Impact of Sacubitril/Valsartan on Cardiac Reverse Remodeling in Patients with Heart Failure Undergoing Cardiac Resynchronization Therapy
Abstract
1. Introduction
2. Materials and Methods
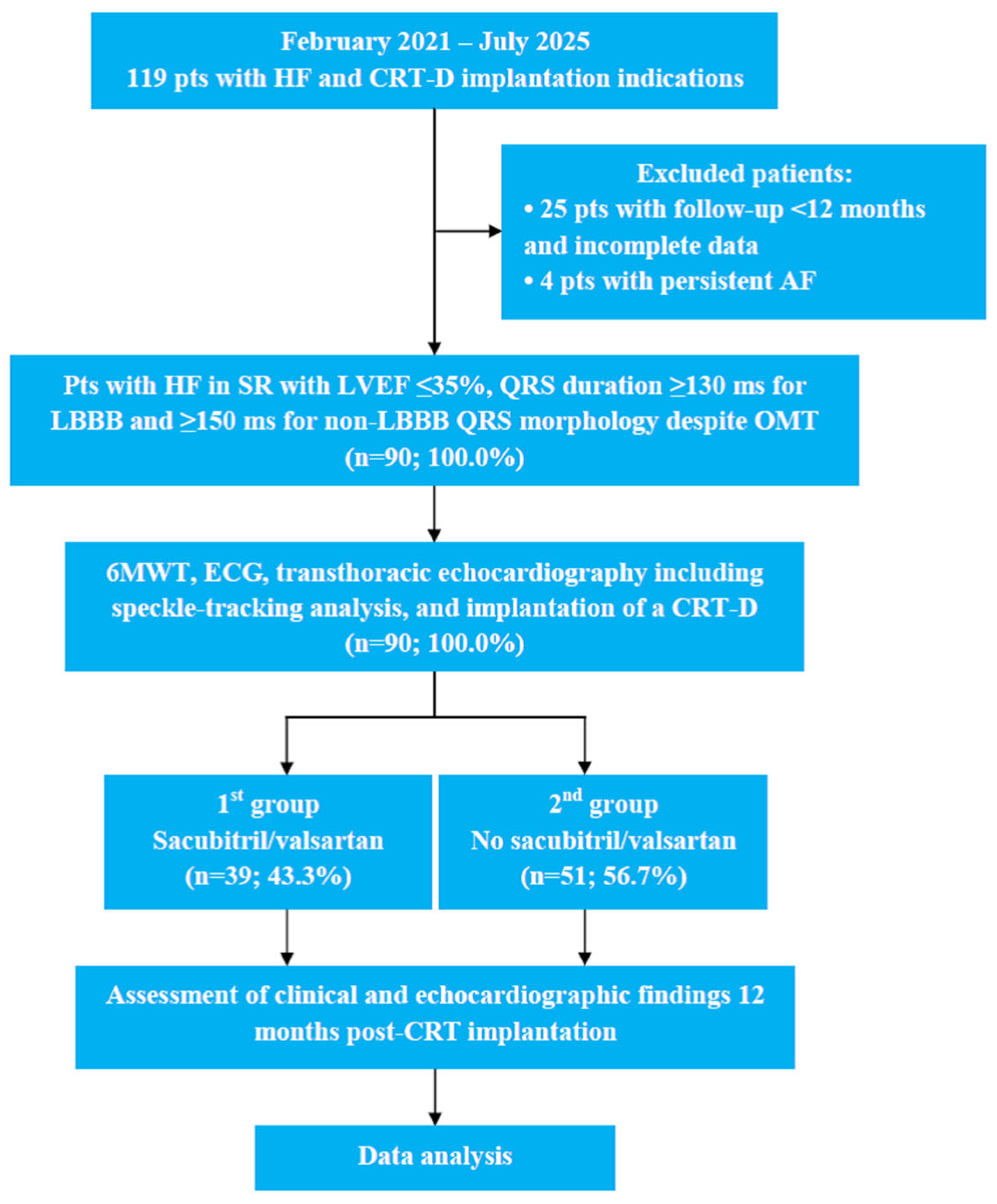
2.1. Study Design and Participants
2.2. Consent
2.3. Data Collection and Methods
2.3.1. Six-Minute Walk Test
- -
- >551 m: NYHA class I (no apparent symptoms);
- -
- 426–550 m: NYHA class II (mild symptoms);
- -
- 301–425 m: NYHA class III (marked symptoms);
- -
- 151–300 m: NYHA class IV (severe symptoms);
- -
- ≤150 m: NYHA class IV.
