Abstract
(1) Background: Exposure to blood carries the risk of transmission of many infectious diseases. Healthcare workers (HCWs), including hospital-based medical students, face high and often under-reported rates of exposure to needlestick and sharps injuries. Previous studies have shown that students’ knowledge of infection control varies, highlighting the importance of pre-placement training. This study aims to assess knowledge, attitudes and practices regarding these risks in a population of medical students from Albania. (2) Methods: A validated questionnaire was administered to 134 medical students in an Italian hospital in May 2023. It assessed HBV vaccination status, adherence to infection control practices, knowledge of pathogen transmission, exposure incidents and attitudes towards infected patients. Three additional questions addressed air-borne transmission of tuberculosis and vaccination recommendations for healthcare workers. (3) Results: Most students (64%) reported being aware of occupational exposure risks. While 93% and 87%, respectively, recognised HIV and HBV as blood-borne pathogens, fewer recognised Treponema pallidum (44%). Awareness of post-exposure prophylaxis for HIV was high (85%), but although 75% reported having received training, only 45% felt it was adequate. Statistical analysis revealed an association between knowledge of infection control, awareness of pathogen transmission and understanding of the importance of vaccination. (4) Conclusions: Our study highlights gaps in medical students’ knowledge of occupational infections and highlights the need for improved pre-clerkship education. Improved education could reduce anxiety, ethical issues and misconceptions and promote safer healthcare practices.
1. Introduction
Exposure to infected blood carries the risk of transmission of blood-borne pathogens, including human immunodeficiency virus (HIV), hepatitis B virus (HBV), hepatitis C virus (HCV) and Treponema pallidum (TP) [1]. Healthcare workers (HCWs) may experience occupational blood exposures when they encounter a needlestick or sustain a percutaneous injury due to a contaminated sharp instrument. Awareness is crucial as exposure to these substances can lead to the contraction and spread of these serious infections [2,3].
The prevalence of HBV is estimated to be around 0.9% and that of HCV is about 1.1% in the European Union, with an estimated total of 4.7 million chronic HBV cases and 5.6 million HCV cases [4]. In 2022, 110,486 HIV diagnoses were reported in Europe, corresponding to 12.4 HIV diagnoses per 100,000 inhabitants for the region as a whole, a slight increase compared with the rate in 2021 (11.9 per 100,000 inhabitants) [5].
Regarding the situation in Albania, despite decreasing HBsAg prevalence estimates, the country remains highly endemic for HBV, with an HBsAg prevalence rate of over 8% [6]. However, recent data on HBV prevalence are limited. The prevalence of HCV infection in the general population is around 1% [7]. Albania is considered a low-prevalence country for HIV, with an estimated rate of 0.04% in the general population [8]. The incidence of tuberculosis has improved over the years, decreasing from 22 cases per 100,000 people in 2000 to 15 cases per 100,000 in 2023 [9]. Despite the Ministry of Health’s approval of a National Measles Elimination Plan in 2000 and minimal cases reported over the past two decades [10], measles resurfaced in 2018–2019 with hospitalisations with different clinical manifestations, highlighting its status as a re-emerging infectious disease in the country [11].
Hospital placements are an obvious risk for medical students. The incidence of accidents due to blood exposure among hospital medical students is high and probably underestimated by official statistics due to the low declaration rate [12,13,14]. It is crucial that medical students are fully aware of the risks associated with their placement.
Needlestick injuries (NSIs) are a major occupational hazard for healthcare workers (HCWs) worldwide, including in Central and Eastern Europe. A systematic review and meta-analysis estimated that 44.5% of HCWs worldwide experience at least one NSI per year [15]. Data on NSIs in Albania are limited. In Bosnia and Herzegovina, a hospital-based study found that 63.3% of HCWs reported exposure to blood and body fluids during their working life, with NSIs (66.1%) being the most common cause, followed by skin contact (12.1%) and cuts from sharp objects (11.3%) [16]. In Turkey, a study of nursing students found that needles caused 54.0% of injuries, mainly during intravenous or intramuscular injections (60.0%). Notably, 31.7% of students did not wear gloves when injured and 68.3% of NSIs were not reported [17].
Although glove use reduces the risk of sharps injuries, compliance among HCWs is variable and influenced by risk perception and workplace culture [18]. In agreement with other European studies, our results highlight that safety-engineered devices significantly reduce the risk of percutaneous exposure among HCWs [19].
Several studies have explored the knowledge, attitudes and practices of health profession students, reporting conflicting results. In some cases, students seem to have important knowledge about infection control [20], while in others they seem not to be fully aware of the risks posed by the work experience and post-exposure measures [21,22], and some studies have reported a low level of needlestick practice [23]. Other studies have shown that healthcare students are aware of the risks of unintentional exposure to HBV [24], although good pre-placement training on the subject is undoubtedly crucial [25]. On the basis of these data, we felt it was essential to investigate the level of knowledge, attitudes and practices regarding exposure to blood-borne and air-borne pathogens in a population of medical students prior to the beginning of their internship at our hospital; in particular, our intention was to assess these aspects in a population of students from the Balkan region.
