Cancer Screening and Prevention in MENA and Mediterranean Populations: A Multi-Level Analysis of Barriers, Knowledge Gaps, and Interventions Across Indigenous and Diaspora Communities
Abstract
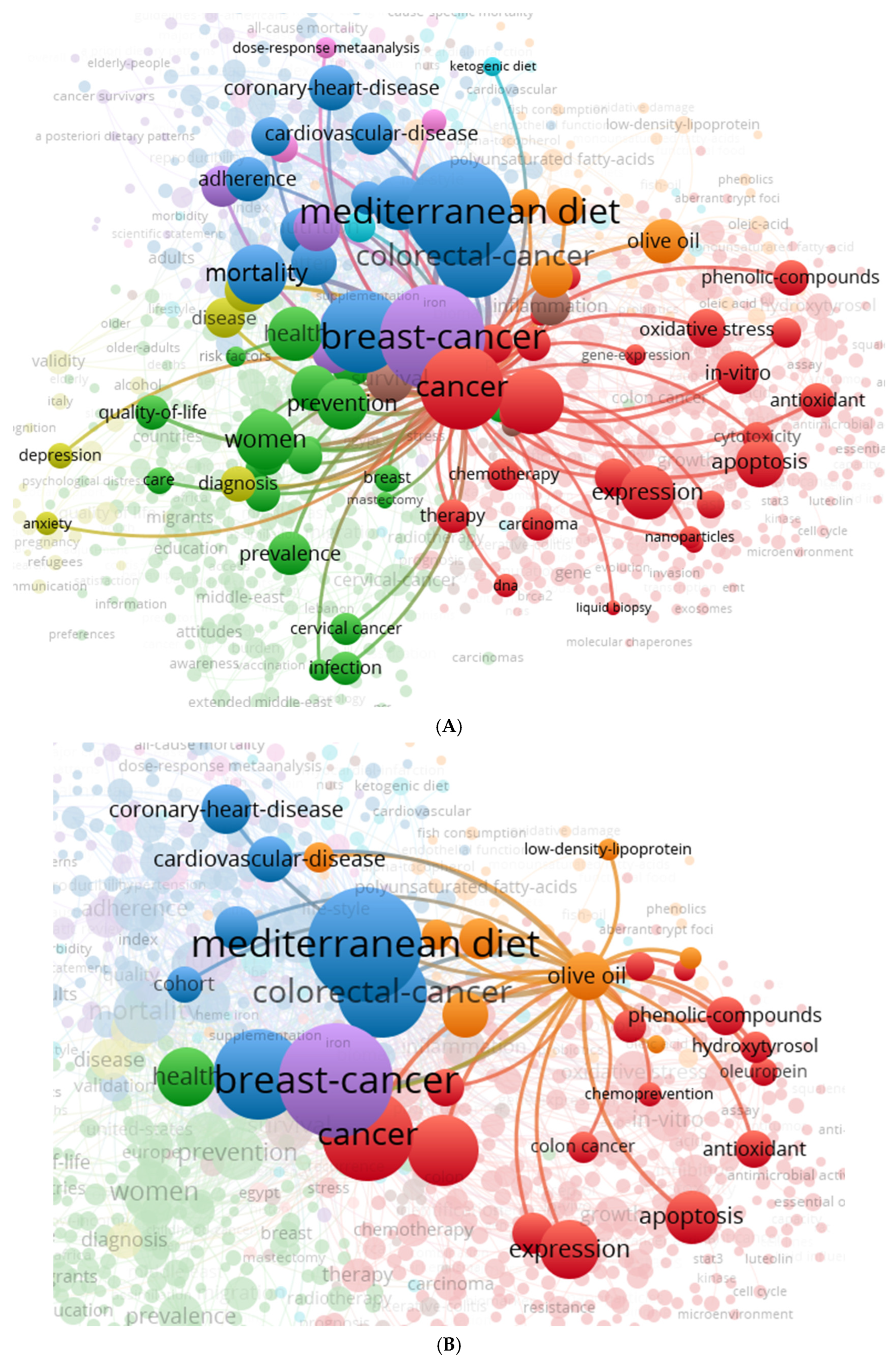
1. Introduction
2. Methods
2.1. Search Strategy and Databases
2.2. Eligibility Criteria
- Study type: peer-reviewed empirical studies (quantitative, qualitative, or mixed-methods);
- Population: women or mixed-gender cohorts from indigenous MENA, Mediterranean Basin residents, or MENA diaspora populations in Europe or North America;
- Outcomes: cancer prevention, screening uptake, awareness, HPV vaccine knowledge, or early detection behaviour for breast, cervical, or colorectal cancer;
- Geographic scope: limited to the Middle East, North Africa, Southern Europe, and Western host countries with significant MENA migrant communities.
