Diaphragmatic Palsy
Abstract
1. Introduction
2. Anatomy
3. Functions
4. Nerve Supply
5. Diaphragmatic Palsy (DP)
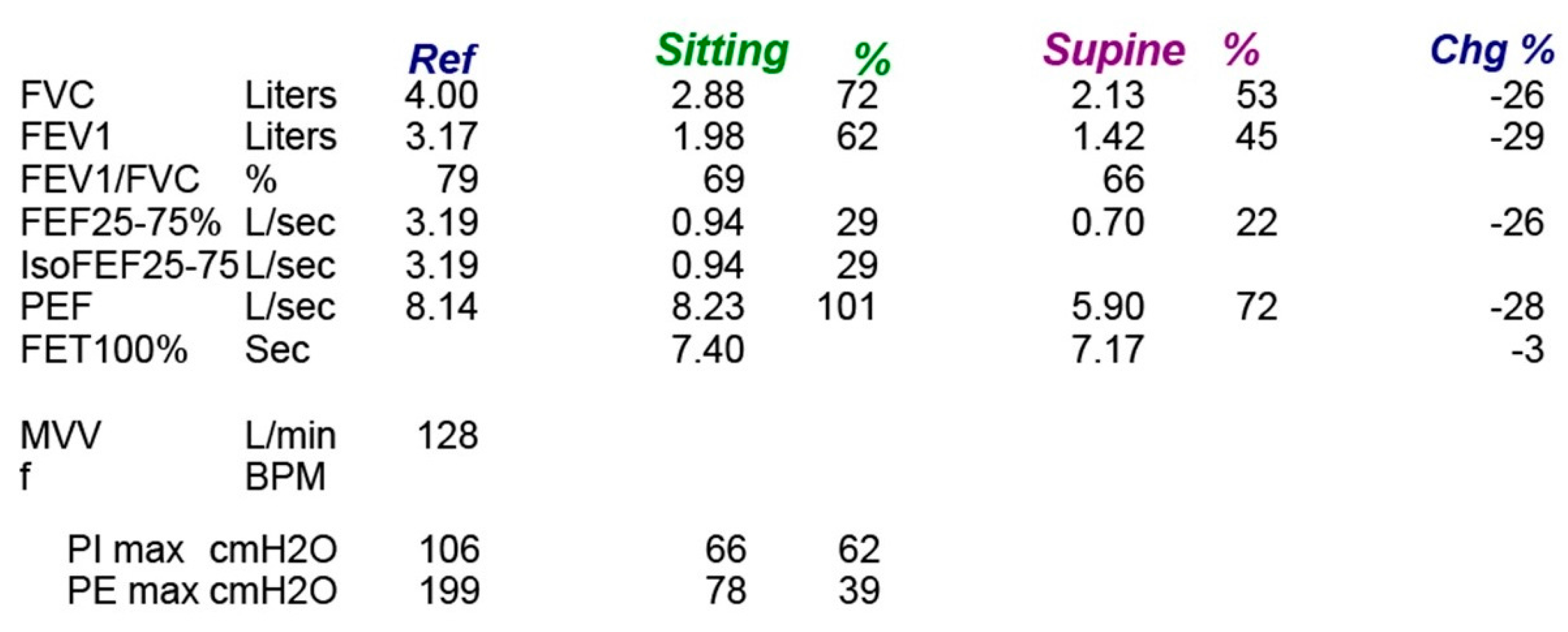
6. Clinical Features
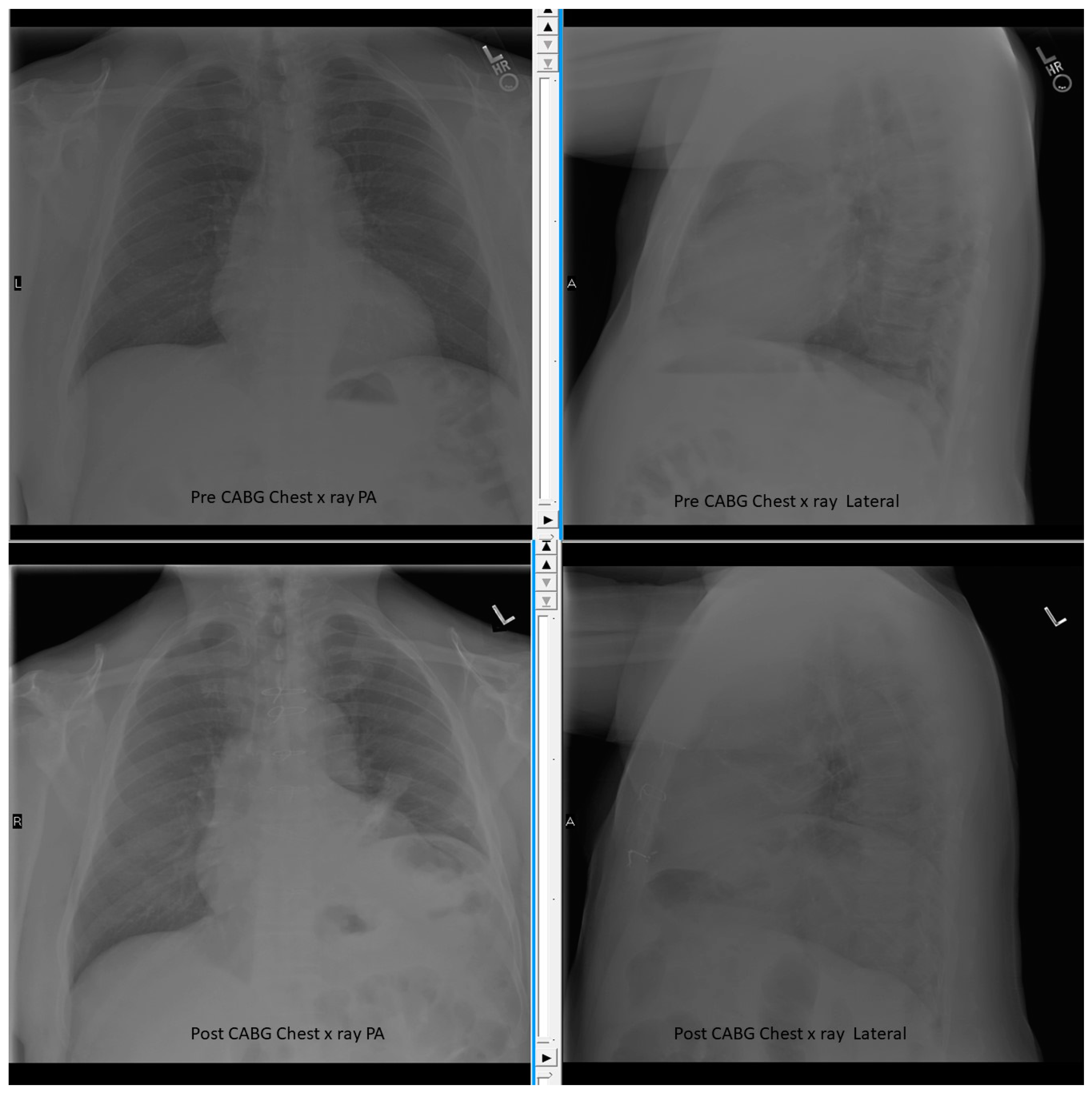
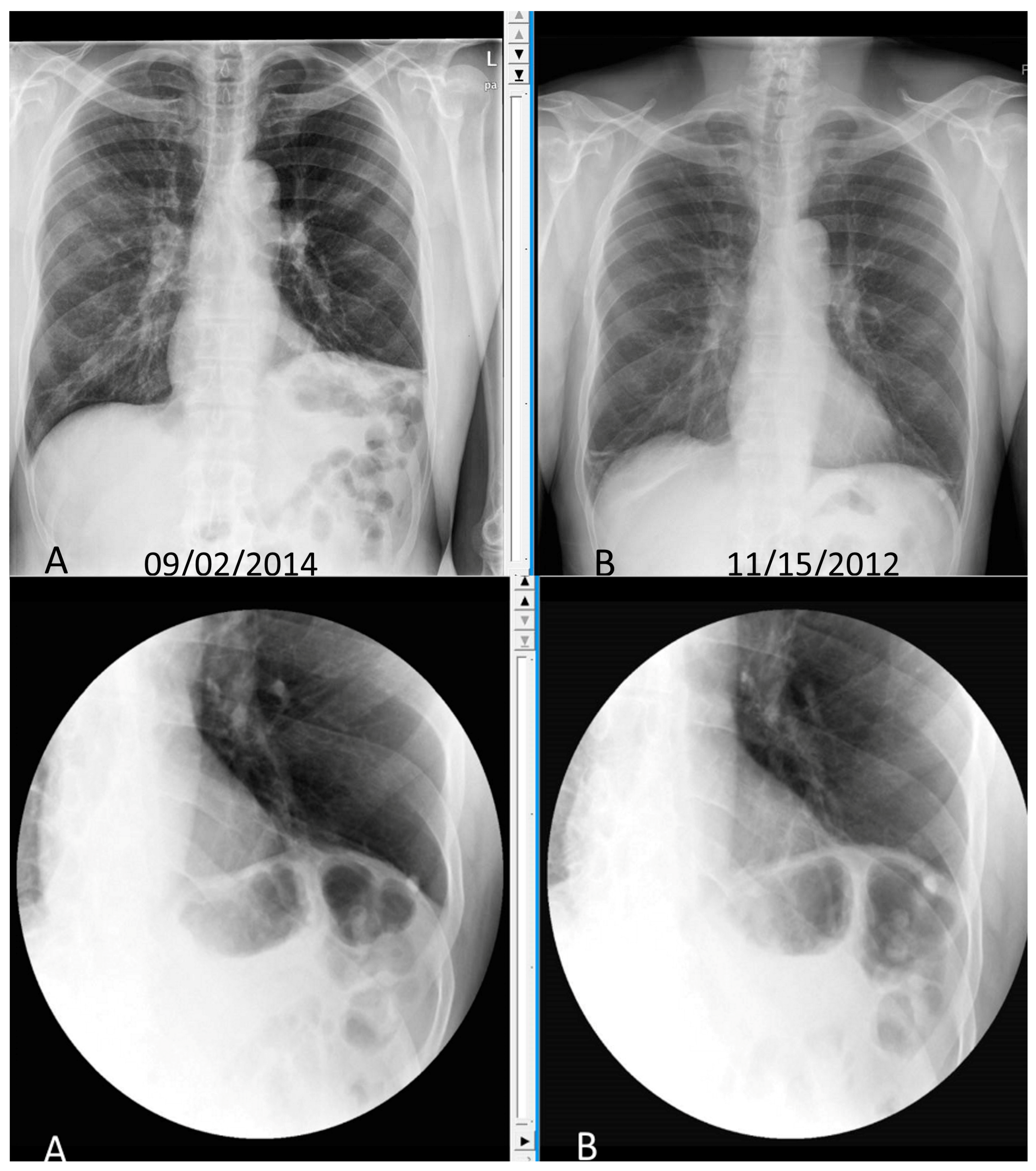
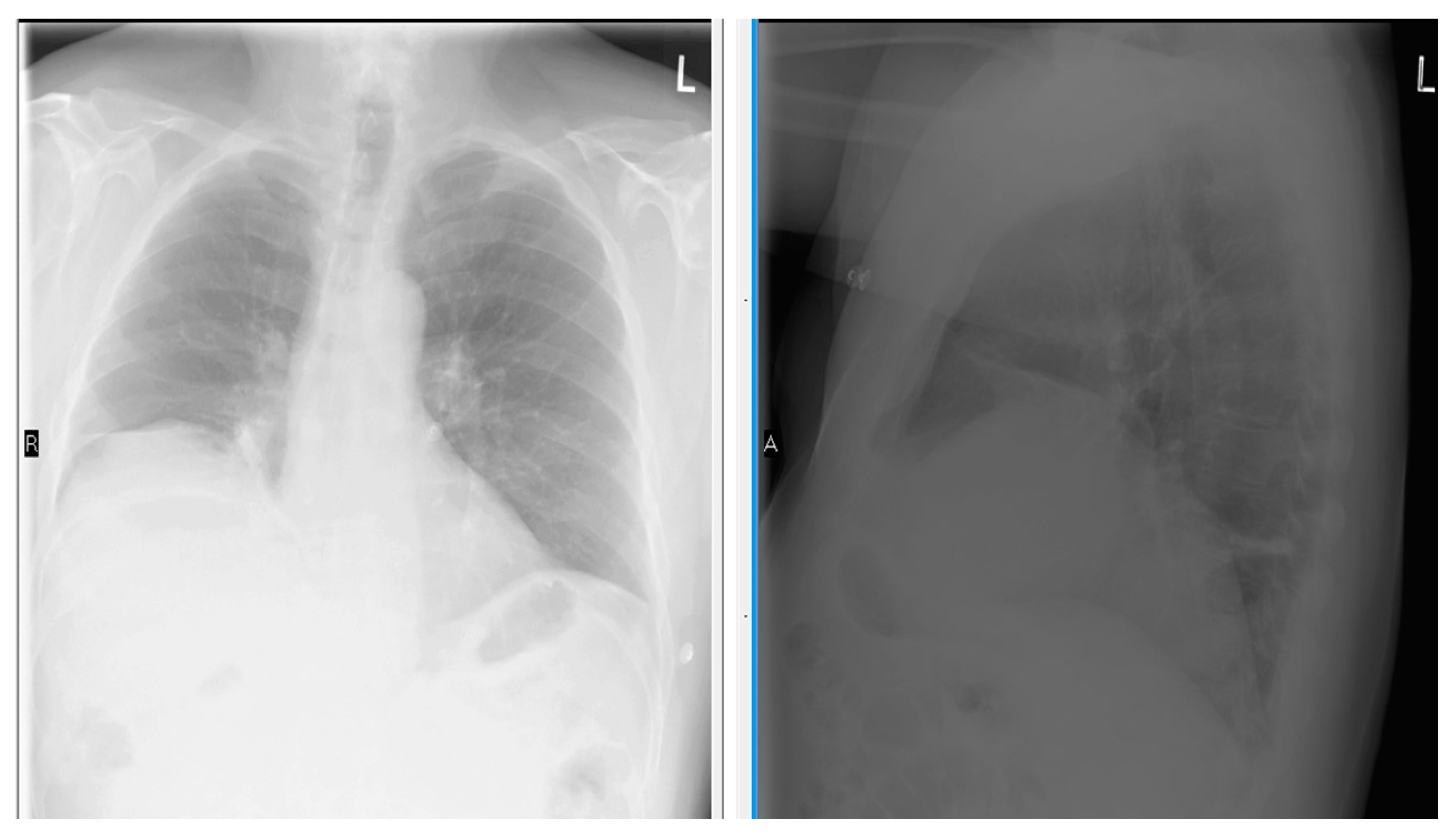
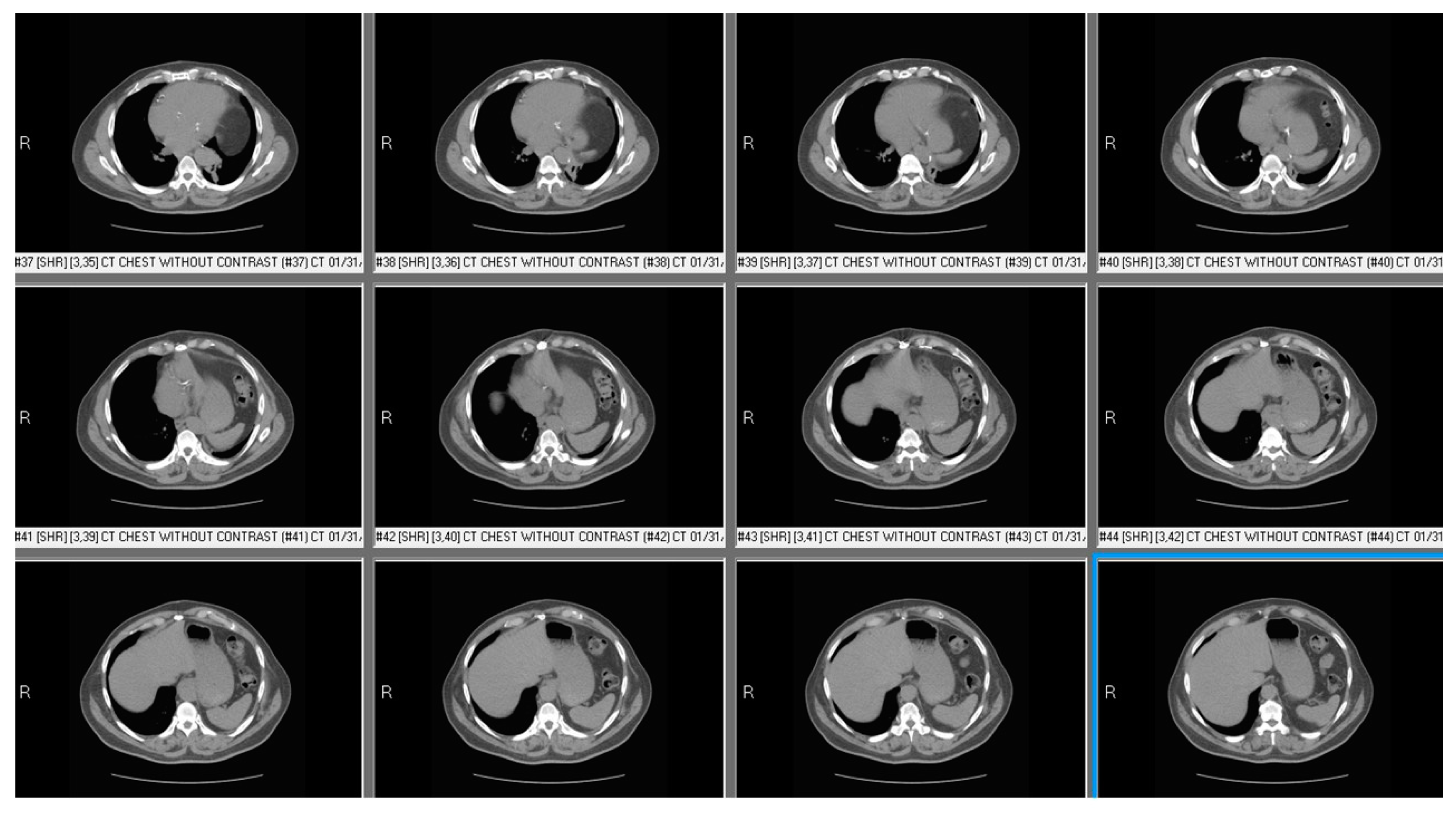
7. Investigation
8. Treatment
9. Prognosis
10. Conclusions
Supplementary Materials
Conflicts of Interest
References
- Bordoni, B.; Zanier, E. Anatomic connections of the diaphragm: Influence of respiration on the body system. J. Multidiscip. Healthc. 2013, 6, 281. [Google Scholar] [CrossRef] [PubMed]
- Schumpelick, V.; Steinau, G.; Schlüper, I.; Prescher, A. Surgical embryology and anatomy of the diaphragm with surgical applications. Surg. Clin. 2000, 80, 213–239. [Google Scholar] [CrossRef]
- Maish, M.S. The diaphragm. Surg. Clin. N. Am. 2010, 90, 955–968. [Google Scholar] [CrossRef] [PubMed]
- Dubé, B.P.; Dres, M. Diaphragm Dysfunction: Diagnostic Approaches and Management Strategies. J. Clin. Med. 2016, 5, 113. [Google Scholar] [CrossRef] [PubMed]
- Aguirre, V.J.; Sinha, P.; Zimmet, A.; Lee, G.A.; Kwa, L.; Rosenfeldt, F. Phrenic nerve injury during cardiac surgery: Mechanisms, management and prevention. Heart Lung Circ. 2013, 22, 895–902. [Google Scholar] [CrossRef] [PubMed]
- Dimopoulou, I.; Daganou, M.; Dafni, U.; Karakatsani, A.; Khoury, M.; Geroulanos, S.; Jordanoglou, J. Phrenic nerve dysfunction after cardiac operations: Electrophysiologic evaluation of risk factors. Chest 1998, 113, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, W.E.; Rubis, L.J.; Jones, C.W.; Harrah, J.D. Etiology and prevention of topical cardiac hypothermia-induced phrenic nerve injury and left lower lobe atelectasis during cardiac surgery. Chest 1985, 88, 680–683. [Google Scholar] [CrossRef] [PubMed]
- Curtis, J.J.; Nawarawong, W.; Walls, J.T.; Schmaltz, R.A.; Boley, T.; Madsen, R.; Anderson, S.K. Elevated hemidiaphragm after cardiac operations: Incidence, prognosis, and relationship to the use of topical ice slush. Ann. Thorac. Surg. 1989, 48, 764–768. [Google Scholar] [CrossRef]
- Efthimiou, J.; Butler, J.; Woodham, C.; Benson, M.K.; Westaby, S. Diaphragm paralysis following cardiac surgery: Role of phrenic nerve cold injury. Ann. Thorac. Surg. 1991, 52, 1005–1008. [Google Scholar] [CrossRef]
- McCaul, J.A.; Hilsop, W.S. Transient hemi-diaphragmatic paralysis following neck surgery: Report of a case and review of the literature. J. R. Coll. Surg. Edinb. 2001, 46, 186–188. [Google Scholar] [PubMed]