We conducted this study to investigate medical students’ knowledge of pathogen transmission, prevention and the management of occupational exposure. We also investigated the frequency and details of medical students’ occupational exposure and assessed medical students’ attitudes towards the impact of pathogen risk on future careers and their attitudes towards infected patients.
2. Materials and Methods
The survey was conducted in an Italian hospital where an Albanian study group (n = 134) was on placement during the month of May 2023. The questionnaire used was validated by a previous study on the same type of operators [25]. The survey included questions on various aspects of the students, such as their general characteristics, whether they had received the HBV vaccine, their adherence to infection control procedures during normal clinical activities and their understanding of blood-borne pathogen transmission and occupational exposure. The questionnaire also explored exposure incidents, students’ attitudes towards training, their professional and practical experience and their willingness to care for HIV/HBV patients. In addition to the validated questionnaire, we included 3 additional items about knowledge of air-borne transmission of Mycobacterium Tuberculosis (MT) and about influenza and measles vaccinations, specifically asking whether they were recommended for HCWs. The survey was distributed to students who came to the occupational health department for a consultation prior to their work placement (see Appendix A). All students participated anonymously and gave informed consent.
Subject characteristics are reported as numbers and percentages, depending on the type of variable. A chi-square test was used to analyse the data. p < 0.05 was considered statistically significant. All analyses were performed with SPSS version 25.0 for Windows.
3. Results
A total of 134 questionnaires were analysed. Although 138 questionnaires were collected (100% response rate), 4 questionnaires were excluded from the analysis because they were incomplete. The characteristics of the study population are shown in Table 1.

Table 1.
Characteristics of study population.
3.1. Knowledge
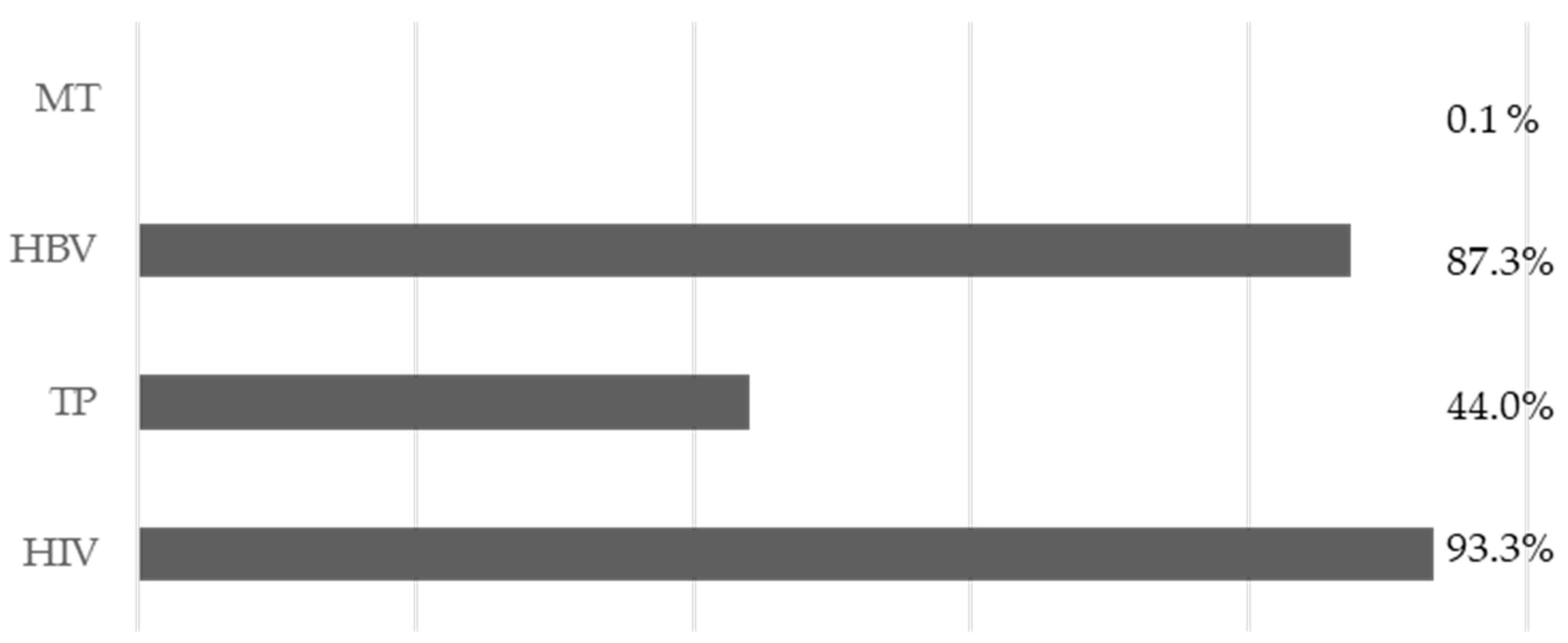
The majority of respondents (64%, n = 86) stated that they were fully aware of the problem of infectious occupational exposure. In addition, 84.3% (n = 113) declared that they have a good understanding of proper hand hygiene. Regarding blood-borne pathogens, the majority of students were aware that HIV (93% n = 125) and HBV (87% n = 117) are transmitted through blood, but less than half (45% = 59) recognised that TP is transmitted in this way (Figure 1).

