Clofazimine as a Treatment for Multidrug-Resistant Tuberculosis: A Review
Abstract
1. Introduction
2. Multidrug-Resistant Tuberculosis
2.1. Epidemiology of MDR-TB
2.2. Treatment of MDR-TB
3. Clofazimine
3.1. Introduction to Clofazimine
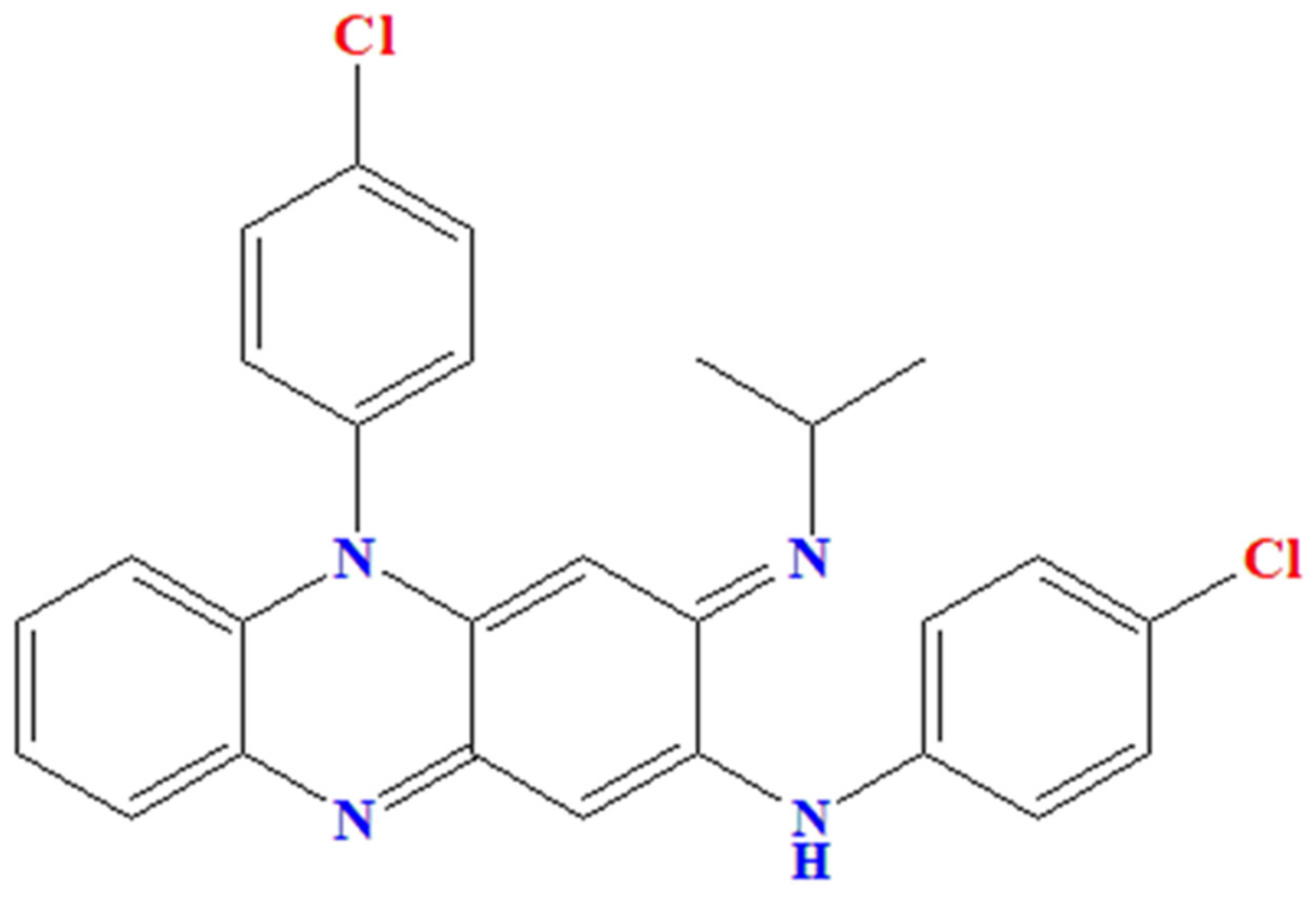
3.2. Chemical Properties of Clofazimine
3.3. Mechanism of Action of Clofazimine
3.4. Synergism Activity of Clofazimine
3.5. Pharmacokinetics of Clofazimine
3.6. Effectivity of Clofazimine for Treating MDR-TB in the Mouse Model Tuberculosis
3.7. Effectivity of Clofazimine for Treating MDR-TB
| Study | Type of Study | Dose and Duration of Clofazimine | Other Drugs included in the Regimen | Outcome | ||
|---|---|---|---|---|---|---|
| Time to Culture Conversion | Cavity Closure | Treatment Success Rate | ||||
| MDR-TB | ||||||
| Van Deun, et al. [12] 2010 | Observational-prospective | Dose: 50 mg (<33 kg) and 100 mg (>33 kg) Duration: Regimen 1: 3 months (intensive phase only) Regimen 2: ≥3 months (intensive phase only) Regimen 3: 3–4 months (intensive phase only) Regimen 4: ≥3 months (intensive phase only) Regimen 5: ≥15 months (intensive and continuation phase) Regimen 6: ≥9 months (intensive and continuation phase) | EMB, GAT, INH, KM, OFX, PTO, PZA | NA | NA | Regimen 1 and 2: 71 of 103 (68.9%) patients were cured Regimen 3: 20 of 35 (57.1%) patients were cured Regimen 4: 30 of 45 (66.7%) patients were cured Regimen 5: 32 of 38 (84.2%) patients were cured Regimen 6: 170 of 206 (82.5%) patients were cured and 11 of 206 (5.3%) had treatment completion (highly significant statistically) |
| Xu, et al. [41] 2012 | Observational-retrospective | Dose: 100 mg, once daily Duration: median 13 months (range 2–25 months) | LFX, MFX, OFX, GAT, PZA, PTO, PA, INH, PAS, CLR, AMK, CM, RFB, LZD, AMX/CLV, RE, AT | Median: 12 weeks (range 2–48 weeks) 22 of 39 patients achieved culture conversion to negative | NA | 15 of 39 (38%) patients had successful treatment |
| Dey, et al. [33] 2013 | Systematic review and meta-analysis | Dose: 50–300 mg, once daily (only stated in 5 studies) Duration: 2–1729 days (only stated in 10 studies) | AMK/CLV, AMK, AMX, CIP, CLR, CM, CYS, EMB, ETO, KM, RIF, SFX, TRD | NA | NA | 16.5–87.8% (11 studies, 3472 patients) had successful treatment Overall pooled proportion of treatment success was 61.96% |
| Aung, et al. [42] 2014 | Observational-prospective | Dose: NA Duration: 9 months | High-dose GTX, EMB, PZA, KM, PTO, INH | At month 2 of treatment, 93% experienced culture conversion | NA | 435 of 515 (84.5%) patients had successful treatment Treatment completion: 50% completed within 272 days (9 months), 75% within 299 days (10 months), 90% within 331 days (11 months), and 95% within 363 days (1 year) |
| Tang, et al. [43] 2015 | Multicenter, prospective, randomized, controlled, and open study (superiority test) | Dose: 100 mg, once daily Duration: 21 months | PTO, PZA, MFX, GAT, LFX, PAS, INHa, CM, AMK, EMB, CLR | Start at 3 months after treatment initiation (earlier in patients who receive CFZ-containing regimen compared with a control group) The proportion of culture-positive patients 60 vs. 75% in months 3 (p = 0.042) | 46 of 53 patients in CFZ-containing regimen vs. 45 of 52 patients in the control group showed cavitary changed Cavity closure starts at 3 months after treatment initiation (earlier in patients who receive CFZ-containing regimen compared with the control group) The proportion of patients having cavity 60 vs. 75% in months 3 (p = 0.047) | 39 of 53 (73.6%) patients in CFZ-containing regimen vs. 28 of 52 (53.8%) patients in control group had successful treatment (p = 0.035) Cured: 27 of 53 (50.9%) vs. 20 of 52 (38.5%) patients Treatment completion: 12 of 53 (22.6%) vs. 8 of 52 (15.4%) patients |
