The Prevalence and Correlation of Carotid Artery Calcifications and Dental Pulp Stones in a Saudi Arabian Population
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Selection
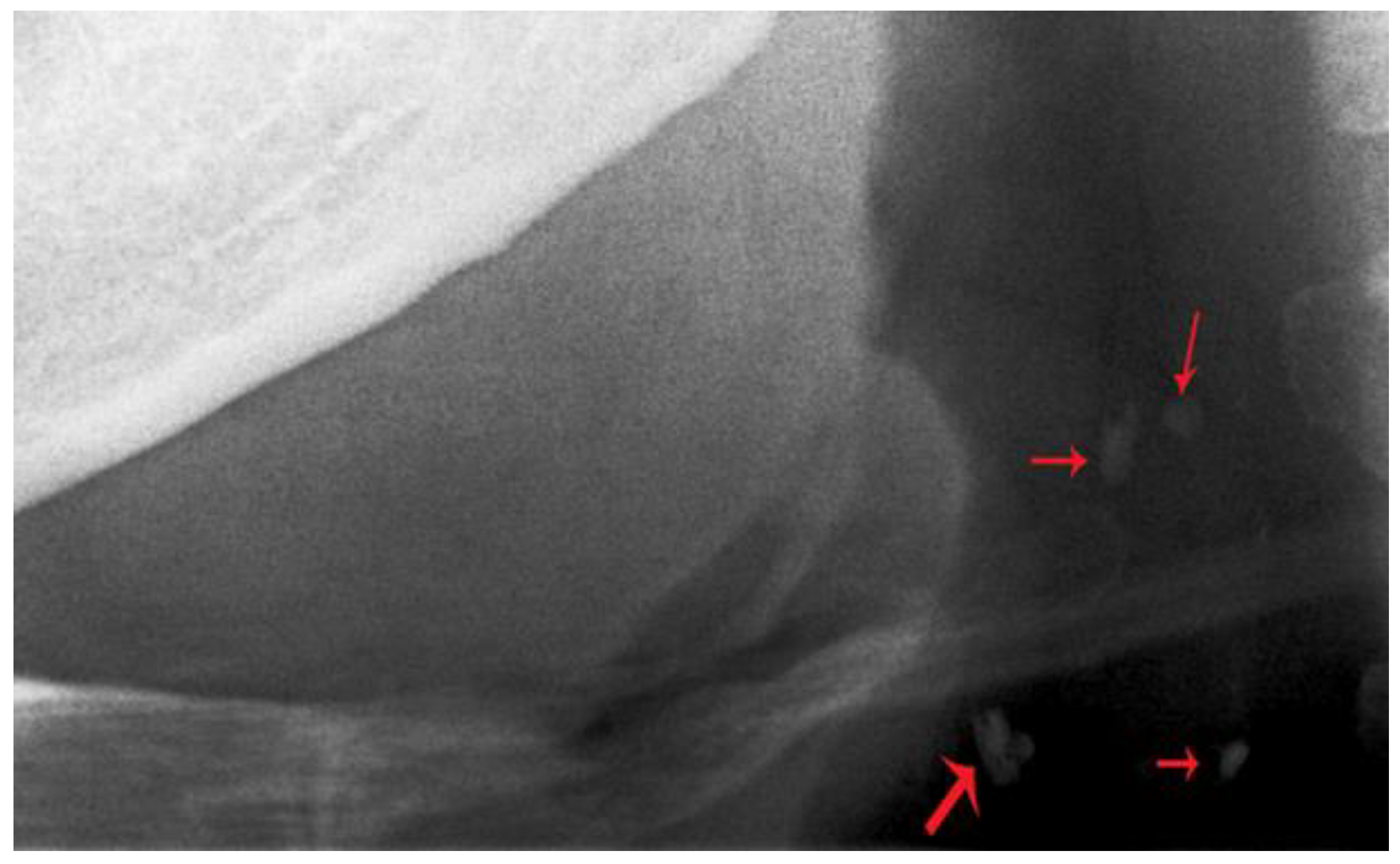
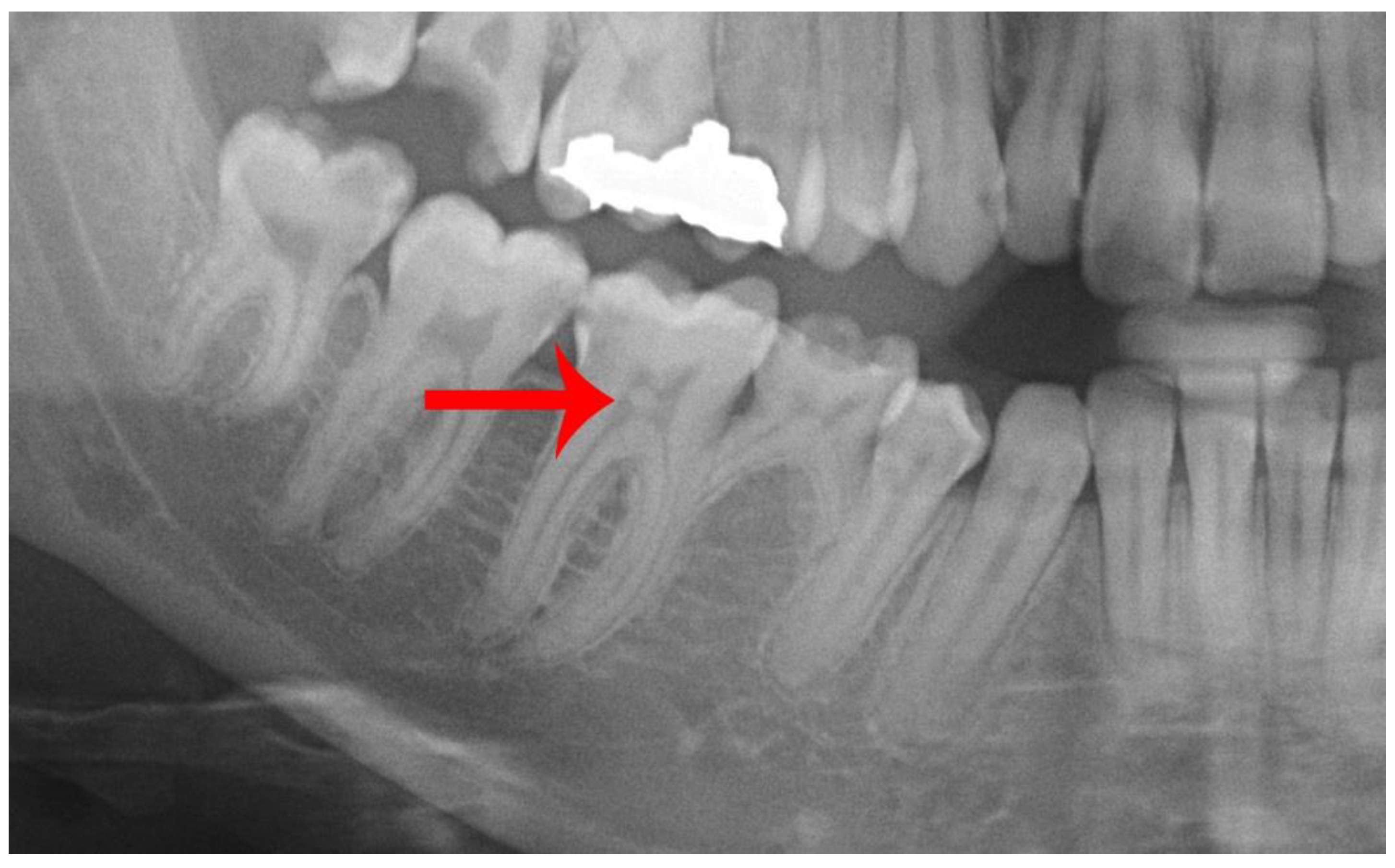
2.2. Radiograph Evaluation
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Virmani:, R.; Burke, A.; Ladich, E.; Kolodgie, F.D. Pathology of carotid artery atherosclerotic disease. In Carotid Disease: The Role of Imaging in Diagnosis and Management, 1st ed.; Gillard, J., Graves, M., Hatsukami, T., Yuan, C., Eds.; Cambridge University Press: Cambridge, MA, USA, 2007; pp. 1–18. [Google Scholar]
- Monteiro, I.A.; Ibrahim, C.; Albuquerque, R.; Donaldson, N.; Salazar, F.; Monteiro, L. Assessment of carotid calcifications on digital panoramic radiographs: Retrospective analysis and review of the literature. J. Stomatol. Oral Maxillofac. Surg. 2018, 119, 102–106. [Google Scholar] [CrossRef] [PubMed]
- Fanning, N.F.; Walters, T.D.; Fox, A.J.; Symons, S.P. Association between calcification of the cervical carotid artery bifurcation and white matter ischemia. AJNR Am. J. Neuroradiol. 2006, 27, 378–383. [Google Scholar] [PubMed]
- Garoff, M.; Johansson, E.; Ahlqvist, J.; Jäghagen, E.L.; Arnerlöv, C.; Wester, P. Detection of calcifications in panoramic radiographs in patients with carotid stenoses ≥50%. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2014, 117, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.N.; Friedlander, A.H.; Jolly, D.A.; Date, L. Carotid calcification on panoramic radiographs: An important marker for vascular risk. Oral Surg. Oral. Med. Oral Pathol. Oral Radiol. Endod. 2002, 94, 510–514. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, N.; Ahlqvist, J.B.; Näslund, U.; Wester, P.; Buhlin, K.; Gustafsson, A.; Levring Jäghagen, E. Calcified carotid artery atheromas in panoramic radiographs are associated with a first myocardial infarction: A case-control study. Oral Surg. Oral Med. Oral Pathol Oral Radiol. 2018, 125, e199–e204. [Google Scholar] [CrossRef] [PubMed]
- Shah, N.; Bansal, N.; Logani, A. Recent advances in imaging technologies in dentistry. World J. Radiol. 2014, 6, 794–807. [Google Scholar] [CrossRef] [PubMed]
- Gavala, S.; Donta, C.; Tsiklakis, K.; Boziari, A.; Kamenopoulou, V.; Stamatakis, H.C. Radiation dose reduction in direct digital panoramic radiography. Eur. J. Radiol. 2009, 71, 42–48. [Google Scholar] [CrossRef]
- Friedlander, A.H.; Lande, A. Panoramic radiographic identification of carotid arterial plaques. Oral Surg. Oral Med. Oral Pathol. 1981, 52, 102–104. [Google Scholar] [CrossRef]
- Alman, A.C.; Johnson, L.R.; Calverley, D.C.; Grunwald, G.K.; Lezotte, D.C.; Hokanson, J.E. Validation of a method for quantifying carotid artery calcification from panoramic radiographs. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 116, 518–524. [Google Scholar] [CrossRef]
- Christou, P.; Leemann, B.; Schimmel, M.; Kiliaridis, S.; Müller, F. Carotid artery calcification in ischemic stroke patients detected in standard dental panoramic radiographs—A preliminary study. Adv. Med. Sci. 2010, 55, 26–31. [Google Scholar] [CrossRef]
- Brito, A.C.; Nascimento, H.A.; Argento, R.; Beline, T.; Ambrosano, G.M.; Freitas, D.Q. Prevalence of suggestive images of carotid artery calcifications on panoramic radiographs and its relationship with predisposing factors. Cien. Saude Colet. 2016, 21, 2201–2208. [Google Scholar] [CrossRef] [PubMed]