2.3.2. Electrocardiogram Analysis
2.3.3. Echocardiographic Acquisition and Analysis
2.3.4. Speckle-Tracking Echocardiography
2.3.5. CRT-D Implantation and Programming
2.4. Definition of CRT Response Criteria
2.5. Study Endpoints
2.6. Statistical Analysis
3. Results
3.1. Study Population Characteristics
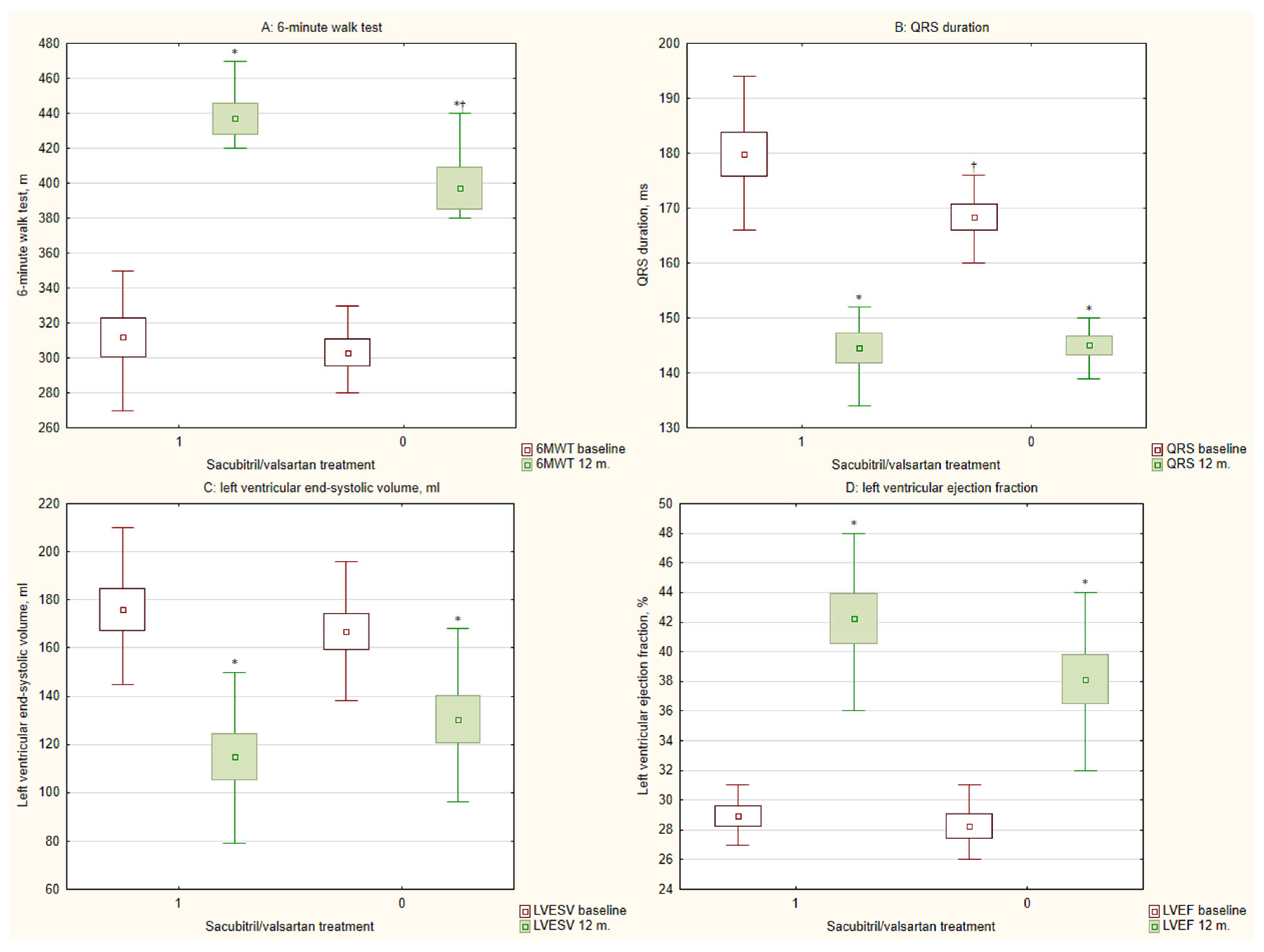
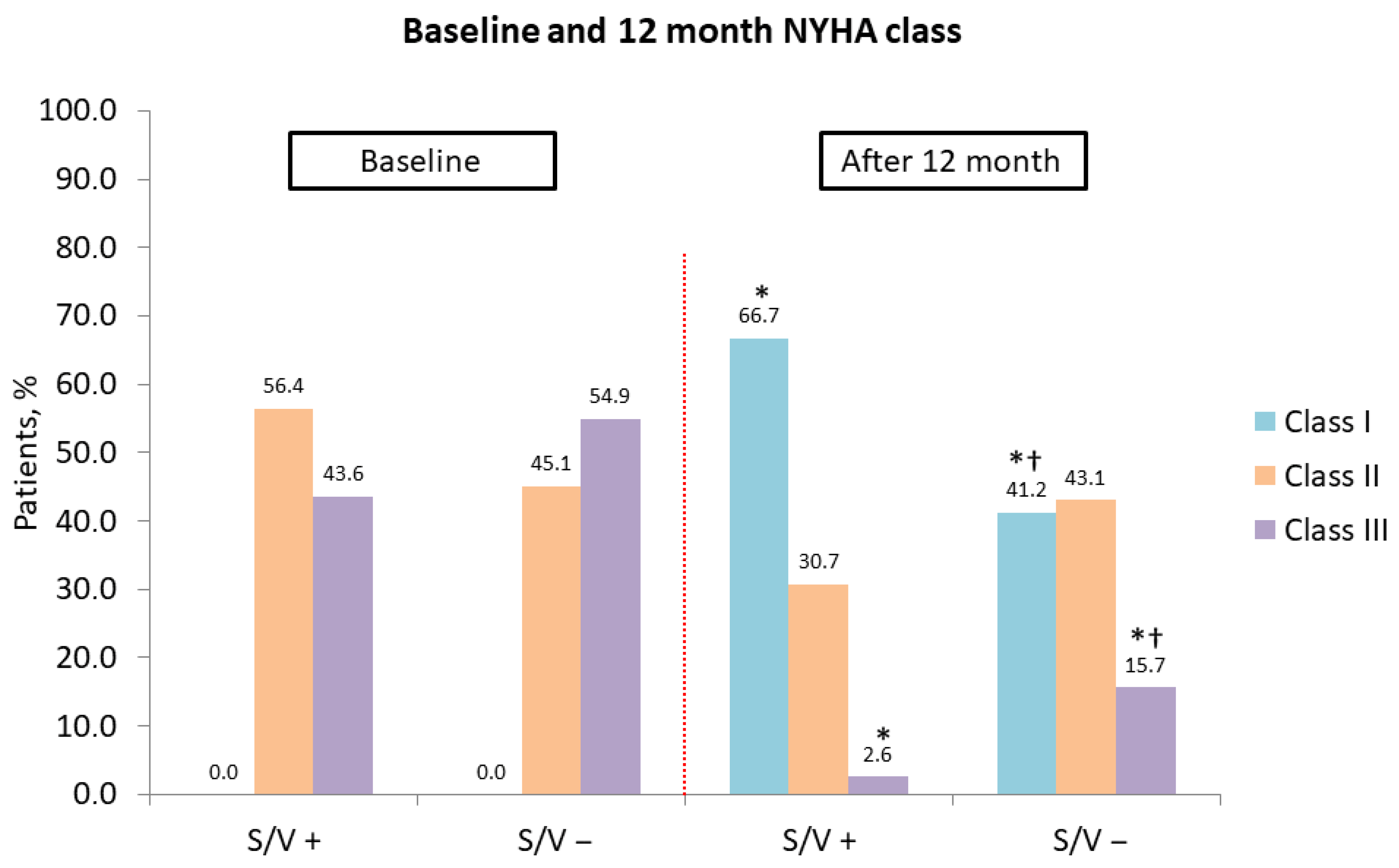
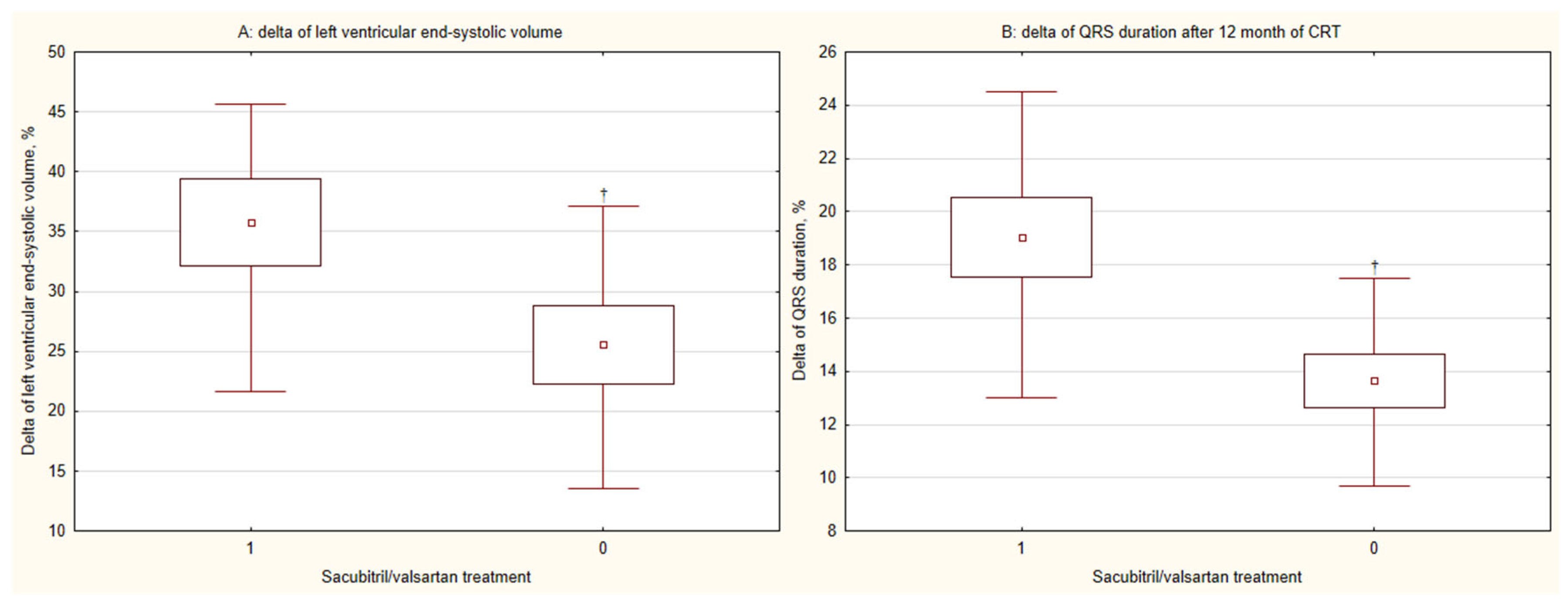
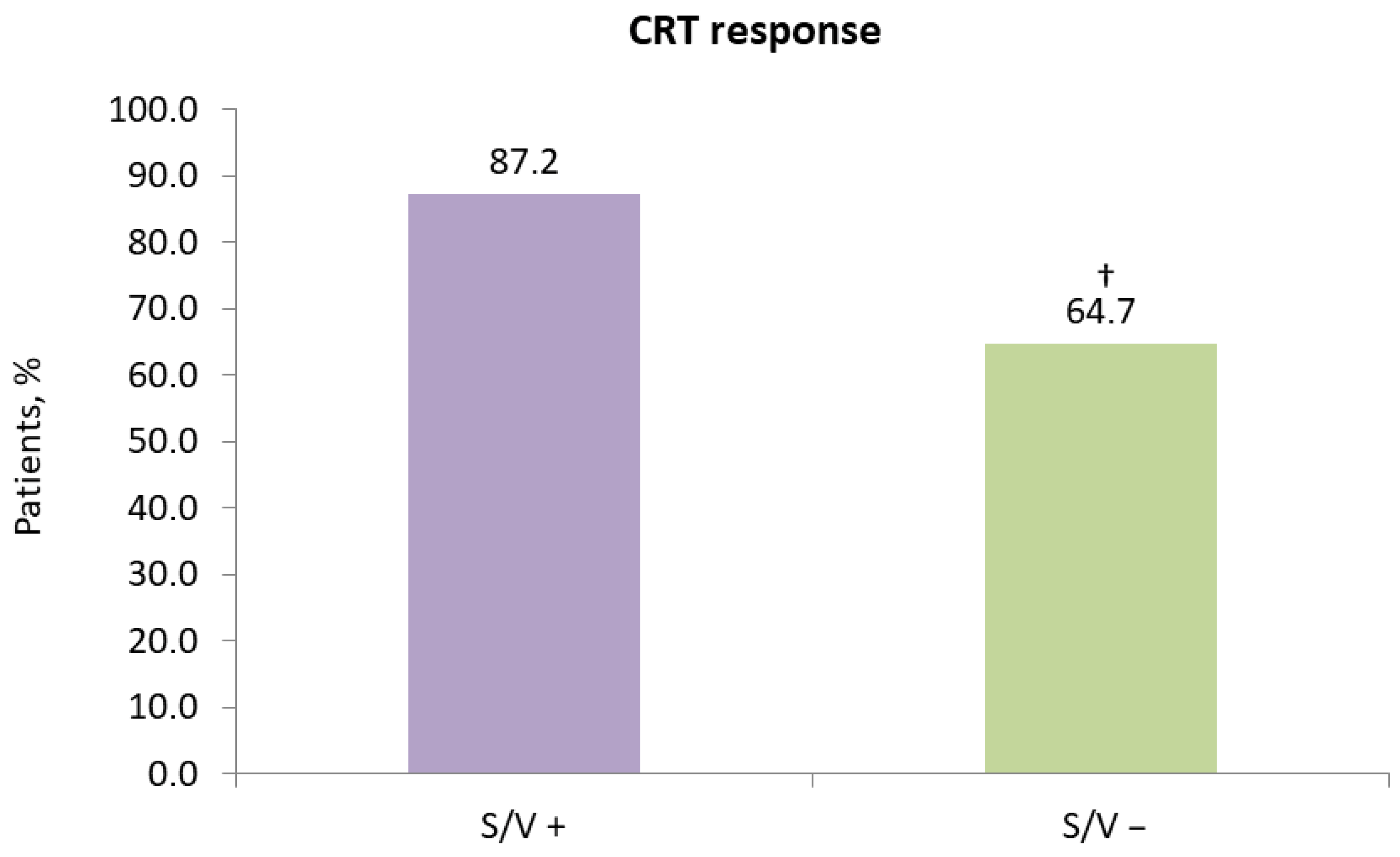
3.2. Clinical and Echocardiographic Outcomes at 12-Month Follow-Up After CRT
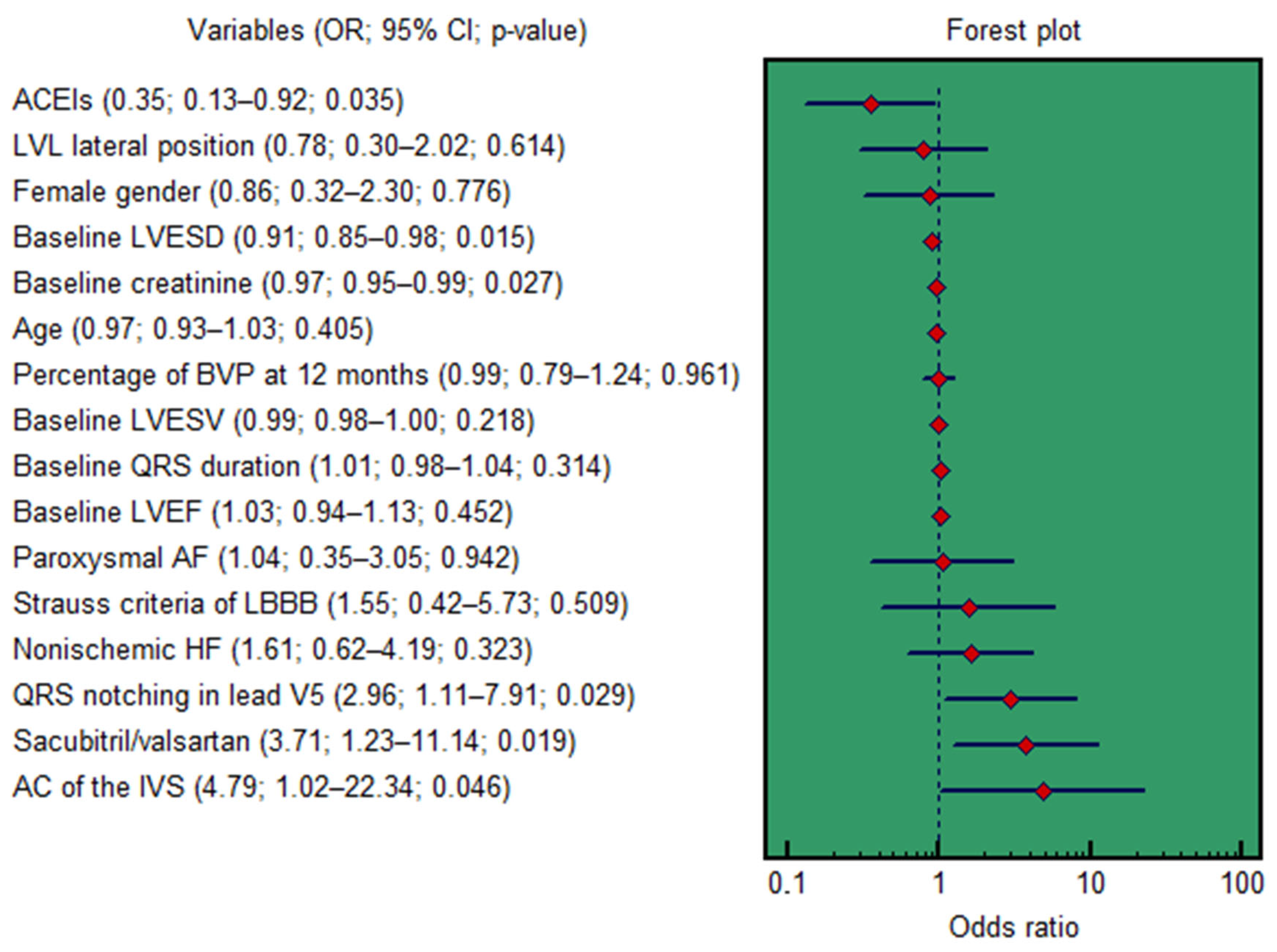
3.3. Risk Stratification Analysis
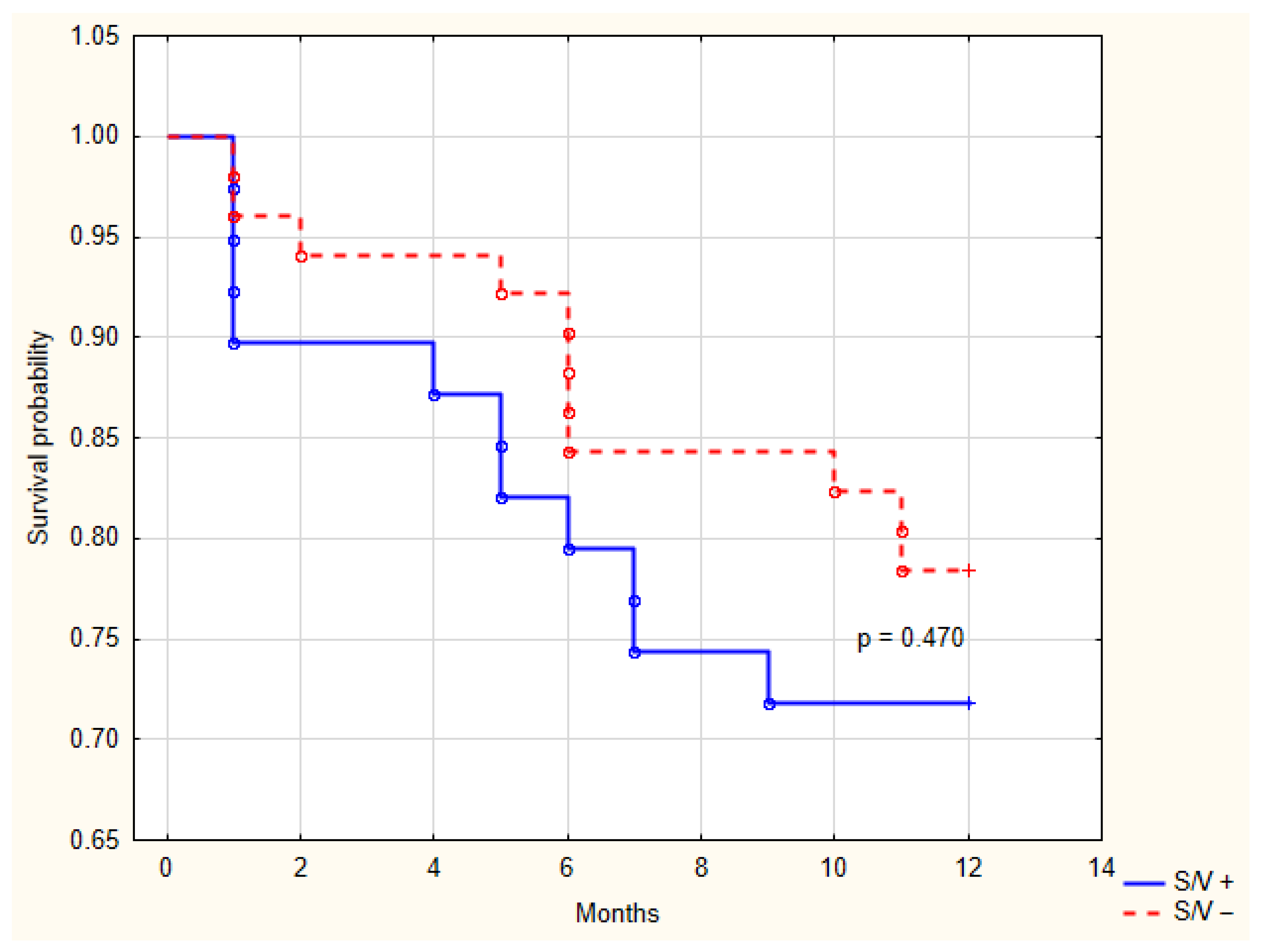
3.4. Overall Survival
4. Discussion
4.1. Clinical Implications
4.2. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 6MWT | 6-Minute Walk Test |
| ACEIs | Angiotensin-Converting Enzyme Inhibitors |
| AF | Atrial Fibrillation |
| ARBs | Angiotensin II Receptor Blockers |
| AUC | Area Under the ROC Curve |
| BP | Biventricular Pacing |
| CI | Confidence Interval |
| CRT | Cardiac Resynchronization Therapy |
| CRT-D | Cardiac Resynchronization Therapy Devices With The Defibrillation Function |
| ECG | Electrocardiography |
| EuroQoL EQ-5D | European Quality Of Life Questionnaire |
| HF | Heart Failure |
| ICD | Implantable Cardiac-Defibrillator |
| LBBB | Left Bundle Branch Block |
| LV | Left Ventricular |
| LVEF | Left Ventricle Ejection Fraction |
| LVESD | Left Ventricle End-Systolic Dimension |
| LVESV | Left Ventricle End-Systolic Volume |
| MLWHFQ | Minnesota Living With Heart Failure Questionnaire |
| NYHA | New York Heart Association |
| OR | Odds Ratio |
| ROC | Receiver Operating Characteristic |
| STE | Speckle-Tracking Echocardiography |
| TTE | Transthoracic Echocardiography |
| VT | Ventricular Tachycardia |
References
- Cleland, J.G.; Daubert, J.C.; Erdmann, E.; Freemantle, N.; Gras, D.; Kappenberger, L.; Tavazzi, L. Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N. Engl. J. Med. 2005, 352, 1539–1549. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.D.; Burns, K.V.; Harbin, M.M.; Espinosa, E.A.; Olson, M.D.; Bank, A.J. Cardiac resynchronization therapy optimization in nonresponders and incomplete responders using electrical dyssynchrony mapping. Heart Rhythm 2022, 19, 1965–1973. [Google Scholar] [CrossRef] [PubMed]
- Kirk, J.A.; Kass, D.A. Cellular and molecular aspects of dyssynchrony and resynchronization. Heart Fail. Clin. 2017, 13, 29–41. [Google Scholar] [CrossRef] [PubMed]