| Dalcolmo, et al. [44] 2017 | Observational-retrospective | Dose: 50 mg (`123+_(≤45 mg) and 100 mg (>45 kg), once daily Duration: 18 months | AMK, OFX, TRD, EMB, STM | NA | NA | 880 of 1446 (60.9%) patients in CFZ-containing regimen vs. 708 of 1096 (64.6%) patients in PZA-containing regimen group had successful treatment (p = 0.054) Cured: 421 of 1446 (29.1%) vs. 384 of 1096 (35%) patients Treatment completion: 459 of 1446 (31.7%) vs. 324 of 1096 (29.6%) patients |
| Duan, et al. [45] 2018 ChiCTR1800014800 | Multicenter and randomized study | Dose: 100 mg, once daily Duration: 24 months | AMK, CM, LFX, PZA, EMB, PAS, PTO, AMX/CLV | Start at 3 months after treatment initiation (earlier in patients who receive CFZ-containing regimen compared with control group) Proportion of culture-positive patients 55 vs. 60% in months 3 (p = 0.0031) | NA | 43 of 66 (65.1%) patients CFZ-containing regimen vs. 35 of 74 (47.3%) patients in control group (p = 0.0034) Cured: 36 of 66 (54.5%) vs. 26 of 74 (35.1%) patients Treatment completion: 7 of 66 (10.6%) vs. 9 of 74 (12.2%) patients |
| Ahmad, et al. [46] 2018 | Meta-analysis | NA | NA | NA | NA | 61% had successful treatment, while 8% had failure or relapse, and 14% died Treatment success was associated positively with the use of linezolid, levofloxacin, carbapenem, moxifloxacin, bedaquiline, and clofazimine |
| Trebucq, et al. [47] 2018 | Observational-prospective | Dose: NA Duration: 9–11 months | KM, MFX, EMB, high-dose INH, PZA, PTO | NA | NA | 821 of 1006 (81.6%) patients had successful treatment Cured: 728 of 1006 (72.4%) patients Treatment completion: 93 of 1006 (9.2%) patients |
| Du, et al. [48] 2019 ChiCTR 1800020391 | Multicenter, prospective, randomized, and controlled study | Dose: NA Duration: 12 months | CM, CYS, LFX, PTO, PZA | Start 3 months after treatment initiation (earlier in patients who receive CFZ-containing short regimen compared with long regimen group) 68.7 vs. 55.9% of patients reached sputum-culture conversion at the end of 3 months of treatment (p = 0.04) The proportion of culture-positive patients around 20 vs. 40% in months 3 | Cavity closure starts at 6 months after treatment initiation (earlier in patients who receive CFZ-containing short regimen compared with long regimen group) The proportion of patients having cavity around 80 vs. 90% in months 6 Cavity closure rate in CFZ-containing short regimen vs. long regimen group were 37.5% vs. 24.1% at the end of treatment (p = 0.06) | 46 of 67 (68.7%) patients CFZ-containing short regimen vs. 44 of 68 (64.7%) patients in long regimen group (p > 0.05) Cured: 42 of 67 (62.7%) vs. 42 of 68 (61.8%) patients Treatment completion: 4 of 67 (6.0%) vs. 2 of 68 (2.9%) patients |
| Harouna, et al. [49] 2019 | Observational-retrospective | Dose: NA Duration: 9–14 months | KM, high-dose GTX, PTO, PZA, medium-high-dose INH, EMB | Start at 1 month after treatment initiation (around 30 adults and 5 children/adolescents reached negative smear-culture conversion in month 1) | NA | 9 month regimen: 88% in adult and 83% in child/adolescent had successful treatment 12 month regimen: 90% in adult and 75% in child/adolescent had successful treatment |
