mood and Eating Regulation. J. Integr. Neurosci. 2022, 21, 047. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Salas, E.; García-Luna, C.; De Gortari, P. New Efforts to Demonstrate the Successful Use of TRH as a Therapeutic Agent. Int. J. Mol. Sci. 2023, 24, 11047. [Google Scholar] [CrossRef]
- Berthoud, H.-R. Neural Control of Appetite: Cross-Talk between Homeostatic and Non-Homeostatic Systems. Appetite 2004, 43, 315–317. [Google Scholar] [CrossRef]
- Kelley, A.; Baldo, B.; Pratt, W.; Will, M. Corticostriatal-Hypothalamic Circuitry and Food Motivation: Integration of Energy, Action and Reward. Physiol. Behav. 2005, 86, 773–795. [Google Scholar] [CrossRef] [PubMed]
- Fulton, S. Appetite and Reward. Front. Neuroendocrinol. 2010, 31, 85–103. [Google Scholar] [CrossRef] [PubMed]
- Narayanan, N.S.; Guarnieri, D.J.; DiLeone, R.J. Metabolic Hormones, Dopamine Circuits, and Feeding. Front. Neuroendocrinol. 2010, 31, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Grill, H.J.; Hayes, M.R. Hindbrain Neurons as an Essential Hub in the Neuroanatomically Distributed Control of Energy Balance. Cell Metab. 2012, 16, 296–309. [Google Scholar] [CrossRef] [PubMed]
- Sternson, S.M.; Nicholas Betley, J.; Cao, Z.F.H. Neural Circuits and Motivational Processes for Hunger. Curr. Opin. Neurobiol. 2013, 23, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Waterson, M.J.; Horvath, T.L. Neuronal Regulation of Energy Homeostasis: Beyond the Hypothalamus and Feeding. Cell Metab. 2015, 22, 962–970. [Google Scholar] [CrossRef] [PubMed]
- Roh, E.; Song, D.K.; Kim, M.-S. Emerging Role of the Brain in the Homeostatic Regulation of Energy and Glucose Metabolism. Exp. Mol. Med. 2016, 48, e216. [Google Scholar] [CrossRef] [PubMed]
- Perez-Leighton, C.; Kerr, B.; Scherer, P.E.; Baudrand, R.; Cortés, V. The Interplay between Leptin, Glucocorticoids, and GLP1 Regulates Food Intake and Feeding Behaviour. Biol. Rev. 2023, 99, 653–674. [Google Scholar] [CrossRef] [PubMed]
- Brüning, J.C.; Fenselau, H. Integrative Neurocircuits That Control Metabolism and Food Intake. Science 2023, 381, eabl7398. [Google Scholar] [CrossRef]
- Rossi, M.A. Control of Energy Homeostasis by the Lateral Hypothalamic Area. Trends Neurosci. 2023, 46, 738–749. [Google Scholar] [CrossRef]
- Lavoie, O.; Michael, N.J.; Caron, A. A Critical Update on the Leptin-Melanocortin System. J. Neurochem. 2023, 165, 467–486. [Google Scholar] [CrossRef] [PubMed]
- Purnell, J.Q.; Le Roux, C.W. Hypothalamic Control of Body Fat Mass by Food Intake: The Key to Understanding Why Obesity Should Be Treated as a Disease. Diabetes Obes. Metab. 2024, 26, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Costa, D.G.; Almeida, C.; Cavadas, C.; Carmo-Silva, S. A Look on Food Intake and Satiety: From Humans to Rodent Models. Nutr. Rev. 2022, 80, 1942–1957. [Google Scholar] [CrossRef] [PubMed]
- Morton, G.J.; Meek, T.H.; Schwartz, M.W. Neurobiology of Food Intake in Health and Disease. Nat. Rev. Neurosci. 2014, 15, 367–378. [Google Scholar] [CrossRef] [PubMed]
- Rui, L. Brain Regulation of Energy Balance and Body Weight. Rev. Endocr. Metab. Disord. 2013, 14, 387–407. [Google Scholar] [CrossRef] [PubMed]
- Plata-Salamán, C. Cytokines and Feeding. Int. J. Obes. 2001, 25, S48–S52. [Google Scholar] [CrossRef] [PubMed]
- Aklan, I.; Sayar Atasoy, N.; Yavuz, Y.; Ates, T.; Coban, I.; Koksalar, F.; Filiz, G.; Topcu, I.C.; Oncul, M.; Dilsiz, P.; et al. NTS Catecholamine Neurons Mediate Hypoglycemic Hunger via Medial Hypothalamic Feeding Pathways. Cell Metab. 2020, 31, 313–326.e5. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, P.; Judge, M.E.; Thim, L.; Ribel, U.; Christjansen, K.N.; Wulff, B.S.; Clausen, J.T.; Jensen, P.B.; Madsen, O.D.; Vrang, N.; et al. Hypothalamic CART Is a New Anorectic Peptide Regulated by Leptin. Nature 1998, 393, 72–76. [Google Scholar] [CrossRef]
- Baird, J.-P.; Gray, N.E.; Fischer, S.G. Effects of Neuropeptide Y on Feeding Microstructure: Dissociation of Appetitive and Consummatory Actions. Behav. Neurosci. 2006, 120, 937–951. [Google Scholar] [CrossRef]
- Aponte, Y.; Atasoy, D.; Sternson, S.M. AGRP Neurons Are Sufficient to Orchestrate Feeding Behavior Rapidly and without Training. Nat. Neurosci. 2011, 14, 351–355. [Google Scholar] [CrossRef]
- Atasoy, D.; Betley, J.N.; Su, H.H.; Sternson, S.M. Deconstruction of a Neural Circuit for Hunger. Nature 2012, 488, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Chou, T.C.; Scammell, T.E.; Gooley, J.J.; Gaus, S.E.; Saper, C.B.; Lu, J. Critical Role of Dorsomedial Hypothalamic Nucleus in a Wide Range of Behavioral Circadian Rhythms. J. Neurosci. 2003, 23, 10691–10702. [Google Scholar] [CrossRef] [PubMed]
- Anand, B.K.; Brobeck, J.R. Localization of a “Feeding Center” in the Hypothalamus of the Rat. Exp. Biol. Med. 1951, 77, 323–325. [Google Scholar] [CrossRef] [PubMed]
- Delgado, J.M.R.; Anand, B.K. Increase of Food Intake Induced by Electrical Stimulation of the Lateral Hypothalamus. Am. J. Physiol.-Leg. Content 1952, 172, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Morgane, P.J. The Function of the Limbic and Rhinic Forebrain-Limbic Midbrain Systems in the Regulation of Food and Water Intake. Ann. N. Y. Acad. Sci. 1969, 157, 806–848. [Google Scholar] [CrossRef] [PubMed]
- Wise, R.A. Lateral Hypothalamic Electrical Stimulation: Does It Make Animals ‘Hungry’? Brain Res. 1974, 67, 187–209. [Google Scholar] [CrossRef]
- Schwartz, M.W.; Woods, S.C.; Porte, D.; Seeley, R.J.; Baskin, D.G. Central Nervous System Control of Food Intake. Nature 2000, 404, 661–671. [Google Scholar] [CrossRef] [PubMed]
- Hussain, S.S.; Bloom, S.R. The Regulation of Food Intake by the Gut-Brain Axis: Implications for Obesity. Int. J. Obes. 2013, 37, 625–633. [Google Scholar] [CrossRef]
- Adamantidis, A.; De Lecea, L. The Hypocretins as Sensors for Metabolism and Arousal. J. Physiol. 2009, 587, 33–40. [Google Scholar] [CrossRef]
- Inutsuka, A.; Inui, A.; Tabuchi, S.; Tsunematsu, T.; Lazarus, M.; Yamanaka, A. Concurrent and Robust Regulation of Feeding Behaviors and Metabolism by Orexin Neurons. Neuropharmacology 2014, 85, 451–460. [Google Scholar] [CrossRef]