- Dugena, O.; Islam, S.; Hayter, J. The rate of phrenic nerve injury following neck dissection for head and neck cancer and its impact on length of hospital stay. Int. J. Oral Maxillofac. Surg. 2017, 46, 283. [Google Scholar] [CrossRef]
- Harris, K.; Maniatis, G.; Siddiqui, F.; Maniatis, T. Phrenic nerve injury and diaphragmatic paralysis following pacemaker pulse generator replacement. Heart Lung J. Acute Crit. Care 2013, 42, 65–66. [Google Scholar] [CrossRef] [PubMed]
- Rosato, L.; Nasi, P.G.; Porcellana, V.; Varvello, G.; Mondini, G.; Bertone, P. Unilateral phrenic nerve paralysis: A rare complication after total thyroidectomy for a large cervico-mediastinal goiter. Il G. Chir. 2007, 28, 149–152. [Google Scholar]
- Ami, M.; Yunus, M.R.; Hashim, N.D.; Baki, M.M. Laryngeal Trauma with Phrenic Nerve Injury: A Rare Association. Philipp. J. Otolaryngol. Head Neck Surg. 2010, 25, 39–41. [Google Scholar]
- Sheridan, J.P.; Cheriyan, A.; Doud, J.; Dornseif, S.E.; Montoya, A.; Houck, J.; Flisak, M.E.; Walsh, J.M.; Garrity, J.E. Incidence of phrenic neuropathy after isolated lung transplantation. The Loyola University Lung Transplant Group. J. Heart Lung Transplant. 1995, 14, 684–691. [Google Scholar] [PubMed]
- Ostrowska, M.; de Carvalho, M. Prognosis of phrenic nerve injury following thoracic interventions: Four new cases and a review. Clin. Neurol. Neurosurg. 2012, 114, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Mogayzel, P.J.; Colombani, P.M.; Crawford, T.O.; Yang, S.C. Bilateral diaphragm paralysis following lung transplantation and cardiac surgery in a 17-year-old. J. Heart Lung Transplant. 2002, 21, 710–712. [Google Scholar] [CrossRef]
- Goffart, Y.; Moreau, P.; Biquet, J.F.; Melon, J. Phrenic nerve paralysis complicating cervicofacial surgery. Acta Oto-Rhino-Laryngol. Belg. 1988, 42, 564–570. [Google Scholar]
- Qureshi, A. Diaphragm paralysis. Semin. Respir. Crit. Care Med. 2009, 30, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Piehler, J.M.; Pairolero, P.C.; Gracey, D.R.; Bernatz, P.E. Unexplained diaphragmatic paralysis: A harbinger of malignant disease? J. Thorac. Cardiovasc. Surg. 1982, 84, 861–864. [Google Scholar] [PubMed]
- Rudrappa, M.; Kokatnur, L. Dyspnea due to osteoarthritis. Diaphragmatic Palsy caused by cervical spondylosis. World J. Pharm. Med. Res. 2016, 2, 214–216. [Google Scholar]
