Abstract
Background: The influence of metabolic syndrome (MetS) on kidneys is related to many complications. We aimed to assess the association between MetS and chronic renal disease defined by a poor estimated glomerular filtration rate (eGFR) and/or the presence of microalbuminuria/macroalbuminuria. Methods: 149 patients (77 males/72 females) were enrolled in the study. Chronic renal disease was defined according to KDIGO 2012 criteria based on eGFR category and classified albuminuria. MetS was studied as a dichotomous variable (0 to 5 components) including hypertension, waist circumference, low HDL-cholesterol, high triglycerides, and high glucose. Results: The association between clustering MetS and both classified eGFR and classified albuminuria (x2 = 50.3, p = 0.001 and x2 = 26.9, p = 0.003 respectively) was found to be significant. The MetS presence showed an odds 5.3-fold (1.6–17.8) higher for low eGFR and 3.2-fold (1.2–8.8) higher for albuminuria in combination with the presence of diabetes mellitus, which also increased the risk for albuminuria by 3.5-fold (1.1–11.3). Albuminuria was significantly associated with high triglycerides, hypertension, high glucose (x2 = 11.8, p = 0.003, x2 = 11.4, p = 0.003 and x2 = 9.1, p = 0.01 respectively), and it was mildly associated with a low HDL-C (x2 = 5.7, p = 0.06). A significant association between classified eGFR and both high triglycerides and hypertension (x2 = 9.7, p = 0.04 and x2 = 16.1, p = 0.003 respectively) was found. Conclusion: The clustering of MetS was significantly associated with chronic renal disease defined by both classified eGFR and albuminuria. The definition of impaired renal function by classified albuminuria was associated with more MetS components rather than the evaluation of eGFR category. MetS may contribute to the manifestation of albuminuria in patients with diabetes mellitus.
1. Introduction
The metabolic syndrome (MetS) is characterized by a combination of metabolic disorders which increase the risk for heart disease, stroke, and all-cause mortality in the general population [1]. These metabolic disorders include central obesity, dyslipidemia (high triglycerides and low HDL-cholesterol), elevated blood pressure and dysregulated glucose homeostasis. Commonly, MetS is defined by the presence of at least three of the above components, but the presence of an increased number of its components confers a much better MetS definition [2,3]. However, some authors have suggested that the relevant risk of cardiovascular disease related to the presence of MetS is no greater than the contribution of the individual components [4]. Previous studies using different populations have reported an elevated age-adjusted prevalence of MetS in relation to increasingly sedentary lifestyle and high rates of obesity [5,6,7].
Chronic kidney disease (CKD) defined by a poor estimated glomerular filtration rate (eGFR) below 60 mL/min/1.73 m2 and/or the presence of albuminuria shows also a worldwide increased age-adjusted prevalence rate [8,9]. The influence of MetS on kidneys is related to many complications, but the predominant manifestation is chronic renal failure and the end-stage renal disease as a consequence. Previous observational studies have reported an independent association between MetS and CKD concluding mostly a positive association and less a non-significant correlation [10,11]. It has been supported that patients with MetS have a 1.4, 2.4, or 2.6-fold greater odds of incident CKD (development of an eGFR < 60 mL/min/1.73 m2) [12,13,14] than individuals without any MetS components. However, a few studies have been reported to the relationship between MetS and urinary protein excretion [10,15]. On the other hand, individuals with CKD have higher prevalence rates of MetS components than individuals without CKD including traditional and non-traditional predictors, insulin resistance, and elevation of inflammatory markers including cytokines and high-sensitivity C-reactive protein (hsCRP) [3,16].
In this study, we aimed to assess the association between MetS and chronic renal disease defined by an eGFR < 60 mL/min/1.73 m2 for a duration of more than 3 months and/or the presence of microalbuminuria/macroalbuminuria in relation to covariates including the age, gender, current smoking, alcohol intake, physical activity, and the presence of diabetes mellitus.
2. Materials and Methods
2.1. Subjects
This is a single-center observational cross-sectional study which was designed to evaluate the relationship between prevalent components of MetS and chronic renal disease among patients from the Department of Nephrology outpatient clinic of our hospital. This study was conducted in the Private “DOCTORS’ Hospital” and it was approved by the Hospital Institutional Review Board. All study participants provided informed oral consent prior to study enrollment.
One hundred forty nine patients, seventy-seven males, and seventy-two females were enrolled in the study on mean aged 69.4 ± 14.6 years old.
We excluded uncooperative patients and those younger than 18 years old. Subjects with psychiatric symptomatology or established dementia diagnosed by neuropsychologists were also excluded from the study.
The underlying diseases for the follow up in the nephrology outpatient clinic included hypertension (50.3%), type 2 diabetes mellitus (24.2%), chronic glomerulonephritis (5.4%), interstitial nephritis (5.4%), polycystic renal disease (2.7%), and other/unknown (12.1%). Detailed individual medical histories, family histories of kidney diseases, and the current pharmaceutical therapy were obtained from the patients.
Interviews were used to collect demographic data, including age, gender, marital status, education level and lifestyle characteristics regarding with alcohol drinking, active and passive smoking habits and physical activity. Subjects who declared no smoking or alcohol consumption during the past month were considered non-smokers or non-drinkers. Physical activity was measured based on the World Health Organization (WHO) recommendations for healthy adults and physically inactive participants (exercise < 300 min per week) were considered sedentary [17].
The current pharmaceutical treatment mainly included anti-hypertensive medications, such as calcium channel blockers, beta-blockers, inhibitors of angiotensin II AT1 receptors or new central-acting, hypolipidemic and anti-diabetic therapy. The participants consumed a free regular diet using low or regular salt intake.
Anthropometric measurements including height, body weight and waist circumference were recorded. Body mass index (BMI) was calculated and categorized based on the WHO classification into underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2) and obese (≥30 kg/m2) [18]. Waist circumference measurements were made approximately at the midpoint between the lower margin of the last palpable rib and the top of iliac crest at the end of a normal expiration according to the WHO guidelines [19].