- non-peer-reviewed sources (excluding specified grey literature reports),
- studies not addressing screening or early detection,
- studies outside the defined geographic scope,
- papers lacking extractable population-specific data.
2.3. Screening and Selection Process
2.4. Data Collection and Synthesis
- (1)
- cancer type (breast, cervical, colorectal),
- (2)
- behavioural constructs (awareness, uptake, education),
- (3)
- vulnerability factors (migrants, refugees, low-literacy populations),
- (4)
- geography (indigenous vs. diaspora populations).
2.4.1. Literature Search and Selection Criteria
2.4.2. The Importance of Early Detection and Prevention
3. HPV and Cervical Cancer in the MENA Population
Knowledge Gaps, Vaccine Introduction and Cost-Effectiveness Models
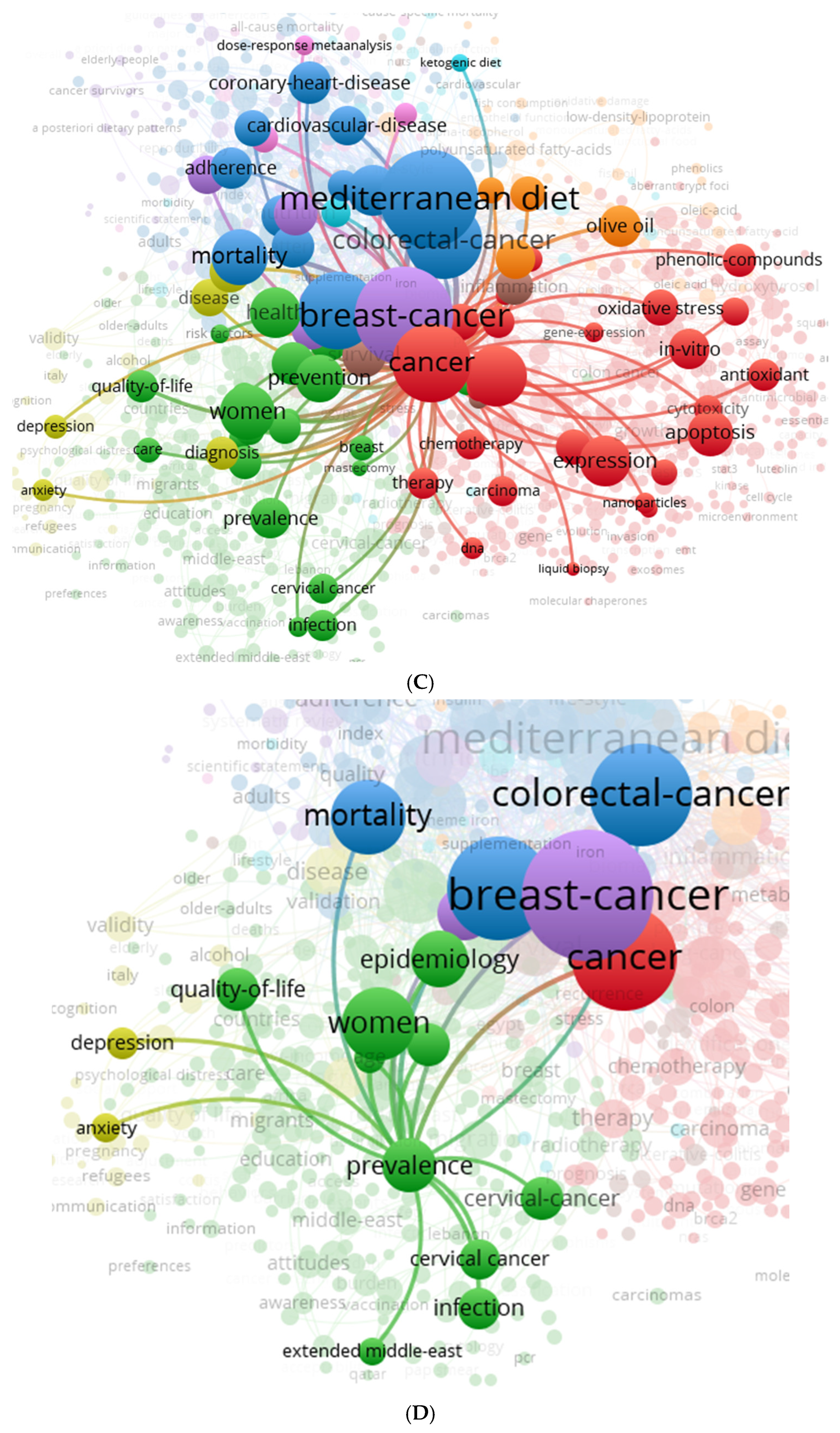
4. Disparities and Indicators in Screening
4.1. Cultural, Socioeconomic, and Systemic Influences
4.1.1. Cultural Elements
4.1.2. Socioeconomic Indicators
4.1.3. Barriers in the System
4.2. Indigenous vs. Diaspora MENA Populations
5. Culturally Adapted Interventions
5.1. Case Studies of Tailored Navigation and Education Programs
5.2. Health Literacy and Culturally Sensitive Education
5.3. Patient Navigation and Language Mediation
5.4. Peer Educator and Community-Led Models
5.5. Integration into Primary Care and Support at System Level
6. Challenges in the Implementation of Health Policy
6.1. Infrastructural and Systemic Gaps
- -
- Trained primary care providers and gynecologists
- -
- Laboratory services for cytology or HPV DNA testing
- -
- Colposcopy and biopsy follow-up services
- -
- Electronic data systems for screening reminders and follow-up
6.2. Access to Healthcare and Equal Opportunities
6.3. Political Instability and Competing Health Priorities
- -
- Integrating screening into routine primary care
- -
- Expanding services in rural areas
- -
- Ensuring long-term funding and policy stability
- -
- Collaborating across sectors to align health, education, and community development
