Success Factors of Demand-Driven Open Innovation as a Policy Instrument in the Case of the Healthcare Industry
Abstract
1. Introduction
2. Open Innovation in Ecosystems
3. The InDemand Process
3.1. Longitudinal Multiple Case Study
3.2. Data Collection and Methodology
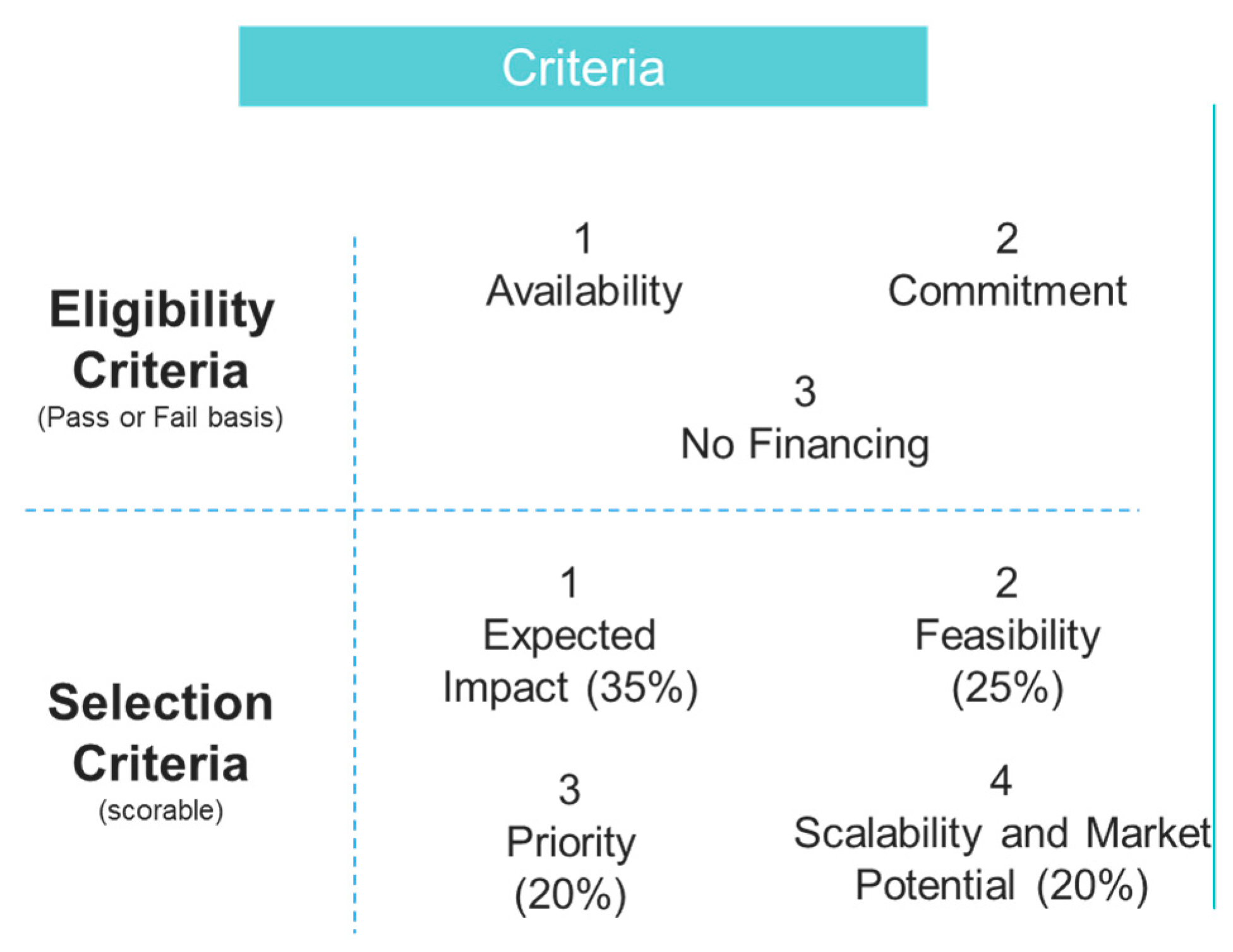
3.3. InDemand Open Innovation Process
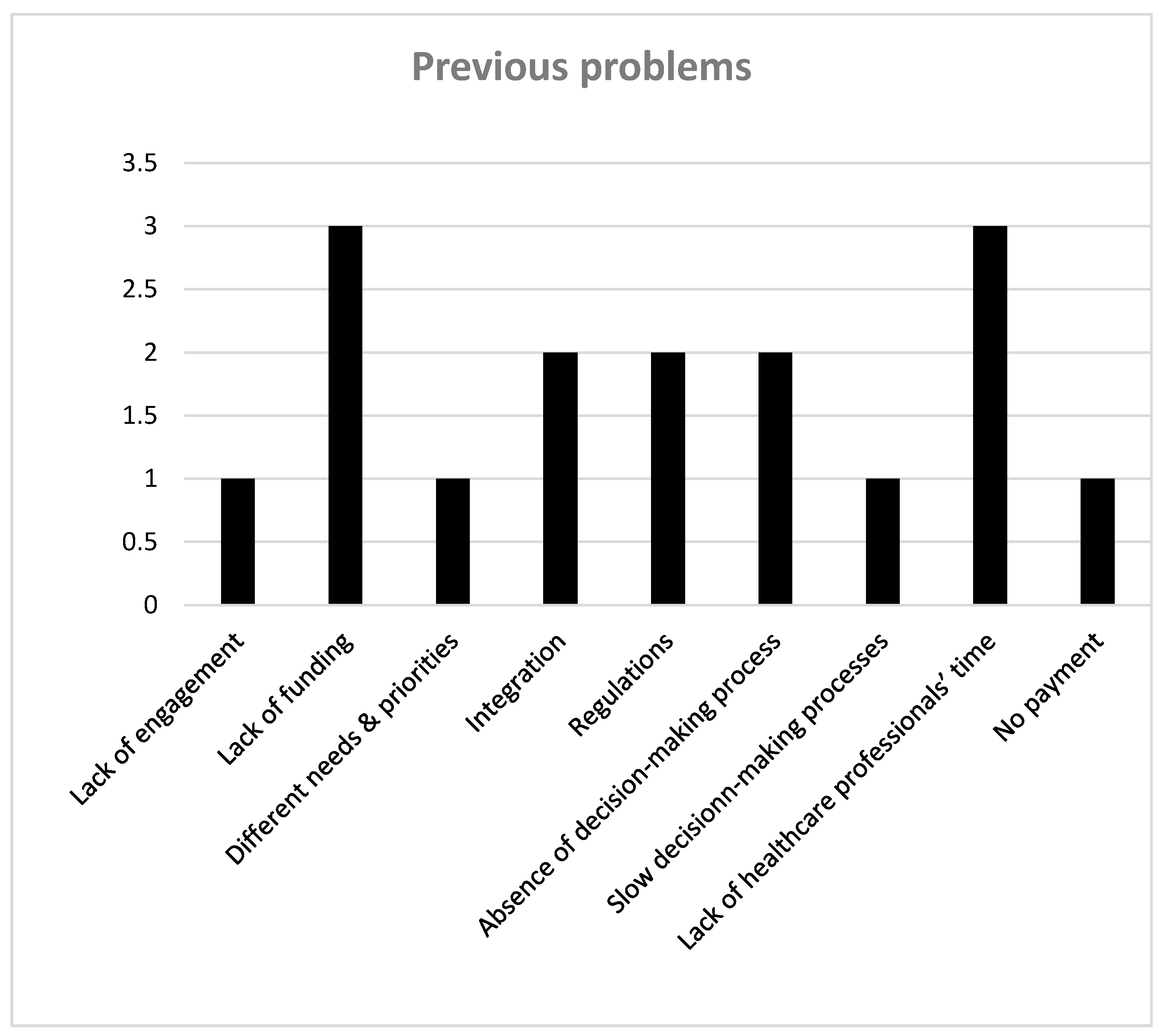
3.4. Previous Challenges of Open Innovation
3.5. Success of Demand-Driven Open Innovation
“The most important thing is to find ‘motivated’ leaders for the challenges”.