- Nattel, S.; Dobrev, D. Electrophysiological and molecular mechanisms of paroxysmal atrial fibrillation. Nat. Rev. Cardiol. 2016, 13, 575–590. [Google Scholar] [CrossRef]
- Tomaselli, G.F.; Marbán, E. Electrophysiological remodeling in hypertrophy and heart failure. Cardiovasc. Res. 1999, 42, 270–283. [Google Scholar] [CrossRef]
- McMurray, J.J.; Packer, M.; Desai, A.S.; Gong, J.; Lefkowitz, M.P.; Rizkala, A.R.; Rouleau, J.L.; Shi, V.C.; Solomon, S.D.; Swedberg, K.; et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N. Engl. J. Med. 2014, 371, 993–1004. [Google Scholar] [CrossRef]
- Packer, M.; McMurray, J.J.; Desai, A.S.; Gong, J.; Lefkowitz, M.P.; Rizkala, A.R.; Rouleau, J.L.; Shi, V.C.; Solomon, S.D.; Swedberg, K.; et al. Angiotensin receptor neprilysin inhibition compared with enalapril on the risk of clinical progression in surviving patients with heart failure. Circulation 2015, 131, 54–61. [Google Scholar] [CrossRef]
- Mazza, A.; Townsend, D.M.; Torin, G.; Schiavon, L.; Camerotto, A.; Rigatelli, G.; Cuppini, S.; Minuz, P.; Rubello, D. The role of sacubitril/valsartan in the treatment of chronic heart failure with reduced ejection fraction in hypertensive patients with comorbidities: From clinical trials to real-world settings. Biomed. Pharmacother. 2020, 130, 110596. [Google Scholar] [CrossRef]
- Pătru, O.; Luca, S.; Cozma, D.; Văcărescu, C.; Crișan, S.; Valcovici, M.D.; Vîrtosu, M.; Zus, A.S.; Luca, C.T.; Drăgan, S.R. The role of ARNI in enhancing outcomes of cardiac resynchronization therapy: A comprehensive review. J. Clin. Med. 2025, 14, 2743. [Google Scholar] [CrossRef]
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: Executive summary: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022, 145, e876–e894. [Google Scholar] [CrossRef]
- Strauss, D.G.; Selvester, R.H.; Wagner, G.S. Defining left bundle branch block in the era of cardiac resynchronization therapy. Am. J. Cardiol. 2011, 107, 927–934. [Google Scholar] [CrossRef]
- Bogossian, H.; Linz, D.; Heijman, J.; Bimpong-Buta, N.Y.; Bandorski, D.; Frommeyer, G.; Erkapic, D.; Seyfarth, M.; Zarse, M.; Crijns, H.J. QTc evaluation in patients with bundle branch block. Int. J. Cardiol. Heart Vasc. 2020, 30, 100636. [Google Scholar] [CrossRef] [PubMed]
- Alizadeh, A.; Shahrbaf, M.A.; Khorgami, M.; Zeighami, M.; Keikhavani, A.; Mokhtari Torshizi, H.; Teimouri-Jervekani, Z. QTc interval measurement in patients with right bundle branch block: A practical method. Ann. Noninvasive Electrocardiol. 2023, 28, e13047. [Google Scholar] [CrossRef] [PubMed]