2.2. Biochemical Measurements
Fasting plasma glucose, creatinine, triglycerides, high-density lipoprotein-cholesterol (HDL-C) were recorded from the patient files using the latest results. These biochemical markers were measured using a spectrophotometric technique by Chemistry Analyzer (MINDRAY BS-200, Diamond Diagnostics, Massachusetts, MA, USA) and were represented as mg/dL.
Spot urine samples from the first micturition after rising were obtained for the measurement of albumin and creatinine concentrations by the Chemistry Analyzer. The urinary albumin analysis by a spot urine sample is more accurate than dipsticks, but this still generates a concentration than a quantity.
2.3. Blood Pressure Measurements—Definitions
Blood pressure data were considered over a month, as the exposure period.
We recommended the home blood pressure record as a peripheral systolic and diastolic blood pressure (SBP and DBP) measurement using an automatic sphygmomanometer OMRON M4-I (Co Ltd., Kyoto, Japan). The blood pressure was doubly measured for two times per day, in the morning after rising and in the evening in a fasting, calming and resting state and two means were recorded per day. Their average was used for statistical analysis. Mean peripheral blood pressure (MBP) was calculated as: MBP = DBP + 1/3(SBP − DBP).
We also used a 24-h ambulatory blood pressure monitor with the Mobil-O-Graph device for verification of measurements and whether the means blood pressure values significantly differed from home recorded values, the means by 24-h monitoring were used for statistical analysis rather than the means by home measurements.
Chronic renal disease was defined according to the Kidney Disease Improving Global Outcomes (KDIGO) 2012 criteria as eGFR < 60 mL/min/1.73 m2 for time duration more than 3 months and the participants were classified in five stages according to eGFR category [20]. The eGFR was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation and the Modification of Diet in Renal Disease (MDRD) equation. The classification of our subjects based on eGFR category included: G1 eGFR ≥ 90 mL/min/1.73 m2 (n = 8, 5.4%); G2 eGFR = 60–90 mL/min/1.73 m2 (n = 34, 22.8%); G3 eGFR = 30–60 mL/min/1.73 m2 (n = 76, 51%); G4 eGFR = 15–30 mL/min/1.73 m2 (n = 29, 19.5%); G5 eGFR < 15 mL/min/1.73 m2 (n = 2, 1.3%).
The enrolled subjects were also classified based on albuminuria, which was defined as urinary albumin-to-creatinine ratio (ACR) ≥ 30 mg/gr according to KDIGO 2012 [20]. ACR calculation by using a spot urine sample, such as in this study, is considered an acceptable calculation, as ACR is correlated well with 24-h urinary albumin excretion. The distribution of albuminuria in our data included the three stages: A1 ACR < 30 mg/gr (normal, n = 51, 34.2%); A2 ACR 30–300 mg/gr (microalbuminuria, n = 69, 46.3%) and A3 ACR > 300 mg/gr (macroalbuminuria/proteinuria, n = 29, 19.5%).
We used the International Diabetes Federation (IDF) criteria for MetS diagnosis [21]. Three or more of the following criteria were used for the diagnosis of MetS: systolic blood pressure (SBP) ≥ 130 mmHg and/or diastolic blood pressure (DBP) ≥ 85 mmHg and/or with pre-existed individual history of hypertension and/or with taking antihypertensive therapy, central obesity defined by a waist circumference ≥ 94 cm in males and ≥80 cm in females, triglycerides ≥ 150 mg/dL or specific treatment for this lipid abnormality, HDL-C < 40 mg/dL in males and <50 mg/dL in females and fasting plasma glucose ≥ 100 mg/dL or previously diagnosed type 2 diabetes mellitus. The prevalence of MetS in our data defined by more than three characteristics was equal to 80.5% (n = 120). The distribution of MetS components included: without any MetS component n = 2, with one MetS component n = 4, with two MetS components n = 23, with three MetS components n = 36, with four MetS components n = 44 and with five MetS components n = 40.
3. Data Analysis
Data were analyzed using SPSS 15.0 statistical package for Windows (SPSS Inc., Chicago, IL, USA) and expressed as mean ± standard deviation or as median value ± inter-quartile range for data that showed skewed distribution. Differences between mean values were assessed by using an unpaired t-test for two groups and data that showed skewed distributions were compared with Mann-Whitney U-test.
Correlations between categorical variables were defined by chi-square tests. p values less than 0.05 were considered significant. We built models using logistic regression analysis showing the risk for the development of low eGFR and albuminuria by the presence of MetS components adjusting to the age, gender, current smoking, alcohol taking, physical activity and the presence of diabetes mellitus.
4. Results
The Socio-demographical and biochemical characteristics of our data are shown in Table 1 and Table 2.

Table 1.
Socio-demographical characteristics of studied patients (n = 149).

Table 2.
Biochemical characteristics of studied patients (n = 149).
In Table 3 the differences between the subjects with and without MetS are shown. We observed that the patients with MetS were older and they had significantly higher BMI, ACR, triglycerides, glucose, waist circumference, but significantly lower HDL-C and eGFR than the patients without MetS.

Table 3.
Differences between groups of patients with (n = 120) and without (n = 29) metabolic syndrome (MetS) defined by more than three components.