“We noted that the challengers are still very motivated to use the tool, which was ultimately proposed by them”.
“This kind of interaction in a completely new role has been very educational and really different”.
“We’ve learnt how to co-create formally, with a formal collaborative framework and now, if we collaborate with others, it would be simpler; we would know what to ask for better”.
4. Demand-Driven Innovation Process as a Policy Instrument
5. Discussion: The Relation between Open Innovation Success Factors and Different Stakeholders
5.1. Impact on Policy-Makers
5.2. Impact on Healthcare Organisations
5.3. Significance for Practitioners
5.4. Impact on Other Sectors
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- WHO. Draft Global Strategy on Digital Health 2020–2024. 2019. Available online: https://www.who.int/docs/defaultsource/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf?sfvrsn=f112ede5_38available10.2.2020 (accessed on 15 May 2020).
- Chesbrough, H. The era of open innovation. MIT Sloan Manag. Rev. 2003, 44, 35–41. [Google Scholar]
- Von Hippel, E. The Sources of Innovation; Oxford University Press: New York, NY, USA, 1988. [Google Scholar]
- Bogers, M.; Zobel, A.-K.; Afuah, A.; Almirall, E.; Brunswicker, S.; Dahlander, L.; Frederiksen, L.; Gawer, A.; Gruber, M.; Haefliger, S.; et al. The open innovation research landscape: Established perspectives and emerging themes across different levels of analysis. Ind. Innov. 2016, 24, 8–40. [Google Scholar]
- Panne, G.; Beers, C.; Kleinknecht, A. Success and failure of innovation: A literature review. Int. J. Innov. Manag. 2003, 7, 309–338. [Google Scholar] [CrossRef]
- Durst, S.; Ståhle, P. Success factors of open innovation—A literature review. Int. J. Bus. Res. Manag. 2013, 4, 111–131. [Google Scholar]
- Von Hippel, E. Horizontal innovation networks—By and for users. Ind. Corp. Chang. 2007, 15, 293–315. [Google Scholar] [CrossRef]
- Chesbrough, H. Open innovation: A new paradigm for understanding industrial innovation. In Open Innovation: Researching a New Paradigm; Chesbrough, H., Vanhaverbeke, W., West, J., Eds.; Oxford University Press: Oxford, UK, 2006; pp. 1–12. [Google Scholar]
- Howells, J. Intermediation and the role of intermediaries in innovation. Res. Policy 2006, 35, 715–728. [Google Scholar] [CrossRef]
- Russell, M.G.; Smorodinskaya, N.V. Leveraging complexity for ecosystemic innovation. Technol. Forecast. Soc. Chang. 2018, 136, 114–131. [Google Scholar] [CrossRef]
- Natalicchio, A.; Ardito, L.; Savino, T.; Albino, V. Managing knowledge assets for open innovation: A systematic literature review. J. Knowl. Manag. 2017, 21, 1362–1383. [Google Scholar] [CrossRef]
- Chesbrough, H.; Vanhaverbeke, W.; West, J. Open Innovation: Researching a New Paradigm; Oxford University Press: New York, NY, USA, 2006. [Google Scholar]
- Richard, E.E.; Davis, J.; Paik, J.H.; Lakhani, K.R. Sustaining Open Innovation through a “Center of Excellence, Strategy and Leadership”; Emerald Publishing Limited: Bentley, UK, 2019; Volume 47, pp. 19–26. [Google Scholar]
- Bullinger, A.C.; Rass, M.; Adamczyk, S.; Moeslein, K.M.; Sohn, S. Open innovation in health care: Analysis of an open health platform. Health Policy 2012, 105, 165–175. [Google Scholar] [CrossRef]
- Dahlander, L.; Gann, D. How open is Innovation. Res. Policy 2010, 39, 699–709. [Google Scholar] [CrossRef]
- Gasco-Hernandez, M.; Sandoval-Almazan, R.; Gil-Garcia, J.R. Open innovation and co-creation in the public sector: Understanding the role of intermediaries. In Electronic Participation, Lecture Notes in Computer Science; Springer: Cham, Switzerland, 2017; Volume 4, pp. 140–148. [Google Scholar]
- Bakici, T.; Almirall, E.; Wareham, J. The role of public open innovation intermediaries in local government and the public sector. Technol. Anal. Strateg. Manag. 2013, 25, 311–327. [Google Scholar] [CrossRef]
- Gassmann, O.; Enkel, E. Towards a Theory of Open Innovation: Three Core Process Archetypes. Available online: https://www.alexandria.unisg.ch/274/ (accessed on 13 May 2020).