- Subramanian, K.S.; Lauer, L.T.; Hayes, A.M.R.; Décarie-Spain, L.; McBurnett, K.; Nourbash, A.C.; Donohue, K.N.; Kao, A.E.; Bashaw, A.G.; Burdakov, D.; et al. Hypothalamic Melanin-Concentrating Hormone Neurons Integrate Food-Motivated Appetitive and Consummatory Processes in Rats. Nat. Commun. 2023, 14, 1755. [Google Scholar] [CrossRef] [PubMed]
- Jennings, J.H.; Ung, R.L.; Resendez, S.L.; Stamatakis, A.M.; Taylor, J.G.; Huang, J.; Veleta, K.; Kantak, P.A.; Aita, M.; Shilling-Scrivo, K.; et al. Visualizing Hypothalamic Network Dynamics for Appetitive and Consummatory Behaviors. Cell 2015, 160, 516–527. [Google Scholar] [CrossRef] [PubMed]
- Suyama, S.; Yada, T. New Insight into GABAergic Neurons in the Hypothalamic Feeding Regulation. J. Physiol. Sci. 2018, 68, 717–722. [Google Scholar] [CrossRef]
- Wu, Q.; Palmiter, R.D. GABAergic Signaling by AgRP Neurons Prevents Anorexia via a Melanocortin-Independent Mechanism. Eur. J. Pharmacol. 2011, 660, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Clark, M.S.; Palmiter, R.D. Deciphering a Neuronal Circuit That Mediates Appetite. Nature 2012, 483, 594–597. [Google Scholar] [CrossRef] [PubMed]
- Sutton, A.K.; Myers, M.G.; Olson, D.P. The Role of PVH Circuits in Leptin Action and Energy Balance. Annu. Rev. Physiol. 2016, 78, 207–221. [Google Scholar] [CrossRef]
- Li, M.M.; Madara, J.C.; Steger, J.S.; Krashes, M.J.; Balthasar, N.; Campbell, J.N.; Resch, J.M.; Conley, N.J.; Garfield, A.S.; Lowell, B.B. The Paraventricular Hypothalamus Regulates Satiety and Prevents Obesity via Two Genetically Distinct Circuits. Neuron 2019, 102, 653–667.e6. [Google Scholar] [CrossRef]
- Alhadeff, A.L.; Goldstein, N.; Park, O.; Klima, M.L.; Vargas, A.; Betley, J.N. Natural and Drug Rewards Engage Distinct Pathways That Converge on Coordinated Hypothalamic and Reward Circuits. Neuron 2019, 103, 891–908.e6. [Google Scholar] [CrossRef]
- Cheng, J.; Feenstra, M.G.P. Individual Differences in Dopamine Efflux in Nucleus Accumbens Shell and Core during Instrumental Learning. Learn. Mem. 2006, 13, 168–177. [Google Scholar] [CrossRef]
- Bassareo, V.; Cucca, F.; Frau, R.; Di Chiara, G. Differential Activation of Accumbens Shell and Core Dopamine by Sucrose Reinforcement with Nose Poking and with Lever Pressing. Behav. Brain Res. 2015, 294, 215–223. [Google Scholar] [CrossRef]
- Maldonado-Irizarry, C.; Swanson, C.; Kelley, A. Glutamate Receptors in the Nucleus Accumbens Shell Control Feeding Behavior via the Lateral Hypothalamus. J. Neurosci. 1995, 15, 6779–6788. [Google Scholar] [CrossRef] [PubMed]
- Stratford, T.R.; Kelley, A.E. Evidence of a Functional Relationship between the Nucleus Accumbens Shell and Lateral Hypothalamus Subserving the Control of Feeding Behavior. J. Neurosci. 1999, 19, 11040–11048. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, S.M.; Berridge, K.C. Fear and Feeding in the Nucleus Accumbens Shell: Rostrocaudal Segregation of GABA-Elicited Defensive Behavior Versus Eating Behavior. J. Neurosci. 2001, 21, 3261–3270. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.; Corkern, M.; Stoyanova, I.; Patterson, L.M.; Tian, R.; Berthoud, H.-R. Appetite-Inducing Accumbens Manipulation Activates Hypothalamic Orexin Neurons and Inhibits POMC Neurons. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2003, 284, R1436–R1444. [Google Scholar] [CrossRef] [PubMed]
- Baldo, B.A.; Gual-Bonilla, L.; Sijapati, K.; Daniel, R.A.; Landry, C.F.; Kelley, A.E. Activation of a Subpopulation of Orexin/Hypocretin-containing Hypothalamic Neurons by GABAA Receptor-mediated Inhibition of the Nucleus Accumbens Shell, but Not by Exposure to a Novel Environment. Eur. J. Neurosci. 2004, 19, 376–386. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.; Patterson, L.M.; Berthoud, H.-R. Orexin Signaling in the Ventral Tegmental Area Is Required for High-Fat Appetite Induced by Opioid Stimulation of the Nucleus Accumbens. J. Neurosci. 2007, 27, 11075–11082. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, E.C.; Kremer, Y.; Lefort, S.; Harada, M.; Pascoli, V.; Rohner, C.; Lüscher, C. Accumbal D1R Neurons Projecting to Lateral Hypothalamus Authorize Feeding. Neuron 2015, 88, 553–564. [Google Scholar] [CrossRef] [PubMed]
- Khomane, K.S.; Nandekar, P.P.; Wahlang, B.; Bagul, P.; Shaikh, N.; Pawar, Y.B.; Meena, C.L.; Sangamwar, A.T.; Jain, R.; Tikoo, K.; et al. Mechanistic Insights into PEPT1-Mediated Transport of a Novel Antiepileptic, NP-647. Mol. Pharm. 2012, 9, 2458–2468. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.E.; Levine, A.S. Thyrotropin Releasing Hormone (TRH) Suppresses Stress Induced Eating. Life Sci. 1980, 27, 269–274. [Google Scholar] [CrossRef]
- Kelly, J.A.; Boyle, N.T.; Cole, N.; Slator, G.R.; Colivicchi, M.A.; Stefanini, C.; Gobbo, O.L.; Scalabrino, G.A.; Ryan, S.M.; Elamin, M.; et al. First-in-Class Thyrotropin-Releasing Hormone (TRH)-Based Compound Binds to a Pharmacologically Distinct TRH Receptor Subtype in Human Brain and Is Effective in Neurodegenerative Models. Neuropharmacology 2015, 89, 193–203. [Google Scholar] [CrossRef]
- Sun, Y.; Lu, X.; Gershengorn, M. Thyrotropin-Releasing Hormone Receptors—Similarities and Differences. J. Mol. Endocrinol. 2003, 30, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Trubacova, R.; Drastichova, Z.; Novotny, J. Biochemical and Physiological Insights into TRH Receptor-Mediated Signaling. Front. Cell Dev. Biol. 2022, 10, 981452. [Google Scholar] [CrossRef]
- Livingston, C.A.; Berger, A.J. Response of Neurons in the Dorsal Motor Nucleus of the Vagus to Thyrotropin-Releasing Hormone. Brain Res. 1993, 621, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Travagli, R.A.; Gillis, R.A.; Vicini, S. Effects of Thyrotropin-Releasing Hormone on Neurons in Rat Dorsal Motor Nucleus of the Vagus, in Vitro. Am. J. Physiol.-Gastrointest. Liver Physiol. 1992, 263, G508–G517. [Google Scholar] [CrossRef] [PubMed]
- Toledo-Aral, J.; Castellano, A.; Ureña, J.; López-Barneo, J. Dual Modulation of K+ Currents and Cytosolic Ca2+ by the Peptide TRH and Its Derivatives in Guinea-pig Septal Neurones. J. Physiol. 1993, 472, 327–340. [Google Scholar] [CrossRef] [PubMed]
- Ebihara, S.; Akaike, N. Potassium Currents Operated by Thyrotrophin-releasing Hormone in Dissociated CA1 Pyramidal Neurones of Rat Hippocampus. J. Physiol. 1993, 472, 689–710. [Google Scholar] [CrossRef] [PubMed]