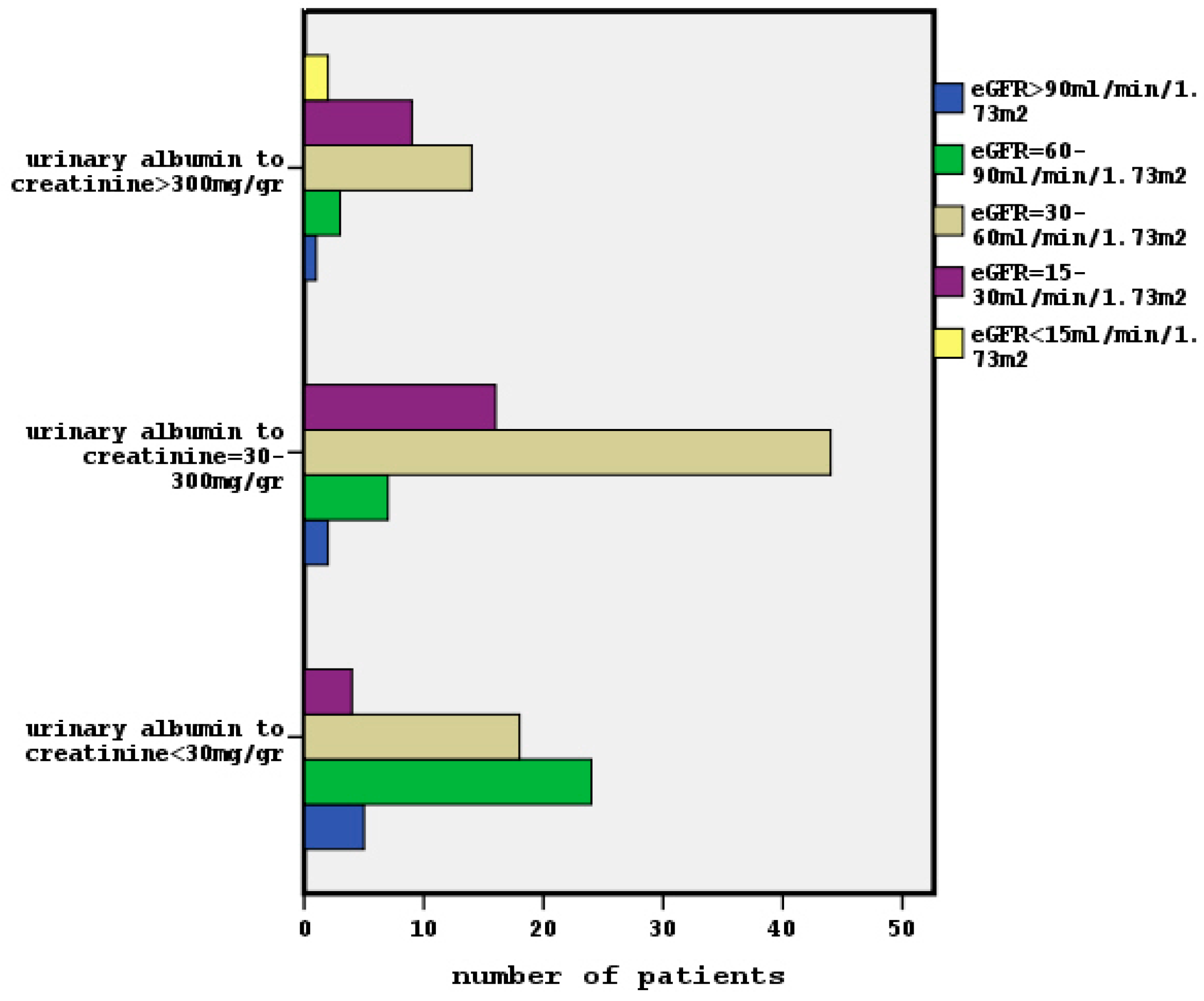
The relationship between classified eGFR and albuminuria is shown in Figure 1 (x2 = 41.8, p = 0.001). Five of our participants had an eGFR > 90 mL/min/1.73 m2 and an ACR < 30 mg/gr (G1 and A1 stages) meaning a normal kidney function.
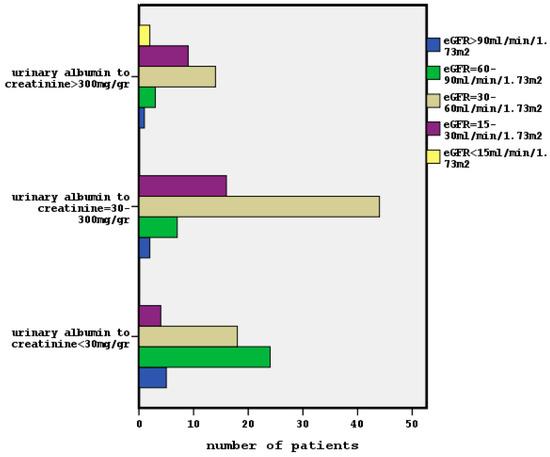
Figure 1.
The association between classified eGFR and classified albuminuria in our data (x2 = 41.8, p = 0.001).
