Association between Low Serum Bicarbonate Concentrations and Cardiovascular Disease in Patients in the End-Stage of Renal Disease
Abstract
:1. Introduction and Aim
2. Methods
2.1. Patients
2.2. Approval and Consent
2.3. Blood Collection
2.4. Laboratory Measurements
2.5. Hemodynamic Measurements
2.6. Data Analysis
3. Results
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Conflicts of Interest
References
- Guérin, A.P.; Pannier, B.; Marchais, S.J.; London, G.M. Cardiovascular disease in the dialysis population: Prognostic significance of arterial disorders. Curr. Opin. Nephrol. Hypertens. 2006, 15, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Wen, C.P.; Cheng, T.Y.; Tsai, M.K.; Chang, Y.C.; Chan, H.T.; Tsai, S.P.; Chiang, P.H.; Hsu, C.C.; Sung, P.K.; Hsu, Y.H.; et al. All-cause mortality attributable to chronic kidney disease: A prospective cohort study based on 462,293 adults in Taiwan. Lancet 2008, 28, 2173–2182. [Google Scholar] [CrossRef]
- Stenvinkel, P.; Heimbürger, O.; Paultre, F.; Diczfalusy, U.; Wang, T.; Berglund, L.; Jogestrand, T. Strong association between malnutrition, inflammation, and atherosclerosis in chronic renal failure. Kidney Int. 1999, 55, 1899–1911. [Google Scholar] [CrossRef] [PubMed]
- Inaba, M.; Ueda, M. Vascular calcification—Pathological mechanism and clinical application—. The significance of arterial calcification in unstable plaques. Clin. Calcium 2015, 25, 679–686. [Google Scholar] [PubMed]