- Hara, J.; Gerashchenko, D.; Wisor, J.P.; Sakurai, T.; Xie, X.S.; Kilduff, T.S. Thyrotropin-Releasing Hormone Increases Behavioral Arousal through Modulation of Hypocretin/Orexin Neurons. J. Neurosci. 2009, 29, 3705–3714. [Google Scholar] [CrossRef] [PubMed]
- Ishibashi, H.; Nakahata, Y.; Eto, K.; Nabekura, J. Excitation of Locus Coeruleus Noradrenergic Neurons by Thyrotropin-releasing Hormone. J. Physiol. 2009, 587, 5709–5722. [Google Scholar] [CrossRef] [PubMed]
- González, J.A.; Horjales-Araujo, E.; Fugger, L.; Broberger, C.; Burdakov, D. Stimulation of Orexin/Hypocretin Neurones by Thyrotropin-releasing Hormone. J. Physiol. 2009, 587, 1179–1186. [Google Scholar] [CrossRef]
- Zhang, L.; Kolaj, M.; Renaud, L.P. Intracellular Postsynaptic Cannabinoid Receptors Link Thyrotropin-Releasing Hormone Receptors to TRPC-like Channels in Thalamic Paraventricular Nucleus Neurons. Neuroscience 2015, 311, 81–91. [Google Scholar] [CrossRef]
- Heuer, H.; Schäfer, M.K.; O’Donnell, D.; Walker, P.; Bauer, K. Expression of Thyrotropin-Releasing Hormone Receptor 2 (TRH-R2) in the Central Nervous System of Rats. J. Comp. Neurol. 2000, 428, 319–336. [Google Scholar] [CrossRef] [PubMed]
- Mitsuma, T.; Rhue, N.; Sobue, G.; Hirooka, Y.; Kayama, M.; Yokoi, Y.; Adachi, K.; Nogimori, T.; Sakai, J.; Sugie, I. Distribution of Thyrotropin Releasing Hormone Receptor in Rats: An Immunohistochemical Study. Endocr. Regul. 1995, 29, 129–134. [Google Scholar] [PubMed]
- Cao, J.; O’Donnell, D.; Vu, H.; Payza, K.; Pou, C.; Godbout, C.; Jakob, A.; Pelletier, M.; Lembo, P.; Ahmad, S.; et al. Cloning and Characterization of a cDNA Encoding a Novel Subtype of Rat Thyrotropin-Releasing Hormone Receptor. J. Biol. Chem. 1998, 273, 32281–32287. [Google Scholar] [CrossRef] [PubMed]
- Drummond, A.H. Chlordiazepoxide Is a Competitive Thyrotropin-Releasing Hormone Receptor Antagonist in GH3 Pituitary Tumour Cells. Biochem. Biophys. Res. Commun. 1985, 127, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Prokai-Tatrai, K.; Nguyen, V.; Prokai, L. [β-Glu2]TRH Is a Functional Antagonist of Thyrotropin-Releasing Hormone (TRH) in the Rodent Brain. Int. J. Mol. Sci. 2021, 22, 6230. [Google Scholar] [CrossRef] [PubMed]
- Regazzoni, L.; Fumagalli, L.; Artasensi, A.; Gervasoni, S.; Gilardoni, E.; Mazzolari, A.; Aldini, G.; Vistoli, G. Cyclo(His-Pro) Exerts Protective Carbonyl Quenching Effects through Its Open Histidine Containing Dipeptides. Nutrients 2022, 14, 1775. [Google Scholar] [CrossRef] [PubMed]
- May, P.; Donalbedian, R.K. Factors in Blood Influencing the Determination of Thyrotropin Releasing Hormone. Clin. Chim. Acta 1973, 46, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Nagai, Y.; Yokohama, S.; Nagawa, Y.; Hirooka, Y.; Nihei, N. Blood level and brain distribution of thyrotropin-releasing hormone (TRH) determined by radioimmunoassay after intravenous administration in rats. J. Pharmacobiodyn. 1980, 3, 500–506. [Google Scholar] [CrossRef] [PubMed]
- Schuhler, S.; Warner, A.; Finney, N.; Bennett, G.W.; Ebling, F.J.P.; Brameld, J.M. Thyrotrophin-Releasing Hormone Decreases Feeding and Increases Body Temperature, Activity and Oxygen Consumption in Siberian Hamsters. J. Neuroendocrinol. 2007, 19, 239–249. [Google Scholar] [CrossRef]
- Chen, H.J.; Meites, J. Effects of Biogenic Amines and TRH on Release of Prolactin and TSH in the Rat. Endocrinology 1975, 96, 10–14. [Google Scholar] [CrossRef]
- Garcia, M.D.; Escobar Del Rey, F.; Morreale De Escobar, G. Thyrotropin-Releasing Hormone and Thyroid Hormone Interactions on Thyrotropin Secretion in the Rat: Lack of Inhibiting Effects of Small Doses of Triiodo-L-Thyronine in the Hypothyroid Rat. Endocrinology 1976, 98, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Nemeroff, C.B.; Konkol, R.J.; Bissette, G.; Youngblood, W.; Martin, J.B.; Brazeau, P.; Rone, M.S.; Prange, A.J.; Breese, G.R.; Kizer, J.S. Analysis of the Disruption in Hypothalamic-Pituitary Regulation in Rats Treated Neonatally with Monosodium L-Glutamate (MSG): Evidence for the Involvement of Tuberoinfundibular Cholinergic and Dopaminergic Systems in Neuroendocrine Regulation. Endocrinology 1977, 101, 613–622. [Google Scholar] [CrossRef] [PubMed]
- Lifschitz, B.M.; Defesi, C.R.; Surks, M.I. Thyrotropin Response to Thyrotropin-Releasing Hormone in the Euthyroid Rat: Dose-Response, Time Course, and Demonstration of Partial Refractoriness to a Second Dose of Thyrotropin-Releasing Hormone. Endocrinology 1978, 102, 1775–1782. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekar, A.; Schmidtlein, P.M.; Neve, V.; Rivagorda, M.; Spiecker, F.; Gauthier, K.; Prevot, V.; Schwaninger, M.; Müller-Fielitz, H. Regulation of Thyroid Hormone Gatekeepers by Thyrotropin in Tanycytes. Thyroid 2024, 34, 261–273. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.E.; Levine, A.S.; Kneip, J.; Grace, M. The Effect of Vagotomy on the Satiety Effects of Neuropeptides and Naloxone. Life Sci. 1982, 30, 1943–1947. [Google Scholar] [CrossRef]
- Peters, J.H.; Simasko, S.M.; Ritter, R.C. Modulation of Vagal Afferent Excitation and Reduction of Food Intake by Leptin and Cholecystokinin. Physiol. Behav. 2006, 89, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Huang, W.; Yi, S. Cellular Complexity of the Peripheral Nervous System: Insights from Single-Cell Resolution. Front. Neurosci. 2023, 17, 1098612. [Google Scholar] [CrossRef] [PubMed]
- Zeisel, A.; Hochgerner, H.; Lönnerberg, P.; Johnsson, A.; Memic, F.; Van Der Zwan, J.; Häring, M.; Braun, E.; Borm, L.E.; La Manno, G.; et al. Molecular Architecture of the Mouse Nervous System. Cell 2018, 174, 999–1014.e22. [Google Scholar] [CrossRef] [PubMed]
- Kupari, J.; Häring, M.; Agirre, E.; Castelo-Branco, G.; Ernfors, P. An Atlas of Vagal Sensory Neurons and Their Molecular Specialization. Cell Rep. 2019, 27, 2508–2523.e4. [Google Scholar] [CrossRef]
- Mamedova, E.; Dmytriyeva, O.; Rekling, J.C. Thyrotropin-Releasing Hormone Induces Ca2+ Increase in a Subset of Vagal Nodose Ganglion Neurons. Neuropeptides 2022, 94, 102261. [Google Scholar] [CrossRef]