- Gosselink, R.; Kovacs, L.; Ketelaer, P.; Carton, H.; Decramer, M. Respiratory muscle weakness and respiratory muscle training in severely disabled multiple sclerosis patients. Arch. Phys. Med. Rehabil. 2000, 81, 747–751. [Google Scholar] [CrossRef]
- McCool, F.D.; Tzelepis, G.E. Dysfunction of the diaphragm. N. Engl. J. Med. 2012, 366, 932–942. [Google Scholar] [CrossRef] [PubMed]
- Van Doorn, P.A.; Ruts, L.; Jacobs, B.C. Clinical features, pathogenesis, and treatment of Guillain-Barré syndrome. Lancet Neurol. 2008, 7, 939–950. [Google Scholar] [CrossRef]
- Rudrappa, M.; Kokatnur, L.; Chernyshev, O. Neurological Respiratory Failure. Diseases 2018, 6, 7. [Google Scholar] [CrossRef] [PubMed]
- Abbott, R.A.; Hammans, S.; Margarson, M.; Aji, B.M. Diaphragmatic paralysis and respiratory failure as a complication of Lyme disease. J. Neurol. Neurosurg. Psychiatry 2005, 76, 1306–1307. [Google Scholar] [CrossRef] [PubMed]
- Dewberry, R.G.; Phillips, L.H.; Schneider, B.F.; Cale, W.F. Sarcoid myopathy presenting with diaphragm weakness. Muscle Nerve 1993, 16, 832–835. [Google Scholar] [CrossRef] [PubMed]
- Borrell, H.; Narváez, J.; Alegre, J.J.; Castellví, I.; Mitjavila, F.; Aparicio, M.; Armengol, E.; Molina-Molina, M.; Nolla, J.M. Shrinking lung syndrome in systemic lupus erythematosus: A case series and review of the literature. Medicine 2016, 95, e4626. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, J.R.; Winther, K.H.; Bonnema, S.J.; Godballe, C.; Hegedüs, L. Respiratory Manifestations of Hypothyroidism: A Systematic Review. Thyroid 2016, 26, 1519–1527. [Google Scholar] [CrossRef] [PubMed]
- Murciano, D.; Rigaud, D.; Pingleton, S.; Armengaud, M.H.; Melchior, J.C.; Aubier, M. Diaphragmatic function in severely malnourished patients with anorexia nervosa. Effects of renutrition. Am. J. Respir. Crit. Care Med. 1994, 150, 1569–1574. [Google Scholar] [CrossRef] [PubMed]
- Dres, M.; Dubé, B.P.; Mayaux, J.; Delemazure, J.; Reuter, D.; Brochard, L.; Similowski, T.; Demoule, A. Coexistence and impact of limb muscle and diaphragm weakness at time of liberation from mechanical ventilation in medical intensive care unit patients. Am. J. Respir. Crit. Care Med. 2017, 195, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Medrinal, C.; Prieur, G.; Frenoy, É.; Quesada, A.R.; Poncet, A.; Bonnevie, T.; Gravier, F.E.; Lamia, B.; Contal, O. Respiratory weakness after mechanical ventilation is associated with one-year mortality-a prospective study. Crit. Care 2016, 20, 231. [Google Scholar] [CrossRef] [PubMed]