- Kalantar-Zadeh, K.; Mehrotra, R.; Fouque, D.; Kopple, J.D. Metabolic acidosis and malnutrition-inflammation complex syndrome in chronic renal failure. Semin. Dial. 2004, 17, 455–465. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Shoji, S.; Yamakawa, T.; Wada, A.; Suzuki, K.; Iseki, K.; Tsubakihara, Y. Predialysis and postdialysis pH and bicarbonate and risk of all-cause and cardiovascular mortality in long-term hemodialysis patients. Am. J. Kidney Dis. 2015, 66, 469–478. [Google Scholar] [CrossRef] [PubMed]
- Chiu, Y.W.; Mehrotra, R. What should define optimal correction of metabolic acidosis in chronic kidney disease? Semin. Dial. 2010, 23, 411–414. [Google Scholar] [CrossRef] [PubMed]
- Chauveau, P.; Nguyen, H.; Combe, C.; Chêne, G.; Azar, R.; Cano, N.; Canaud, B.; Fouque, D.; Laville, M.; Leverve, X.; et al. Dialyzer membrane permeability and survival in hemodialysis patients. Am. J. Kidney Dis. 2005, 45, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Daugirdas, J.T. Second generation logarithmic estimates of single-pool variable volume Kt/V: An analysis of error. J. Am. Soc. Nephrol. 1993, 4, 1205–1213. [Google Scholar] [PubMed]
- Kirschbaum, B. Spurious metabolic acidosis in hemodialysis patients. Am. J. Kidney Dis. 2000, 35, 1068–1071. [Google Scholar] [CrossRef]
- Daugirdas, J.T. Simplified equations for monitoring Kt/V, PCRn, eKt/V, and ePCRn. Adv. Ren. Replace Ther. 1995, 2, 295–304. [Google Scholar] [PubMed]
- Nitta, K.; Kawashima, A.; Yumura, W.; Naruse, M.; Oba, T.; Kabaya, T.; Nihei, H. Plasma concentration of brain natriuretic peptide as an indicator of cardiac ventricular function in patients on hemodialysis. Am. J. Nephrol. 1998, 18, 411–415. [Google Scholar] [CrossRef] [PubMed]