- Ertas, E.T.; Sisman, Y. Detection of incidental carotid artery calcifications during dental examinations: Panoramic radiography as an important aid in dentistry. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011, 112, e11–e17. [Google Scholar] [CrossRef] [PubMed]
- Almog, D.M.; Tsimidis, K.; Moss, M.E.; Gottlieb, R.H.; Carter, L.C. Evaluation of a training program for detection of carotid artery calcifications on panoramic radiographs. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2000, 90, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Goga, R.; Chandler, N.P.; Oginni, A.O. Pulp stones: A review. Int. Endod. J. 2008, 41, 457–468. [Google Scholar] [CrossRef] [PubMed]
- Marwaha, M.; Chopra, R.; Chaudhuri, P.; Gupta, A.; Sachdev, J. Multiple pulp stones in primary and developing permanent dentition: A report of 4 cases. Case Rep. Dent. 2012, 2012, 408045. [Google Scholar] [CrossRef] [PubMed]
- Norman, N.P.; Johnstone, H.M. Neuralgias of the superior and inferior maxillary branches of the fifth nerve caused by dental pulp nodules. N. Y. Med. J. 1921, 114, 88. [Google Scholar]
- Bevelander, G.; Johnson, P.L. Histogenesis and histochemistry of pulpal calcification. J. Dent. Res. 1956, 35, 714–722. [Google Scholar]
- Khojastepour, L.; Bronoosh, P.; Khosropanah, S.; Rahimi, E. Can dental pulp calcification predict the risk of ischemic cardiovascular disease? J. Dent. (Tehran) 2013, 10, 456–460. [Google Scholar]
- Yeluri, G.; Kumar, C.A.; Raghav, N. Correlation of dental pulp stones, carotid artery and renal calcifications using digital panoramic radiography and ultrasonography. Contemp. Clin. Dent. 2015, 6, S147–S151. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Saudi Arabia Data and Statistics for Non-Communicable Diseases (NCDs). 2016. Available online: https://www.who.int/nmh/countries/sau_en.pdf (accessed on 31 January 2019).