Figure 1.
Answers to item 7, “Which of the following pathogenic microorganisms can be transmitted by blood?”
In the section on post-exposure procedures, the majority of participants were aware of HIV prophylaxis regimens (85%, n = 114), but only 55% (n = 74) were aware of the possibility of using the HBV vaccine in some post-exposure prophylaxis regimens. In addition, according to 27% (n = 36) of participants, the HCV vaccine can be used in post-exposure prophylaxis.
Regarding the three additional items, 94% (n = 126) of students answered that MT can be transmitted by respiratory droplets; 74.6% (n = 100) and 64.2% (n = 86) of participants were aware that influenza and measles vaccinations are strongly recommended for HCWs, respectively.
3.2. Professional Exposures
Of the total, only two participants reported a biological injury. In the first case, the injury occurred in the 6 months prior to the questionnaire, due to exposure to abrasions during a manoeuvre involving the use of sharps (surgery). In the second case, the injury occurred more than a year before, due to a skin wound from a needle during a blood test. In both cases, the students reported that they had all the necessary personal protective equipment and that they had not received any post-exposure treatment because the source patients were negative for infectious diseases.
3.3. Attitudes
All students agreed that it was very important to have in-depth knowledge of the pathogens they might be exposed to in their work, but only 74.6% (n = 100) declared that they had received education on the matter, and only 44.8% (n = 60) stated that it had been sufficient.
In terms of future work choices, 47.0% (n = 63) said that the risk of exposure to biological agents would influence their careers. In addition, 79.8% (n = 107) said that this risk of professional exposure will affect the way they work and their subsequent practices on infection control.
In addition, five students (4.7%) reported that they refused to treat infectious patients for fear of transmission.
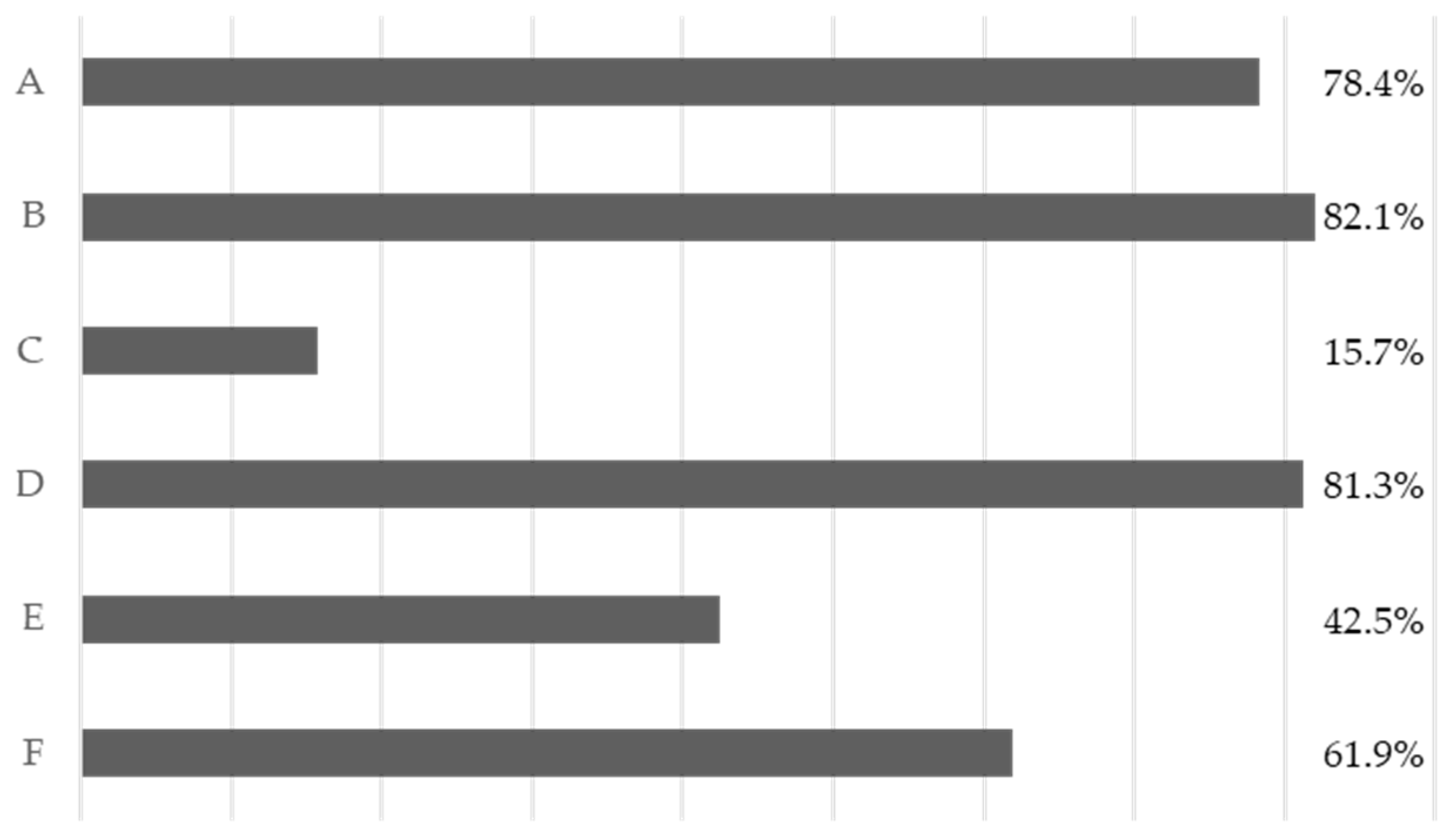
Nevertheless, regarding common infection control practices, as shown in Figure 2, the students surveyed do not have a full understanding of the regulations.