- Lee, S.M.; Hwang, T.; Choi, D. Open Innovation in the Public Sector of Leading Countries. Manag. Decis. 2012, 50, 147–162. [Google Scholar] [CrossRef]
- Bommert, B. Collaborative Innovation in the Public Sector. Int. Public Manag. Rev. 2010, 11, 15–33. [Google Scholar]
- Geroski, P.; Machin, S.; Van Reenen, J. The Profitability of Innovating Firms. Rand J. Econ. 1993, 24, 198–211. [Google Scholar] [CrossRef]
- Niehaves, B. Open process innovation. Bus. Process. Manag. J. 2010, 16, 377–393. [Google Scholar] [CrossRef]
- Edvisson, L. Regional intellectual capital in waiting: A strategic intellectual capital quest. In Intellectual Capital for Communities-Nations, Regions and Cities; Bonfour, A., Edvinsson, L., Eds.; Elsevier Butterworth Heinemann: Oxford, UK, 2005. [Google Scholar]
- Lichtenthaler, U.; Hoegl, M.; Muethel, M. Is your company ready for open innovation? MIT Sloan Manag. Rev. 2011, 53, 45–48. [Google Scholar]
- Potel, L.; Alalääkkölä, T.; Sanchez, G. D3.1 Challenge Report of First InDemand Model Iteration. Available online: https://cordis.europa.eu/project/rcn/211099/results/en (accessed on 13 May 2020).
- Yin, R.K. Case Study Research: Design and Methods, 3rd ed.; Sage: Thousand Oaks, CA, USA, 2003. [Google Scholar]
- Jick, T.D. Mixing qualitative and quantitative methods: Triangulation in action, administrative science quarterly. Qual. Methodol. 1979, 24, 602–611. [Google Scholar]
- Garpenby, P.; Bäckman, K. Formal priority setting in health care: The Swedish experience. J. Health Organ. Manag. 2016, 30, 891–907. [Google Scholar] [CrossRef]
- Stevenson, T. Essay Anticipatory action learning: Conversations about the future. Futures 2002, 34, 417–425. [Google Scholar] [CrossRef]
- Malm, H.; López, E. InDemand Deliverable Report: D5.1 Co-Creation and Business Support of the First InDemand Model Iteration. Available online: https://www.indemandhealth.eu/cocreation_business_support_report/ (accessed on 13 May 2020).