7. Possibilities and Future Directions
7.1. AI-Supported Education, Digital Health Literacy and Policy Recommendations
7.2. AI-Powered Outreach and Risk Stratification
- -
- Identify high-risk individuals using electronic health records or self-reported data with minimal input
- -
- Automate reminder systems tailored to language, literacy or screening history
- -
- Prediction of non-compliance and suggestions for personalized nudges or navigator support
7.3. Digital Health Literacy and Mobile Health Interventions
- -
- SMS-based appointment reminders and health alerts
- -
- Video education via WhatsApp in local dialects
- -
- QR codes that lead to visual explanations of Pap smears or mammograms
- -
- Teleconsultation apps with culturally competent providers
7.4. Suggestions for Policies to Support Fair and Long-Term Growth
- 1)
- Integrate screening for cervical, breast, and colorectal cancer into maternal and child health services.
- -
- Leverage vaccination campaigns (such as HPV) to coordinate with other interventions.
- 2)
- Launch cost-effective national HPV vaccination programs. Use school-based models to reach girls before puberty. Seek support from Gavi or WHO for vaccine procurement and distribution.
- 3)
- Institutionalize community health workers and mediators.
- -
- Train culturally competent navigators to serve in clinics, refugee centers, and community settings.
- -
- Provide certification, fair compensation, and digital tools to expand their reach.
- 4)
- Ensure providers receive training that is both gender-sensitive and culturally sensitive. This will address provider bias and ensure patients are treated with respect and understanding. Incorporate cross-cultural communication skills into medical and nursing education.
- 5)
- Strengthen data systems and evaluation frameworks. Use AI and digital registries to monitor participation, follow-up, and outcomes. Disaggregate reports by gender, location, and migration status.