| XDR-TB | ||||||
| Padayatchi, et al. [31] 2014 | Observational-retrospective | Dose: 200–300 mg (based on weight), once daily Duration: NA | PZA, CM, ETO, MFX, PAS, TRD, EMB, INH, AMX/CLV, CLR, RIF, OFX | 20 of 50 (40%) patients in the CFZ-containing regimen group vs. 10 of 35 (28.6%) patients in the control group had culture converted (p = 0.05) Median time: 16.4 vs. 11.9 weeks After 2 months, the probability of culture conversion was higher in the CFZ-containing regimen (around 10 vs. 5%) | Change in CXR score by 6 months was statistically significant | 11 of 85 (12.9%) patients in all group were cured or completed treatment 37 of 85 (43.5%) patients in all group died or were lost to follow-up (no significant difference) (p = 0.493) |
| Wang, et al. [51] 2018 ChiCTR1800014800 | Multicenter, prospective, and randomized study | Dose: 100 mg, once daily Duration: 36 months | CM, MFX, GTX, PZA, EMB, PAS, PTO, LFX, AMK, INH, RIF, OFX | Start at 3 months after treatment initiation Mean time: 19.7 vs. 20.3 months | NA | 8 of 22 (36.4%) patients CFZ-containing regimen vs. 12 of 27 (44.4%) patients in control group had successful treatment Cured: 7 of 22 (31.8%) vs. 6 of 27 (22.2%) patients Treatment completion: 1 of 22 (4.5%) vs. 6 of 27 (22.2%) patients |
3.8. Effectivity of Clofazimine for Treating XDR-TB
3.9. Safety and Tolerability of Clofazimine
3.10. Mechanisms of Resistance to Clofazimine
4. Future of Clofazimine for Treating Multidrug-Resistant Tuberculosis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Brown, E.G.; Dooley, D.S.; Smith, K. Drug-Resistant Tuberculosis: A Survival Guide for Clinicians, 3rd ed.; Curry International Tuberculosis Center: Berkeley, CA, USA, 2016. [Google Scholar]
- World Health Organization. What is New in the WHO Consolidated Guidelines on Drug-Resistant Tuberculosis Treatment? WHO: Geneva, Switzerland, 2019; ISBN 9789241550529. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Core Curriculum on Tuberculosis: What the Clinician Should Know, 6th ed.; CDC: Atlanta, GA, USA, 2013. [Google Scholar]
- World Health Organization. Global Tuberculosis Report 2020; WHO: Geneva, Switzerland, 2020; ISBN 9789240013131. [Google Scholar]
- Cholo, M.C.; Steel, H.C.; Fourie, P.B.; Germishuizen, W.A.; Anderson, R. Clofazimine: Current status and future prospects. J. Antimicrob. Chemother. 2012, 67, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Lange, C.; Dheda, K.; Chesov, D.; Mandalakas, A.M.; Udwadia, Z.; Horsburgh, C.R. Management of drug-resistant tuberculosis. Lancet 2019, 394, 953–966. [Google Scholar] [CrossRef]
- Barry, V.C.; Belton, J.G.; Conalty, M.L. A New Series of Phenazine (Rimino-Compounds) with High Antituberculosis Activity. Nature 1957, 179, 1013–1015. [Google Scholar] [CrossRef] [PubMed]
- Cholo, M.C.; Mothiba, M.T.; Fourie, B.; Anderson, R. Mechanisms of action and therapeutic efficacies of the lipophilic antimycobacterial agents clofazimine and bedaquiline. J. Antimicrob. Chemother. 2017, 72, 338–353. [Google Scholar] [CrossRef] [PubMed]
- Vischer, W.A. The experimental properties of G 30 320 (B 663)—A new anti-leprotic agent. Lepr. Rev. 1969, 40, 107–110. [Google Scholar] [CrossRef] [PubMed]