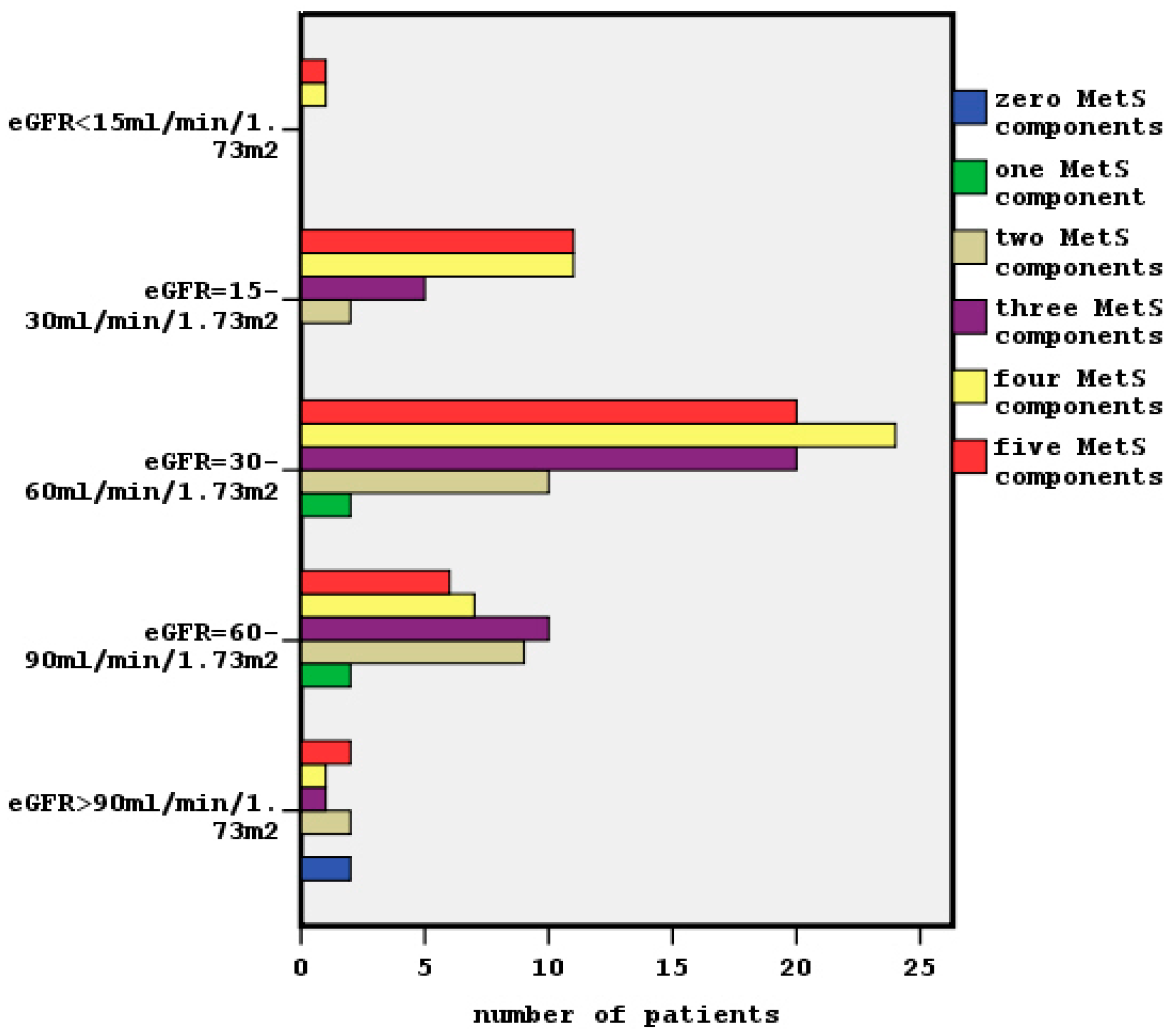
Chi-square tests showed a significant association between clustering MetS components and both classified eGFR and classified albuminuria (x2 = 50.3, p = 0.001, Figure 2 and x2 = 26.9, p = 0.003 respectively).We observed that the most of patients in G3 and G4 stages had four and five MetS components, although in G2 stage the presence of two and three MetS components was predominant. Similarly, the distribution of increased MetS components was shown in A2 and A3 stages of albuminuria. The two patients without any MetS characteristic were in stages G1 and A1, so they had normal kidney function.
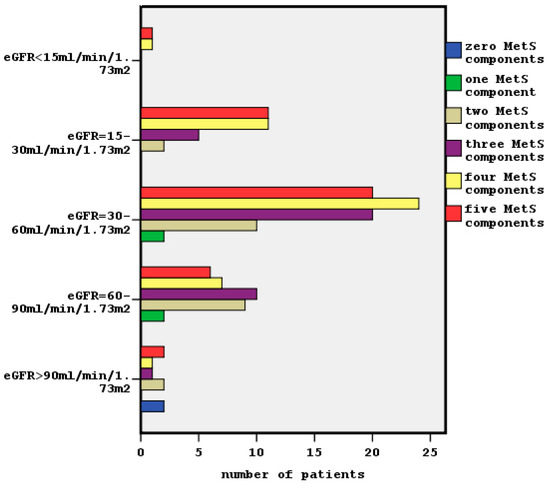
Figure 2.
The relationship between clustering of MetS and classified eGFR (x2 = 50.3, p = 0.001).
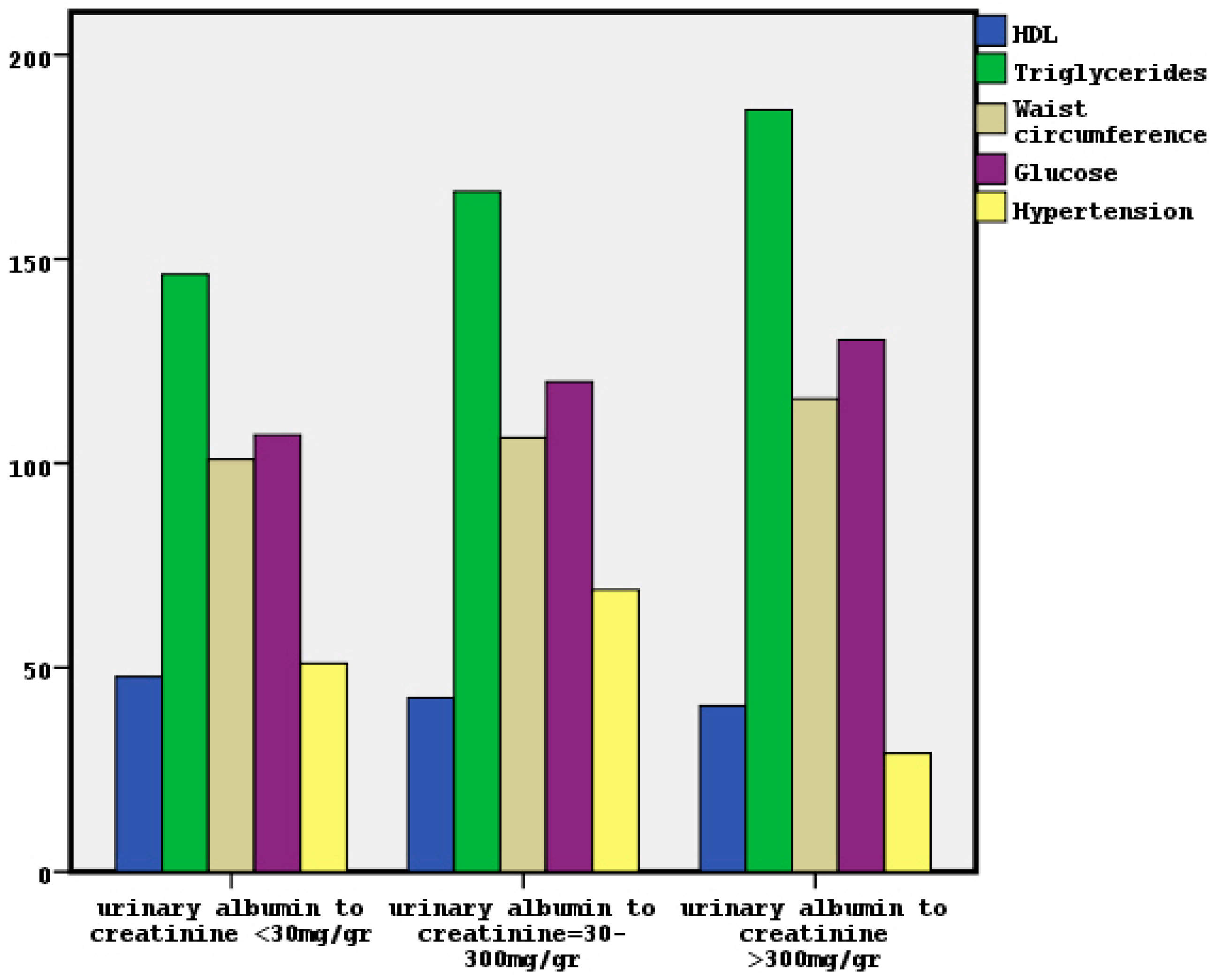
In Figure 3 the nomination of MetS characteristics in classified albuminuria is depicted. We noted significant association between classified albuminuria and high triglycerides, hypertension and high glucose by x2 tests (x2 = 11.8, p = 0.003, x2 = 11.4, p = 0.003 and x2 = 9.1, p = 0.01 respectively). The relationship between classified albuminuria and low HDL-C trended to be significant (x2 = 5.7, p = 0.06), although the association with waist circumference was found non-significant. On the other hand, we observed a significant association between classified eGFR and both high triglycerides and hypertension (x2 = 9.7, p = 0.04 and x2 = 16.1, p = 0.003 respectively). The association between classified eGFR and low HDL-C, high waist circumference or high glucose was found non-significant.
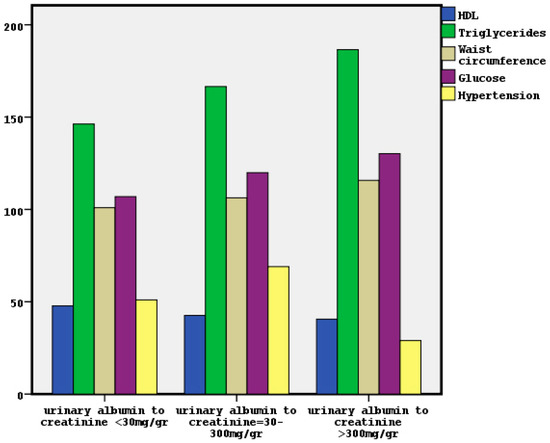
Figure 3.
The distribution of MetS components in classified albuminuria.
Moreover, x2 tests showed a significant association between the presence of MetS and the cause of renal disease, female gender and positive family history for cardiovascular events (x2 = 17.8, p = 0.003, x2 = 8.4, p = 0.003 and x2 = 7.3, p = 0.003 respectively). We could observe that everybody of diabetic patients had manifested MetS, although a few hypertensive subjects (n = 15) had not MetS. The association between MetS and smoking, alcohol taking and physical activity was found non-significant.