- Thunea, T.; Mina, A. Hospitals as innovators in the health-care system: A literature review and research agenda. Res. Policy 2016, 45, 1545–1557. [Google Scholar] [CrossRef]
- Prahalad, C.K.; Ramaswamy, V. Co-creation experiences: The next practice value in creation. J. Interact. Mark. 2004, 18, 5–14. [Google Scholar] [CrossRef]
- Mahra, D.; Lievens, A. Virtual lead user communities: Drivers of knowledge creation for innovation. Res. Policy 2012, 41, 167–177. [Google Scholar] [CrossRef]
- Hao, Y.W.; Geng, B.; Wu, B.; Luyanghe, Z.; Yinyaochen, L. Hospital efficiency and utilization of high-technology medical equipment: A panel data analysis. Health Policy Technol. 2018, 7, 65–72. [Google Scholar]
- Yun, J.J.; Won, D.; Park, K. Entrepreneurial cyclical dynamics of open innovation. J. Evol. Econ. 2018, 28, 1151–1174. [Google Scholar] [CrossRef]
- Secundo, G.; Toma, A.; Schiuma, G.; Passiante, G. Knowledge transfer in open innovation. A classification framework for healthcare ecosystems. Bus. Process Manag. J. 2019, 25, 144–163. [Google Scholar] [CrossRef]
- West, J.; Bogers, M. Leveraging external sources of innovation: A review of research on open innovation. J. Prod. Innov. Manag. 2013, 31, 814–831. [Google Scholar] [CrossRef]
- Yun, J.J.; Liu, Z. Micro- and macro-dynamics of open innovation with a quadruple-helix model. Sustainability 2019, 11, 3301. [Google Scholar] [CrossRef]
- Sahrish, A.; Halim, H.A. Open and closed innovation and enhanced performance of SME hospitals—A conceptual model. Bus. Perspect. Res. 2017, 6, 1–12. [Google Scholar]
- Frow, P.; McColl-Kennedy, J.R.; Payne, A. Co-creation practices: Their role in shaping a health care ecosystem. Ind. Mark. Manag. 2016, 56, 24–39. [Google Scholar] [CrossRef]
- Klijn, H.-E.; Teisman, G.R. Public-private partnership as the management of co-production: Strategic and institutional obstacles in a difficult marriage. In The Challenge of Public-Private Partnerships, Learning from International Experience; Hodge, G., Greve, C., Eds.; Edward Elgar Publishing: Cheltenham, UK, 2005; pp. 95–116. [Google Scholar]
- Yun, J.J.; Park, K.; Gaudio, G.D.; Corte, V.D. Open innovation ecosystems of restaurants: Geographical economics of successful restaurants from three cities. Eur. Plan. Stud. 2020. [Google Scholar] [CrossRef]

| Success Factor | Author |
|---|---|
| Previous experience | Richard, Davis, Paik, et al. [13], Panne, Beers and Kleinknecht [5] |
| Engagement | Richard, Davis, Paik, et al. [13] |
| Recruitment and resources | Durst and Ståhle [6], Richard, Davis, Paik, et al. [13] |
| Training | Richard, Davis, Paik, et al. [13] |
| Communication | Panne, Beers and Kleinknecht [5] |
| Skills, motivation | Panne, Beers and Kleinknecht [5], Durst and Ståhle [6] |
| Good time to market | Panne, Beers and Kleinknecht [5] |
| Trust and compatibility | Durst and Ståhle [6] |
| Governance in the meaning of coordination | Durst and Ståhle [6] |
| Facilitators | Durst and Ståhle [6] |
| Culture | Richard, Davis, Paik, et al. [13] |
| Data Collection | Source | Iteration |
|---|---|---|
| 16 company representatives | Expectation surveys | Co-creation iteration 1 |
| 11 hospital representatives | ||
| 6 intermediate organisations | ||
| 11 company representatives | Individual interviews | Co-creation iteration 1 |
| 11 hospital representatives | ||
| 3 hospital representatives, 3 intermediate organisations, 3 policy-makers | Focus group interviews | Co-creation iteration 1 |
| 26 hospital representatives, 14 companies, 3 policy-makers, 4 intermediate organisations | Co-creation surveys | Co-creation iteration 1 |
| 14 companies, 23 hospital representatives, 4 policy-makers, 4 intermediate organisations | Expectation surveys | Co-creation iteration 2 |
| 18 hospital representatives, 13 companies, 1 policy-maker, 4 intermediate organisations | Co-Creation survey | Co-creation iteration 2 |
| Region | Selected Challenges |
|---|---|
| Spain | |
| Challenge 1 | Need to reduce the risk of patients requiring re-entry to the Intensive Care Unit (ICU) |