- Redd, V.M.; O’Sullivan, J.F.; Gangadharam, P.R.J. Antimycobacterial activities of riminophenazines. J. Antimicrob. Chemother. 1999, 43, 615–623. [Google Scholar] [CrossRef] [PubMed]
- Schaad-Lanyi, Z.; Dieterle, W.; Dubois, J.P.; Theobald, W.; Vischer, W. Pharmacokinetics of clofazimine in healthy volunteers. Int. J. Lepr. 1987, 55, 9–15. [Google Scholar]
- Van Deun, A.; Maug, A.K.J.; Salim, M.A.H.; Das, P.K.; Sarker, M.R.; Daru, P.; Rieder, H.L. Short, highly effective, and inexpensive standardized treatment of multidrug-resistant tuberculosis. Am. J. Respir. Crit. Care Med. 2010, 182, 684–692. [Google Scholar] [CrossRef]
- Lange, C.; Chesov, D.; Heyckendorf, J. Clofazimine for the treatment of multidrug-resistant tuberculosis. Clin. Microbiol. Infect. 2019, 25, 128–130. [Google Scholar] [CrossRef]
- World Health Organization. WHO Consolidated Guidelines on Tuberculosis; WHO: Geneva, Switzerland, 2020; ISBN 9789240007048. [Google Scholar]
- Mirnejad, R.; Asadi, A.; Khoshnood, S.; Mirzaei, H.; Heidary, M.; Fattorini, L.; Ghodousi, A.; Darban-Sarokhalil, D. Clofazimine: A useful antibiotic for drug-resistant tuberculosis. Biomed. Pharmacother. 2018, 105, 1353–1359. [Google Scholar] [CrossRef]
- NCBI Clofazimine. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Clofazimine (accessed on 15 December 2020).
- Bopape, M.C.; Steel, H.C.; Cockeran, R.; Matlola, N.M.; Fourie, P.B.; Anderson, R. Antimicrobial activity of clofazimine is not dependent on mycobacterial C-type phospholipases. J. Antimicrob. Chemother. 2004, 53, 971–974. [Google Scholar] [CrossRef][Green Version]
- Fukutomi, Y.; Maeda, Y.; Makino, M. Apoptosis-inducing activity of clofazimine in macrophages. Antimicrob. Agents Chemother. 2011, 55, 4000–4005. [Google Scholar] [CrossRef]
- Lechartier, B.; Cole, S.T. Mode of Action of Clofazimine and Combination Therapy with Benzothiazinones against Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 2015, 59, 4457–4463. [Google Scholar] [CrossRef]
- Diacon, A.H.; Dawson, R.; Von Groote-Bidlingmaier, F.; Symons, G.; Venter, A.; Donald, P.R.; van Niekerk, C.; Everitt, D.; Hutchings, J.; Burger, D.A.; et al. Bactericidal activity of pyrazinamide and clofazimine alone and in combinations with pretomanid and bedaquiline. Am. J. Respir. Crit. Care Med. 2015, 191, 943–953. [Google Scholar] [CrossRef]
- Ammerman, N.C.; Swanson, R.V.; Tapley, A.; Moodley, C.; Ngcobo, B.; Adamson, J.; Dorasamy, A.; Moodley, S.; Mgaga, Z.; Bester, L.A.; et al. Clofazimine has delayed antimicrobial activity against Mycobacterium tuberculosis both in vitro and in vivo. J. Antimicrob. Chemother. 2017, 72, 455–461. [Google Scholar] [CrossRef]
- Li, G.; Xu, Z.; Jiang, Y.; Liu, H.; Zhao, L.-l.; Li, M.; Xu, D.; Zhao, X.; Liu, Z.; Wang, R.; et al. Synergistic activities of clofazimine with moxifloxacin or capreomycin against Mycobacterium tuberculosis in China. Int. J. Antimicrob. Agents 2019, 54, 642–646. [Google Scholar] [CrossRef]
- López-Gavín, A.; Tudó, G.; Vergara, A.; Hurtado, J.C.; Gonzalez-Martín, J. In vitro activity against Mycobacterium tuberculosis of levofloxacin, moxifloxacin and UB-8902 in combination with clofazimine and pretomanid. Int. J. Antimicrob. Agents 2015, 46, 582–585. [Google Scholar] [CrossRef]