Figure 2.
Adherence to the various forms of risk prevention for infectious agents. A: Wearing a mask and working coats. B: Wearing gloves during procedures and patient-care activities. C: Wearing protective eyewear during procedures and patient-care activities. D: Removing gloves and washing hands immediately after operation and correctly antisepticising hands. E: Wearing two pairs of gloves when there are wounds on hands. F: Wearing gloves to clear away instruments and medical waste.
3.4. Statistical Analysis
A chi-squared test was performed between items 34 and 35 (vaccination recommendations) and items 2, 3, 4, 14, 24, 25, 26, 29, 30 and 33; see Table 2 and Table 3.

Table 2.
Cross-tab item 34.

Table 3.
Cross-tab item 35.
A statistically significant association was found for both items (influenza and measles vaccination) with knowledge of parenteral transmission of Treponema pallidum and with knowledge of aerogenic transmission (droplets) of MT.
Another statistical analysis (chi-square test) was also carried out to assess the correlation between item 10C and the previously analysed items (2, 3, 4, 14, 24, 25, 26, 29, 30 and 33); see Table 4.

Table 4.
Cross-tab item 10C. * PEP: post-exposure prophylaxis.
Again, a statistically significant association was found between knowledge of parenteral transmission of Treponema pallidum and items 25, 26 and 30 (“Do you think that training on occupational exposure for medical students is sufficient?”, “After learning about the risks of occupational exposure to biological agents do you think the risk will influence your future career choices?” and “Have you ever refused to treat an infectious patient for fear of transmission?”).
4. Discussion
The problem of biohazard exposure among students in health education courses is a topical issue that requires attention. It is crucial to provide adequate education and training to prospective students before they begin their journey in hospital facilities. Medical students seem to be less knowledgeable than other HCWs about healthcare-associated infections [26]. Undergraduate years are the appropriate time for acquiring the necessary knowledge and skills in this area [27]. In addition, training in infection control measures improves the compliance of HCWs with the standard precautions [28]. Such measures are essential to protect patients, HCWs and students [29].
Our study was conducted on a sample of 138 medical students from an Albanian university who were about to start their internship in our hospital. The analysis was possible because the students were visited in the occupational medicine department before starting their internship and all students were given the evaluation questionnaire. Unfortunately, the results showed that a significant percentage of the students had a significant lack of knowledge about healthcare-associated infections.
The results show the importance of improving pre-service training programmes and ensuring that the medical course includes sufficient lectures on occupational hazards. We could suggest the possibility of including pre-clinical practice examinations in order to highlight the deficiencies of the students prior to the placement.
Our analysis revealed a statistically significant association between knowledge of influenza and measles vaccination recommendations and participants’ understanding of the modes of transmission of both Treponema pallidum and MT. This finding may highlight a correlation between awareness of vaccination programmes, high vaccination compliance and comprehensive understanding of infectious disease transmission, suggesting a link between vaccination education and broader knowledge of infectious diseases. In the literature, we can already find a possible association between vaccine hesitancy and knowledge of vaccination [30].
The data also suggest that improved education about immunisation and occupational infections, particularly during the student years (e.g., during medical training), may play a critical role in preventing future problems with vaccine adherence. Previous studies have shown that students’ risk perceptions are low at the beginning of the study period, as evidenced by Ginji et al.’s study in relation to measles [31]. Healthcare professionals who understand the complexities of infectious disease transmission are more likely to adopt preventive measures such as vaccination, both for personal protection and for public health. Vaccine hesitancy, particularly among HCWs, is an ongoing problem that could be reduced by strengthening the link between disease prevention (through vaccination) and occupational health risks [32]. It has been argued that vaccine hesitancy should be addressed early in medical training to protect future health workers, preserve essential health services and reduce the risk of further pandemics [33].
The fact that vaccine hesitancy among health workers remains a persistent problem, as highlighted by previous studies in Albania, has important implications for public health strategies; it is fundamental to assess students’ attitudes to vaccination [34]. HCWs are role models and play a key role in promoting vaccination to the general population.
Statistical analysis using the chi-squared test revealed significant associations between the knowledge of HCV PEP measures (item 10C) and several other variables.
