Abstract
Contemporary literature lacks examples of intradural, extramedullary spinal glomangiomas. Moreover, glomus tumors in general are exceedingly rare among benign spinal tumors and are mostly located within epidural space or within intervertebral foramen, and only a few cases have been documented to date. This report provides a detailed analysis of the clinical presentation, imaging characteristics, surgical intervention, and pathological findings of a 45-year-old patient experiencing progressive locomotor deterioration. The tumor was surgically excised, and subsequent histological examination identified it as a representative of glomus tumors—a glomangioma. Notably, this represents a unique case as it was the first example of such a tumor being discovered intradurally. Radical surgical excision remains the modality of choice in most benign spinal tumors of this localization. Although the malignant transformation of glomus tumors within the spine has not been documented thus far, cases have arisen in other areas. Consequently, we will investigate potential oncological treatments for cases with malignant potential and highlight advancements in surgical techniques for benign intradural spinal tumors.
1. Introduction
Spinal tumors comprise around 15% of central nervous system tumors [1]. They are categorized as primary benign or primary/metastatic malignant tumors. While benign lesions make up to 80% of all primary spinal cord tumors, the remainder are malignant [2]. Anatomical localization within the spinal column distinguishes them as intradural or extradural. Intradural tumors can be further classified based on their relationship to the spinal cord as either intramedullary (IDIM) or extramedullary (IDEM). Primary spinal neoplasms exhibit a relatively low incidence rate, accounting for approximately 2–4% of CNS tumors, with an estimated 65% manifesting as intradural extramedullary lesions [3,4].
Although the manifestation of intradural extramedullary tumors may not invariably demonstrate pathognomonic traits and their presentation is most commonly related to the affected spinal cord level, the utilization of magnetic resonance imaging (MRI) frequently facilitates the recognition of essential characteristic features. Given the anatomical proximity to spinal nerves or the dura mater, schwannomas, meningiomas, and ependymomas emerge as the predominant primary tumors of the spinal canal [5,6]. Certain malignant primary [7,8,9,10] or metastatic [11,12] intradural lesions, although infrequent, may resemble their primary counterparts; however, their initial management differs as it typically requires adjunct oncological treatment [13,14]. Among the less commonly encountered non-malignant tumors are ependymomas, hemangiomas, lipomas, paragangliomas, vascular neoplasms, nerve sheath myxoma, and other exceptionally rare entities, including the seldom-described glomus tumors of the spinal canal [15,16].
In this study, we present a case report elucidating a unique example of an intradural extramedullary histological variant of a glomus tumor—glomangioma.
2. General Information and Histopathological Considerations
Glomus tumors, categorized as mesenchymal tumors in the latest WHO Classification of Tumors (2021), account for less than 2% of soft tissue neoplasms [17,18]. In contrast to paragangliomas, which stem from chromaffin cells [19], glomus tumors are thought to arise from the Sucquet–Hoyer canal situated within the glomus body—a specialized arteriovenous anastomosis regulating skin temperature. These structures are surrounded by layers of epithelioid glomus cells that express smooth muscle actin (SMA) [20,21]. Low temperatures prompt the relaxation of glomus cells, facilitating the opening of the anastomosis and redirecting blood flow away from the capillary network, thus conserving body heat [22]. Although glomus tumors typically manifest in the dermis or subcutis of the distal extremities, especially phalanges, a plethora of various other extracutaneous localizations has been described in the literature [23]. One conceivable rationale of this ever-present distribution is that these tumors may originate from abundant perivascular cells capable of differentiating into glomoid cells [23]. This can be hypothesized through the neural crest origin of glomus cells and the ability of perivascular cells to adopt neural characteristics [24,25]. Perivascular cells, or pericytes, are cells situated along the walls of blood vessels, originating primarily from mesenchymal stem cells during embryonic development from the mesoderm, the middle layer of embryonic germ cells [26,27]. In certain organs, such as the central nervous system, pericytes may also arise from neuroectodermal cells [28,29]. In adults, these cells can differentiate from local precursor cells or stem cells, including those in the bone marrow, and are capable of transforming into various cell types like chondrocytes, osteoblasts, and adipocytes. The specific origin of pericytes can vary by organ, and their migration and localization are critical during vascular development, where they embed in vessel walls to regulate blood flow, vascular stability, and angiogenesis [30].