- Vaziri, N.D. Dyslipidemia of chronic renal failure: The nature, mechanisms and potential consequences. Am. J. Physiol. Ren. Physiol. 2006, 290, F262–F272. [Google Scholar] [CrossRef] [PubMed]
- Vaziri, N.D. Oxidative stress in chronic renal failure: The nature, mechanism and consequences. Semin. Nephrol. 2004, 24, 469–473. [Google Scholar] [CrossRef] [PubMed]
- Price, S.R.; Du, J.D.; Bailey, J.L.; Mitch, W.E. Molecular mechanisms regulating protein turnover in muscle. Am. J. Kidney Dis. 2001, 37, S112–S114. [Google Scholar] [CrossRef] [PubMed]
- London, G.M.; Drueke, T.B. Atherosclerosis and arteriosclerosis in chronic renal failure. Kidney Int. 1997, 51, 1678–1695. [Google Scholar] [CrossRef] [PubMed]
- Vashistha, T.; Kalantar-Zadeh, K.; Molnar, M.Z.; Torlén, K.; Mehrotra, R. Dialysis modality and correction of uremic metabolic acidosis: Relationship with all-cause and cause-specific mortality. Clin. J. Am. Soc. Nephrol. 2013, 8, 254–264. [Google Scholar] [CrossRef] [PubMed]
- Maurer, M.S.; Burkhoff, D.; Fried, L.P.; Gottdiener, J.; King, D.L.; Kitzman, D.W. Ventricular structure and function in hypertensive participants with heart failure and a normal ejection fraction: The cardiovascular health study. J. Am. Coll. Cardiol. 2007, 49, 972–981. [Google Scholar] [CrossRef] [PubMed]
- McDermott, M.M.; Liu, K.; Greenland, P.; Guralnik, J.M.; Criqui, M.H.; Chan, C.; Pearce, W.H.; Schneider, J.R.; Ferrucci, L.; Celic, L.; et al. Functional decline in peripheral arterial disease: Associations with the ankle brachial index and leg symptoms. J. Am. Med. Assoc. 2004, 292, 453–461. [Google Scholar] [CrossRef] [PubMed]