- DiNino, E.; Gartman, E.J.; Sethi, J.M.; McCool, F.D. Diaphragm ultrasound as a predictor of successful extubation from mechanical ventilation. Thorax 2013. [Google Scholar] [CrossRef] [PubMed]
- Jung, B.; Moury, P.H.; Mahul, M.; de Jong, A.; Galia, F.; Prades, A.; Albaladejo, P.; Chanques, G.; Molinari, N.; Jaber, S. Diaphragmatic dysfunction in patients with ICU-acquired weakness and its impact on extubation failure. Intensive Care Med. 2016, 42, 853–861. [Google Scholar] [CrossRef] [PubMed]
- Demoule, A.; Jung, B.; Prodanovic, H.; Molinari, N.; Chanques, G.; Coirault, C.; Matecki, S.; Duguet, A.; Similowski, T.; Jaber, S. Diaphragm dysfunction on admission to the intensive care unit. Prevalence, risk factors, and prognostic impact—A prospective study. Am. J. Respir. Crit. Care Med. 2013, 188, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Hooijman, P.E.; Beishuizen, A.; Witt, C.C.; de Waard, M.C.; Girbes, A.R.; Spoelstra-de Man, A.M.; Niessen, H.W.; Manders, E.; van Hees, H.W.; van den Brom, C.E.; et al. Diaphragm muscle fiber weakness and ubiquitin–proteasome activation in critically Ill patients. Am. J. Respir. Crit. Care Med. 2015, 191, 1126–1138. [Google Scholar] [CrossRef] [PubMed]
- Shanely, R.A.; Zergeroglu, M.A.; Lennon, S.L.; Sugiura, T.; Yimlamai, T.; Enns, D.; Belcastro, A.; Powers, S.K. Mechanical ventilation–induced diaphragmatic atrophy is associated with oxidative injury and increased proteolytic activity. Am. J. Respir. Crit. Care Med. 2002, 166, 1369–1374. [Google Scholar] [CrossRef] [PubMed]
- Levine, S.; Biswas, C.; Dierov, J.; Barsotti, R.; Shrager, J.B.; Nguyen, T.; Sonnad, S.; Kucharchzuk, J.C.; Kaiser, L.R.; Singhal, S.; et al. Increased proteolysis, myosin depletion, and atrophic AKT-FOXO signaling in human diaphragm disuse. Am. J. Respir. Crit. Care Med. 2011, 183, 483–490. [Google Scholar] [CrossRef] [PubMed]
- McClung, J.M.; Kavazis, A.N.; DeRuisseau, K.C.; Falk, D.J.; Deering, M.A.; Lee, Y.; Sugiura, T. Caspase-3 Regulation of Diaphragm Myonuclear Domain during Mechanical Ventilation–induced Atrophy. Am. J. Respir. Crit. Care Med. 2007, 175, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Grosu, H.B.; Im Lee, Y.; Lee, J.; Eden, E.; Eikermann, M.; Rose, K.M. Diaphragm muscle thinning in patients who are mechanically ventilated. Chest J. 2012, 142, 1455–1460. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Folger, W.N.; Bolton, C.F. Dyspnea as the predominant manifestation of bilateral phrenic neuropathy. Mayo Clin. Proc. 2004, 79, 1563–1565. [Google Scholar] [CrossRef] [PubMed]