While the precise etiology of glomus tumors remains elusive, several predisposing factors have been proposed to date. These include sporadic mutations in the glomulin gene (GLMN—coded by 1p21–1p22) and a diagnosis of neurofibromatosis type 1 [31,32]. Yanai et al. highlighted an association between neurofibromatosis type 1 (NF1) and glomangioma, with multiple glomus tumors characteristic of NF1 patients [33]. Brems et al. identified germline and somatic NF1 mutations, as well as RAS-MAPK hyperactivation, in NF1-associated glomus tumors, distinguishing them from sporadic cases [34].
Preliminary research has indicated that genetic modifications involve BRAF, NOTCH, PDGFRB, KRAS, and SMARCB1 [18,35,36,37,38]. Moreover, certain authors propose a traumatic etiology, drawing from a documented case involving a digital glomangioma [39]. Glomus tumors tend to affect individuals between 20 to 40 years old with female preponderance [23,40].
Glomus tumors are distinguished by their histological composition, primarily consisting of glomus cells, blood vessels, and vascular smooth muscle cells [23,41,42]. Within this tumor group, classification into three variants based on histological structure is feasible: solid tumors, glomangiomas, and glomangiomyomas [43,44,45] (Table 1). These variants display varying proportions of the aforementioned histological elements [42,43]. Hematoxylin and eosin (H&E) staining is conventionally employed for visualization [46,47,48]. Glomus cells are a consistent finding across all variants, with solid tumors predominantly composed of glomus cells, glomangiomas characterized by an abundance of blood vessels, and glomangiomyomas exhibiting a prevalence of smooth muscle cells among a network of blood vessels [41].

Table 1.
Histological classification of glomus tumors.
The microscopic examination of glomangiomas reveals vascular structures reminiscent of cavernous hemangiomas surrounded by round or oval cells featuring well-defined margins, eosinophilic cytoplasm, centrally located nuclei, and an absence of atypia [18,46,47]. Nevertheless, immunohistochemical analysis plays a pivotal role in confirming the diagnosis. Integrating standard histological examination with immunohistochemistry enhances diagnostic precision [49]. Several markers associated with glomus tumors aid in their identification, including smooth muscle actin (SMA), collagen type IV, vimentin, and muscle-specific actin (MSA) [50]. Conversely, glomus tumors typically lack positive staining for antibodies targeting S100, chromogranin, desmin, cytokeratin, HMB-45, melan-A, or synaptophysin [18,51]. The proliferation index, as indicated by Ki-67 staining, generally remains low. Furthermore, while tumor cells may exhibit positive staining for CD34, caldesmon, or calponin, there have been reports of negative immunostaining for these markers in selected cases [41]. Notably, positive staining for SMA serves as a definitive marker for distinguishing glomus tumors from other types of neoplasms [45].
Malignant glomus tumors are extremely uncommon, accounting for up to 2.9% of all glomus tumors, and are exclusively documented in the literature as isolated case reports originating from different institutions. Glomus tumors of uncertain malignant potential are defined by tumors that do not meet the standards for malignancy yet display at least one unusual feature other than nuclear pleomorphism [52].
The primary aim of this investigation was to outline both the diagnostic methodologies and treatment modalities for glomangiomas of the spinal canal. Furthermore, we conducted a systematic review of the literature to provide a comprehensive scientific understanding of this topic. Given that the standard approach for most benign intradural tumors typically involves radical excision, we also expounded upon various surgical techniques, including microsurgical, endoscopic, or robotic approaches. In certain instances where residual tumor remains due to incomplete resection or in cases where malignant potential necessitates adjuvant therapy, we discussed the current radiotherapy methods, as well as the employment of chemotherapy and immunotherapy for malignant cases.
3. Case Presentation
A 45-year-old male sought medical attention at our outpatient facility, reporting a progressive decline in locomotor function. Upon evaluation via magnetic resonance imaging (MRI), an oval-shaped intradural lesion was identified at the L3 vertebral level, occupying the spinal canal and exerting bilateral nerve root compression. Neurological examination revealed diminished lower extremity tendon reflexes and mild weakness in knee extension and hip external rotation, devoid of sensory deficits.