- Mallik, T.K.; Wilber, J.F.; Pegues, J. Measurements of Thyrotropin-Releasing Hormone-Like Material in Human Peripheral Blood by Affinity Chromatography and Radioimmunoassay. J. Clin. Endocrinol. Metab. 1982, 54, 1194–1198. [Google Scholar] [CrossRef] [PubMed]
- Banks, W.A. Viktor Mutt Lecture: Peptides Can Cross the Blood-Brain Barrier. Peptides 2023, 169, 171079. [Google Scholar] [CrossRef] [PubMed]
- Lipinski, C.A. Lead- and drug-like compounds: The rule-of-five revolution. Drug Discov Today Technol. 2004, 1, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Meisenberg, G.; Simmons, W.H. Peptides and the Blood-Brain Barrier. Life Sci. 1983, 32, 2611–2623. [Google Scholar] [CrossRef] [PubMed]
- Brooks, B.R.; Kalin, N.; Beaulieu, D.A.; Barksdale, C.; Sufit, R.L.; Dills, D.G. Thyrotropin Releasing Hormone Uptake into Serum and Cerebrospinal Fluid Following Intravenous or Subcutaneous Administration. Neurol. Res. 1988, 10, 236–238. [Google Scholar] [CrossRef] [PubMed]
- Pardridge, W.M. Neuropeptides and the Blood-Brain Barrier. Annu. Rev. Physiol. 1983, 45, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Zloković, B.V.; Segal, M.B.; Begley, D.J.; Davson, H.; Rakić, L. Permeability of the Blood-Cerebrospinal Fluid and Blood-Brain Barriers to Thyrotropin-Releasing Hormone. Brain Res. 1985, 358, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Zloković, B.V.; Lipovac, M.N.; Begley, D.J.; Davson, H.; Rakić, L. Slow Penetration of Thyrotropin-Releasing Hormone Across the Blood-Brain Barrier of an In Situ Perfused Guinea Pig Brain. J. Neurochem. 1988, 51, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Langlet, F.; Levin, B.E.; Luquet, S.; Mazzone, M.; Messina, A.; Dunn-Meynell, A.A.; Balland, E.; Lacombe, A.; Mazur, D.; Carmeliet, P.; et al. Tanycytic VEGF-A Boosts Blood-Hypothalamus Barrier Plasticity and Access of Metabolic Signals to the Arcuate Nucleus in Response to Fasting. Cell Metab. 2013, 17, 607–617. [Google Scholar] [CrossRef]
- Schaeffer, M.; Langlet, F.; Lafont, C.; Molino, F.; Hodson, D.J.; Roux, T.; Lamarque, L.; Verdié, P.; Bourrier, E.; Dehouck, B.; et al. Rapid Sensing of Circulating Ghrelin by Hypothalamic Appetite-Modifying Neurons. Proc. Natl. Acad. Sci. USA 2013, 110, 1512–1517. [Google Scholar] [CrossRef]
- Rodríguez-Cortés, B.; Hurtado-Alvarado, G.; Martínez-Gómez, R.; León-Mercado, L.A.; Prager-Khoutorsky, M.; Buijs, R.M. Suprachiasmatic Nucleus-Mediated Glucose Entry into the Arcuate Nucleus Determines the Daily Rhythm in Blood Glycemia. Curr. Biol. 2022, 32, 796–805.e4. [Google Scholar] [CrossRef] [PubMed]
- Peruzzo, B.; Pastor, F.; Blázquez, J.; Amat, P.; Rodríguez, E. Polarized Endocytosis and Transcytosis in the Hypothalamic Tanycytes of the Rat. Cell Tissue Res. 2004, 317, 147–164. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, E.; Blazquez, J.; Pastor, F.; Pelaez, B.; Pena, P.; Peruzzo, B.; Amat, P. Hypothalamic Tanycytes: A Key Component of Brain–Endocrine Interaction. Int. Rev. Cytol. 2005, 247, 89–164. [Google Scholar] [CrossRef] [PubMed]
- Müller-Fielitz, H.; Stahr, M.; Bernau, M.; Richter, M.; Abele, S.; Krajka, V.; Benzin, A.; Wenzel, J.; Kalies, K.; Mittag, J.; et al. Tanycytes Control the Hormonal Output of the Hypothalamic-Pituitary-Thyroid Axis. Nat. Commun. 2017, 8, 484. [Google Scholar] [CrossRef] [PubMed]
- Farkas, E.; Varga, E.; Kovács, B.; Szilvásy-Szabó, A.; Cote-Vélez, A.; Péterfi, Z.; Matziari, M.; Tóth, M.; Zelena, D.; Mezriczky, Z.; et al. A Glial-Neuronal Circuit in the Median Eminence Regulates Thyrotropin-Releasing Hormone-Release via the Endocannabinoid System. iScience 2020, 23, 100921. [Google Scholar] [CrossRef] [PubMed]
- Duquenne, M.; Folgueira, C.; Bourouh, C.; Millet, M.; Silva, A.; Clasadonte, J.; Imbernon, M.; Fernandois, D.; Martinez-Corral, I.; Kusumakshi, S.; et al. Leptin Brain Entry via a Tanycytic LepR–EGFR Shuttle Controls Lipid Metabolism and Pancreas Function. Nat. Metab. 2021, 3, 1071–1090. [Google Scholar] [CrossRef] [PubMed]
- Uriarte, M.; De Francesco, P.N.; Fernández, G.; Castrogiovanni, D.; D’Arcangelo, M.; Imbernon, M.; Cantel, S.; Denoyelle, S.; Fehrentz, J.-A.; Praetorius, J.; et al. Circulating Ghrelin Crosses the Blood-Cerebrospinal Fluid Barrier via Growth Hormone Secretagogue Receptor Dependent and Independent Mechanisms. Mol. Cell. Endocrinol. 2021, 538, 111449. [Google Scholar] [CrossRef]
- Brewster, D.; Dettmar, P.W.; Metcalf, G. Biologically stable analogues of TRH with increased neuropharmacological potency. Neuropharmacology 1981, 20, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Charli, J.; Ponce, G.; McKelvy, J.F.; Joseph-Bravo, P. Accumulation of Thyrotropin Releasing Hormone by Rat Hypothalamic Slices. J. Neurochem. 1984, 42, 981–986. [Google Scholar] [CrossRef]
- Banks, W.A.; Kastin, A.J. Peptide Transport Systems for Opiates across the Blood-Brain Barrier. Am. J. Physiol.-Endocrinol. Metab. 1990, 259, E1–E10. [Google Scholar] [CrossRef]
- Oliver, C.; Ben-Jonathan, N.; Mical, S.; Porter, J.C. Transport of Thyrotropin-Releasing Hormone from Cerebrospinal Fluid to Hypophysial Portal Blood and the Release of Thyrotropin. Endocrinology 1975, 97, 1138–1143. [Google Scholar] [CrossRef] [PubMed]
- Yamada, M.; Saga, Y.; Shibusawa, N.; Hirato, J.; Murakami, M.; Iwasaki, T.; Hashimoto, K.; Satoh, T.; Wakabayashi, K.; Taketo, M.M.; et al. Tertiary Hypothyroidism and Hyperglycemia in Mice with Targeted Disruption of the Thyrotropin-Releasing Hormone Gene. Proc. Natl. Acad. Sci. USA 1997, 94, 10862–10867. [Google Scholar] [CrossRef] [PubMed]
- Landa, M.S.; García, S.I.; Schuman, M.L.; Peres Diaz, L.S.; Aisicovich, M.; Pirola, C.J. Cardiovascular and Body Weight Regulation Changes in Transgenic Mice Overexpressing Thyrotropin-Releasing Hormone (TRH). J. Physiol. Biochem. 2020, 76, 599–608. [Google Scholar] [CrossRef] [PubMed]
- Rabeler, R.; Mittag, J.; Geffers, L.; Rüther, U.; Leitges, M.; Parlow, A.F.; Visser, T.J.; Bauer, K. Generation of Thyrotropin-Releasing Hormone Receptor 1-Deficient Mice as an Animal Model of Central Hypothyroidism. Mol. Endocrinol. 2004, 18, 1450–1460. [Google Scholar] [CrossRef] [PubMed]
- Zeng, H.; Schimpf, B.A.; Rohde, A.D.; Pavlova, M.N.; Gragerov, A.; Bergmann, J.E. Thyrotropin-Releasing Hormone Receptor 1-Deficient Mice Display Increased Depression and Anxiety-like Behavior. Mol. Endocrinol. Baltim. Md 2007, 21, 2795–2804. [Google Scholar] [CrossRef] [PubMed]