The association between participants’ knowledge of the transmission of Treponema pallidum and the misconception of an HCV prophylaxis regimen (which does not currently exist) may indicate a wider gap in understanding of the routes of disease transmission and available preventive measures. Confusion may arise from the fact that both HCV and Treponema Pallidum can be transmitted by blood or parenterally. This highlights the need for more focused training on the specifics of post-exposure protocols and the non-availability of certain prophylactics, such as the HCV vaccine.
The second significant correlation is related to the question of occupational exposure training for students. Participants who felt that occupational exposure training was inadequate were more likely to believe in the availability of an HCV vaccine for post-exposure prophylaxis. This may reflect inadequacies in curricula or clinical training regarding HCV risks and appropriate post-exposure protocols, highlighting the need to improve medical training in infectious diseases.
The third significant correlation relates to whether risk can influence future career choices, suggesting that those who believe in the existence of an HCV vaccine are also more likely to consider occupational exposure risks in their future career decisions. This suggests that misinformation or gaps in knowledge about available preventive measures could influence participants’ career choices, possibly leading them away from specialties with a higher risk of exposure due to unfounded fears or misunderstandings about protective strategies.
The last correlation, related to the question of whether they ever refused to care for patients for fear of infection, indicates a deeper issue of fear and uncertainty when dealing with infectious patients, particularly if HCW students are uncertain about available prophylaxis options or do not understand post-exposure protocols. This may contribute to stigmatisation of infectious patients and reluctance to engage in certain medical practices, further highlighting the need for comprehensive training on occupational exposure risks and protection methods to reduce fear-based refusals to treat.
The small sample size, unevenly distributed in gender (F = 80.9%), is certainly a limitation of the study, but the 100% response rate reinforces the validity of the results obtained.
5. Conclusions
In our study, we found that a small (not negligible) percentage of medical students have little knowledge of occupational infections and biohazards.
Furthermore, although the majority of students recognise a moral obligation to care for infectious patients, there are cases of refusal by some students. Statistical analysis shows a positive correlation between vaccination awareness and knowledge of infectious diseases, with greater vaccination compliance among those with a better understanding of biological risks. This highlights the importance of accurate information to prevent problems with vaccine adherence. The findings indicate that pre-clinical training programmes need to be strengthened to ensure better preparation of students before they enter the hospital environment. Also crucial are information programmes regarding vaccinations to prevent adherence and hesitation problems.
Further investigations are needed to confirm and extend these findings, and we hope that the questionnaire we used can be reproduced in further studies to extend the research.
Author Contributions
Conceptualization, L.I. and L.C.; data curation, L.C., G.B., C.F., A.M. (Andrea Mazza), A.P. (Agostino Paolino), C.S. and V.C.; writing—original draft, L.I.; writing—review and editing, E.B., G.S., A.P. (Antonio Pietroiusti) and A.M. (Andrea Magrini). All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Policlinico Tor Vergata of Rome (IRB number: 133/21, date: 28 March 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
We are grateful to the Policlinico Tor Vergata in Rome for supporting our research.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
Occupational exposure questionnaire for medical students
Complete the questionnaire in its entirety by marking the correct answer with an X.
To guide in answering the following questions effectively, here is the definition of occupational exposure: “any needle-stick injury, cut abrasion or instrument puncture or any other exposure to blood and other body fluids such as splashes into the eyes, nose, mouth or broken skin”.
Part I
| 1 | You are a medical student | Graduate | Undergraduate | |||||||||
| 2 | You are | Male | Female | |||||||||
| 3 | How much do you know about the infectious occupational exposure problem before this survey? | Fully known | Just know a little | Completely have no idea about it | ||||||||
| 4 | The infection control programme you are compliant with during routine clinical work is/are. (You can choose more than one) | Wearing masks, working coats and hats | A | |||||||||
| Wearing gloves during procedures and patient-care activities | B | |||||||||||
| Wearing protective eyewear or face shield during procedures and patient-care activities | C | |||||||||||
| Removing gloves and washing hands immediately after operation and correctly antisepticising hands | D | |||||||||||
| Wearing two pairs of gloves when there are wounds on hands | E | |||||||||||
| Wearing gloves to clear away instruments and medical waste | F | |||||||||||
| 5 | How much do you know about the correct methods for hand hygiene? | Fully known | Just know a little | Completely have no idea about it | ||||||||
| 6 | Have you received HBV vaccines? | Yes | No | |||||||||
| 7 | Which of the following pathogenic microorganisms can be transmitted by blood? | Human immunodeficiency virus (HIV) | A | |||||||||
| Treponema pallidum (TP) | B | |||||||||||