- 6)
- Promote cross-border collaboration and knowledge sharing by establishing regional consortia (such as the Maghreb-Eastern Med Cancer Screening Network) and facilitating the exchange of best practices, digital tools, and joint procurement agreements.
- 7)
- Ensure sustainable funding mechanisms for cancer screening programs.
- -
- Allocate long-term budget lines in national health plans.
- -
- Explore public–private partnerships and international donor engagement to maintain program continuity, especially in low-income and conflict-affected countries.
8. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zahwe, M.; Bendahhou, K.; Eser, S.; Mukherji, D.; Fouad, H.; Fadhil, I.; Soerjomataram, I.; Znaor, A. Current and future burden of female breast cancer in the Middle East and North Africa region using estimates from GLOBOCAN 2022. Int. J. Cancer 2025, 156, 2320–2329. [Google Scholar] [CrossRef] [PubMed]
- Shukla, A.; Zeidan, R.K.; Saddik, B. Pediatric and adolescent cancer disparities in the Middle East and North Africa (MENA) region: Incidence, mortality, and survival across socioeconomic strata. BMC Public Health 2024, 24, 3602. [Google Scholar] [CrossRef]
- Carlos, R.C.; Dempsey, A.F.; Patel, D.A.; Dalton, V.K. Cervical cancer prevention through human papillomavirus vaccination: Using the “teachable moment” for educational interventions. Obstet. Gynecol. 2010, 115, 834–838. [Google Scholar] [CrossRef]
- Vincent, S.C.; Al Yaquobi, S.; Al Hashmi, A. A Systematic Review of Knowledge, Attitudes, and Factors Influencing HPV Vaccine Acceptance Among Adolescents, Parents, Teachers, and Healthcare Professionals in the Middle East and North Africa (MENA) Region. Cureus 2024, 16, e60293. [Google Scholar] [CrossRef]
- Shamseddine, A.; Chehade, L.; Al Mahmasani, L.; Charafeddine, M. Colorectal Cancer Screening in the Middle East: What, Why, Who, When, and How? Am. Soc. Clin. Oncol. Educ. Book 2023, 43, e390520. [Google Scholar] [CrossRef]
- Balata, G.F.; Azzam, H.N. Synopsis of colorectal cancer: Prevalence, symptoms, screening, staging, risk factors, and treatment. Egypt. J. Intern. Med. 2025, 37, 4. [Google Scholar] [CrossRef]
- Pace, L.E.; Shulman, L.N. Breast Cancer in Sub-Saharan Africa: Challenges and Opportunities to Reduce Mortality. Oncologist 2016, 21, 739–744. [Google Scholar] [CrossRef] [PubMed]
- Gorina, Y.; Elgaddal, N. Patterns of Mammography, Pap Smear, and Colorectal Cancer Screening Services Among Women Aged 45 and Over. Natl. Health Stat. Rep. 2021, 157, 1–18. [Google Scholar] [PubMed]
- Chiumento, A.; Hosny, W.; Gaber, E.; Emadeldin, M.; El Barabry, W.; Hamoda, H.M.; Alonge, O. Exploring the acceptability of a WHO school-based mental health program in Egypt: A qualitative study. SSM-Ment. Health 2022, 2, 100075. [Google Scholar] [CrossRef]
- Adigüzel, F.I.; Adigüzel, C.; Seyfettinoglu, S.; Hürriyetoglu, S.; Kazgan, H.; Yilmaz, E.S.S.; Yücel, O.; Baser, E. HPV awareness and HPV vaccine acceptance among women who apply to the gynecology outpatient clinics at a tertiary referral hospital in the south Mediterranean region of Turkey. Med. J. Bakirkoy 2016, 12, 136–139. [Google Scholar] [CrossRef]
- Cervantes-Amat, M.; López-Abente, G.; Aragonés, N.; Pollán, M.; Pastor-Barriuso, R.; Pérez-Gómez, B. The end of the decline in cervical cancer mortality in Spain: Trends across the period 1981–2012. BMC Cancer 2015, 15, 287. [Google Scholar] [CrossRef]