- Groba, C.; Mayerl, S.; Van Mullem, A.A.; Visser, T.J.; Darras, V.M.; Habenicht, A.J.; Heuer, H. Hypothyroidism Compromises Hypothalamic Leptin Signaling in Mice. Mol. Endocrinol. 2013, 27, 586–597. [Google Scholar] [CrossRef] [PubMed]
- Mayerl, S.; Liebsch, C.; Visser, T.J.; Heuer, H. Absence of TRH Receptor 1 in Male Mice Affects Gastric Ghrelin Production. Endocrinology 2015, 156, 755–767. [Google Scholar] [CrossRef] [PubMed]
- Cummings, D.E. Ghrelin and the Short- and Long-Term Regulation of Appetite and Body Weight. Physiol. Behav. 2006, 89, 71–84. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Liu, C.; Uchida, A.; Chuang, J.-C.; Walker, A.; Liu, T.; Osborne-Lawrence, S.; Mason, B.L.; Mosher, C.; Berglund, E.D.; et al. Arcuate AgRP Neurons Mediate Orexigenic and Glucoregulatory Actions of Ghrelin. Mol. Metab. 2014, 3, 64–72. [Google Scholar] [CrossRef]
- Liu, X.-G.; Tan, L.-J.; Lei, S.-F.; Liu, Y.-J.; Shen, H.; Wang, L.; Yan, H.; Guo, Y.-F.; Xiong, D.-H.; Chen, X.-D.; et al. Genome-Wide Association and Replication Studies Identified TRHR as an Important Gene for Lean Body Mass. Am. J. Hum. Genet. 2009, 84, 418–423. [Google Scholar] [CrossRef]
- Lunardi, C.C.; Lima, R.M.; Pereira, R.W.; Leite, T.K.M.; Siqueira, A.B.M.; Oliveira, R.J. Association between Polymorphisms in the TRHR Gene, Fat-Free Mass, and Muscle Strength in Older Women. AGE 2013, 35, 2477–2483. [Google Scholar] [CrossRef] [PubMed]
- Semenova, E.A.; Hall, E.C.R.; Ahmetov, I.I. Genes and Athletic Performance: The 2023 Update. Genes 2023, 14, 1235. [Google Scholar] [CrossRef] [PubMed]
- Chagnon, Y.C.; Rice, T.; Pérusse, L.; Borecki, I.B.; Ho-Kim, M.-A.; Lacaille, M.; Paré, C.; Bouchard, L.; Gagnon, J.; Leon, A.S.; et al. Genomic Scan for Genes Affecting Body Composition before and after Training in Caucasians from HERITAGE. J. Appl. Physiol. 2001, 90, 1777–1787. [Google Scholar] [CrossRef] [PubMed]
- Platte, P.; Papanicolaou, G.J.; Johnston, J.; Klein, C.M.; Doheny, K.F.; Pugh, E.W.; Roy-Gagnon, M.-H.; Stunkard, A.J.; Francomano, C.A.; Wilson, A.F. A Study of Linkage and Association of Body Mass Index in the Old Order Amish. Am. J. Med. Genet. C Semin. Med. Genet. 2003, 121C, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Thirunarayanan, N.; Nir, E.A.; Raaka, B.M.; Gershengorn, M.C. Thyrotropin-Releasing Hormone Receptor Type 1 (TRH-R1), Not TRH-R2, Primarily Mediates Taltirelin Actions in the CNS of Mice. Neuropsychopharmacology 2013, 38, 950–956. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Zupan, B.; Raaka, B.M.; Toth, M.; Gershengorn, M.C. TRH-Receptor-Type-2-Deficient Mice Are Euthyroid and Exhibit Increased Depression and Reduced Anxiety Phenotypes. Neuropsychopharmacology 2009, 34, 1601–1608. [Google Scholar] [CrossRef] [PubMed]
- Lamberton, R.P.; Lechan, R.M.; Jackson, I.M.D. Ontogeny of Thyrotropin-Releasing Hormone and Histidyl Proline Diketopiperazine in the Rat Central Nervous System and Pancreas. Endocrinology 1984, 115, 2400–2405. [Google Scholar] [CrossRef] [PubMed]
- Prasad, C. Limited Proteolysis and Physiological Regulation: An Example from Thyrotropin-Releasing Hormone Metabolism. Thyroid 1998, 8, 969–975. [Google Scholar] [CrossRef] [PubMed]
- Yamada, M.; Shibusawa, N.; Hashida, T.; Satoh, T.; Monden, T.; Prasad, C.; Mori, M. Abundance of Cyclo (His-Pro)-Like Immunoreactivity in the Brain of TRH-Deficient Mice. Endocrinology 1999, 140, 538–541. [Google Scholar] [CrossRef]
- Lazcano, I.; Uribe, R.M.; Martínez-Chávez, E.; Vargas, M.A.; Matziari, M.; Joseph-Bravo, P.; Charli, J.-L. Pyroglutamyl Peptidase II Inhibition Enhances the Analeptic Effect of Thyrotropin-Releasing Hormone in the Rat Medial Septum. J. Pharmacol. Exp. Ther. 2012, 342, 222–231. [Google Scholar] [CrossRef]
- Tang, T.; Li, L.; Tang, J.; Li, Y.; Lin, W.Y.; Martin, F.; Grant, D.; Solloway, M.; Parker, L.; Ye, W.; et al. A Mouse Knockout Library for Secreted and Transmembrane Proteins. Nat. Biotechnol. 2010, 28, 749–755. [Google Scholar] [CrossRef] [PubMed]
- Michaud, J.L.; Rosenquist, T.; May, N.R.; Fan, C.-M. Development of Neuroendocrine Lineages Requires the bHLH–PAS Transcription Factor SIM1. Genes Dev. 1998, 12, 3264–3275. [Google Scholar] [CrossRef]
- Balthasar, N.; Dalgaard, L.T.; Lee, C.E.; Yu, J.; Funahashi, H.; Williams, T.; Ferreira, M.; Tang, V.; McGovern, R.A.; Kenny, C.D.; et al. Divergence of Melanocortin Pathways in the Control of Food Intake and Energy Expenditure. Cell 2005, 123, 493–505. [Google Scholar] [CrossRef] [PubMed]
- Kublaoui, B.M.; Holder, J.L.; Tolson, K.P.; Gemelli, T.; Zinn, A.R. SIM1 Overexpression Partially Rescues Agouti Yellow and Diet-Induced Obesity by Normalizing Food Intake. Endocrinology 2006, 147, 4542–4549. [Google Scholar] [CrossRef]
- Yang, C.; Gagnon, D.; Vachon, P.; Tremblay, A.; Levy, E.; Massie, B.; Michaud, J.L. Adenoviral-Mediated Modulation of Sim1 Expression in the Paraventricular Nucleus Affects Food Intake. J. Neurosci. 2006, 26, 7116–7120. [Google Scholar] [CrossRef]
- Xi, D.; Gandhi, N.; Lai, M.; Kublaoui, B.M. Ablation of Sim1 Neurons Causes Obesity through Hyperphagia and Reduced Energy Expenditure. PLoS ONE 2012, 7, e36453. [Google Scholar] [CrossRef]
- Simmons, D.M.; Swanson, L.W. Comparison of the Spatial Distribution of Seven Types of Neuroendocrine Neurons in the Rat Paraventricular Nucleus: Toward a Global 3D Model. J. Comp. Neurol. 2009, 516, 423–441. [Google Scholar] [CrossRef] [PubMed]
- Berkhout, J.B.; Poormoghadam, D.; Yi, C.; Kalsbeek, A.; Meijer, O.C.; Mahfouz, A. An Integrated Single-cell RNA -seq Atlas of the Mouse Hypothalamic Paraventricular Nucleus Links Transcriptomic and Functional Types. J. Neuroendocrinol. 2024, 36, e13367. [Google Scholar] [CrossRef]
- Joseph-Bravo, P.; Gutiérrez-Mariscal, M.; Jaimes-Hoy, L.; Charli, J.-L. Thyroid Axis and Energy Balance: Focus on Animals and Implications for Humankind. In Handbook of Famine, Starvation, and Nutrient Deprivation; Preedy, V., Patel, V.B., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 1–28. ISBN 978-3-319-40007-5. [Google Scholar]