- Douglas, P.S.; Carabello, B.A.; Lang, R.M.; Lopez, L.; Pellikka, P.A.; Picard, M.H.; Thomas, J.D.; Varghese, P.; Wang, T.Y.; Weissman, N.J.; et al. 2019 ACC/AHA/ASE key data elements and definitions for transthoracic echocardiography: A report of the American College of Cardiology/American Heart Association task force on clinical data standards (writing committee to develop cardiovascular endpoints data standards) and the American Society of Echocardiography. J. Am. Coll. Cardiol. 2019, 74, 403–469. [Google Scholar] [CrossRef] [PubMed]
- Stiles, M.K.; Fauchier, L.; Morillo, C.A.; Wilkoff, B.L. 2019 HRS/EHRA/APHRS/LAHRS focused update to 2015 expert consensus statement on optimal implantable cardioverter-defibrillator programming and testing. Heart Rhythm 2020, 17, e220–e228. [Google Scholar] [CrossRef]
- Pitzalis, M.V.; Iacoviello, M.; Romito, R.; Guida, P.; De Tommasi, E.; Luzzi, G.; Anaclerio, M.; Forleo, C.; Rizzon, P. Ventricular asynchrony predicts a better outcome in patients with chronic heart failure receiving cardiac resynchronization therapy. J. Am. Coll. Cardiol. 2005, 45, 65–69. [Google Scholar] [CrossRef]
- Pires, L.A.; Abraham, W.T.; Young, J.B.; Johnson, K.M.; MIRACLE and MIRACLE-ICD Investigators. Clinical predictors and timing of New York Heart Association class improvement with cardiac resynchronization therapy in patients with advanced chronic heart failure: Results from the Multicenter InSync Randomized Clinical Evaluation (MIRACLE) and Multicenter InSync ICD Randomized Clinical Evaluation (MIRACLE-ICD) trials. Am. Heart J. 2006, 151, 837–843. [Google Scholar] [CrossRef]
- Januzzi, J.L., Jr.; Prescott, M.F.; Butler, J.; Felker, G.M.; Maisel, A.S.; McCague, K.; Camacho, A.; Piña, I.L.; Rocha, R.A.; Shah, A.M.; et al. Association of Change in N-Terminal Pro-B-Type Natriuretic Peptide Following Initiation of Sacubitril-Valsartan Treatment With Cardiac Structure and Function in Patients With Heart Failure With Reduced Ejection Fraction. JAMA 2019, 322, 1085–1095. [Google Scholar] [CrossRef]
- Abdin, A.; Schulz, M.; Riemer, U.; Hadëri, B.; Wachter, R.; Laufs, U.; Bauersachs, J.; Kindermann, I.; Vukadinović, D.; Böhm, M. Sacubitril/valsartan in heart failure: Efficacy and safety in and outside clinical trials. ESC Heart Fail. 2022, 9, 3737–3750. [Google Scholar] [CrossRef]