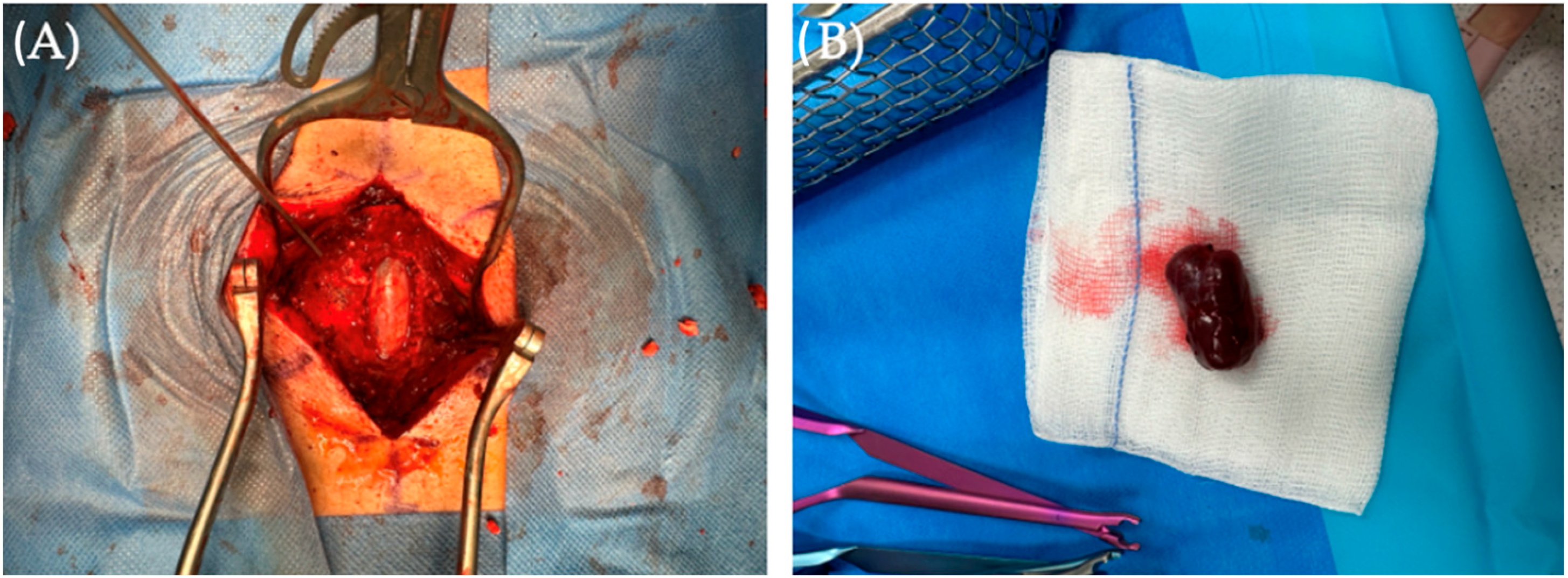
Given the diagnostic findings, surgical intervention was deemed necessary. We employed a traditional microsurgical approach for radical tumor excision. In June 2023, the patient underwent L2, L3, and L4 laminectomy with intraoperative peripheral nerve function monitoring conducted by a neurophysiologist. Intraoperatively, a bulging of the dural sac at the L3 level was observed (Figure 1A). After precise incision and dissection, we performed dural splitting and microsurgical resection of the inner dura while preserving the outer layer using the Saito method. This exposed the arachnoid membrane, which was subsequently incised, revealing clear cerebrospinal fluid (CSF) and a solid, red-grayish tumor compressing the spinal nerve roots dorsally. The tumor had a small vascular peduncle, which was coagulated and cut. Careful microsurgical dissection enabled complete tumor removal, confirming its non-neural and non-dural origin (Figure 1B). Importantly, neither motor nor sensory responses (MEP and SEP) were decreased during or after surgery
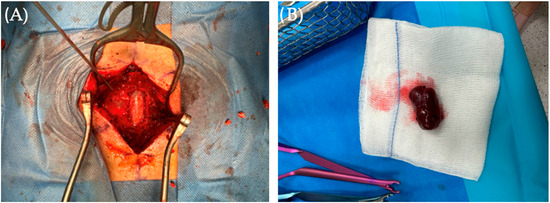
Figure 1.