- Mehrotra, R.; Kopple, J.D.; Wolfson, M. Metabolic acidosis in maintenance dialysis patients: Clinical considerations. Kidney Int. Suppl. 2003, 88, S13–S25. [Google Scholar] [CrossRef]
- Bommer, J.; Locatelli, F.; Satayathum, S.; Keen, M.L.; Goodkin, D.A.; Saito, A.; Akiba, T.; Port, F.K.; Young, E.W. Association of predialysis serum bicarbonate levels with risk of mortality and hospitalization in the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am. J. Kidney Dis. 2004, 44, 661–671. [Google Scholar] [CrossRef]
- Wu, D.Y.; Shinaberger, C.S.; Regidor, D.L.; McAllister, C.J.; Kopple, J.D.; Kalantar-Zadeh, K. Association between serum bicarbonate and death in hemodialysis patients: Is it better to be acidotic or alkalotic? Clin. J. Am. Soc. Nephrol. 2006, 1, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Kovacic, V.; Roguljic, L.; Kovacic, V. Metabolic acidosis of chronically hemodialyzed patients. Am. J. Nephrol. 2003, 23, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Yonova, D. Vascular calcification and metabolic acidosis in end stage renal disease. Hippokratia 2009, 13, 139–140. [Google Scholar] [PubMed]
- Al-Aly, Z. Vascular calcification in uremia: What is new and where are we going? Adv. Chronic Kidney Dis. 2008, 15, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Swarthout, J.T.; D’Alonzo, R.C.; Selvamurugan, N.; Partridge, N.C. Parathyroid hormone-dependent signaling pathways regulating genes in bone cells. Gene 2002, 282, 1–17. [Google Scholar] [CrossRef]