- Fonderico, C.; Pergola, V.; Faccenda, D.; Salucci, A.; Comparone, G.; Marrese, A.; Ammirati, G.; Cocchiara, L.; Varriale, A.; Esposito, G.; et al. Impact of sacubitril/valsartan and gliflozins on cardiac resynchronization therapy response in ischemic and non-ischemic heart failure patients. Int. J. Cardiol. 2023, 393, 131391. [Google Scholar] [CrossRef]
- Hsing, J.M.; Selzman, K.A.; Leclercq, C.; Pires, L.A.; McLaughlin, M.G.; McRae, S.E.; Peterson, B.J.; Zimetbaum, P.J. Paced left ventricular QRS width and ECG parameters predict outcomes after cardiac resynchronization therapy: PROSPECT-ECG substudy. Circ. Arrhythm. Electrophysiol. 2011, 4, 851–857. [Google Scholar] [CrossRef] [PubMed]
- Myhre, P.L.; Prescott, M.F.; Murphy, S.P.; Fang, J.C.; Mitchell, G.F.; Ward, J.H.; Claggett, B.; Desai, A.S.; Solomon, S.D.; Januzzi, J.L. Early B-type natriuretic peptide change in HFrEF patients treated with sacubitril/valsartan: A pooled analysis of EVALATE-HF and PROVE-HF. JACC Heart Fail. 2022, 10, 119–128. [Google Scholar] [CrossRef] [PubMed]
- de Diego, C.; González-Torres, L.; Núñez, J.M.; Centurión Inda, R.; Martin-Langerwerf, D.A.; Sangio, A.D.; Chochowski, P.; Casasnovas, P.; Blazquéz, J.C.; Almendral, J. Effects of angiotensin-neprilysin inhibition compared to angiotensin inhibition on ventricular arrhythmias in reduced ejection fraction patients under continuous remote monitoring of implantable defibrillator devices. Heart Rhythm 2018, 15, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Heywood, J.T.; Fonarow, G.C.; Costanzo, M.R.; Mathur, V.S.; Wigneswaran, J.R.; Wynne, J.; ADHERE Scientific Advisory Committee and Investigators. High prevalence of renal dysfunction and its impact on outcome in 118,465 patients hospitalized with acute decompensated heart failure: A report from the ADHERE database. J. Card. Fail. 2007, 13, 422–430. [Google Scholar] [CrossRef]
- Schefold, J.C.; Filippatos, G.; Hasenfuss, G.; Anker, S.D.; von Haehling, S. Heart failure and kidney dysfunction: Epidemiology, mechanisms and management. Nat. Rev. Nephrol. 2016, 12, 610–623. [Google Scholar] [CrossRef]
- Haynes, R.; Zhu, D.; Judge, P.K.; Herrington, W.G.; Kalra, P.A.; Baigent, C. Chronic kidney disease, heart failure and neprilysin inhibition. Nephrol. Dial. Transplant. 2020, 35, 558–564. [Google Scholar] [CrossRef]
- Beltrami, C.A.; Finato, N.; Rocco, M.; Feruglio, G.A.; Puricelli, C.; Cigola, E.; Quaini, F.; Sonnenblick, E.H.; Olivetti, G.; Anversa, P. Structural basis of end-stage failure in ischemic cardiomyopathy in humans. Circulation 1994, 89, 151–163. [Google Scholar] [CrossRef]