- Guilleminault, C.; Shergill, R.P. Sleep-disordered breathing in neuromuscular disease. Curr. Treat. Options Neurol. 2002, 4, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Aboussouan, L.S. Sleep-disordered breathing in neuromuscular disease. Am. J. Respir. Crit. Care Med. 2015, 191, 979–989. [Google Scholar] [CrossRef] [PubMed]
- Benditt, J.O.; Boitano, L.J. Pulmonary issues in patients with chronic neuromuscular disease. Am. J. Respir. Crit. Care Med. 2013, 187, 1046–1055. [Google Scholar] [CrossRef] [PubMed]
- McCool, F.D.; Mead, J. Dyspnea on immersion: Mechanisms in patients with bilateral diaphragm paralysis. Am. Rev. Respir. Dis. 1989, 139, 275–276. [Google Scholar] [CrossRef] [PubMed]
- Chetta, A.; Rehman, A.K.; Moxham, J.; Carr, D.H.; Polkey, M.I. Chest radiography cannot predict diaphragm function. Respir. Med. 2005, 99, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Nason, L.K.; Walker, C.M.; McNeeley, M.F.; Burivong, W.; Fligner, C.L.; Godwin, J.D. Imaging of the diaphragm: Anatomy and function. Radiographics 2012, 32, E51–E70. [Google Scholar] [CrossRef] [PubMed]
- Blumhof, S.; Wheeler, D.; Thomas, K.; McCool, F.D.; Mora, J. Change in diaphragmatic thickness during the respiratory cycle predicts extubation success at various levels of pressure support ventilation. Lung 2016, 194, 519–525. [Google Scholar] [CrossRef] [PubMed]
- Boussuges, A.; Gole, Y.; Blanc, P. Diaphragmatic motion studied by m-mode ultrasonography: Methods, reproducibility, and normal values. Chest J. 2009, 135, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Lerolle, N.; Guérot, E.; Dimassi, S.; Zegdi, R.; Faisy, C.; Fagon, J.Y.; Diehl, J.L. Ultrasonographic diagnostic criterion for severe diaphragmatic dysfunction after cardiac surgery. Chest J. 2009, 135, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Antenora, F.; Fantini, R.; Iattoni, A.; Castaniere, I.; Sdanganelli, A.; Livrieri, F.; Tonelli, R.; Zona, S.; Monelli, M.; Clini, E.M.; et al. Prevalence and outcomes of diaphragmatic dysfunction assessed by ultrasound technology during acute exacerbation of COPD: A pilot study. Respirology 2017, 22, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Boon, A.J.; Sekiguchi, H.; Harper, C.J.; Strommen, J.A.; Ghahfarokhi, L.S.; Watson, J.C.; Sorenson, E.J. Sensitivity and specificity of diagnostic ultrasound in the diagnosis of phrenic neuropathy. Neurology 2014, 83, 1264–1270. [Google Scholar] [CrossRef] [PubMed]