- Mansori, K.; Khazaei, S.; Khosravi Shadmani, F.; Hanis, S.M.; Jenabi, E.; Soheylizad, M.; Sani, M.; Ayubi, E. Global Inequalities in Cervical Cancer Incidence and Mortality. Middle East J. Cancer 2018, 9, 235–242. [Google Scholar]
- Zhang, X.X.; Zeng, Q.L.; Cai, W.W.; Ruan, W.Q. Trends of cervical cancer at global, regional, and national level: Data from the Global Burden of Disease study 2019. BMC Public Health 2021, 21, 894. [Google Scholar] [CrossRef] [PubMed]
- Caron, R.M.; Noel, K.; Reed, R.N.; Sibel, J.; Smith, H.J. Health Promotion, Health Protection, and Disease Prevention: Challenges and Opportunities in a Dynamic Landscape. AJPM Focus 2024, 3, 100167. [Google Scholar] [CrossRef]
- Al-Awadhi, R.; Chehadeh, W.; Jaragh, M.; Al-Shaheen, A.; Sharma, P.; Kapila, K. Distribution of human papillomavirus among women with abnormal cervical cytology in Kuwait. Diagn. Cytopathol. 2013, 41, 107–114. [Google Scholar] [CrossRef]
- Baddal, B.; Oktay, M.N.; Bostanci, A.; Yenen, M.C. Prevalence and genotype screening of human papillomavirus among women attending a private hospital in Northern Cyprus: An 11-year retrospective study. BMC Womens Health 2023, 23, 297. [Google Scholar] [CrossRef]
- Dom-Chima, N.; Ajang, Y.A.; Dom-Chima, C.I.; Biswas-Fiss, E.; Aminu, M.; Biswas, S.B. Human papillomavirus spectrum of HPV-infected women in Nigeria: An analysis by next-generation sequencing and type-specific PCR. Virol. J. 2023, 20, 144. [Google Scholar] [CrossRef] [PubMed]
- Bencherit, D.; Kidar, R.; Otmani, S.; Sallam, M.; Samara, K.; Barqawi, H.J.; Lounis, M. Knowledge and Awareness of Algerian Students about Cervical Cancer, HPV and HPV Vaccines: A Cross-Sectional Study. Vaccines 2022, 10, 1420. [Google Scholar] [CrossRef]
- Elmi, A.A.; Bansal, D.; Acharya, A.; Skariah, S.; Dargham, S.R.; Abu-Raddad, L.J.; Mohamed-Nady, N.; Amuna, P.; Al-Thani, A.A.J.; Sultan, A.A. Human Papillomavirus (HPV) Infection: Molecular Epidemiology, Genotyping, Seroprevalence and Associated Risk Factors among Arab Women in Qatar. PLoS ONE 2017, 12, e0169197. [Google Scholar] [CrossRef]
- Ayash, C.; Raad, N.; Finik, J.; Attia, N.; Nourredine, S.; Aragones, A.; Gany, F. Arab American Mothers’ HPV Vaccination Knowledge and Beliefs. J. Community Health 2022, 47, 716–725. [Google Scholar] [CrossRef]
- Finan, R.R.; Chemaitelly, H.; Racoubian, E.; Aimagambetova, G.; Almawi, W.Y. Genetic diversity of human papillomavirus (HPV) as specified by the detection method, gender, and year of sampling: A retrospective cross-sectional study. Arch. Gynecol. Obstet. 2023, 307, 1469–1479. [Google Scholar] [CrossRef]
- Drolet, M.; Laprise, J.-F.; Boily, M.-C.; Franco, E.; Brisson, M. Potential cost-effectiveness of the nonavalent human papillomavirus (HPV) vaccine. J. Int. Cancer 2014, 134, 2264–2268. [Google Scholar] [CrossRef]
- Sanders, G.D.; Taira, A.V. Cost-effectiveness of a potential vaccine for human papillomavirus. Emerg. Infect. Dis. 2003, 9, 37–48. [Google Scholar] [CrossRef]
- Gobbo, E.L.S.; Hanson, C.; Abunnaja, K.S.S.; van Wees, S.H. Do peer-based education interventions effectively improve vaccination acceptance? a systematic review. BMC Public Health 2023, 23, 1354. [Google Scholar] [CrossRef]