Table 4 and Table 5 show the risk factors for low eGFR and manifestation of albuminuria. The presence of MetS showed an odds 5.3-fold (1.6–17.8) higher for a low eGFR and 3.2-fold (1.2–8.8) higher for albuminuria adjusting to the age, gender, smoking, alcohol intake, physical activity and the presence of diabetes mellitus. The old age and female gender were also found to be significant risk factors for the low eGFR, although the presence of diabetes mellitus showed a risk 3.5-fold (1.1–11.3) higher for manifested albuminuria in combination with clustering of MetS.

Table 4.
Logistic regression analysis showing the predictors for the manifestation of a poor estimated glomerular filtration rate, eGFR < 60 mL/min/1.73 m2 (n = 149).

Table 5.
Logistic regression analysis showing the predictors for the manifestation of albuminuria (albumin-to-creatinine ratio in urine sample, ACR > 30 mg/gr) (n = 149).
5. Discussion
In this cross-sectional study, we aimed to examine the associations between metabolic components and (i) classified chronic renal disease based on eGFR category and (ii) classified albuminuria using the MetS as a dichotomous variable (0 to 5 components) in a population of patients who were followed in the outpatient clinic of a Department of Nephrology in Greece. We also evaluated the role of underlying disease including diabetes mellitus and socio-demographic characteristics.
In our data, the prevalence of a low eGFR (<60 mL/min/1.73 m2) was found in 71.8% of patients and the presence of microalbuminuria/macroalbuminuria in 65.8%. A few of our subjects had microalbuminuria/macroalbuminuria (n = 13) despite having an eGFR > 60 mL/min/1.73 m2 (G1 and G2 stages), as depicted in Figure 1. Conversely, some of our participants with a poor eGFR (n = 22) did not have albuminuria. Indeed, the kidney damage defined by the presence of albuminuria (ACR > 30 mg/gr) can be combined by a normal or raised GFR, in agreement with previous reports [9]. Only five of our enclosed subjects had a normal renal function determined by an ACR < 30 mg/gr in conjunction with an eGFR > 90 mL/min/1.73 m2.