- Laroche, C.M.; Carroll, N.; Moxham, J.; Green, M. Clinical significance of severe isolated diaphragm weakness. Am. Rev. Respir. Dis. 1988, 138, 862–866. [Google Scholar] [CrossRef] [PubMed]
- Lisboa, C.; Paxré, P.D.; Pertuzé, J.; Contreras, G.; Moreno, R.; Guillemi, S.; Cruz, E. Inspiratory Muscle Function In Unilateral Diaphragmatic Paralysis 1–3. Am. Rev. Respir. Dis. 1986, 134, 488–492. [Google Scholar] [PubMed]
- Mier-Jedrzejowicz, A.; Brophy, C.; Moxham, J.; Green, M. Assessment of diaphragm weakness. Am. Rev. Respir. Dis. 1988, 137, 877–883. [Google Scholar] [CrossRef] [PubMed]
- Steier, J.; Kaul, S.; Seymour, J.; Jolley, C.; Rafferty, G.; Man, W. The value of multiple tests of respiratory muscle strength. Thorax 2007, 62, 975–980. [Google Scholar] [CrossRef] [PubMed]
- Multz, A.S.; Aldrich, T.K.; Prezant, D.J.; Karpel, J.P.; Hendler, J.M. Maximal inspiratory pressure is not a reliable test of inspiratory muscle strength in mechanically ventilated patients. Am. Rev. Respir. Dis. 1990, 142, 529–532. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.H.; Cooke, N.T.; Edwards, R.H.; Spiro, S.G. Predicted normal values for maximal respiratory pressures in Caucasian adults and children. Thorax 1984, 39, 535–538. [Google Scholar] [CrossRef] [PubMed]
- Podnar, S. An algorithm for the safety of costal diaphragm electromyography derived from ultrasound. Muscle Nerve 2013, 47, 618–619. [Google Scholar] [CrossRef] [PubMed]
- Gechev, A.; Kane, N.M.; Koltzenburg, M.; Rao, D.G.; van der Star, R. Potential risks of iatrogenic complications of nerve conduction studies (NCS) and electromyography (EMG). Clin. Neurophysiol. Pract. 2016, 1, 62–66. [Google Scholar] [CrossRef]
- Hill, K.; Jenkins, S.C.; Philippe, D.L.; Cecins, N.; Shepherd, K.L.; Green, D.J.; Hillman, D.R.; Eastwood, P.R. High-intensity inspiratory muscle training in COPD. Eur. Respir. J. 2006, 27, 1119–1128. [Google Scholar] [CrossRef] [PubMed]
- Kodric, M.; Trevisan, R.; Torregiani, C.; Cifaldi, R.; Longo, C.; Cantarutti, F.; Confalonieri, M. Inspiratory muscle training for diaphragm dysfunction after cardiac surgery. J. Thorac. Cardiovasc. Surg. 2013, 145, 819–823. [Google Scholar] [CrossRef] [PubMed]
- Moodie, L.; Reeve, J.; Elkins, M. Inspiratory muscle training increases inspiratory muscle strength in patients weaning from mechanical ventilation: A systematic review. J. Physiother. 2011, 57, 213–221. [Google Scholar] [CrossRef]
