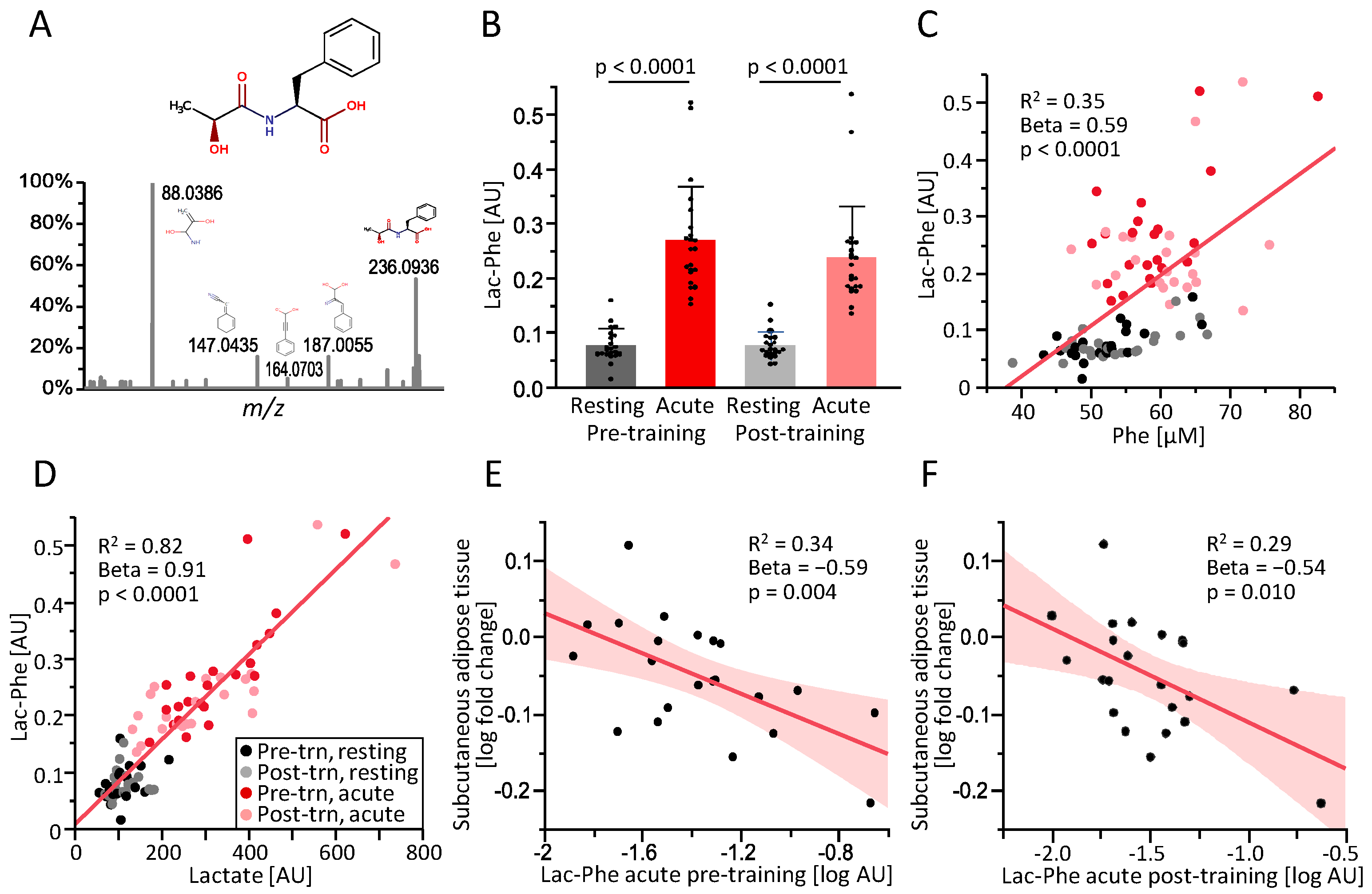
Exercise-Induced N-Lactoylphenylalanine Predicts Adipose Tissue Loss during Endurance Training in Overweight and Obese Humans
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Delahanty, L.M. Weight loss in the prevention and treatment of diabetes. Prev. Med. 2017, 104, 120–123. [Google Scholar] [CrossRef] [PubMed]
- Solomon, T.P.J. Sources of Inter-individual Variability in the Therapeutic Response of Blood Glucose Control to Exercise in Type 2 Diabetes: Going Beyond Exercise Dose. Front. Physiol. 2018, 9, 896. [Google Scholar] [CrossRef] [PubMed]
- O’Donoghue, G.; Kennedy, A.; Andersen, G.S.; Carr, B.; Cleary, S.; Durkan, E.; Davis, H.; Færch, K.; Fitzpatrick, P.; Kenny, H.; et al. Phenotypic Responses to a Lifestyle Intervention Do Not Account for Inter-Individual Variability in Glucose Tolerance for Individuals at High Risk of Type 2 Diabetes. Front. Physiol. 2019, 10, 317. [Google Scholar] [CrossRef] [PubMed]
- Magalhães, J.P.; Hetherington-Rauth, M.; Júdice, P.B.; Correia, I.R.; Rosa, G.B.; Henriques-Neto, D.; Melo, X.; Silva, A.M.; Sardinha, L.B. Interindividual Variability in Fat Mass Response to a 1-Year Randomized Controlled Trial With Different Exercise Intensities in Type 2 Diabetes: Implications on Glycemic Control and Vascular Function. Front. Physiol. 2021, 12, 698971. [Google Scholar] [CrossRef] [PubMed]
- Maurer, J.; Hoene, M.; Weigert, C. Signals from the Circle: Tricarboxylic Acid Cycle Intermediates as Myometabokines. Metabolites 2021, 11, 474. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.R.; Kwon, K.S. Potential Roles of Exercise-Induced Plasma Metabolites Linking Exercise to Health Benefits. Front. Physiol. 2020, 11, 602748. [Google Scholar] [CrossRef] [PubMed]
- Chow, L.S.; Gerszten, R.E.; Tylor, J.M.; Pedersen, B.K.; van Praag, H.; Trappe, S.; Febbraio, M.A.; Galis, Z.S.; Gao, Y.; Haus, J.M.; et al. Exerkines in health, resilience and disease. Nat. Rev. Endocrinol. 2022, 18, 273–289. [Google Scholar] [CrossRef] [PubMed]
- Jansen, R.S.; Addie, R.; Merkx, R.; Fish, A.; Mahakena, S.; Bleijerveld, O.B.; Altelaar, M.; Jlst, L.I.; Wanders, R.J.; Borst, P.; et al. N-lactoyl-amino acids are ubiquitous metabolites that originate from CNDP2-mediated reverse proteolysis of lactate and amino acids. Proc. Natl. Acad. Sci. USA 2015, 112, 6601–6606. [Google Scholar] [CrossRef]