- Shioi, A.; Mori, K.; Jono, S.; Wakikawa, T.; Hiura, Y.; Koyama, H.; Okuno, Y.; Nishizawa, Y.; Morii, H. Mechanism of atherosclerotic calcification. Z. Kardiol. 2000, 89, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Johnson, R.C.; Leopold, J.A.; Loscalzo, J. Vascular calcification: Pathobiological mechanisms and clinical implications. Circ. Res. 2006, 99, 1044–1059. [Google Scholar] [CrossRef] [PubMed]
- Schutte, E.; Lambers Heerspink, H.J.; Lutgers, H.L.; Bakker, S.J.; Vart, P.; Wolffenbuttel, B.H.; Umanath, K.; Lewis, J.B.; de Zeeuw, D.; Gansevoort, R.T. Serum bicarbonate and kidney disease progression and cardiovascular outcome in patients with diabetic nephropathy: A post hoc analysis of the renaal (reduction of end points in non-insulin-dependent diabetes with the angiotensin II antagonist losartan) study and IDNT (Irbesartan diabetic nephropathy trial). Am. J. Kidney Dis. 2015, 66, 450–458. [Google Scholar] [PubMed]
- Dobre, M.; Yang, W.; Chen, J.; Drawz, P.; Hamm, L.L.; Horwitz, E.; Hostetter, T.; Jaar, B.; Lora, C.M.; Nessel, L.; et al. Association of serum bicarbonate with risk of renal and cardiovascular outcomes in CKD: A report from the Chronic Renal Insufficiency Cohort (CRIC) study. Am. J. Kidney Dis. 2013, 62, 670–678. [Google Scholar] [CrossRef] [PubMed]
- Checherita, I.A.; David, C.; Ciocalteu, A.; Lascar, I.; Budala, L. Oral treatment of metabolic acidosis in hemodialyzed patients and the implications on the hemodynamic status. Rom. J. Morphol. Emplryol. 2013, 54, 539–543. [Google Scholar]
- Fontes-Carvalho, R.; Leite-Moreira, A. The pathophysiology of heart failure with preserved ejection fraction and its therapeutic implications. Rev. Port. Cardiol. 2009, 28, 63–82. [Google Scholar] [PubMed]