- Lechan, R.M.; Fekete, C. The TRH Neuron: A Hypothalamic Integrator of Energy Metabolism. In Progress in Brain Research; Elsevier: Amsterdam, The Netherlands, 2006; Volume 153, pp. 209–235. ISBN 978-0-444-52261-0. [Google Scholar]
- Ghamari-Langroudi, M.; Vella, K.R.; Srisai, D.; Sugrue, M.L.; Hollenberg, A.N.; Cone, R.D. Regulation of Thyrotropin-Releasing Hormone-Expressing Neurons in Paraventricular Nucleus of the Hypothalamus by Signals of Adiposity. Mol. Endocrinol. 2010, 24, 2366–2381. [Google Scholar] [CrossRef]
- Kádár, A.; Sánchez, E.; Wittmann, G.; Singru, P.S.; Füzesi, T.; Marsili, A.; Larsen, P.R.; Liposits, Z.; Lechan, R.M.; Fekete, C. Distribution of Hypophysiotropic Thyrotropin-releasing Hormone (TRH)-synthesizing Neurons in the Hypothalamic Paraventricular Nucleus of the Mouse. J. Comp. Neurol. 2010, 518, 3948–3961. [Google Scholar] [CrossRef]
- Füzesi, T.; Wittmann, G.; Lechan, R.M.; Liposits, Z.; Fekete, C. Noradrenergic Innervation of Hypophysiotropic Thyrotropin-Releasing Hormone-Synthesizing Neurons in Rats. Brain Res. 2009, 1294, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Salas, E.; Aceves, C.; Anguiano, B.; Uribe, R.M.; García-Luna, C.; Sánchez, E.; De Gortari, P. Food-Restricted and Dehydrated-Induced Anorexic Rats Present Differential TRH Expression in Anterior and Caudal PVN. Role of Type 2 Deiodinase and Pyroglutamyl Aminopeptidase II. Endocrinology 2012, 153, 4067–4076. [Google Scholar] [CrossRef] [PubMed]
- Wittmann, G.; Füzesi, T.; Singru, P.S.; Liposits, Z.; Lechan, R.M.; Fekete, C. Efferent Projections of Thyrotropin-releasing Hormone-synthesizing Neurons Residing in the Anterior Parvocellular Subdivision of the Hypothalamic Paraventricular Nucleus. J. Comp. Neurol. 2009, 515, 313–330. [Google Scholar] [CrossRef] [PubMed]
- Lyons, D.J.; Horjales-Araujo, E.; Broberger, C. Synchronized Network Oscillations in Rat Tuberoinfundibular Dopamine Neurons: Switch to Tonic Discharge by Thyrotropin-Releasing Hormone. Neuron 2010, 65, 217–229. [Google Scholar] [CrossRef] [PubMed]
- Ebling, F.J.P.; Barrett, P. The Regulation of Seasonal Changes in Food Intake and Body Weight. J. Neuroendocrinol. 2008, 20, 827–833. [Google Scholar] [CrossRef] [PubMed]
- Vargas, Y.; Parra-Montes De Oca, M.; Sánchez-Jaramillo, E.; Jaimes-Hoy, L.; Sánchez-Islas, E.; Uribe, R.M.; Joseph-Bravo, P.; Charli, J.-L. Sex-Dependent and -Independent Regulation of Thyrotropin-Releasing Hormone Expression in the Hypothalamic Dorsomedial Nucleus by Negative Energy Balance, Exercise, and Chronic Stress. Brain Res. 2022, 1796, 148083. [Google Scholar] [CrossRef] [PubMed]
- Krashes, M.J.; Shah, B.P.; Madara, J.C.; Olson, D.P.; Strochlic, D.E.; Garfield, A.S.; Vong, L.; Pei, H.; Watabe-Uchida, M.; Uchida, N.; et al. An Excitatory Paraventricular Nucleus to AgRP Neuron Circuit That Drives Hunger. Nature 2014, 507, 238–242. [Google Scholar] [CrossRef]
- Grzelka, K.; Wilhelms, H.; Dodt, S.; Dreisow, M.-L.; Madara, J.C.; Walker, S.J.; Wu, C.; Wang, D.; Lowell, B.B.; Fenselau, H. A Synaptic Amplifier of Hunger for Regaining Body Weight in the Hypothalamus. Cell Metab. 2023, 35, 770–785.e5. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Van Den Pol, A.N. Thyrotropin-Releasing Hormone (TRH) Inhibits Melanin-Concentrating Hormone Neurons: Implications for TRH-Mediated Anorexic and Arousal Actions. J. Neurosci. 2012, 32, 3032–3043. [Google Scholar] [CrossRef]
- Péterfi, Z.; Farkas, E.; Nagyunyomi-Sényi, K.; Kádár, A.; Ottó, S.; Horváth, A.; Füzesi, T.; Lechan, R.M.; Fekete, C. Role of TRH/UCN3 Neurons of the Perifornical Area/Bed Nucleus of Stria Terminalis Region in the Regulation of the Anorexigenic POMC Neurons of the Arcuate Nucleus in Male Mice and Rats. Brain Struct. Funct. 2017, 223, 1329–1341. [Google Scholar] [CrossRef]
- Horjales-Araujo, E.; Hellysaz, A.; Broberger, C. Lateral Hypothalamic Thyrotropin-Releasing Hormone Neurons: Distribution and Relationship to Histochemically Defined Cell Populations in the Rat. Neuroscience 2014, 277, 87–102. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Kohno, H.; Sakurada, T.; Tadano, T.; Kisara, K. Intracranial Injection of Thyrotropin Releasing Hormone (TRH) Suppresses Starvation-Induced Feeding and Drinking in Rats. Pharmacol. Biochem. Behav. 1982, 17, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Imoto, D.; Yamamoto, I.; Matsunaga, H.; Yonekura, T.; Lee, M.-L.; Kato, K.X.; Yamasaki, T.; Xu, S.; Ishimoto, T.; Yamagata, S.; et al. Refeeding activates neurons in the dorsomedial hypothalamus to inhibit food intake and promote positive valence. Mol. Metab. 2021, 54, 101366. [Google Scholar] [CrossRef] [PubMed]
- Wittmann, G.; Füzesi, T.; Liposits, Z.; Lechan, R.M.; Fekete, C. Distribution and Axonal Projections of Neurons Coexpressing Thyrotropin-releasing Hormone and Urocortin 3 in the Rat Brain. J. Comp. Neurol. 2009, 517, 825–840. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Jaramillo, E.; Wittmann, G.; Menyhért, J.; Singru, P.; Gómez-González, G.B.; Sánchez-Islas, E.; Yáñez-Recendis, N.; Pimentel-Cabrera, J.A.; León-Olea, M.; Gereben, B.; et al. Origin of Thyrotropin-Releasing Hormone Neurons That Innervate the Tuberomammillary Nuclei. Brain Struct. Funct. 2022, 227, 2329–2347. [Google Scholar] [CrossRef] [PubMed]
- Gotoh, K.; Fukagawa, K.; Fukagawa, T.; Noguchi, H.; Kakuma, T.; Sakata, T.; Yoshimatsu, H. Hypothalamic Neuronal Histamine Mediates the Thyrotropin-releasing Hormone-induced Suppression of Food Intake. J. Neurochem. 2007, 103, 1102–1110. [Google Scholar] [CrossRef] [PubMed]
- Gotoh, K.; Masaki, T.; Chiba, S.; Ando, H.; Shimasaki, T.; Mitsutomi, K.; Fujiwara, K.; Katsuragi, I.; Kakuma, T.; Sakata, T.; et al. Nesfatin-1, Corticotropin-releasing Hormone, Thyrotropin-releasing Hormone, and Neuronal Histamine Interact in the Hypothalamus to Regulate Feeding Behavior. J. Neurochem. 2013, 124, 90–99. [Google Scholar] [CrossRef] [PubMed]
- Khouma, A.; Moeini, M.M.; Plamondon, J.; Richard, D.; Caron, A.; Michael, N.J. Histaminergic Regulation of Food Intake. Front. Endocrinol. 2023, 14, 1202089. [Google Scholar] [CrossRef] [PubMed]
- Shian, L.R.; Wu, M.H.; Lin, M.T.; Ho, L.T. Hypothalamic Involvement in the Locomotor Stimulant or Satiety Action of Thyrotropin-Releasing Hormone and Amphetamine. Pharmacology 1985, 30, 259–265. [Google Scholar] [CrossRef]