- Grossman, W.; Jones, D.; McLaurin, L.P. Wall stress and patterns of hypertrophy in the human left ventricle. J. Clin. Investig. 1975, 56, 56–64. [Google Scholar] [CrossRef]
- Ypenburg, C.; van Bommel, R.J.; Borleffs, C.J.; Bleeker, G.B.; Boersma, E.; Schalij, M.J.; Bax, J.J. Long-term prognosis after cardiac resynchronization therapy is related to the extent of left ventricular reverse remodeling at midterm follow-up. J. Am. Coll. Cardiol. 2009, 53, 483–490. [Google Scholar] [CrossRef]
- Ferreira, J.M.; Ferreira, S.M.; Ferreira, M.J.; Falcão-Pires, I. Circulating Biomarkers of Collagen Metabolism and Prognosis of Heart Failure with Reduced or Mid-Range Ejection Fraction. Curr. Pharm. Des. 2017, 23, 3217–3223. [Google Scholar] [CrossRef]
- Cleland, J.G.F.; Bristow, M.R.; Freemantle, N.; Olshansky, B.; Gras, D.; Saxon, L.; Tavazzi, L.; Boehmer, J.; Ghio, S.; Feldman, A.M.; et al. The effect of cardiac resynchronization without a defibrillator on morbidity and mortality: An individual patient data meta-analysis of COMPANION and CARE-HF. Eur. J. Heart Fail. 2022, 24, 1080–1090. [Google Scholar] [CrossRef]

| Characteristics | Overall (n = 90) | 1st Group S/V + (n = 39) | 2nd Group S/V − (n = 51) | p2–3 |
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| Age, year, M ± SD | 60.1 ± 9.8 | 60.0 ± 9.0 | 60.1 ± 10.4 | 0.596 |
| Male gender, n (%) | 57 (63.3) | 25 (64.1) | 32 (62.7) | 0.895 |
| Ischemic heart failure, n (%) | 29 (32.2) | 15 (38.5) | 14 (27.4) | 0.271 |
| Non-ischemic heart failure, n (%) | 51 (56.7) | 20 (51.3) | 31 (60.8) | 0.370 |
| Mixed etiology of heart failure, n (%) | 10 (11.1) | 4 (10.2) | 6 (11.8) | 0.822 |
| Coronary artery stenting in anamnesis, n (%) | 22 (24.4) | 13 (33.3) | 9 (17.6) | 0.087 |
| Body mass index, kg/m2, M ± SD | 29.1 ± 5.0 | 29.8 ± 4.7 | 28.5 ± 5.3 | 0.098 |
| Estimated GFR, mL/min/1.73 m2, M ± SD | 71.6 ± 18.9 | 72.1 ± 19.8 | 71.2 ± 18.5 | 0.941 |
| Heart failure severity (New York Heart Association functional class): | ||||
| II, n (%) | 45 (50.0) | 22 (56.4) | 23 (45.1) | 0.290 |
| III, n (%) | 45 (50.0) | 17 (43.6) | 28 (54.9) | 0.290 |
| Arrhythmias prior to cardiac resynchronization therapy device implantation | ||||
| Paroxysmal atrial fibrillation, n (%) | 24 (26.7) | 8 (20.5) | 16 (31.4) | 0.251 |
| Sustained ventricular tachycardia, n (%) | 5 (5.6) | 2 (5.1) | 3 (5.9) | 0.877 |