- Gosselink, R.; De Vos, J.; Van Den Heuvel, S.P.; Segers, J.; Decramer, M.; Kwakkel, G. Impact of inspiratory muscle training in patients with COPD: What is the evidence? Eur. Respir. J. 2011, 37, 416–425. [Google Scholar] [CrossRef] [PubMed]
- Oo, T.; Watt, J.W.; Soni, B.M.; Sett, P.K. Delayed diaphragm recovery in 12 patients after high cervical spinal cord injury. A retrospective review of the diaphragm status of 107 patients ventilated after acute spinal cord injury. Spinal Cord 1999, 37, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Berlowitz, D.; Tamplin, J. Respiratory muscle training for cervical spinal cord injury (Protocol). Cochrane Database Syst. Rev. 2010, CD008507. [Google Scholar] [CrossRef]
- Van Houtte, S.; Vanlandewijck, Y.; Gosselink, R. Respiratory muscle training in persons with spinal cord injury: A systematic review. Respir. Med. 2006, 100, 1886–1895. [Google Scholar] [CrossRef] [PubMed]
- Groth, S.S.; Andrade, R.S. Diaphragm plication for eventration or paralysis: A review of the literature. Ann. Thorac. Surg. 2010, 89, S2146–S2150. [Google Scholar] [CrossRef] [PubMed]
- Groth, S.S.; Rueth, N.M.; Kast, T.; D’cunha, J.; Kelly, R.F.; Maddaus, M.A.; Andrade, R.S. Laparoscopic diaphragmatic plication for diaphragmatic paralysis and eventration: An objective evaluation of short-term and midterm results. J. Thorac. Cardiovasc. Surg. 2010, 139, 1452–1456. [Google Scholar] [CrossRef] [PubMed]
- Bourke, S.C.; Tomlinson, M.; Williams, T.L.; Bullock, R.E.; Shaw, P.J.; Gibson, G.J. Effects of non-invasive ventilation on survival and quality of life in patients with amyotrophic lateral sclerosis: A randomised controlled trial. Lancet Neurol. 2006, 5, 140–147. [Google Scholar] [CrossRef]
- Ambrosino, N.; Carpene, N.; Gherardi, M. Chronic respiratory care for neuromuscular diseases in adults. Eur. Respir. J. 2009, 34, 444–451. [Google Scholar] [CrossRef] [PubMed]
- Annane, D.; Orlikowski, D.; Chevret, S.; Chevrolet, J.C.; Raphaël, J.C. Nocturnal mechanical ventilation for chronic hypoventilation in patients with neuromuscular and chest wall disorders. Cochrane Database Syst. Rev. 2007. [Google Scholar] [CrossRef]
- Pinto, A.C.; Evangelista, T.; Carvalho, M.D.; Alves, M.A.; Luis, M.S. Respiratory assistance with a non-invasive ventilator (Bipap) in MND/ALS patients: Survival rates in a controlled trial. J. Neurol. Sci. 1995, 129, 19–26. [Google Scholar] [CrossRef]