- Martínez, A.C.; Balbino, J.E.; Lemgruber, A.; Ruiz, E.M.; Lima, A.O.D.; Mochón, L.G.; Lessa, F. Adoption of the HPV vaccine: A case study of three emerging countries. J. Comp. Eff. Res. 2017, 6, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Bennacef, A.C.; Khodja, A.A.; Abou-Bekr, F.A.; Ndao, T.; Holl, R.; Bencina, G. Costs and Resource Use Among Patients with Cervical Cancer, Cervical Intraepithelial Neoplasia, and Genital Warts in Algeria. J. Health Econ. Outcomes Res. 2022, 9, 31–38. [Google Scholar] [CrossRef]
- Bencina, G.; Ugrekhelidze, D.; Shoel, H.; Oliver, E.; Meiwald, A.; Hughes, R.; Eiden, A.; Weston, G. The indirect costs of vaccine-preventable cancer mortality in the Middle East and North Africa (MENA). J. Med. Econ. 2024, 27, 1036–1045. [Google Scholar] [CrossRef] [PubMed]
- Cheema, S.; Abraham, A.; Maisonneuve, P.; Jithesh, A.; Chaabna, K.; al Janahi, R.; Sarker, S.; Hussain, A.; Rao, S.; Lowenfels, A.B.; et al. HPV infection and vaccination: A cross-sectional study of knowledge, perception, and attitude to vaccine uptake among university students in Qatar. BMC Public Health 2024, 24, 2316. [Google Scholar] [CrossRef]
- Mahmoud, I.; Al Eid, M.M.A.; Mohamed, M.A.; Aladwani, A.J.; El Amin, N. Human papillomavirus vaccination and Pap test uptake, awareness, and barriers among young adults in Gulf Cooperation Council countries: A comparative cross-sectional survey. J. Infect. Public Health 2024, 17, 102525. [Google Scholar] [CrossRef] [PubMed]
- Pierz, A.J.; Randall, T.C.; Castle, P.E.; Adedimeji, A.; Ingabire, C.; Kubwimana, G.; Uwinkindi, F.; Hagenimana, M.; Businge, L.; Musabyimana, F.; et al. A scoping review: Facilitators and barriers of cervical cancer screening and early diagnosis of breast cancer in Sub-Saharan African health settings. Gynecol. Oncol. Rep. 2020, 33, 100605. [Google Scholar] [CrossRef]
- Afsah, Y.R.; Kaneko, N. Barriers to cervical cancer screening faced by immigrant Muslim women: A systematic scoping review. BMC Public Health 2023, 23, 2375. [Google Scholar] [CrossRef]
- Kim, J.J.; Sharma, M.; O’Shea, M.; Sweet, S.; Diaz, M.; Sancho-Garnier, H.; Seoud, M. Model-Based Impact and Cost-Effectiveness of Cervical Cancer Prevention in the Extended Middle East and North Africa (EMENA). Vaccine 2013, 31, G65–G77. [Google Scholar] [CrossRef]
- Bhattacharjee, N.V.; Schumacher, A.E.; Aali, A.; Abate, Y.H.; Abbasgholizadeh, R.; Abbasian, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd ElHafeez, S.; Abd-Elsalam, S.; et al. Global fertility in 204 countries and territories, 1950–2021, with forecasts to 2100: A comprehensive demographic analysis for the Global Burden of Disease Study 2021. Lancet 2024, 403, 2057–2099. [Google Scholar] [CrossRef]
- Makhlouf, S.M.; Ahmed, S.; Mulvey, M.; Bennett, M.I. Attitudes, Knowledge, and Perceived Barriers Towards Cancer Pain Management Among Healthcare Professionals in Libya: A National Multicenter Survey. J. Cancer Educ. 2023, 38, 789–797. [Google Scholar] [CrossRef]
- Soled, D. Language and Cultural Discordance: Barriers to Improved Patient Care and Understanding. J. Patient Exp. 2020, 7, 830–832. [Google Scholar] [CrossRef] [PubMed]
- Balamou, C.; Rodrigue-Moulinie, C.; Rahmani, S.; de Jesus, M. Optimizing cancer screening rates in populations with low literacy in France: Results of a mixed-methods cancer educational intervention study. Cancer Res. Stat. Treat. 2023, 6, 365–375. [Google Scholar] [CrossRef]