| Ventricular fibrillation, n (%) | 2 (2.2) | 2 (5.1) | 0 (0.0) | 0.103 |
| Paroxysmal SVT, n (%) | 2 (2.2) | 0 (0.0) | 2 (3.9) | 0.213 |
| Comorbidities: | ||||
| Diabetes mellitus, n (%) | 21 (23.3) | 12 (30.7) | 9 (17.6) | 0.147 |
| Dyslipidemia, n (%) | 53 (58.9) | 24 (61.5) | 29 (56.8) | 0.656 |
| Stroke, n (%) | 5 (5.6) | 2 (5.1) | 3 (5.9) | 0.877 |
| Smoking, n (%) | 21 (23.3) | 8 (20.5) | 13 (25.5) | 0.582 |
| Therapy: | ||||
| Beta-blockers, n (%) | 86 (95.6) | 36 (92.3) | 50 (98.0) | 0.193 |
| Loop diuretics, n (%) | 58 (64.4) | 23 (58.9) | 35 (68.6) | 0.345 |
| Mineralocorticoid receptor antagonists, n (%) | 86 (95.6) | 37 (94.8) | 49 (96.1) | 0.784 |
| ACEIs, n (%) | 33 (36.7) | 0 (0.0) | 33 (64.7) | <0.001 |
| Antiplatelet agents, n (%) | 49 (54.4) | 22 (56.4) | 27 (52.9) | 0.744 |
| Statins, n (%) | 72 (80.0) | 32 (82.0) | 40 (78.4) | 0.672 |
| Angiotensin II receptor blockers, n (%) | 18 (20.0) | 0 (0.0) | 18 (35.3) | <0.001 |
| Amiodarone, n (%) | 39 (43.3) | 17 (43.6) | 22 (43.1) | 0.966 |
| Anticoagulants, n (%) | 29 (32.2) | 11 (28.2) | 18 (35.3) | 0.478 |
| Ivabradine, n (%) | 3 (3.3) | 2 (5.1) | 1 (1.9) | 0.409 |
| SGLT2Is, n (%) | 69 (76.7) | 31 (79.5) | 38 (74.5) | 0.582 |
| Characteristics | 1st Group S/V + (n = 39) | 2nd Group S/V − (n = 51) | p1–4 | p2–5 | ||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 12 m. | p | Baseline | 12 m. | p | |||
| 1 | 2 | 3 | 4 | 5 | 6 | |||
| EuroQol EQ-5D, score | 57.3 ± 10.3 | 76.6 ± 9.6 | <0.001 | 58.5 ± 9.5 | 75.1 ± 9.2 | <0.001 | 0.363 | 0.277 |
| MLWHFQ, score | 59.6 ± 17.9 | 24.7 ± 14.8 | <0.001 | 59.4 ± 17.7 | 28.3 ± 18.8 | <0.001 | 0.829 | 0.579 |
| 6MWT, m | 311.8 ± 70.4 | 436.9 ± 53.9 | <0.001 | 303.1 ± 53.9 | 397.1 ± 84.0 | <0.001 | 0.381 | 0.013 |
| QRS, ms | 179.8 ± 24.7 | 144.5 ± 16.8 | <0.001 | 168.0 ± 19.5 | 146.9 ± 16.7 | <0.001 | 0.019 | 0.896 |
| ∆QRS, ms | - | 19.0 ± 9.5 | - | - | 13.6 ± 7.1 | - | - | 0.005 |
| cQTc, ms | 432.4 ± 30.4 | 437.1 ± 30.0 | 0.711 | 417.0 ± 38.1 | 437.8 ± 27.8 | 0.015 | 0.052 | 0.883 |
| AA, ° | −30.0 [−47.0; −5.0] | 85.0 [−42.0; 135.0] | 0.002 | −30.0 [−47.0; 15.0] | −30.0 [−100.0; 90.0] | 0.403 | 0.499 | 0.087 |
| QRSN in V5 | 27 (69.2) | - | - | 33 (64.7) | - | - | 0.653 | - |
| SC of LBBB | 33 (84.6) | - | - | 45 (88.2) | - | - | 0.618 | - |
| SBP, mmHg | 118.5 ± 8.5 | 119.1 ± 5.8 | 0.010 | 119.6 ± 5.5 | 118.5 ± 5.3 | 0.022 | 0.368 | 0.681 |