- Li, V.L.; He, Y.; Contrepois, K.; Liu, H.; Kim, J.T.; Wiggenhorn, A.L.; Tanzo, J.T.; Tung, A.S.-H.; Lyu, X.; Zushin, P.-J.H.; et al. An exercise-inducible metabolite that suppresses feeding and obesity. Nature 2022, 606, 785–790. [Google Scholar] [CrossRef]
- Lund, J.; Clemmensen, C.; Schwartz, T.W. Outrunning obesity with Lac-Phe? Cell Metab. 2022, 34, 1085–1087. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, C.; Schneeweiss, P.; Randrianarisoa, E.; Schnauder, G.; Kappler, L.; Machann, J.; Schick, F.; Fritsche, A.; Heni, M.; Birkenfeld, A.; et al. Response of Mitochondrial Respiration in Adipose Tissue and Muscle to 8 Weeks of Endurance Exercise in Obese Subjects. J. Clin. Endocrinol. Metab. 2020, 105, dgaa571. [Google Scholar] [CrossRef] [PubMed]
- Machann, J.; Thamer, C.; Stefan, N.; Schwenzer, N.F.; Kantartzis, K.; Häring, H.U.; Claussen, C.D.; Fritsche, A.; Schick, F. Follow-up Whole-Body Assessment of Adipose Tissue Compartments during a Lifestyle Intervention in a Large Cohort at Increased Risk for Type 2 Diabetes. Radiology 2010, 257, 353–363. [Google Scholar] [CrossRef] [PubMed]
- Würslin, C.; Machann, J.; Rempp, H.; Claussen, C.; Yang, B.; Schick, F. Topography mapping of whole body adipose tissue using a fully automated and standardized procedure. J. Magn. Reson. Imaging 2010, 31, 430–439. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Zeng, Z.; Chen, A.; Lu, X.; Zhao, C.; Hu, C.; Zhou, L.; Liu, X.; Wang, X.; Hou, X.; et al. Comprehensive Strategy to Construct In-House Database for Accurate and Batch Identification of Small Molecular Metabolites. Anal. Chem. 2018, 90, 7635–7643. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, S.F.; Islam, H.; Hazell, T.J. The emerging role of lactate as a mediator of exercise-induced appetite suppression. Am. J. Physiol. Endocrinol. Metab. 2020, 319, E814–E819. [Google Scholar] [CrossRef] [PubMed]
- Schultes, B.; Schmid, S.M.; Wilms, B.; Jauch-Chara, K.; Oltmanns, K.M.; Hallschmid, M. Lactate infusion during euglycemia but not hypoglycemia reduces subsequent food intake in healthy men. Appetite 2012, 58, 818–821. [Google Scholar] [CrossRef] [PubMed]
| Pre-Training | Post-Training | p-Value | |
|---|---|---|---|
| Sex | 14 female/8 male | - | |
| Age [years] | 30 ± 8.9 (19–59) | - | |
| VO2peak/body mass [mL/(kg ∗ min)] | 25.0 ± 4.2 (18.3–32.3) | 26.5 ± 4.7 (16.0–34.9) | 0.042 * |
| BMI [kg/m2] | 31.7 ± 4.5 (27.5–45.5) | 31.3 ± 4.7 (26.3–45.2) | 0.006 * |
| Subcutaneous abdominal adipose tissue [L] | 15.3 ± 5.9 (8.4–32.2) | 14.7 ± 6.1 (7.2–33.1) | 0.006 * |
| Visceral adipose tissue [L] | 3.53 ± 1.65 (0.81–7.26) | 3.38 ± 1.57 (0.94–6.68) | 0.012 * |