- Mathew, A.T.; Fishbane, S.; Obi, Y.; Kalantar-Zadeh, K. Preservation of residual kidney function in hemodialysis patients: Reviving an old concept. Kidney Int. 2016, 90, 262–271. [Google Scholar] [CrossRef] [PubMed]
- Marrón, B.; Remón, C.; Pérez-Fontán, M.; Quirós, P.; Ortíz, A. Benefits of preserving residual renal function in peritoneal dialysis. Kidney Int. Suppl. 2008, S42–S51. [Google Scholar] [CrossRef] [PubMed]
- Chang, T.I.; Oh, H.J.; Kang, E.W.; Yoo, T.H.; Shin, S.K.; Kang, S.W.; Choi, K.H.; Han, D.S.; Han, S.H. A low serum bicarbonate concentration as a risk factor for mortality in peritoneal dialysis patients. PLoS ONE 2013, 8, e82912. [Google Scholar] [CrossRef] [PubMed]
| Patients with Serum Bicarbonate Less than 22 mmol/L (n = 41) | Patients with Serum Bicarbonate More than 22 mmol/L (n = 11) | |
|---|---|---|
| Sex (males/females) | 25 (61%)–16 (39%) | 7 (63.6%)–4 (36.4%) |
| Age (years) | 60.5 ± 14.5 * | 48.7 ± 16 |
| Dialysis vintage (years) | 7.6 ± 7.1 | 7.4 ± 5.9 |
| Kt/V for urea | 1.4 ± 0.20 | 1.4 ± 0.23 |
| nPCR (g/kg/day) | 2.4 ± 0.54 | 2.4 ± 0.39 |
| Urine volume (mL/day) | 238.4 ± 166 | 190 ± 96.4 |
| BMI (kg/m2) | 24.5 ± 3.4 | 23.9 ± 2.13 |
| Serum bicarbonate (mmol/L) | 19.3 ± 1.9 * | 22.8 ± 1.03 |
| i-PTH (pg/mL) | 14.4 ± 231.6 * | 106.6 ± 94.7 |
| Hb (gr/dL) | 11.8 ± 1.3 | 12.3 ± 1.3 |
| Albumin (gr/dL) | 3.9 ± 0.2 * | 4.15 ± 0.2 |
| LDL/HDL | 2.4 ± 0.8 | 2.6 ± 0.8 |
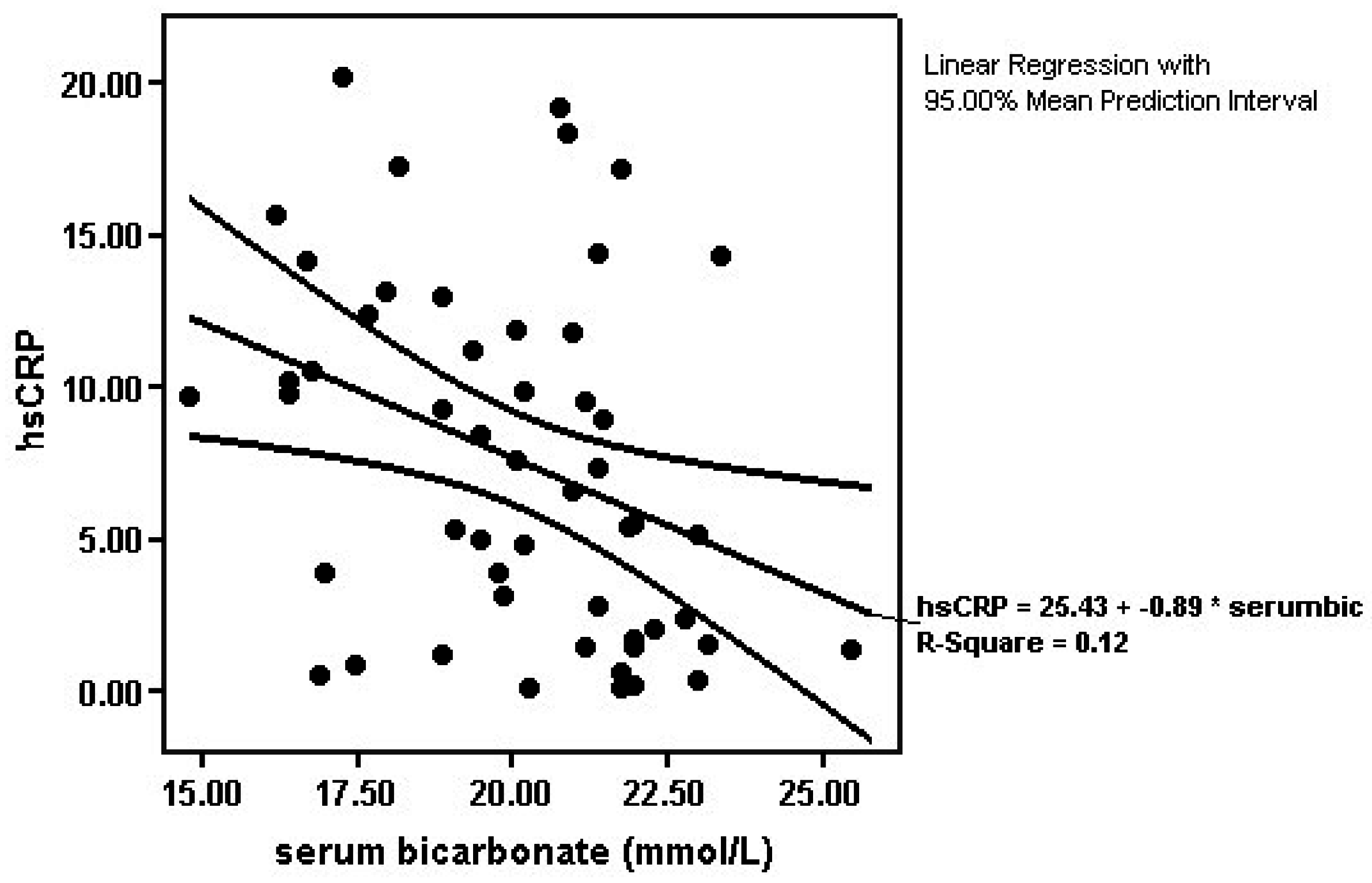
| hsCRP (mg/L) | 8.74 ± 5.7 * | 3.32 ± 4.03 |
| oxLDL (ng/mL) | 140.7 ± 187.1 | 127.4 ± 112 |
| MBP (mmHg) | 97.1 ± 11.8 | 91.7 ± 11.2 |