The adjusted association between MetS and both low eGFR and the presence of albuminuria was significant in our data using, as covariates, the age, gender, current smoking, alcohol intake, physical activity, and the presence of diabetes mellitus. The presence of MetS showed an odds 5.3-fold (1.6–17.8) higher for the low eGFR in combination with the old age and female gender and a risk 3.2-fold (1.2–8.8) higher for albuminuria in combination with the presence of diabetes mellitus. In agreement, previous studies reported an elevated risk for CKD due to the presence of MetS [14,15].
The presence of diabetes mellitus showed an odds 3.5-fold (1.1–11.3) higher in our adjusted model for the prediction of albuminuria in conjunction with MetS, but not for a low eGFR prediction. MetS may contribute to the manifestation of albuminuria in patients with diabetes mellitus, but it does not contribute to an impaired glomerular filtration rate in diabetic patients. However, there is a debate about the role of MetS on the overall risk of patients with diabetes mellitus. Previously, it has been reported that inflammatory markers related to cardiovascular disease did not significantly differ in subjects with and without MetS [22]. On the other hand, albuminuria in diabetics may be associated with comorbidities due to diabetes mellitus [23,24].
Moreover, according to our findings, the presence of MetS in the elderly population may be associated with an impaired eGFR in these patients (mainly female) rather than with manifested albuminuria. Smoking and alcohol were not found to be significant risk factors for a poor eGFR or albuminuria in our data, despite their known association with CKD [3].
In the meantime, in this study, we observed that the patients who had advanced chronic renal disease (G3, G4 and G5 stages) presented with more MetS components (mainly 4 and 5 components) than the patients in the earlier chronic renal disease stages (whom had 2 or 3 MetS components) as it is shown in Figure 2. The findings for the prevalence of dichotomous MetS on microalbuminuria/macroalbuminuria were similar.
In agreement, it has previously been supported that MetS, when studied by number of components rather than by a single component, was a significant independent risk factor for CKD defined by eGFR < 60 mL/min/1.73 m2 [3]. Individuals with up to five components present had increased odds of developing CKD, as opposed to those without any components present, due perhaps to an additive detrimental effect by the cluster of MetS components rather than by single components [10,13].
Furthermore, the unadjusted association between classified albuminuria and separated MetS components showed that high triglycerides, high glucose, manifested hypertension and low HDL were significant factors, although only the high triglycerides and hypertension were found to be important factors for classified eGFR. As albuminuria determines the presence of underlying kidney damage, even with normal or high eGFR, the findings related to the CKD classification based on albuminuria may be more valid to define the role of metabolic abnormalities on kidney function, in comparison to the findings regarding classified eGFR.
In accordance, previously it has been reported that hypertriglyceridemia was associated with an increased risk of CKD development, and that high triglycerides were the main risk factor for proteinuria [25,26].
The relationship between MetS and CKD should be biologically plausible, but the pathophysiological mechanisms of MetS-induced kidney disease are not fully understood. Visceral obesity and adipose tissue expansion, which accompany the MetS, are highly correlated with insulin resistance [27]. Adipose tissue promotes chronic inflammation and oxidative stress that exacerbate insulin resistance. Insulin resistance is increasingly becoming recognized as a non-traditional risk factor for CKD because it is linked with the causal pathway to CKD rather than inflammation [3,28]. Insulin resistance and inflammation are associated with endothelial dysfunction, reduced synthase of endothelial nitric oxide, and worsening of renal hemodynamic function in conjunction with injury of podocytes resulting in hypertension and albuminuria [29,30]. Moreover, it has been reported that insulin resistance is associated with sodium retention, overproduction of low-density lipoprotein cholesterol, and hypertriglyceridemia, which may impair mitochondrial function and promote kidney cell damage [31].
Indeed, despite not evaluating insulin resistance in the present study, we noted that the subjects with MetS had significantly higher BMI and waist circumference, perhaps implicating a higher insulin resistance, in combination with significantly higher triglycerides, glucose, and ACR. However, they were found to have significantly lower HDL and eGFR than the patients without MetS.
Furthermore, the role of insulin resistance linked with the MetS establishment may explain the observed significant association between the MetS presence and the cause of renal disease. We noted that some patients with hypertensive nephrosclerosis had not manifested MetS, although the total of diabetic participants had MetS, due perhaps to increasingly insulin resistance in diabetics rather than in hypertensive patients.
Hypertension and diabetes mellitus and their combination may be associated with an increased prevalence of CKD [32,33]. Indeed, in our data, hypertension was recorded as the main cause of chronic renal disease. Type 2 diabetes mellitus was recorded as the secondary cause in agreement with recent previous study [14].
In this study, we also observed that the definition of MetS was significantly associated with female gender, in agreement with previous studies [14,34]. The reasons for this finding may include a complex of hormonal and socio-cultural interactions that predispose females to demonstrate more MetS components than males.
The relationship between MetS and positive family history for cardiovascular events was found to be significant, although the associations with smoking habits, alcohol intake and physical inactivity were found to be non-significant in this data. The association between alcohol consumption and MetS is controversial. Studies have shown a positive association and others have observed a negative association or no relation at all, as is the case in our study [35,36]. The controversy is attributed to a complicated relationship between alcohol consumption and each component of MetS.
Mild to moderate alcohol consumption may have a favorable influence on lipid metabolism, central obesity and glucose regulation [37], but, on the other hand, alcohol causes hypertension [38] and hypertriglyceridemia [39], resulting in alcohol-related MetS.
As the clustering of MetS was significantly associated with both classified eGFR and classified albuminuria in this study, bigger studies need to clarify the role of mild alcohol consumption on MetS outcomes in patients with impaired renal function. However, the change of lifestyle including physical activity, better nutrition and the avoidance of obesity should be very beneficial to adverse the intensive MetS and prevent the progression of cardiovascular and renal disease.
6. Limitations
The main limitation of this study is the cross-sectional nature of the study performed in a single-center: the Department of Nephrology. Also, the measurement of albumin using spot urine confers a concentration rather than a quantitative measurement.