| Challenge 2 | Need for a new intervention for children and families addressing education, motivation and adherence |
| Challenge 3 | Need for better patient-doctor communication for epilepsy management |
| Challenge 4 | Need to develop an online platform in the planning, monitoring and evaluation of healthcare education |
| Finland | |
| Challenge 5 | Need for room resource planning support |
| Challenge 6 | Better remote control for children’s asthma examinations |
| Challenge 7 | Better breastfeeding guidance between the hospital and the mother and child clinic |
| Challenge 8 | Need for electronic communication in the case of paediatric and adolescent diabetes care |
| France | |
| Challenge 9 | Optimisation of continuous monitoring of stroke patients in neuro-vascular units |
| Challenge 10 | Need for remote monitoring of real-life patient data to anticipate complications in health status |
| Policy Goal 1: People-Centred Health | |
| Motivation | Companies very motivated due to the great feedback from hospitals |
| Hospital personnel better engaged with the innovation | |
| Solution relevancy | Better solution relevancy due to the continuous hospital feedback |
| Time to market | References from hospitals speed up the involved companies’ access to the market |
| Policy Goal 2: Strengthen the Governance of Digital Health | |
| Governance | Efficient way to bring together a team of multidisciplinary people so that each person in the team contributes with their own knowledge |
| All parties very satisfied with the systemic model; clear roles and responsibilities | |
| Provision of resources | Hospital personnel had difficulties allocating the time for innovation activities, which had a negative impact on the project performance |
| Facilitators | Intermediate organisations ensure that companies transfer the lessons learnt from the co-creation into a new business model to meet the needs of the target market. Funders lower the threshold for companies to take part in open innovation projects. |
| Solution relevancy | The demand-driven innovation process was an efficient way to stimulate the digital health service development and to continuously test the solutions |
| Strategy | The work should be aligned with company, hospital and regional strategy -> supporters’ and funders’ roles were considered important |
| Skills | The demand-driven innovation process increased the networking skills of the involved ecosystem players |
| Policy Goal 3: Promote Global Collaboration and Knowledge Transfer in Digital Health | |
| Governance | An efficient way to bring together a team of multidisciplinary people so that each person in the team contributes with their own knowledge |
| Solution relevancy | It was shown that the demand-driven innovation process resulted in better outcomes than initially expected |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pikkarainen, M.; Hyrkäs, E.; Martin, M. Success Factors of Demand-Driven Open Innovation as a Policy Instrument in the Case of the Healthcare Industry. J. Open Innov. Technol. Mark. Complex. 2020, 6, 39. https://doi.org/10.3390/joitmc6020039
Pikkarainen M, Hyrkäs E, Martin M. Success Factors of Demand-Driven Open Innovation as a Policy Instrument in the Case of the Healthcare Industry. Journal of Open Innovation: Technology, Market, and Complexity. 2020; 6(2):39. https://doi.org/10.3390/joitmc6020039
Chicago/Turabian StylePikkarainen, Minna, Elina Hyrkäs, and Myriam Martin. 2020. "Success Factors of Demand-Driven Open Innovation as a Policy Instrument in the Case of the Healthcare Industry" Journal of Open Innovation: Technology, Market, and Complexity 6, no. 2: 39. https://doi.org/10.3390/joitmc6020039
APA StylePikkarainen, M., Hyrkäs, E., & Martin, M. (2020). Success Factors of Demand-Driven Open Innovation as a Policy Instrument in the Case of the Healthcare Industry. Journal of Open Innovation: Technology, Market, and Complexity, 6(2), 39. https://doi.org/10.3390/joitmc6020039