| ABPI | 1.04 ± 0.4 | 1.01 ± 0.3 |
| Diabetes mellitus (yes/no) | 5 (12.2%)/36 (87.8%) | 0 (0%)/11 (100%) |
| Hypertension (yes/no) | 18 (44%)/23 (56.1%) * | 1 (9%)/10 (91%) |
| Smoking (yes/no) | 12 (29.3%)/29 (70.7%) | 3 (27.3%)/8 (72.7%) |
| Coronary artery disease (yes/no) | 12 (29.3%)/29 (70.7%) | 2 (18.2%)/9 (81.8%) |
| Heart failure (EF<50%) (yes/no) | 10 (24.4%)/31 (75.6%) | 1 (9%)/10 (91%) |
| EF (%) | 49.8 ± 14.8 | 56.6 ± 11.4 |
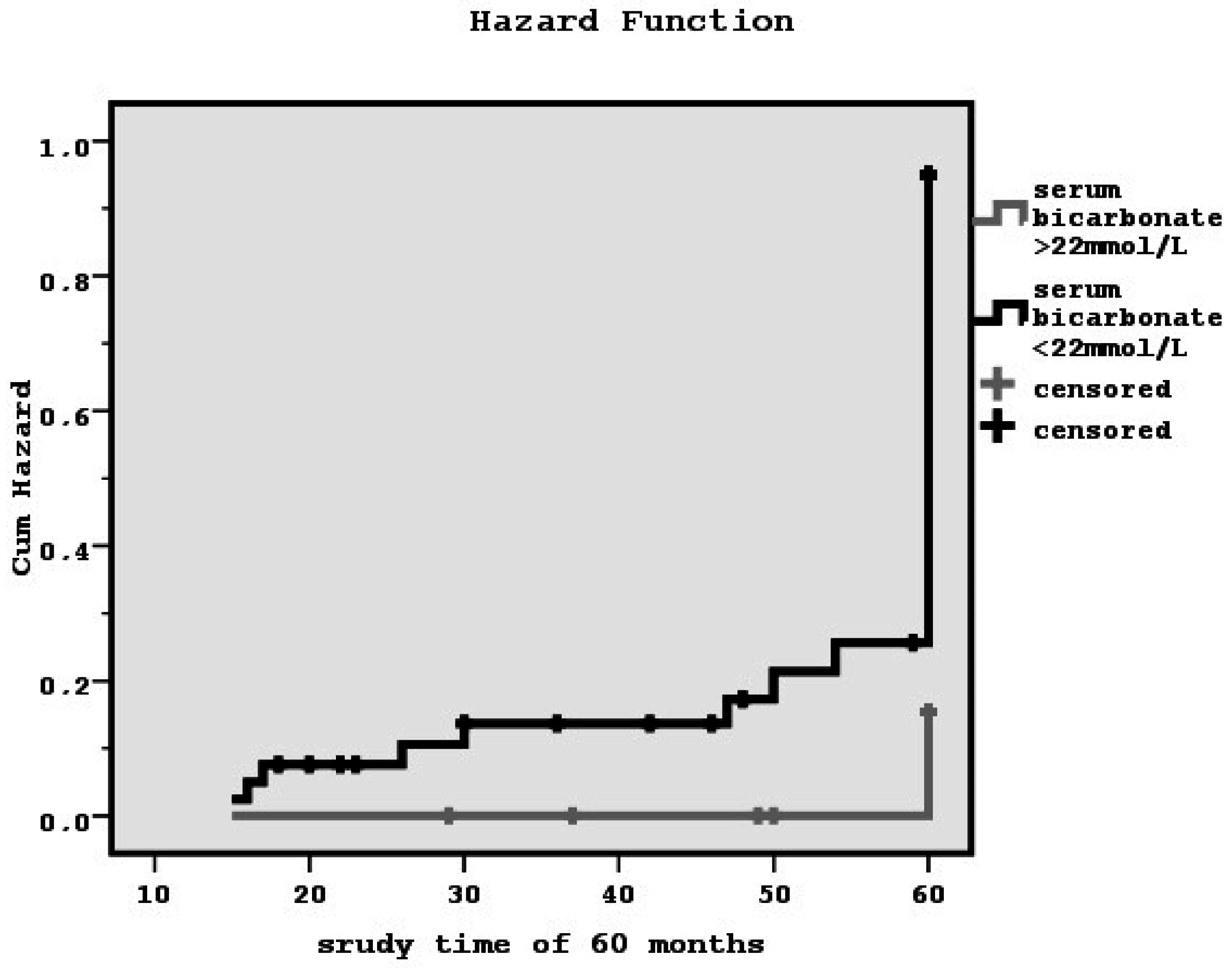
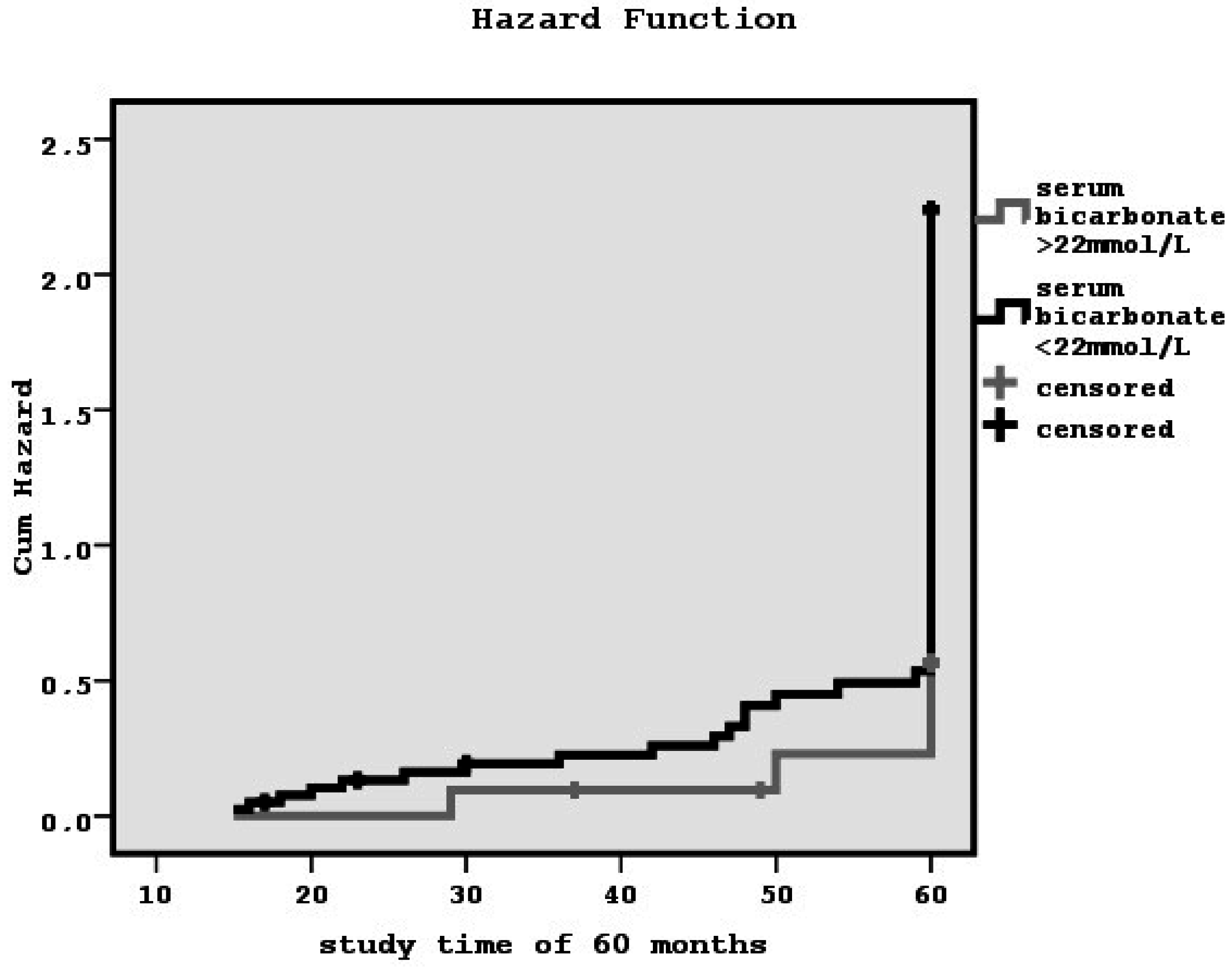
| Diastolic dysfunction (yes/no) | 34 (82.9%)/7 (17.1%) * | 4 (36.4%)/7 (63.6%) |
| E/A ratio | 0.98 ± 0.1 * | 1.2 ± 0.2 |
| Peripheral vascular disease (yes/no) | 19 (46.3%)/22 (53.7%) * | 1 (9%)/10 (91%) |
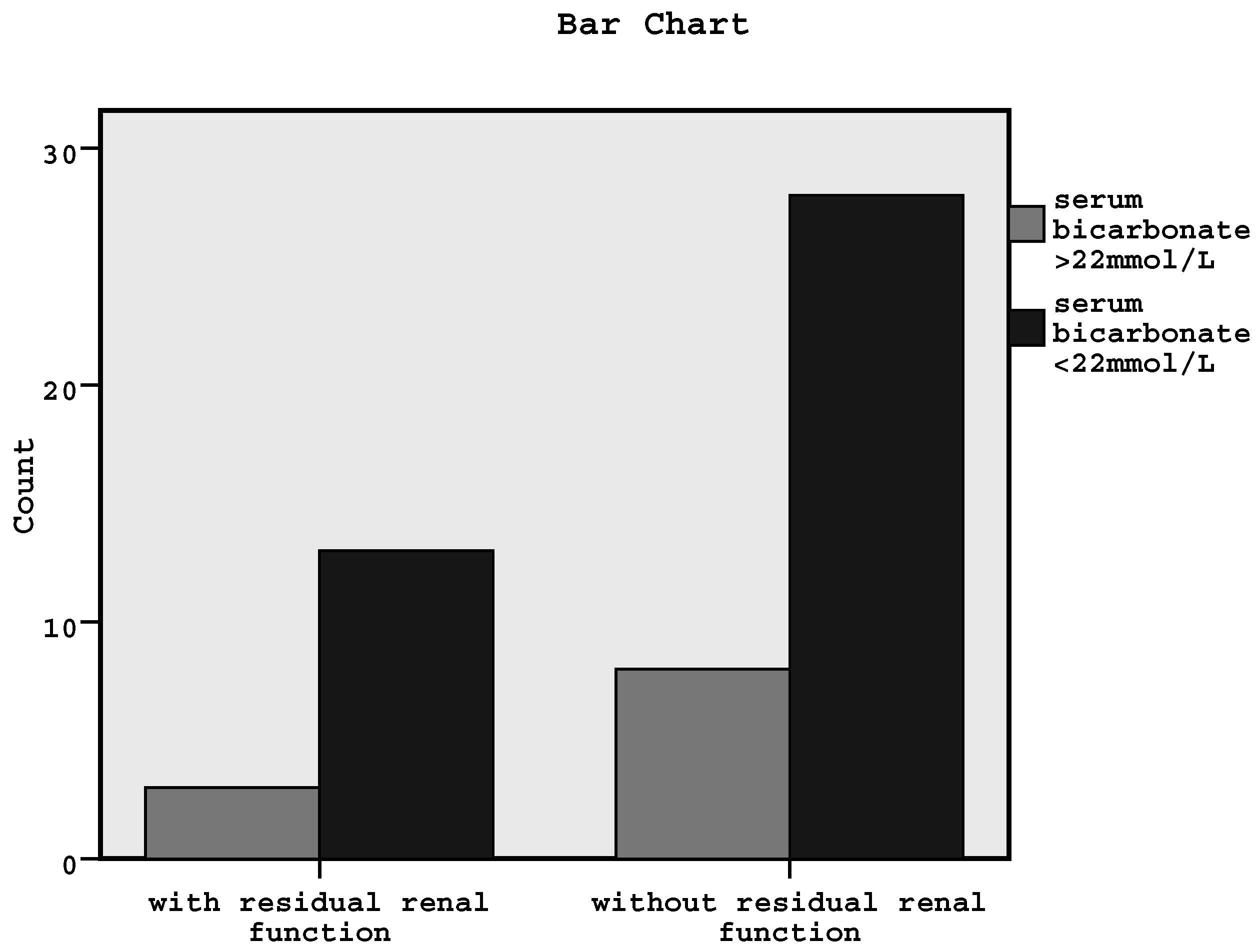
| Residual renal function (yes/no) | 13 (31.7%)/28 (68.3%) * | 3 (27.3%)/8 (72.7%) |
| Phosphate binders (yes/no) | 34 (82.9%)/7 (17.1%) | 8 (72.7%)/3 (27.3%) 5 (45.4%) 3 (27.2%) |
| Sevelamer carbonate | 16 (39%) | |
| Sevelamer hydrochloride | 7 (17.1%) | |
| Lanthanum | 8 (19.5%) | |
| Aluminum hydroxide | 3 (7.3%) |
| p-Value | Odds Ratio | Confidence Interval | |
|---|---|---|---|
| Interdialytic urine volume | 0.02 | 1.008 | 1.001–1.015 |
| Kt/V for urea | 0.8 | 0.35 | 0.009–2.95 |
| LDL/HDL | 0.14 | 0.20 | 0.02–1.76 |
| i-PTH | 0.17 | 0.99 | 0.98–1.003 |
| Serum bicarbonate | 0.03 | 0.45 | 0.20–0.96 |
| p-Value | Odds Ratio | Confidence Interval | |
|---|---|---|---|
| Age | 0.8 | 0.99 | 0.9–1.06 |
| Family atherosclerotic history | 0.5 | 1.9 | 0.2–16.9 |
| Previous atherosclerotic events | 0.07 | 10.8 | 0.7–149.7 |