- Ward, S.; Chatwin, M.; Heather, S.; Simonds, A.K. Randomised controlled trial of non-invasive ventilation (NIV) for nocturnal hypoventilation in neuromuscular and chest wall disease patients with daytime normocapnia. Thorax 2005, 60, 1019–1024. [Google Scholar] [CrossRef] [PubMed]
- DiMarco, A.F.; Kowalski, K.E. High-frequency spinal cord stimulation of inspiratory muscles in dogs: A new method of inspiratory muscle pacing. J. Appl. Physiol. 2009, 107, 662–669. [Google Scholar] [CrossRef] [PubMed]
- Onders, R.P.; Elmo, M.; Khansarinia, S.; Bowman, B.; Yee, J.; Bass, B.; Dunkin, B.; Ingvarsson, P.E.; Oddsdóttir, M. Complete worldwide operative experience in laparoscopic diaphragm pacing: Results and differences in spinal cord injured patients and amyotrophic lateral sclerosis patients. Surg. Endosc. 2009, 23, 1433–1440. [Google Scholar] [CrossRef] [PubMed]
- Onders, R.P.; Elmo, M.; Kaplan, C.; Katirji, B.; Schilz, R. Final analysis of the pilot trial of diaphragm pacing in amyotrophic lateral sclerosis with long-term follow-up: Diaphragm pacing positively affects diaphragm respiration. Am. J. Surg. 2014, 207, 393–397. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Bermejo, J.; Morélot-Panzini, C.; Salachas, F.; Redolfi, S.; Straus, C.; Becquemin, M.H.; Arnulf, I.; Pradat, P.F.; Bruneteau, G.; Ignagni, A.R.; et al. Diaphragm pacing improves sleep in patients with amyotrophic lateral sclerosis. Amyotroph. Lateral Scler. 2012, 13, 44–54. [Google Scholar] [CrossRef] [PubMed]
- McDermott, C.J.; Bradburn, M.J.; Maguire, C.; Cooper, C.L.; Baird, W.O.; Baxter, S.K.; Bourke, S.C.; Imam, I.; Bentley, A.; Ealing, J.; et al. Safety and efficacy of diaphragm pacing in patients with respiratory insufficiency due to amyotrophic lateral sclerosis (DiPALS): A multicentre, open-label, randomised controlled trial. Lancet Neurol. 2015, 14, 883–892. [Google Scholar]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kokatnur, L.; Rudrappa, M. Diaphragmatic Palsy. Diseases 2018, 6, 16. https://doi.org/10.3390/diseases6010016
Kokatnur L, Rudrappa M. Diaphragmatic Palsy. Diseases. 2018; 6(1):16. https://doi.org/10.3390/diseases6010016
Chicago/Turabian StyleKokatnur, Laxmi, and Mohan Rudrappa. 2018. "Diaphragmatic Palsy" Diseases 6, no. 1: 16. https://doi.org/10.3390/diseases6010016
APA StyleKokatnur, L., & Rudrappa, M. (2018). Diaphragmatic Palsy. Diseases, 6(1), 16. https://doi.org/10.3390/diseases6010016