- de Jesus, M.; Rodrigue, C.; Rahmani, S.; Balamou, C. Addressing Cancer Screening Inequities by Promoting Cancer Prevention Knowledge, Awareness, Self-Efficacy, and Screening Uptake Among Low-Income and Illiterate Immigrant Women in France. Int. J. Public Health 2021, 66, 1604055. [Google Scholar] [CrossRef] [PubMed]
- Silva, J.; Gama, A.; Fronteira, I.; Marques, P.; Dias, S. Knowledge and attitudes towards cervical cancer and screening among migrant women: A qualitative study in Portugal. BMJ Open 2024, 14, e082538. [Google Scholar] [CrossRef]
- Hamdiui, N.; Stein, M.L.; van Steenbergen, J.; Crutzen, R.; Bouman, M.; Khan, A.; Çetin, M.N.; Timen, A.; van den Muijsenbergh, M. Evaluation of a Web-Based Culturally Sensitive Educational Video to Facilitate Informed Cervical Cancer Screening Decisions Among Turkish- and Moroccan-Dutch Women Aged 30 to 60 Years: Randomized Intervention Study. J. Med. Internet Res. 2022, 24, e35962. [Google Scholar] [CrossRef]
- Comparetto, C.; Epifani, C.; Manca, M.C.; Lachheb, A.; Bravi, S.; Cipriani, F.; Bellomo, F.; Olivieri, S.; Fiaschi, C.; Marco, L.; et al. Uptake of cervical cancer screening among the migrant population of Prato Province, Italy. Int. J. Gynaecol. Obstet. 2016, 136, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Travier, N.; Vidal, C.; Garcia, M.; Benito, L.; Medina, P.; Moreno, V. Communication Channels Used by Women to Contact a Population-Based Breast Cancer Screening Program in Catalonia, Spain. J. Med. Syst. 2019, 43, 244. [Google Scholar] [CrossRef]
- Ricardo-Rodrigues, I.; Jiménez-García, R.; Hernández-Barrera, V.; Carrasco-Garrido, P.; Jiménez-Trujillo, I.; López de Andrés, A. Social disparities in access to breast and cervical cancer screening by women living in Spain. Public Health 2015, 129, 881–888. [Google Scholar] [CrossRef]
- Piana, A.; Sotgiu, G.; Castiglia, P.; Pischedda, S.; Cocuzza, C.; Capobianco, G.; Marras, V.; Dessole, S.; Muresu, E. Prevalence and type distribution of human papillomavirus infection in women from North Sardinia, Italy. BMC Public Health 2011, 11, 785. [Google Scholar] [CrossRef]
- Sande, C.M.; Yang, G.; Mohamed, A.; Legendre, B.L.; Pion, D.; Ferro, S.L.; Grimm, K.; Elenitoba-Johnson, K.S.J. High-resolution melting assay for rapid, simultaneous detection of JAK2, MPL and CALR variants. J. Clin. Pathol. 2024, 77, 639–644. [Google Scholar] [CrossRef]
- Durand, M.A.; Lamouroux, A.; Redmond, N.M.; Rotily, M.; Bourmaud, A.; Schott, A.M.; Auger-Aubin, I.; Frachon, A.; Exbrayat, C.; Balamou, C.; et al. Impact of a health literacy intervention combining general practitioner training and a consumer facing intervention to improve colorectal cancer screening in underserved areas: Protocol for a multicentric cluster randomized controlled trial. BMC Public Health 2021, 21, 1684. [Google Scholar] [CrossRef] [PubMed]
- Kale, S.; Hirani, S.; Vardhan, S.; Mishra, A.; Ghode, D.B.; Prasad, R.; Wanjari, M. Addressing Cancer Disparities Through Community Engagement: Lessons and Best Practices. Cureus 2023, 15, e43445. [Google Scholar] [CrossRef] [PubMed]
- Priaulx, J.; Turnbull, E.; Heijnsdijk, E.; Csanadi, M.; Senore, C.; Koning, H.; McKee, M. The influence of health systems on breast, cervical and colorectal cancer screening: An overview of systematic reviews using health systems and implementation research frameworks. J. Health Serv. Res. Policy 2019, 25, 135581961984231. [Google Scholar] [CrossRef]