- Alzoman, H.A.; Al-Sadhan, R.I.; Al-Lahem, Z.H.; Al-Sakaker, A.N.; Al-Fawaz, Y.F. Prevalence of carotid calcification detected on panoramic radiographs in a Saudi population from a training institute in Central Saudi Arabia. Saudi Med. J. 2012, 33, 177–181. [Google Scholar]
- Abreu, T.Q.; Ferreira, E.B.; de Brito Filho, S.B.; de Sales, K.P.; Lopes, F.F.; de Oliveira, A.E. Prevalence of carotid artery calcifications detected on panoramic radiographs and confirmed by Doppler ultrasonography: Their relationship with systemic conditions. Indian J. Dent. Res. 2015, 26, 345–350. [Google Scholar]
- Pornprasertsuk-Damrongsri, S.; Virayavanich, W.; Thanakun, S.; Amaekchok, P.; Khovidhunkit, W. The prevalence of carotid artery calcifications detected on panoramic radiographs in patients with metabolic syndrome. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 108, e57–e62. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Kim, O.S.; Chung, H.J.; Kim, Y.J.; Kweon, S.S.; Lee, Y.H.; Shin, M.H.; Yoon, S.J. The prevalence and correlation of carotid artery calcification on panoramic radiographs and peripheral arterial disease in a population from the Republic of Korea: The Dong-gu study. Dentomaxillofac. Radiol. 2013, 42, 29725099. [Google Scholar] [CrossRef]
- Bayer, S.; Helfgen, E.H.; Bös, C.; Kraus, D.; Enkling, N.; Mues, S. Prevalence of findings compatible with carotid artery calcifications on dental panoramic radiographs. Clin. Oral Investig. 2011, 15, 563–569. [Google Scholar] [CrossRef] [PubMed]
- Santos, J.M.; Soares, G.C.; Alves, A.P.; Kurita, L.M.; Silva, P.G.; Costa, F.W. Prevalence of carotid artery calcifications among 2,500 digital panoramic radiographs of an adult Brazilian population. Med. Oral Patol. Oral Cir. Bucal 2018, 23, e256–e261. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, J.R.; Yamada, J.L.; Berrocal, C.; Westphalen, F.H.; Franco, A.; Fernandes, Â. Prevalence of Pathologic Findings in Panoramic Radiographs: Calcified Carotid Artery Atheroma. Acta Stomatol. Croat. 2016, 50, 230–234. [Google Scholar] [CrossRef] [PubMed]
- Friedlander, A.H.; Garrett, N.R.; Norman, D.C. The prevalence of calcified carotid artery atheromas on the panoramic radiographs of patients with type 2 diabetes mellitus. J. Am. Dent. Assoc. 2002, 133, 1516–1523. [Google Scholar] [CrossRef]
- Central Intelligence Agency (CIA). The World Factbook; Central Intelligence Agency (CIA): Washington, DC, USA, 2018. Available online: https://www.cia.gov/library/publications/the-world-factbook/geos/sa.html (accessed on 31 January 2019).