| Hepatitis B virus (HBV) | C | |||||||||||
| Mycobacterium tubercolosis (MT) | D | |||||||||||
| 8 | Please rank the risk level of the following options from high to low. (e.g., A > B > C) | __ | > | __ | > | __ | > | __ | > | __ | > | __ |
| A | Contact with patients’ blood and body fluids through touching integrated skin | |||||||||||
| B | Contact with patients’ blood and body fluid through the mucous membranes of the eyes/nose/mouth | |||||||||||
| C | Exposure by abrasion | |||||||||||
| D | Exposure via a sharp cutting injury | |||||||||||
| E | Exposure by an injury with a non-hollow needle without visible blood | |||||||||||
| F | Exposure by an injury with a hollow bore needle and visible blood on the device | |||||||||||
| 9 | Once exposed to blood or contaminated body fluids, what general measures should be taken as soon as possible? | |||||||||||
Part II
| 10 | Which of the following is/are correct? | |||||||
| A | A ‘basic’ drug regimen and an ‘expanded’ drug regimen were recommended measures for post-exposure prophylaxis (PEP) after occupational exposure to HIV | True | False | |||||
| B | The HBV vaccine can be chosen for PEP after occupational exposure to HBV | True | False | |||||
| C | There is an immediate PEP regimen—HCV vaccine—to prevent infection after occupational exposure to HCV | True | False | |||||
| D | Intramuscular injection of Benzathine Benzylpenicillinis is one of the prophylaxis measures after occupational exposure to TP. | True | False | |||||
| 11 | The PEP drug regimen should be initiated within ( ) hours after occupational exposure to HIV. | 1 | 12 | 24 | 48 | I don’t know | ||
| 12 | The recommended duration of PEP drug regimen after occupational exposure to HIV is | 7 days | 14 days | 28 days | 60 days | I don’t know | ||
| 13 | Do you know the correct time point for medical workers exposed to HIV to evaluate HIV seroconversion? | Yes (the correct time point is:) | No | |||||
| 14 | Have you experienced occupational exposure since starting dental clinical work? | Yes | No | |||||
| Note: if yes, please continue from question 15; otherwise, please continue from question 23 (part III) | ||||||||
| 15 | How many occupational exposures have you experienced? | 1 | 2 | 3–5 | >5 | |||
| 16 | When did your last occupational exposure occur? | Within 1–6 months | Within 6–12 months | Before 1 year | ||||
| 17 | The nature of your exposure is (you can choose more than one) | Percutaneous injuries with a needle | A | |||||
| Exposed by abrasion | B | |||||||
| Contacted with patients’ blood and body fluid through the mucous membranes of the eyes/nose/mouth | C | |||||||
| Contacted with patients’ blood and body fluid through touching integrated skin; | D | |||||||
| Others, such as: | E | |||||||
| 18 | The processing you performed during your occupational exposure is | Use of needles (blood sampling) | A | |||||
| Use of cutting edges (surgery) | B | |||||||
| Drug administration | C | |||||||
| Others, such as: | D | |||||||
| 19 | At the time of exposure, you wore (you can choose more than one) | Gloves | A | |||||
| Face shield or protective eyewear | B | |||||||
| Mask | C | |||||||
| Protective apron | D | |||||||
| No protection | E | |||||||
| 20 | Did the source patients have infectious diseases? | Yes: | No | Unknown | ||||
| 21 | Did you take any treatment or measure after exposure? | Yes | No | |||||
| 22 | The treatments or measures you took after exposure included the following: | |||||||
Part III
| 23 | Do you think that there is a necessity for dental students to gain knowledge about infectious professional exposure and its prevention and management? | Yes, it is highly necessary | A | |||||
| Yes, it is necessary | B | |||||||
| I don’t care | C | |||||||
| No, there is no necessity | D | |||||||
| 24 | Had you ever received education about infectious professional exposure and its prevention and management? | Yes | No | |||||
| 25 | Do you think that the ‘occupational exposure’ education for medical students is sufficient? | Yes | No | |||||
| 26 | After knowing the risk of infectious professional exposure, will the concerns about risk influence your career choice? | Yes | No | |||||
| 27 | After knowing the risk of infectious professional exposure, will the concerns about risk influence your subsequent treating way (namely strengthen personal protection)? | Yes | No | |||||
| 28 | What changing aspects will you perform to strengthen personal protection in the subsequent clinical work? | |||||||
| 29 | Do you think that dental students have morality and responsibility for treating infected patients? | Yes | No | |||||
| 30 | Had you ever refused to treat infected patients because of fear of transmission? | Yes | No | |||||
| 31 | After knowing about infectious professional exposure, you will be with ( ) to treat HIV-infected patients? | Very strong unwillingness | A | |||||
| Strong unwillingness | B | |||||||
| Moderate unwillingness | C | |||||||
| Slight unwillingness | D | |||||||
| No unwillingness | E | |||||||
| 32 | After knowing about infectious professional exposure, you will be with ( ) to treat HBV-infected patients? | Very strong unwillingness | A | |||||
| Strong unwillingness | B | |||||||
| Moderate unwillingness | C | |||||||
| Slight unwillingness | D | |||||||
| No unwillingness | E | |||||||
| 33 | Tuberculosis is transmitted through respiratory droplets (droplets or Flügge) | True | False | Unknown | ||||
| 34 | The flu vaccine is strongly recommended for healthcare workers. | True | False | Unknown | ||||
| 35 | The measles vaccine is strongly recommended for healthcare workers. | True | False | Unknown | ||||
References
- ILO/WHO Joint ILO/WHO Guidelines on Health Services and HIV/AIDS; International Labour Organization and World Health Organization: Geneva, Switzerland, 2005.