- Basha, L.; Ahmed, H.; Hamze, M.; Ali, A.A.; Alahdab, F.; Marzouk, M.; Sullivan, R.; Abbara, A. Cancer and Syria in conflict: A systematic review. BMC Cancer 2024, 24, 1537. [Google Scholar] [CrossRef]
- Abdelaziz, M.N.; Hefnawy, A.; Azzam, H.; Reisha, O.; Hamdy, O. Knowledge and attitude among Egyptian medical students regarding the role of human papillomavirus vaccine in prevention of oropharyngeal cancer: A questionnaire-based observational study. Sci. Rep. 2025, 15, 3767. [Google Scholar] [CrossRef]
- Jaafar, I.; Atallah, D.; Mirza, F.; Abu Musa, A.; El-Kak, F.; Seoud, M. Determinants of Human Papillomavirus Vaccine recommendation among Middle Eastern and Lebanese Healthcare Providers. Clin. Epidemiol. Glob. Health 2022, 17, 101092. [Google Scholar] [CrossRef]
- Tun, H.M.; Rahman, H.A.; Naing, L.; Malik, O.A. Artificial intelligence utilization in cancer screening program across ASEAN: A scoping review. BMC Cancer 2025, 25, 703. [Google Scholar] [CrossRef] [PubMed]
- Eisemann, N.; Bunk, S.; Mukama, T.; Baltus, H.; Elsner, S.A.; Gomille, T.; Hecht, G.; Heywang-Köbrunner, S.; Rathmann, R.; Siegmann-Luz, K.; et al. Nationwide real-world implementation of AI for cancer detection in population-based mammography screening. Nat. Med. 2025, 31, 917–924. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.R.; Egemen, D.; Befano, B.; Rodriguez, A.C.; Jeronimo, J.; Desai, K.; Teran, C.; Alfaro, K.; Fokom-Domgue, J.; Charoenkwan, K.; et al. Assessing generalizability of an AI-based visual test for cervical cancer screening. PLoS Digit. Health 2024, 3, e0000364. [Google Scholar] [CrossRef]
- Adapa, K.; Gupta, A.; Singh, S.; Kaur, H.; Trikha, A.; Sharma, A.; Rahul, K. A real world evaluation of an innovative artificial intelligence tool for population-level breast cancer screening. npj Digit. Med. 2025, 8, 2. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Gozum, S.; Nimri, O.F.; Merzah, M.A.; Vitorino, R. Cancer Screening and Prevention in MENA and Mediterranean Populations: A Multi-Level Analysis of Barriers, Knowledge Gaps, and Interventions Across Indigenous and Diaspora Communities. Diseases 2026, 14, 10. https://doi.org/10.3390/diseases14010010
Gozum S, Nimri OF, Merzah MA, Vitorino R. Cancer Screening and Prevention in MENA and Mediterranean Populations: A Multi-Level Analysis of Barriers, Knowledge Gaps, and Interventions Across Indigenous and Diaspora Communities. Diseases. 2026; 14(1):10. https://doi.org/10.3390/diseases14010010
Chicago/Turabian StyleGozum, Sebahat, Omar F. Nimri, Mohammed Abdulridha Merzah, and Rui Vitorino. 2026. "Cancer Screening and Prevention in MENA and Mediterranean Populations: A Multi-Level Analysis of Barriers, Knowledge Gaps, and Interventions Across Indigenous and Diaspora Communities" Diseases 14, no. 1: 10. https://doi.org/10.3390/diseases14010010
APA StyleGozum, S., Nimri, O. F., Merzah, M. A., & Vitorino, R. (2026). Cancer Screening and Prevention in MENA and Mediterranean Populations: A Multi-Level Analysis of Barriers, Knowledge Gaps, and Interventions Across Indigenous and Diaspora Communities. Diseases, 14(1), 10. https://doi.org/10.3390/diseases14010010