- Uribe, R.M.; Jaimes-Hoy, L.; Ramírez-Martínez, C.; García-Vázquez, A.; Romero, F.; Cisneros, M.; Cote-Vélez, A.; Charli, J.-L.; Joseph-Bravo, P. Voluntary Exercise Adapts the Hypothalamus-Pituitary-Thyroid Axis in Male Rats. Endocrinology 2014, 155, 2020–2030. [Google Scholar] [CrossRef]
- Webster, A.N.; Becker, J.J.; Li, C.; Schwalbe, D.C.; Kerspern, D.; Karolczak, E.O.; Godschall, E.N.; Belmont-Rausch, D.M.; Pers, T.H.; Lutas, A.; et al. Molecular Connectomics Reveals a Glucagon-Like Peptide 1 Sensitive Neural Circuit for Satiety. bioRxiv, 2023; Preprint. [Google Scholar] [CrossRef]
- Hökfelt, T.; Fuxe, K.; Johansson, O.; Jeffcoate, S.; White, N. Distribution of thyrotropin-releasing hormone (TRH) in the central nervous system as revealed with immunohistochemistry. Eur. J. Pharmacol. 1975, 34, 389–392. [Google Scholar] [CrossRef] [PubMed]
- Pazos, A.; Cortés, R.; Palacios, J.M. Thyrotropin-Releasing Hormone Receptor Binding Sites: Autoradiographic Distribution in the Rat and Guinea Pig Brain. J. Neurochem. 1985, 45, 1448–1463. [Google Scholar] [CrossRef] [PubMed]
- Calzá, L.; Giardino, L.; Ceccatelli, S.; Zanni, M.; Elde, R.; Hökfelt, T. Distribution of Thyrotropin-Releasing Hormone Receptor Messenger RNA in the Rat Brain: An in Situ Hybridization Study. Neuroscience 1992, 51, 891–909. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Salas, E.; Gama, F.; Matamoros-Trejo, G.; Amaya, M.; De Gortari, P. TRH in the Nucleus Accumbens Acts Downstream to α-MSH to Decrease Food Intake in Rats. Neurosci. Lett. 2020, 739, 135403. [Google Scholar] [CrossRef] [PubMed]
- Lynn, R.B.; Kreider, M.S.; Miselis, R.R. Thyrotropin-releasing Hormone-immunoreactive Projections to the Dorsal Motor Nucleus and the Nucleus of the Solitary Tract of the Rat. J. Comp. Neurol. 1991, 311, 271–288. [Google Scholar] [CrossRef] [PubMed]
- Palkovits, M.; Mezey, É.; Eskay, R.L.; Brownstein, M.J. Innervation of the Nucleus of the Solitary Tract and the Dorsal Vagal Nucleus by Thyrotropin-Releasing Hormone-Containing Raphe Neurons. Brain Res. 1986, 373, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Rinaman, L.; Miselis, R.R.; Kreider, M.S. Ultrastructural Localization of Thyrotropin-Releasing Hormone Immunoreactivity in the Dorsal Vagal Complex in Rat. Neurosci. Lett. 1989, 104, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Rinaman, L.; Miselis, R.R. Thyrotropin-releasing Hormone-immunoreactive Nerve Terminals Synapse on the Dendrites of Gastric Vagal Motoneurons in the Rat. J. Comp. Neurol. 1990, 294, 235–251. [Google Scholar] [CrossRef] [PubMed]
- Manaker, S.; Rizio, G. Autoradiographic Localization of Thyrotropin-releasing Hormone and Substance p Receptors in the Rat Dorsal Vagal Complex. J. Comp. Neurol. 1989, 290, 516–526. [Google Scholar] [CrossRef]
- Zheng, H.; Berthoud, H.-R. Functional Vagal Input to Gastric Myenteric Plexus as Assessed by Vagal Stimulation-Induced Fos Expression. Am. J. Physiol.-Gastrointest. Liver Physiol. 2000, 279, G73–G81. [Google Scholar] [CrossRef]
- McCann, M.J.; Hermann, G.E.; Rogers, R.C. Thyrotropin-Releasing Hormone: Effects on Identified Neurons of the Dorsal Vagal Complex. J. Auton. Nerv. Syst. 1989, 26, 107–112. [Google Scholar] [CrossRef]
- Raggenbass, M.; Vozzi, C.; Tribollet, E.; Dubois-Dauphin, M.; Dreifuss, J.J. Thyrotropin-Releasing Hormone Causes Direct Excitation of Dorsal Vagal and Solitary Tract Neurones in Rat Brainstem Slices. Brain Res. 1990, 530, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Somiya, H.; Tonoue, T. Neuropeptides as Central Integrators of Autonomic Nerve Activity: Effects of TRH, SRIF, VIP and Bombesin on Gastric and Adrenal Nerves. Regul. Pept. 1984, 9, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Taché, Y.; Goto, Y.; Hamel, D.; Pekary, A.; Novin, D. Mechanisms Underlying Intracisternal TRH-Induced Stimulation of Gastric Acid Secretion in Rats. Regul. Pept. 1985, 13, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.J.; Wei, J.Y.; Taché, Y. Intracisternal TRH and RX 77368 Potently Activate Gastric Vagal Efferent Discharge in Rats. Peptides 1997, 18, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Taché, Y.; Vale, W.; Brown, M. Thyrotropin-Releasing Hormone—CNS Action to Stimulate Gastric Acid Secretion. Nature 1980, 287, 149–151. [Google Scholar] [CrossRef] [PubMed]
- Miampamba, M.; Yang, H.; Sharkey, K.A.; Taché, Y. Intracisternal TRH Analog Induces Fos Expression in Gastric Myenteric Neurons and Glia in Conscious Rats. Am. J. Physiol.-Gastrointest. Liver Physiol. 2001, 280, G979–G991. [Google Scholar] [CrossRef] [PubMed]
- Ao, Y.; Go, V.L.W.; Toy, N.; Li, T.; Wang, Y.; Song, M.K.; Reeve, J.R.; Liu, Y.; Yang, H. Brainstem Thyrotropin-Releasing Hormone Regulates Food Intake through Vagal-Dependent Cholinergic Stimulation of Ghrelin Secretion. Endocrinology 2006, 147, 6004–6010. [Google Scholar] [CrossRef] [PubMed]
- Vogel, R.A.; Cooper, B.R.; Barlow, T.S.; Prange, A.J.; Mueller, R.A.; Breese, G.R. Effects of Thyrotropin-Releasing Hormone on Locomotor Activity, Operant Performance and Ingestive Behavior. J. Pharmacol. Exp. Ther. 1979, 208, 161–168. [Google Scholar]
- Lin, M.T.; Chu, P.C.; Leu, S.Y. Effects of TSH, TRH, LH and LHRH on Thermoregulation and Food and Water Intake in the Rat. Neuroendocrinology 1983, 37, 206–211. [Google Scholar] [CrossRef]
- Buckley, C.; MacDonald, E.E.; Tuziak, S.M.; Volkoff, H. Molecular Cloning and Characterization of Two Putative Appetite Regulators in Winter Flounder (Pleuronectes americanus): Preprothyrotropin-Releasing Hormone (TRH) and Preproorexin (OX). Peptides 2010, 31, 1737–1747. [Google Scholar] [CrossRef] [PubMed]
- Abbott, M.; Volkoff, H. Thyrotropin Releasing Hormone (TRH) in Goldfish (Carassius auratus): Role in the Regulation of Feeding and Locomotor Behaviors and Interactions with the Orexin System and Cocaine- and Amphetamine Regulated Transcript (CART). Horm. Behav. 2011, 59, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Mayorova, T.D.; Tian, S.; Cai, W.; Semmens, D.C.; Odekunle, E.A.; Zandawala, M.; Badi, Y.; Rowe, M.L.; Egertová, M.; Elphick, M.R. Localization of Neuropeptide Gene Expression in Larvae of an Echinoderm, the Starfish Asterias Rubens. Front. Neurosci. 2016, 10, 553. [Google Scholar] [CrossRef] [PubMed]