- Mengistu, D.A.; Dirirsa, G.; Mati, E.; Ayele, D.M.; Bayu, K.; Deriba, W.; Alemu, F.K.; Demmu, Y.M.; Asefa, Y.A.; Geremew, A. Global Occupational Exposure to Blood and Body Fluids among Healthcare Workers: Systematic Review and Meta-Analysis. Can. J. Infect. Dis. Med. Microbiol. 2022, 2022, 5732046. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Auta, A.; O Adewuyi, E.; Tor-Anyiin, A.; Edor, J.P.; Kureh, G.T.; Khanal, V.; Oga, E.; Adeloye, D. Global prevalence of percutaneous injuries among healthcare workers: A systematic review and meta-analysis. Int. J. Epidemiol. 2018, 47, 1972–1980. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Systematic Review on Hepatitis B and C Prevalence in the EU/EEA; ECDC: Stockholm, Sweden, 2016. [Google Scholar]
- European Centre for Disease Prevention and Control/WHO Regional Office for Europe. HIV/AIDS Surveillance in Europe 2023—2022 Data; ECDC: Stockholm, Sweden, 2023. [Google Scholar]
- Resuli, B.; Prifti, S.; Kraja, B.; Nurka, T.; Basho, M.; Sadiku, E. Epidemiology of hepatitis B virus infection in Albania. World J. Gastroenterol. 2009, 15, 849–852. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shundi, L.; Vila, B.; Zeqiraj, E.; Ahmeti, A.; Vasili, A.; Shehu, A.; Balla, F.; Bino, S. Epidemiology of Hepatitis C in Albania. In Proceedings of the ESCAIDE, Stockholm, Sweden, 6–8 November 2011; p. 122. [Google Scholar]
- UNAIDS—Joint United Nations Programme on HIV/AIDS: Country Progress Report—Albania; Global AIDS Monitoring 2020. 2020. Available online: https://www.ecoi.net/en/file/local/2038350/ALB_2020_countryreport.pdf (accessed on 20 December 2024).
- Tuberculosis Incidence (per 100000 Population). Available online: https://data.who.int/indicators/i/13B4226/C288D13#disclaimer-maps (accessed on 20 December 2024).
- Bino, S.; Kakarriqi, E.; Xibinaku, M.; Ion-Nedelcu, N.; Bukli, M.; Emiroglu, N.; Uzicanin, A. Measles-rubella mass immunization campaign in Albania, November 2000. J. Infect. Dis. 2003, 187, S223–S229. [Google Scholar] [CrossRef]
- Çomo, N.; Meta, E.; Qato, M.; Kraja, D.; Pipero, P.; Fico, A. Measles, a re-emerging disease in Albania: Epidemiology and clinical presentations. South East. Eur. J. Public Health 2022. [Google Scholar] [CrossRef]
- Keita-Perse, O.; Pradier, C.; Rosenthal, E.; Altare, J.; Cassuto, J.P.; Dellamonica, P. Les étudiants hospitaliers: Une population à risque d’accidents d’exposition au sang (AES) [Hospital medical students: A population at risk for accidental exposure to blood]. Presse Med. 1998, 27, 1723–1726. (In French) [Google Scholar] [PubMed]
- Elisa, N.; Ssenyonga, L.; Iramiot, J.S.; Nuwasiima, D.; Nekaka, R. Sharp/needlestick injuries among clinical students at a tertiary hospital in eastern Uganda. medRxiv 2023. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Charca-Benavente, L.C.; Huanca-Ruelas, G.H.; Moreno-Loaiza, O. Biological accidents in last-year medical students from three hospitals in Lima Peru. Medwave 2016, 16, e6514. [Google Scholar] [CrossRef] [PubMed]
- Bouya, S.; Balouchi, A.; Rafiemanesh, H.; Amirshahi, M.; Dastres, M.; Moghadam, M.P.; Behnamfar, N.; Shyeback, M.; Badakhsh, M.; Allahyari, J.; et al. Global Prevalence and Device Related Causes of Needle Stick Injuries among Health Care Workers: A Systematic Review and Meta-Analysis. Ann. Glob. Health 2020, 86, 35. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Musa, S.; Peek-Asa, C.; Young, T.; Jovanovic, N. Needle Stick Injuries, Sharp Injuries and other Occupational Exposures to Blood and Body Fluids among Health Care Workers in a general hospital in Sarajevo, Bosnia and Herzegovina. Int. J. Occup. Saf. Health 2014, 4, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Irmak, Z.; Baybuga, M.S. Needlestick and sharps injuries among Turkish nursing students: A cross-sectional study. Int. J. Nurs. Pract. 2011, 17, 151–157. [Google Scholar] [CrossRef]
- Kinlin, L.M.; Mittleman, M.A.; Harris, A.D.; Rubin, M.A.; Fisman, D.N. Use of gloves and reduction of risk of injury caused by needles or sharp medical devices in healthcare workers: Results from a case-crossover study. Infect. Control Hosp. Epidemiol. 2010, 31, 908–917. [Google Scholar] [CrossRef] [PubMed]
- Ottino, M.C.; Argentero, A.; Argentero, P.A.; Garzaro, G.; Zotti, C.M. Needlestick prevention devices: Data from hospital surveillance in Piedmont, Italy—Comprehensive analysis on needlestick injuries between healthcare workers after the introduction of safety devices. BMJ Open 2019, 9, e030576. [Google Scholar] [CrossRef] [PubMed]