| Cardioactive medications | 0.3 | 2.3 | 0.4–11.9 |
| Smoking | 0.5 | 0.4 | 0.03–6.3 |
| Urine volume | 0.02 | 1.01 | 1–1.02 |
| LDL/HDL | 0.8 | 1.12 | 0.4–3.04 |
| i-PTH | 0.05 | 1.008 | 1–1.02 |
| Serum bicarbonate | 0.4 | 1.3 | 0.6–2.8 |
| p-Value | Odds Ratio | Confidence Interval | |
|---|---|---|---|
| Age | 0.1 | 1.04 | 0.9–1.1 |
| Sex | 0.3 | 0.47 | 0.09–2.2 |
| Diabetes mellitus | 0.6 | 0.3 | 0.006–22.1 |
| Dialysis vintage | 0.03 | 1.3 | 1.02–1.7 |
| Urine volume | 0.02 | 1.007 | 1.001–1.02 |
| nPCR | 0.4 | 0.5 | 0.1–2.37 |
| Serum albumin | 0.03 | 0.005 | 0–0.7 |
| hsCRP | 0.7 | 1.04 | 0.8–1.3 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raikou, V.D.; Kyriaki, D. Association between Low Serum Bicarbonate Concentrations and Cardiovascular Disease in Patients in the End-Stage of Renal Disease. Diseases 2016, 4, 36. https://doi.org/10.3390/diseases4040036
Raikou VD, Kyriaki D. Association between Low Serum Bicarbonate Concentrations and Cardiovascular Disease in Patients in the End-Stage of Renal Disease. Diseases. 2016; 4(4):36. https://doi.org/10.3390/diseases4040036
Chicago/Turabian StyleRaikou, Vaia D., and Despina Kyriaki. 2016. "Association between Low Serum Bicarbonate Concentrations and Cardiovascular Disease in Patients in the End-Stage of Renal Disease" Diseases 4, no. 4: 36. https://doi.org/10.3390/diseases4040036
APA StyleRaikou, V. D., & Kyriaki, D. (2016). Association between Low Serum Bicarbonate Concentrations and Cardiovascular Disease in Patients in the End-Stage of Renal Disease. Diseases, 4(4), 36. https://doi.org/10.3390/diseases4040036