- Chaiyamoon, A.; Tinikul, R.; Nontunha, N.; Chaichotranunt, S.; Poomtong, T.; Sobhon, P.; Tinikul, Y. Characterization of TRH/GnRH-like Peptides in the Sea Cucumber, Holothuria Scabra, and Their Effects on Oocyte Maturation. Aquaculture 2020, 518, 734814. [Google Scholar] [CrossRef]
- Paxinos, G.; Watson, C. The Rat Brain in Stereotaxic Coordinates, 5th ed.; Elsevier Academic Press: Amsterdam, The Netherlands, 2005; ISBN 978-0-08-047412-0. [Google Scholar]
- Iglesias, R.; Llobera, M.; Montoya, E. Long-Term Effects of TRH Administration on Food Intake and Body Weight in the Rat. Pharmacol. Biochem. Behav. 1986, 24, 1817–1819. [Google Scholar] [CrossRef]
- Choi, Y.-H.; Hartzell, D.; Azain, M.J.; Baile, C.A. TRH Decreases Food Intake and Increases Water Intake and Body Temperature in Rats. Physiol. Behav. 2002, 77, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Pierpaoli, W.; Lesnikov, V.A. Effects of Long-Term Intraperitoneal Injection of Thyrotropin-Releasing Hormone (TRH) on Aging- and Obesity-Related Changes in Body Weight, Lipid Metabolism, and Thyroid Functions. Curr. Aging Sci. 2011, 4, 25–32. [Google Scholar] [CrossRef]
- Konturek, S.J.; Tasler, J.; Jaworek, J.; Dobrzańska, M.; Coy, D.H.; Schally, A.V. Comparison of TRH and Anorexigenic Peptide on Food Intake and Gastrointestinal Secretions. Peptides 1981, 2, 235–240. [Google Scholar] [CrossRef]
- Kong, W.M.; Martin, N.M.; Smith, K.L.; Gardiner, J.V.; Connoley, I.P.; Stephens, D.A.; Dhillo, W.S.; Ghatei, M.A.; Small, C.J.; Bloom, S.R. Triiodothyronine Stimulates Food Intake via the Hypothalamic Ventromedial Nucleus Independent of Changes in Energy Expenditure. Endocrinology 2004, 145, 5252–5258. [Google Scholar] [CrossRef]
- Abraham, G.; Falcou, R.; Rozen, R.; Mandenoff, A.; Autissier, N.; Apfelbaum, M. The Effects of a Constant T3 Level and Thermoneutrality in Diet-Induced Hyperphagia. Horm. Metab. Res. 1987, 19, 96–100. [Google Scholar] [CrossRef]
- Syed, M.A.; Thompson, M.P.; Pachucki, J.; Burmeister, L.A. The Effect of Thyroid Hormone on Size of Fat Depots Accounts for Most of the Changes in Leptin mRNA and Serum Levels in the Rat. Thyroid 1999, 9, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Ishii, S.; Kamegai, J.; Tamura, H.; Shimizu, T.; Sugihara, H.; Oikawa, S. Hypothalamic Neuropeptide Y/Y1 Receptor Pathway Activated by a Reduction in Circulating Leptin, but Not by an Increase in Circulating Ghrelin, Contributes to Hyperphagia Associated with Triiodothyronine-Induced Thyrotoxicosis. Neuroendocrinology 2003, 78, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Ishii, S.; Kamegai, J.; Tamura, H.; Shimizu, T.; Sugihara, H.; Oikawa, S. Triiodothyronine (T3) Stimulates Food Intake via Enhanced Hypothalamic AMP-Activated Kinase Activity. Regul. Pept. 2008, 151, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Barrett, P.; Ebling, F.J.P.; Schuhler, S.; Wilson, D.; Ross, A.W.; Warner, A.; Jethwa, P.; Boelen, A.; Visser, T.J.; Ozanne, D.M.; et al. Hypothalamic Thyroid Hormone Catabolism Acts as a Gatekeeper for the Seasonal Control of Body Weight and Reproduction. Endocrinology 2007, 148, 3608–3617. [Google Scholar] [CrossRef] [PubMed]
- Dhillo, W.S.; Bewick, G.A.; White, N.E.; Gardiner, J.V.; Thompson, E.L.; Bataveljic, A.; Murphy, K.G.; Roy, D.; Patel, N.A.; Scutt, J.N.; et al. The Thyroid Hormone Derivative 3-iodothyronamine Increases Food Intake in Rodents. Diabetes Obes. Metab. 2009, 11, 251–260. [Google Scholar] [CrossRef]
- Vijayan, E.; McCann, S.M. Suppression of feeding and drinking activity in rats following intraventricular injection of thyrotropin releasing hormone (TRH). Endocrinology 1977, 100, 1727–1730. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.E.; Levine, A.S.; Prasad, C. Histidyl-Proline Diketopiperazine Decreases Food Intake in Rats. Brain Res. 1981, 210, 475–478. [Google Scholar] [CrossRef]
- González, Y.; Fernández-Tomé, M.P.; Sánchez-Franco, F.; Del Río, J. Antagonism of Diazepam-Induced Feeding in Rats by Antisera to Opioid Peptides. Life Sci. 1984, 35, 1423–1429. [Google Scholar] [CrossRef] [PubMed]
- Steward, C.A.; Horan, T.L.; Schuhler, S.; Bennett, G.W.; Ebling, F.J.P. Central Administration of Thyrotropin Releasing Hormone (TRH) and Related Peptides Inhibits Feeding Behavior in the Siberian Hamster. NeuroReport 2003, 14, 687–691. [Google Scholar] [CrossRef]
- Akieda-Asai, S.; Poleni, P.-E.; Date, Y. Coinjection of CCK and Leptin Reduces Food Intake via Increased CART/TRH and Reduced AMPK Phosphorylation in the Hypothalamus. Am. J. Physiol.-Endocrinol. Metab. 2014, 306, E1284–E1291. [Google Scholar] [CrossRef]
- Puga, L.; Alcántara-Alonso, V.; Coffeen, U.; Jaimes, O.; De Gortari, P. TRH Injected into the Nucleus Accumbens Shell Releases Dopamine and Reduces Feeding Motivation in Rats. Behav. Brain Res. 2016, 306, 128–136. [Google Scholar] [CrossRef]
- Alvarez-Salas, E.; González, A.; Amaya, M.I.; De Gortari, P. Accumbal TRH Is Downstream of the Effects of Isolation Stress on Hedonic Food Intake in Rats. Nutr. Neurosci. 2021, 24, 554–563. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vargas, Y.; Castro Tron, A.E.; Rodríguez Rodríguez, A.; Uribe, R.M.; Joseph-Bravo, P.; Charli, J.-L. Thyrotropin-Releasing Hormone and Food Intake in Mammals: An Update. Metabolites 2024, 14, 302. https://doi.org/10.3390/metabo14060302
Vargas Y, Castro Tron AE, Rodríguez Rodríguez A, Uribe RM, Joseph-Bravo P, Charli J-L. Thyrotropin-Releasing Hormone and Food Intake in Mammals: An Update. Metabolites. 2024; 14(6):302. https://doi.org/10.3390/metabo14060302
Chicago/Turabian StyleVargas, Yamili, Ana Elena Castro Tron, Adair Rodríguez Rodríguez, Rosa María Uribe, Patricia Joseph-Bravo, and Jean-Louis Charli. 2024. "Thyrotropin-Releasing Hormone and Food Intake in Mammals: An Update" Metabolites 14, no. 6: 302. https://doi.org/10.3390/metabo14060302
APA StyleVargas, Y., Castro Tron, A. E., Rodríguez Rodríguez, A., Uribe, R. M., Joseph-Bravo, P., & Charli, J.-L. (2024). Thyrotropin-Releasing Hormone and Food Intake in Mammals: An Update. Metabolites, 14(6), 302. https://doi.org/10.3390/metabo14060302