- Maartens, G.; Brill, M.J.E.; Pandie, M.; Svensson, E.M. Pharmacokinetic interaction between bedaquiline and clofazimine in patients with drug-resistant tuberculosis. Int. J. Tuberc. Lung Dis. 2018, 22, 26–29. [Google Scholar] [CrossRef]
- Holdiness, M.R. Clinical Pharmacokinetics of Clofazimine: A Review. Clin. Pharmacokinet. 1989, 85, 74–85. [Google Scholar] [CrossRef]
- Nix, D.E.; Adam, R.D.; Auclair, B.; Krueger, T.S.; Godo, P.G.; Peloquin, C.A. Pharmacokinetics and relative bioavailability of clofazimine in relation to food, orange juice and antacid. Tuberculosis 2004, 365–373. [Google Scholar] [CrossRef]
- Baik, J.; Stringer, K.A.; Mane, G.; Rosania, G.R. Multiscale distribution and bioaccumulation analysis of clofazimine reveals a massive immune system-mediated xenobiotic sequestration response. Antimicrob. Agents Chemother. 2013, 57, 1218–1230. [Google Scholar] [CrossRef]
- Silva Miranda, M.; Breiman, A.; Allain, S.; Deknuydt, F.; Altare, F. The tuberculous granuloma: An unsuccessful host defence mechanism providing a safety shelter for the bacteria? Clin. Dev. Immunol. 2012, 2012. [Google Scholar] [CrossRef]
- Prideaux, B.; Via, L.E.; Zimmerman, M.D.; Eum, S.; Sarathy, J.; O’brien, P.; Chen, C.; Kaya, F.; Weiner, D.M.; Chen, P.; et al. The association between sterilizing activity and drug distribution into tuberculosis lesions. Nat. Med. 2015, 21, 1223–1227. [Google Scholar] [CrossRef]
- Te Brake, L.H.M.; Russel, F.G.M.; Van Den Heuvel, J.J.M.W.; De Knegt, G.J.; De Steenwinkel, J.E.; Burger, D.M.; Aarnoutse, R.E.; Koenderink, J.B. Inhibitory potential of tuberculosis drugs on ATP-binding cassette drug transporters. Tuberculosis 2016, 96, 150–157. [Google Scholar] [CrossRef]
- Padayatchi, N.; Gopal, M.; Naidoo, R.; Werner, L.; Naidoo, K.; Master, I.; O’Donnell, M.R.; Donnell, M.R.O. Clofazimine in the treatment of extensively drug-resistant tuberculosis with HIV coinfection in South Africa: A retrospective cohort study. J. Antimicrob. Chemother. 2014, 69, 3103–3107. [Google Scholar] [CrossRef]
- Mitnick, C.D.; Shin, S.S.; Seung, K.J.; Rich, M.L.; Atwood, S.S.; Furin, J.J.; Fitzmaurice, G.M.; Alcantara Viru, F.A.; Appleton, S.C.; Bayona, J.N.; et al. Comprehensive Treatment of Extensively Drug-Resistant Tuberculosis. N. Engl. J. Med. 2008, 359, 563–574. [Google Scholar] [CrossRef]
- Dey, T.; Brigden, G.; Cox, H.; Shubber, Z.; Cooke, G.; Ford, N. Outcomes of clofazimine for the treatment of drug-resistant tuberculosis: A systematic review and meta-analysis. J. Antimicrob. Chemother. 2013, 68, 284–293. [Google Scholar] [CrossRef]
- Grosset, J.H.; Tyagi, S.; Almeida, D.V.; Converse, P.J.; Li, S.Y.; Ammerman, N.C.; Bishai, W.R.; Enarson, D.; Trébucq, A. Assessment of clofazimine activity in a second-line regimen for tuberculosis in mice. Am. J. Respir. Crit. Care Med. 2013, 188, 608–612. [Google Scholar] [CrossRef]
- Ammerman, N.C.; Swanson, R.V.; Bautista, E.M.; Almeida, D.V.; Saini, V.; Omansen, T.F.; Guo, H.; Chang, Y.S.; Li, S.-Y.Y.; Tapley, A.; et al. Impact of clofazimine dosing on treatment shortening of the first-line regimen in a mouse model of tuberculosis. Antimicrob. Agents Chemother. 2018, 62, 1–18. [Google Scholar] [CrossRef]
- Gautam, U.S.; McGillivray, A.; Mehra, S.; Didier, P.J.; Midkiff, C.C.; Kissee, R.S.; Golden, N.A.; Alvarez, X.; Niu, T.; Rengarajan, J.; et al. DosS is required for the complete virulence of mycobacterium tuberculosis in mice with classical granulomatous lesions. Am. J. Respir. Cell Mol. Biol. 2015, 52, 708–716. [Google Scholar] [CrossRef]