- Milward, M.R.; Cooper, P.R. Competency assessment for infection control in the undergraduate dental curriculum. Eur. J. Dent. Educ. 2007, 11, 148–154. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Saleem, H.; Waly, N.; Abdelgawad, F. Knowledge, Attitude, and Practice (KAP) of post exposure prophylaxis for fifth year dental students at a private Egyptian university: A cross-sectional study. BMC Oral Health 2023, 23, 167. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Abu-Siniyeh, A.; Al-Shehri, S.S. Safety in Medical Laboratories: Perception and Practice of University Students and Laboratory Workers. Appl. Biosaf. 2021, 26 (Suppl. S1), S34–S42. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Al-Mugheed, K.; Farghaly, S.M.; Baghdadi, N.A.; Oweidat, I.; Alzoubi, M.M. Incidence, knowledge, attitude and practice toward needle stick injury among nursing students in Saudi Arabia. Front. Public Health 2023, 11, 1160680. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Albadrani, M.S.; Abdulaal, A.M.; Aljabri, A.M.; Aljohani, S.S.; Aljohani, S.F.; Sindi, M.A.; Jan, H.K.; Alsaedi, H.; Alamri, W.M.; Alharbi, A.M.; et al. Knowledge, Attitudes, and Practices Toward the Prevention of Hepatitis B Virus Infection Among Medical Students in Medina City, Kingdom of Saudi Arabia. Cureus 2023, 15, e48845. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wu, L.; Yin, Y.L.; Song, J.L.; Chen, Y.; Wu, Y.F.; Zhao, L. Knowledge, attitudes and practices surrounding occupational blood-borne pathogen exposure amongst students in two Chinese dental schools. Eur. J. Dent. Educ. 2016, 20, 206–212. [Google Scholar] [CrossRef] [PubMed]
- D’Alessandro, D.; Agodi, A.; Auxilia, F.; Brusaferro, S.; Calligaris, L.; Ferrante, M.; Montagna, M.T.; Mura, I.; Napoli, C.; Pasquarella, C.; et al. Prevention of healthcare associated infections: Medical and nursing students’ knowledge in Italy. Nurse Educ. Today 2014, 34, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Tipple, A.F.V.; Pereira, M.S.; Hayashida, M.; Moriya, T.M.; Souza, A.C.S. O ensino do controle de infecção: Um ensaio teórico-prático. Rev. Latino-Am. Enferm. 2003, 11, 245–250. [Google Scholar] [CrossRef]
- Moralejo, D.; El Dib, R.; Prata, R.A.; Barretti, P.; Corrêa, I. Improving adherence to Standard Precautions for the control of health care-associated infections. Cochrane Database Syst. Rev. 2018, 2, CD010768. [Google Scholar] [CrossRef] [PubMed]
- Clarke, S.P.; Rockett, J.L.; Sloane, D.M.; Aiken, L.H. Organizational climate, staffing, and safety equipment as predictors of needlestick injuries and near-misses in hospital nurses. Am. J. Infect. Control 2002, 30, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Trabucco Aurilio, M.; Mennini, F.S.; Ferrari, C.; Somma, G.; Di Giampaolo, L.; Bolcato, M.; De-Giorgio, F.; Muscatello, R.; Magrini, A.; Coppeta, L. Main Predictors of COVID-19 Vaccination Uptake among Italian Healthcare Workers in Relation to Variable Degrees of Hesitancy: Result from a Cross-Sectional Online Survey. Trop. Med. Infect. Dis. 2022, 7, 419. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gjini, E.; Cenko, F.; Mehmeti, I.; Giulia, A.; Biondi, G.; Moramarco, S.; Buonomo, E. Perceptions of Measles and vaccine Knowledge and Hesitancy among Health-care students in an Albanian University: Results from a survey. Biomed. Prev. Issues 2019, 1, 210. [Google Scholar] [CrossRef]
- Kaur, M.; Coppeta, L.; Olesen, O.F. Vaccine Hesitancy among Healthcare Workers in Europe: A Systematic Review. Vaccines 2023, 11, 1657. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Buonomo, E.; Cenko, F.; Piunno, G.; Di Giovanni, D.; Gjini, E.; Kërpi, B.; Carestia, M.; Moramarco, S.; Ferrari, C.; Coppeta, L. Vaccine Hesitancy, Knowledge, and COVID-19 Vaccination in a Sample of Italian and Albanian Healthcare Students Attending an University in Albania. Trop. Med. Infect. Dis. 2024, 9, 57. [Google Scholar] [CrossRef] [PubMed]
- Gjini, E.; Carestia, M.; Cenko, F.; Di Giovanni, D.; Mehmeti, I.; Moramarco, S.; Yulli, A.; Buonomo, E. Hesitancy toward Childhood Vaccinations: Preliminary Results from an Albanian Nursing Staff’s Investigation. Nurs. Res. Pract. 2022, 2022, 7814488. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).