| DBP, mmHg | 73.8 ± 4.9 | 74.5 ± 3.8 | 0.384 | 75.8 ± 4.2 | 74.8 ± 3.1 | <0.001 | 0.059 | 0.944 |
| Creatinine, µmol/L | 91.9 ± 22.6 | 89.6 ± 24.0 | <0.001 | 95.7 ± 21.7 | 98.2 ± 28.3 | <0.001 | 0.332 | 0.196 |
| LVEDD, mm | 68.1 ± 6.7 | 62.1 ± 9.1 | <0.001 | 67.1 ± 6.6 | 63.2 ± 10.1 | <0.001 | 0.636 | 0.593 |
| LVESD, mm | 58.6 ± 6.7 | 49.5 ± 10.8 | <0.001 | 57.8 ± 7.0 | 51.9 ± 12.4 | <0.001 | 0.560 | 0.338 |
| LVEF, % | 28.9 ± 4.3 | 42.2 ± 10.5 | <0.001 | 28.2 ± 5.6 | 38.1 ± 11.8 | <0.001 | 0.711 | 0.068 |
| ∆LVEF, % | - | 48.4 ± 40.1 | - | - | 37.8 ± 41.2 | - | - | 0.079 |
| LVESV, ml | 175.8 ± 54.6 | 114.9 ± 60.2 | <0.001 | 166.8 ± 53.3 | 130.4 ± 70.1 | <0.001 | 0.385 | 0.311 |
| ∆LVESV, % | - | 35.8 ± 22.4 | - | - | 25.5 ± 23.2 | - | - | 0.025 |
| AC of the IVS | 12 (30.7) | - | - | 11 (21.5) | - | - | 0.324 | - |
| Long strain, % | −8.4 ± 2.4 | −12.1 ± 2.8 | <0.001 | −9.0 ± 2.2 | −12.6 ± 3.0 | <0.001 | 0.234 | 0.397 |
| Left ventricular lead position: | ||||||||
| Lateral | 19 (48.8) | - | - | 22 (43.1) | - | - | 0.600 | - |
| Posterolateral | 13 (33.3) | - | - | 21 (41.2) | - | - | 0.449 | - |
| Anterolateral | 7 (17.9) | - | - | 8 (15.7) | - | - | 0.776 | - |
| BP rate, % | - | 97.9 ± 2.7 | - | - | 98.1 ± 1.6 | - | - | 0.533 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Atabekov, T.; Silivanova, I.; Kisteneva, I.; Krivolapov, S.; Batalov, R.; Popov, S. Impact of Sacubitril/Valsartan on Cardiac Reverse Remodeling in Patients with Heart Failure Undergoing Cardiac Resynchronization Therapy. Diseases 2026, 14, 6. https://doi.org/10.3390/diseases14010006
Atabekov T, Silivanova I, Kisteneva I, Krivolapov S, Batalov R, Popov S. Impact of Sacubitril/Valsartan on Cardiac Reverse Remodeling in Patients with Heart Failure Undergoing Cardiac Resynchronization Therapy. Diseases. 2026; 14(1):6. https://doi.org/10.3390/diseases14010006
Chicago/Turabian StyleAtabekov, Tariel, Irina Silivanova, Irina Kisteneva, Sergey Krivolapov, Roman Batalov, and Sergey Popov. 2026. "Impact of Sacubitril/Valsartan on Cardiac Reverse Remodeling in Patients with Heart Failure Undergoing Cardiac Resynchronization Therapy" Diseases 14, no. 1: 6. https://doi.org/10.3390/diseases14010006
APA StyleAtabekov, T., Silivanova, I., Kisteneva, I., Krivolapov, S., Batalov, R., & Popov, S. (2026). Impact of Sacubitril/Valsartan on Cardiac Reverse Remodeling in Patients with Heart Failure Undergoing Cardiac Resynchronization Therapy. Diseases, 14(1), 6. https://doi.org/10.3390/diseases14010006