- Irwin, S.M.; Gruppo, V.; Brooks, E.; Gilliland, J.; Scherman, M.; Reichlen, M.J.; Leistikow, R.; Kramnik, I.; Nuermberger, E.L.; Voskuil, M.I.; et al. Limited activity of clofazimine as a single drug in a mouse model of tuberculosis exhibiting caseous necrotic granulomas. Antimicrob. Agents Chemother. 2014, 58, 4026–4034. [Google Scholar] [CrossRef] [PubMed]
- Harper, J.; Skerry, C.; Davis, S.L.; Tasneen, R.; Weir, M.; Kramnik, I.; Bishai, W.R.; Pomper, M.G.; Nuermberger, E.L.; Jain, S.K. Mouse model of necrotic tuberculosis granulomas develops hypoxic lesions. J. Infect. Dis. 2012, 205, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Gautam, U.S.; Mehra, S.; Kaushal, D. In-vivo gene signatures of Mycobacterium tuberculosis in C3HeB/FeJ mice. PLoS ONE 2015, 10, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Driver, E.R.; Ryan, G.J.; Hoff, D.R.; Irwin, S.M.; Basaraba, R.J.; Kramnik, I.; Lenaerts, A.J. Evaluation of a mouse model of necrotic granuloma formation using C3HeB/FeJ mice for testing of drugs against Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 2012, 56, 3181–3195. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.-B.B.; Jiang, R.-H.H.; Xiao, H.-P.P. Clofazimine in the treatment of multidrug-resistant tuberculosis. Clin. Microbiol. Infect. 2012, 18, 1104–1110. [Google Scholar] [CrossRef] [PubMed]
- Aung, K.J.M.M.; Van Deun, A.; Declercq, E.; Sarker, M.R.; Das, P.K.; Hossain, M.A.; Rieder, H.L. Successful “9-month Bangladesh regimen” for multidrugresistant tuberculosis among over 500 consecutive patients. Int. J. Tuberc. Lung Dis. 2014, 18, 1180–1187. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Yao, L.; Hao, X.; Liu, Y.; Zeng, L.; Liu, G.; Li, M.; Li, F.; Wu, M.; Zhu, Y.; et al. Clofazimine for the treatment of multidrug-resistant tuberculosis: Prospective, multicenter, randomized controlled study in China. Clin. Infect. Dis. 2015, 60, 1361–1367. [Google Scholar] [CrossRef]
- Dalcolmo, M.; Gayoso, R.; Sotgiu, G.; D’Ambrosio, L.; Rocha, J.L.; Borga, L.; Fandinho, F.; Braga, J.U.; Galesi, V.M.N.N.; Barreira, D.; et al. Effectiveness and safety of clofazimine in multidrug-resistant tuberculosis: A nationwide report from Brazil. Eur. Respir. J. 2017, 49, 9–13. [Google Scholar] [CrossRef]
- Duan, H.; Chen, X.; Li, Z.; Pang, Y.; Jing, W.; Liu, P.; Wu, T.; Cai, C.; Shi, J.; Qin, Z.; et al. Clofazimine improves clinical outcomes in multidrug-resistant tuberculosis: A randomized controlled trial. Clin. Microbiol. Infect. 2019, 25, 190–195. [Google Scholar] [CrossRef]
- Ahmad, N.; Ahuja, S.D.; Akkerman, O.W.; Alffenaar, J.-W.C.; Anderson, L.F.; Baghaei, P.; Bang, D.; Barry, P.M.; Bastos, M.L.; Behera, D.; et al. Treatment correlates of successful outcomes in pulmonary multidrug-resistant tuberculosis: An individual patient data meta- analysis. Lancet 2018, 392, 821–834. [Google Scholar] [CrossRef]
- Trebucq, A.; Schwoebel, V.; Kashongwe, Z.; Bakayoko, A.; Kuaban, C.; Noeske, J.; Hassane, S.; Souleymane, B.; Piubello, A.; Ciza, F.; et al. Treatment outcome with a short multidrug-resistant tuberculosis regimen in nine African countries. Int. J. Tuberc. Lung Dis. 2018, 22, 17–25. [Google Scholar] [CrossRef]