7. Conclusions
The clustering of MetS was significantly associated with chronic renal disease defined by both classified eGFR and albuminuria. The definition of impaired renal function by the classification based on albuminuria was associated with more MetS components rather than the evaluation of eGFR category. MetS may contribute to the manifestation of albuminuria in patients with diabetes mellitus and to a poor eGFR in the elderly female population.
Author Contributions
Vaia Draikou: research plan, data collection, statistic analyses and manuscript writing. Sotiris Gavriil: research plan, data collection, approval of the written manuscript.
Conflicts of Interest
Author Vaia D. Raikou declares that she has no conflict of interest. Author Sotiris Gavriil declares that he has no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed oral consent was obtained from all individual participants included in the study.
References
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [PubMed]
- Ford, E.S.; Giles, W.H.; Dietz, W.H. Prevalence of the metabolic syndrome among US adults: Findings from the third National Health and Nutrition Examination Survey. JAMA 2002, 287, 356–359. [Google Scholar] [CrossRef] [PubMed]
- Zammit, R.A.; Katz, J.M.; Derby, C.; Bitzer, M.; Lipton, B.R. Chronic Kidney Disease in Non-Diabetic Older Adults: Associated Roles of the Metabolic Syndrome, Inflammation, and Insulin Resistance. PLoS ONE 2015, 10, e0139369. [Google Scholar]
- Guembe, M.J.; Toledo, E.; Barba, J.; Martínez-Vila, E.; González-Diego, P.; Irimia, P.; Díez, J.; Viñes, J.J. Association between metabolic syndrome or its components and asymptomatic cardiovascular disease in the RIVANA-study. Atherosclerosis 2010, 211, 612–617. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, M.; Bhuket, T.; Torres, S.; Liu, B.; Wong, R.J. Prevalence of the metabolic syndrome in the United States, 2003–2012. JAMA 2015, 313, 1973–1974. [Google Scholar] [PubMed]
- Tanamas, S.K.; Magliano, D.J.; Lynch, B.; Sethi, P.; Willenberg, L.; Polkinghorne, K.R. The Australian Diabetes, Obesity and Lifestyle Study (AusDiab); Baker IDI Heart and Diabetes Institute: Melbourne, Australia, 2013. [Google Scholar]
- Oguoma, V.M.; Nwose, E.U.; Richards, R.S. Prevalence of cardio-metabolic syndrome in Nigeria: A systematic review. Public Health 2015, 129, 413–423. [Google Scholar] [CrossRef] [PubMed]
- Sesso, R.C.; Lopes, A.A.; Thomé, F.S.; Lugon, J.R.; Martins, C.T. Brazilian Chronic Dialysis Survey 2016. J. Bras. Nefrol. 2017, 39, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Moţa, E.; Popa, S.G.; Moţa, M.; Mitrea, A.; Penescu, M.; Tuţă, L.; Serafinceanu, C.; Hâncu, N.; Gârneaţă, L.; Verzan, C. Prevalence of chronic kidney disease and its association with cardio-metabolic risk factors in the adult Romanian population: The PREDATORR study. Int. Urol. Nephrol. 2015, 47, 1831–1838. [Google Scholar] [CrossRef] [PubMed]
- Thomas, G.; Sehgal, R.A.; Kashyap, R.S.; Srinivas, R.T.; Kirwan, P.J.; Navaneethan, D.S. Metabolic Syndrome and Kidney Disease: A Systematic Review and Meta-analysis. Clin. J. Am. Soc. Nephrol. 2011, 6, 2364–2373. [Google Scholar] [CrossRef] [PubMed]
- Tozawa, M.; Iseki, C.; Tokashiki, K.; Chinen, S.; Kohagura, K.; Kinjo, K.; Takishita, S.; Iseki, K. Metabolic syndrome and risk of developing chronic kidney disease in Japanese adults. Hypertens. Res. 2007, 30, 937–943. [Google Scholar] [CrossRef] [PubMed]
- Ming, J.; Xu, S.; Yang, C.; Gao, B.; Wan, Y.; Xing, Y.; Zhang, L.; Yang, W.; Ji, Q.; China National Diabetes and Metabolic Disorders Study Group. Metabolic syndrome and chronic kidney disease in general Chinese adults: Results from the 2007–2008 China National Diabetes and Metabolic Disorders Study. Clin. Chim. Acta 2014, 430, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Kurella, M.; Chertow, G.M.; Fried, L.F.; Cummings, S.R.; Harris, T.; Simonsick, E.; Satterfield, S.; Ayonayon, H.; Yaffe, K. Chronic kidney disease and cognitive impairment in the elderly: The health, aging, and body composition study. J. Am. Soc. Nephrol. JASN 2005, 16, 2127–2133. [Google Scholar] [CrossRef] [PubMed]
- Alswat, K.A.; Althobaiti, A.; Alsaadi, K.; Alkhaldi, A.S.; Alharthi, M.M.; Abuharba, W.A.; Alzaidi, A.A. Prevalence of Metabolic Syndrome Among the End-Stage Renal Disease Patients on Hemodialysis. J. Clin. Med. Res. 2017, 9, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Bonnet, F.; Marre, M.; Halimi, J.M.; Stengel, B.; Lange, C.; Laville, M.; Tichet, J.; Balkau, B. Waist circumference and the metabolic syndrome predict the development of elevated albuminuria in non-diabetic subjects: The DESIR Study. J. Hypertens. 2006, 24, 1157–1163. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.-T.; Huang, J.-W.; Chiang, C.-K.; Yen, C.-J.; Hung, K.-Y.; Wu, K.-D. Metabolic syndrome and insulin resistance as risk factors for development of chronic kidney disease and rapid decline in renal function in elderly. JECM 2012, 97, 1268–1276. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Recommendations on Physical Activity for Health; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- World Health Organization. BMI Classification. Global Database on Body Mass Index: An Interactive Surveillance Tool for Monitoring Nutrition Transition; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- WHO Expert Consultation. Waist Circumference and Waist-Hip Ratio; Report of a WHO Expert Consultation Geneva; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Kdigo CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 2013, 3, 1–150. [Google Scholar]