- Nasseh, I.; Aoun, G. Carotid Artery Calcification: A Digital Panoramic-Based Study. Diseases 2018, 6, 15. [Google Scholar] [CrossRef]
- Friedlander, A.H.; El Saden, S.M.; Hazboun, R.C.; Chang, T.I.; Wong, W.K.; Garrett, N.R. Detection of carotid artery calcification on the panoramic images of post-menopausal females is significantly associated with severe abdominal aortic calcification: A risk indicator of future adverse vascular events. Dentomaxillofac. Radiol. 2015, 44, 20150094. [Google Scholar] [CrossRef]
- Sandeepa, N.C.; Ajmal, M.; Deepika, N. A retrospective panoramic radiographic study on prevalence of pulp stones in South Karnataka population. World J. Dent. 2016, 7, 14–17. [Google Scholar] [CrossRef]
- Gulsahi, A.; Cebeci, A.I.; Ozden, S. A radiographic assessment of the prevalence of pulp stones in a group of Turkish dental patients. Int. Endod. J. 2009, 42, 735–739. [Google Scholar] [CrossRef] [PubMed]
- Çolak, H.; Çelebi, A.; Hamidi, M.; Bayraktar, Y.; Çolak, T.; Uzgur, R. Assessment of the prevalence of pulp stones in a sample of Turkish Central Anatolian population. Sci. World J. 2012, 2012, 804278. [Google Scholar] [CrossRef] [PubMed]
- Zahrani, A.A. Dental health status among a sample of elderly dental patients in Riyadh, Saudi Arabia. Saudi Dent. J. 2005, 17, 74–82. [Google Scholar]
- Al-Shehri, S.M. Oral health status of older people in residential homes in Saudi Arabia. Open J. Stomatol. 2012, 2, 307–313. [Google Scholar] [CrossRef]
- Kansu, O.; Ozbek, M.; Avcu, N.; Aslan, U.; Kansu, H.; Gençtoy, G. Can dental pulp calcification serve as a diagnostic marker for carotid artery calcification in patients with renal diseases? Dentomaxillofac. Radiol. 2009, 38, 542–545. [Google Scholar] [CrossRef] [PubMed]
- Horsley, S.H.; Beckstrom, B.; Clark, S.J.; Scheetz, J.P.; Khan, Z.; Farman, A.G. Prevalence of carotid and pulp calcifications: A correlation using digital panoramic radiographs. Int. J. Comput. Assist. Radiol. Surg. 2009, 4, 169–173. [Google Scholar] [CrossRef] [PubMed]

| Variables | Category | Total Number | Percentage % | CACs | p Value | ||
|---|---|---|---|---|---|---|---|
| Absent | Present | Percentage % | |||||
| Gender | Male | 1212 | 60.2% | 1182 | 30 | 2.5% | 0.087 |
| Female | 801 | 39.8% | 790 | 11 | 1.4% | ||
| Age group | 18–25 | 712 | 35.4% | 712 | 0 | 0% | <0.001 * |
| 26–40 | 624 | 31.0% | 622 | 2 | 0.3% | ||
| 41–54 | 473 | 23.5% | 460 | 13 | 2.7% | ||
| ≥55 | 204 | 10.1 | 178 | 26 | 12.7% | ||
| Variables | Category | Total Number | Percentage % | Pulp Stones | p Value | ||
|---|---|---|---|---|---|---|---|
| Absent | Present | Percentage % | |||||
| Gender | Male | 1212 | 60.2% | 1151 | 61 | 5% | 0.278 |
| Female | 801 | 39.8% | 769 | 32 | 4% | ||
| Age group | 18–25 | 712 | 35.4% | 663 | 49 | 6.9% | 0.001 * |
| 26–40 | 624 | 31.0% | 596 | 28 | 4.5% | ||
| 41–54 | 473 | 23.5% | 462 | 11 | 2.3% | ||
| ≥55 | 204 | 10.1% | 199 | 5 | 2.5% | ||
| Variables | Category | Total Number | CACs/Pulp Stones | |||
|---|---|---|---|---|---|---|
| −/− | +/− | −/+ | +/+ | |||
| Gender | Male | 1212 | 1123 | 28 | 59 | 2 |
| Female | 801 | 758 | 11 | 32 | 0 | |
| Age group | 18–25 | 712 | 663 | 0 | 49 | 0 |
| 26–40 | 624 | 594 | 2 | 28 | 0 | |
| 41–54 | 473 | 449 | 13 | 11 | 0 | |
| ≥55 | 204 | 175 | 24 | 3 | 2 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsweed, A.; Farah, R.; PS, S.; Farah, R. The Prevalence and Correlation of Carotid Artery Calcifications and Dental Pulp Stones in a Saudi Arabian Population. Diseases 2019, 7, 50. https://doi.org/10.3390/diseases7030050
Alsweed A, Farah R, PS S, Farah R. The Prevalence and Correlation of Carotid Artery Calcifications and Dental Pulp Stones in a Saudi Arabian Population. Diseases. 2019; 7(3):50. https://doi.org/10.3390/diseases7030050
Chicago/Turabian StyleAlsweed, Ali, Randa Farah, Satheeshkumar PS, and Rafat Farah. 2019. "The Prevalence and Correlation of Carotid Artery Calcifications and Dental Pulp Stones in a Saudi Arabian Population" Diseases 7, no. 3: 50. https://doi.org/10.3390/diseases7030050
APA StyleAlsweed, A., Farah, R., PS, S., & Farah, R. (2019). The Prevalence and Correlation of Carotid Artery Calcifications and Dental Pulp Stones in a Saudi Arabian Population. Diseases, 7(3), 50. https://doi.org/10.3390/diseases7030050