- Du, Y.; Qiu, C.; Chen, X.; Wang, J.J.; Jing, W.; Pan, H.; Chen, W.; Liu, Y.; Li, C.; Xi, X.; et al. Treatment outcome of a shorter regimen containing clofazimine for multidrug-resistant tuberculosis: A randomized control trial in China. Clin. Infect. Dis. 2019, 1–8. [Google Scholar] [CrossRef]
- Harouna, S.H.; Souleymane, M.B.; Kizito, W.; Morou, S.; Boukary, I. Short-course treatment outcomes and adverse events in adults and children-adolescents with MDR-TB in Niger. Int. J. Tuberc. Lung Dis. 2019, 23, 625–630. [Google Scholar] [CrossRef]
- Laserson, K.F.; Thorpe, L.E.; Leimane, V.; Weyer, K.; Mitnick, C.D.; Riekstina, V.; Zarovska, E.; Rich, M.L.; Fraser, H.S.F.; Alarcón, E.; et al. Speaking the same language: Treatment outcome definitions for multidrug-resistant tuberculosis. Int. J. Tuberc. Lung Dis. 2005, 9, 640–645. [Google Scholar]
- Wang, Q.; Pang, Y.; Jing, W.; Liu, Y.; Wang, N.; Yin, H.; Zhang, Q.; Ye, Z.; Zhu, M.; Li, F.; et al. Clofazimine for treatment of extensively drug-resistant pulmonary tuberculosis in China. Antimicrob. Agents Chemother. 2018, 62, 1–9. [Google Scholar] [CrossRef]
- Anderson, R.; Theron, A.J.; Nel, J.G.; Durandt, C.; Cholo, M.C.; Feldman, C.; Tintinger, G.R. Clofazimine, but not isoniazid or rifampicin, augments platelet activation in vitro. Front. Pharmacol. 2018, 9, 1–5. [Google Scholar] [CrossRef]
- Gopal, M.; Padayatchi, N.; Metcalfe, J.Z.; O’Donnell, M.R.; Donnell, M.R.O. Systematic review of clofazimine for the treatment of drug-resistant tuberculosis. Int. J. Tuberc. Lung Dis. 2013, 17, 1001–1007. [Google Scholar] [CrossRef]
- Borisov, S.; Danila, E.; Maryandyshev, A.; Dalcolmo, M.; Miliauskas, S.; Kuksa, L.; Manga, S.; Skrahina, A.; Diktanas, S.; Codecasa, L.R.; et al. Surveillance of adverse events in the treatment of drug-resistant tuberculosis: First global report. Eur. Respir. J. 2019, 54, 1901522. [Google Scholar] [CrossRef]
- Zweijpfenning, S.M.H.; Van Groningen, H.; Van Ingen, J.; Magis-Escurra, C.; Boeree, M.J.; Wagner, D.; Bax, H.; Andrejak, C.; Wener, R.; Rahman, A.; et al. Clofazimine does not lead to significant QT interval prolongation: A multicentre study. Eur. Respir. J. 2018, 52, 8–10. [Google Scholar] [CrossRef]
- Lan, Z.; Ahmad, N.; Baghaei, P.; Barkane, L.; Benedetti, A.; Brode, S.K.; Brust, J.C.M.; Campbell, J.R.; Chang, V.W.L.; Falzon, D.; et al. Drug-associated adverse events in the treatment of multidrug-resistant tuberculosis: An individual patient data meta-analysis. Lancet Respir. Med. 2020, 8, 383–394. [Google Scholar] [CrossRef]
- Zhang, S.; Chen, J.; Cui, P.; Shi, W.; Zhang, W.; Zhang, Y. Identification of novel mutations associated with clofazimine resistance in Mycobacterium tuberculosis. J. Antimicrob. Chemother. 2015, 70, 2507–2510. [Google Scholar] [CrossRef] [PubMed]
- Hartkoorn, R.C.; Uplekar, S.; Cole, S.T. Cross-resistance between clofazimine and bedaquiline through upregulation of mmpl5 in mycobacterium tuberculosis. Antimicrob. Agents Chemother. 2014, 58, 2979–2981. [Google Scholar] [CrossRef] [PubMed]
- Somoskovi, A.; Bruderer, V.; Homke, R.; Bloemberg, G.V.; Bottger, E.C. A mutation associated with clofazimine and bedaquiline cross-resistance in MDR-TB following bedaquiline treatment. Eur. Respir. J. 2015, 45, 554–557. [Google Scholar] [CrossRef] [PubMed]
- Pym, A.S.; Diacon, A.H.; Tang, S.J.; Conradie, F.; Danilovits, M.; Chuchottaworn, C.; Vasilyeva, I.; Andries, K.; Bakare, N.; De Marez, T.; et al. Bedaquiline in the treatment of multidrug- and extensively drugresistant tuberculosis. Eur. Respir. J. 2016, 47, 564–574. [Google Scholar] [CrossRef]