- Alberti, G.; Zimmet, P.; Shaw, J.; Grundy, S. IDF Worldwide Definition of the Metabolic Syndrome; International Diabetes Federation (IDF): Brussels, Belgium, 2006; Volume 1. [Google Scholar]
- Wen, M.J.; Hsieh, C.H.; Wu, C.Z.; Hsiao, F.C.; Hsia, T.L.; Hung, Y.J.; Pei, D. The adipokines and inflammatory marker in young type 2 diabetics with metabolic syndrome: A pilot study. Obes. Res. Clin. Pract. 2013, 7, e206–e210. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, S.; Saito, I.; Yamamoto, S.; Miyake, T.; Ueda, T.; Niiya, T.; Torisu, M.; Kumagi, T.; Sakai, T.; Minami, H. Nocturnal intermittent hypoxia as an associated risk factor for microalbuminuria in Japanese patients with type 2 diabetes mellitus. Eur. J. Endocrinol. 2013, 169, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, S.; Sakai, T.; Niiya, T.; Miyaoka, H.; Miyake, T.; Yamamoto, S.; Tanaka, K.; Ueda, T.; Senba, H.; Torisu, M. B-type natriuretic peptide and renal function in Japanese patients with type 2 diabetes mellitus: The Dogo Study. Endocr. J. 2017, 64, 1131–1136. [Google Scholar] [CrossRef] [PubMed]
- Tozawa, M.; Iseki, K.; Iseki, C.; Oshiro, S.; Ikemiya, Y.; Takishita, S. Triglyceride, but not total cholesterol or low-density lipoprotein cholesterol levels, predict development of proteinuria. Kidney Int. 2002, 62, 1743–1749. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Kong, X.; Jia, X.; Li, W.; Wang, Z.; Cui, M.; Xu, D. Association between metabolic syndrome and chronic kidney disease in a Chinese urban population. Clin. Chim. Acta 2017, 470, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Wisse, B.E. The inflammatory syndrome: The role of adipose tissue cytokines in metabolic disorders linked to obesity. J. Am. Soc. Nephrol. 2004, 15, 2792–2800. [Google Scholar] [CrossRef] [PubMed]
- Liao, M.-T.; Sung, C.-C.; Hung, K.-C.; Wu, C.-C.; Lo, L.; Lu, K.-C. Insulin resistance in patients with chronic kidney disease. J. Biomed. Biotechnol. 2012, 691369, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Lerman, L.O. The metabolic syndrome and chronic kidney disease. Transl. Res. 2017, 183, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.C.; Chang, H.Y.; Huang, M.C.; Hwang, S.J.; Yang, Y.C.; Tai, T.Y.; Yang, H.J.; Chang, C.T.; Chang, C.J.; Li, Y.S. Association between insulin resistance and development of microalbuminuria in type 2 diabetes: A prospective cohort study. Diabetes Care 2011, 34, 982–987. [Google Scholar] [CrossRef] [PubMed]
- Gluba, A.; Mikhailidis, D.; Lip, G.Y.H.; Hannam, S.; Rysz, J.; Banach, M. Metabolic syndrome and renal disease. Int. J. Cardiol. 2013, 164, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Michishita, R.; Matsuda, T.; Kawakami, S.; Tanaka, S.; Kiyonaga, A.; Tanaka, H.; Morito, N.; Higaki, Y. Hypertension and hyperglycemia and the combination there of enhances the incidence of chronic kidney disease (CKD) in middle-aged and older males. Clin. Exp. Hypertens. 2017, 7, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kurata, M.; Tsuboi, A.; Takeuchi, M.; Fukuo, K.; Kazumi, T. Association of Metabolic Syndrome with Chronic Kidney Disease in Elderly Japanese Women: Comparison by Estimation of Glomerular Filtration Rate from Creatinine, Cystatin C, and Both. Metab. Syndr. Relat. Disord. 2016, 14, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.; Zimmet, P.; Shaw, J.; IDF Epidemiology Task Force Consensus Group. The metabolic syndrome—A new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- Fan, A.Z.; Russell, M.; Dorn, J.; Freudenheim, J.L.; Nochajski, T.; Hovey, K.; Trevisan, M. Lifetime alcohol drinking pattern is related to the prevalence of metabolic syndrome. The Western New York Health Study (WNYHS). Eur. J. Epidemiol. 2006, 21, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Djousse, L.; Arnett, D.K.; Eckfeldt, J.H.; Province, M.A.; Singer, M.R.; Ellison, R.C. Alcohol consumption and metabolic syndrome: Does the type of beverage matter? Obes. Res. 2004, 12, 1375–1385. [Google Scholar] [CrossRef] [PubMed]
- Koppes, L.L.; Dekker, J.M.; Hendriks, H.F.; Bouter, L.M.; Heine, R.J. Moderate alcohol consumption lowers the risk of type 2 diabetes: A meta-analysis of prospective observational studies. Diabetes Care 2005, 28, 719–725. [Google Scholar] [CrossRef] [PubMed]
- Xin, X.; He, J.; Frontini, M.G.; Ogden, L.G.; Motsamai, O.I.; Whelton, P.K. Effects of alcohol reduction on blood pressure: A meta-analysis of randomized controlled trials. Hypertension 2001, 38, 1112–1117. [Google Scholar] [CrossRef] [PubMed]
- Kato, I.; Kiyohara, Y.; Kubo, M.; Tanizaki, Y.; Arima, H.; Iwamoto, H.; Shinohara, N.; Nakayama, K.; Fujishima, M. Insulin-mediated effects of alcohol intake on serum lipid levels in a general population: The Hisayama Study. J. Clin. Epidemiol. 2003, 56, 196–204. [Google Scholar] [CrossRef]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).