| Lean tissue legs [L] | 17.9 ± 4.1 (12.3–27.5) | 18.2 ± 3.9 (13.2–27.7) | 0.034 * |
| Lean tissue arms [L] | 9.73 ± 1.96 (7.31–14.27) | 9.85 ± 2.26 (7.19–14.42) | 0.551 |
| Glucose fasting [mmol/L] | 5.09 ± 0.40 (4.61–6.00) | 5.02 ± 0.40 (4.33–5.61) | 0.336 |
| Training Fold Change | Lac-Phe Pre-Training Acute | Lac-Phe Post-Training Acute | Lactate Pre-Training Acute | Lactate Post-Training Acute |
|---|---|---|---|---|
| Subcutaneous abdominal adipose tissue [L] | Beta = −0.62 p = 0.004 * | Beta = −0.52 p = 0.028 * | Beta = −0.60 p = 0.008 * | Beta = −0.39 p = 0.102 |
| Visceral adipose tissue [L] | Beta = −0.42 p = 0.075 | Beta = −0.48 p = 0.037 * | Beta = −−0.23 p = 0.372 | Beta = −0.37 p = 0.123 |
| BMI [kg/m2] | Beta = −0.25 p = 0.279 | Beta = −0.15 p = 0.538 | Beta = −0.13 p = 0.600 | Beta = 0.07 p = 0.784 |
| Lean tissue legs [L] | Beta = 0.37 p = 0.079 | Beta = 0.22 p = 0.357 | Beta = 0.42 p = 0.047* | Beta = 0.47 p = 0.036 * |
| Lean tissue arms [L] | Beta = 0.14 p = 0.584 | Beta = 0.08 p = 0.758 | Beta = 0.27 p = 0.279 | Beta = 0.08 p = 0.759 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hoene, M.; Zhao, X.; Machann, J.; Birkenfeld, A.L.; Heni, M.; Peter, A.; Niess, A.; Moller, A.; Lehmann, R.; Xu, G.; et al. Exercise-Induced N-Lactoylphenylalanine Predicts Adipose Tissue Loss during Endurance Training in Overweight and Obese Humans. Metabolites 2023, 13, 15. https://doi.org/10.3390/metabo13010015
Hoene M, Zhao X, Machann J, Birkenfeld AL, Heni M, Peter A, Niess A, Moller A, Lehmann R, Xu G, et al. Exercise-Induced N-Lactoylphenylalanine Predicts Adipose Tissue Loss during Endurance Training in Overweight and Obese Humans. Metabolites. 2023; 13(1):15. https://doi.org/10.3390/metabo13010015
Chicago/Turabian StyleHoene, Miriam, Xinjie Zhao, Jürgen Machann, Andreas L. Birkenfeld, Martin Heni, Andreas Peter, Andreas Niess, Anja Moller, Rainer Lehmann, Guowang Xu, and et al. 2023. "Exercise-Induced N-Lactoylphenylalanine Predicts Adipose Tissue Loss during Endurance Training in Overweight and Obese Humans" Metabolites 13, no. 1: 15. https://doi.org/10.3390/metabo13010015
APA StyleHoene, M., Zhao, X., Machann, J., Birkenfeld, A. L., Heni, M., Peter, A., Niess, A., Moller, A., Lehmann, R., Xu, G., & Weigert, C. (2023). Exercise-Induced N-Lactoylphenylalanine Predicts Adipose Tissue Loss during Endurance Training in Overweight and Obese Humans. Metabolites, 13(1), 15. https://doi.org/10.3390/metabo13010015