- Andries, K.; Villellas, C.; Coeck, N.; Thys, K.; Gevers, T.; Vranckx, L.; Lounis, N.; de Jong, B.C.; Koul, A. Acquired Resistance of Mycobacterium tuberculosis to Bedaquiline. PLoS ONE 2014, 9. [Google Scholar] [CrossRef]
- Nimmo, C.; Millard, J.; van Dorp, L.; Brien, K.; Moodley, S.; Wolf, A.; Grant, A.D.; Padayatchi, N.; Pym, A.S.; Balloux, F.; et al. Population-level emergence of bedaquiline and clofazimine resistance-associated variants among patients with drug-resistant tuberculosis in southern Africa: A phenotypic and phylogenetic analysis. Lancet Microbe 2020, 1, e165–e174. [Google Scholar] [CrossRef]
- Hamidian, M.; Hall, R.M. Origin of the AbGRI1 antibiotic resistance island found in the comM gene of Acinetobacter baumannii GC2 isolates. J. Antimicrob. Chemother. 2017, 72, 2944–2947. [Google Scholar] [CrossRef]
- Nguyen, T.V.A.; Anthony, R.M.; Bañuls, A.L.; Vu, D.H.; Alffenaar, J.W.C. Bedaquiline Resistance: Its Emergence, Mechanism, and Prevention. Clin. Infect. Dis. 2018, 66, 1625–1630. [Google Scholar] [CrossRef]
- Anthony Malinga, L.; Stoltz, A. Efflux Pump Mediated Second-Line Tuberculosis Drug Resistance. Mycobact. Dis. 2016, 6. [Google Scholar] [CrossRef]
- Rodrigues, L.; Cravo, P.; Viveiros, M. Efflux pump inhibitors as a promising adjunct therapy against drug resistant tuberculosis: A new strategy to revisit mycobacterial targets and repurpose old drugs. Expert Rev. Anti. Infect. Ther. 2020, 18, 741–757. [Google Scholar] [CrossRef]
- Gupta, S.; Cohen, K.A.; Winglee, K.; Maiga, M.; Diarra, B.; Bishai, W.R. Efflux inhibition with verapamil potentiates bedaquiline in mycobacterium tuberculosis. Antimicrob. Agents Chemother. 2014, 58, 574–576. [Google Scholar] [CrossRef]
- Lu, Y.; Zheng, M.; Wang, B.; Fu, L.; Zhao, W.; Li, P.; Xu, J.; Zhu, H.; Jin, H.; Yin, D.; et al. Clofazimine analogs with efficacy against experimental tuberculosis and reduced potential for accumulation. Antimicrob. Agents Chemother. 2011, 55, 5185–5193. [Google Scholar] [CrossRef]
- Murashov, M.D.; Diaz-Espinosa, J.; Lalone, V.; Tan, J.W.Y.Y.; Laza, R.; Wang, X.; Stringer, K.A.; Rosania, G.R. Synthesis and characterization of a biomimetic formulation of clofazimine hydrochloride microcrystals for parenteral administration. Pharmaceutics 2018, 10, 238. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nugraha, R.V.; Yunivita, V.; Santoso, P.; Aarnoutse, R.E.; Ruslami, R. Clofazimine as a Treatment for Multidrug-Resistant Tuberculosis: A Review. Sci. Pharm. 2021, 89, 19. https://doi.org/10.3390/scipharm89020019
Nugraha RV, Yunivita V, Santoso P, Aarnoutse RE, Ruslami R. Clofazimine as a Treatment for Multidrug-Resistant Tuberculosis: A Review. Scientia Pharmaceutica. 2021; 89(2):19. https://doi.org/10.3390/scipharm89020019
Chicago/Turabian StyleNugraha, Rhea Veda, Vycke Yunivita, Prayudi Santoso, Rob E. Aarnoutse, and Rovina Ruslami. 2021. "Clofazimine as a Treatment for Multidrug-Resistant Tuberculosis: A Review" Scientia Pharmaceutica 89, no. 2: 19. https://doi.org/10.3390/scipharm89020019
APA StyleNugraha, R. V., Yunivita, V., Santoso, P., Aarnoutse, R. E., & Ruslami, R. (2021). Clofazimine as a Treatment for Multidrug-Resistant Tuberculosis: A Review. Scientia Pharmaceutica, 89(2), 19. https://doi.org/10.3390/scipharm89020019