(A) Following laminectomy for spinal canal decompression, a bulging dural sack appeared with tumor located intradurally. (B) Picture presents the brownish-in-color tumor, resected en bloc.
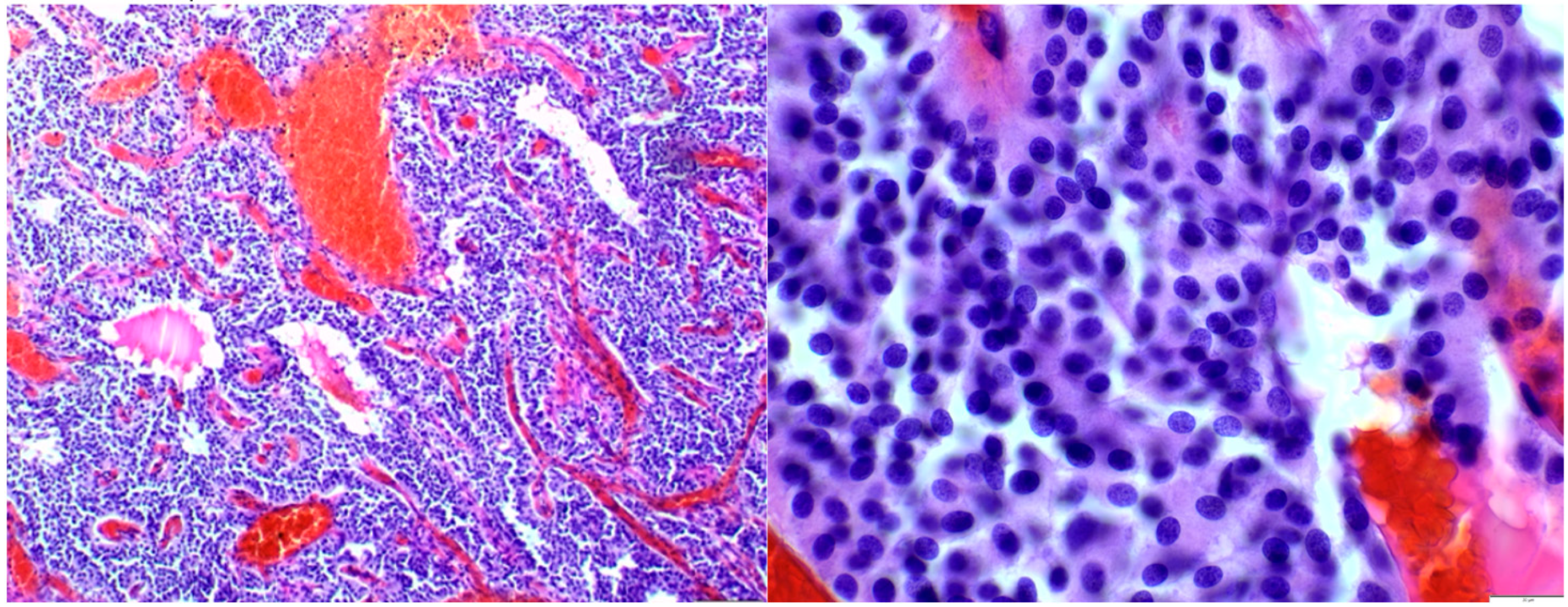
Histological examination revealed a solid and syncytial proliferation of round cells surrounding blood vessels exhibiting perivascular hyalinization. Immunohistochemical staining demonstrated positivity for smooth muscle actin (SMA) and negativity for epithelial membrane antigen (EMA), glial fibrillary acidic protein (GFAP), S100, and GATA3, consistent with a diagnosis of glomangioma (Figure 2).
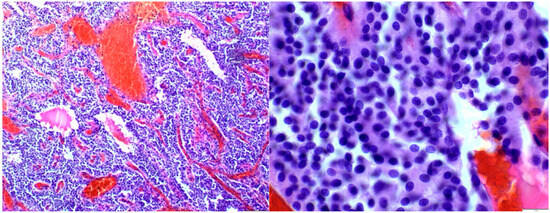
Figure 2.
Histological analysis showed cohesive round cell proliferation around blood vessels with perivascular hyalinization.
Following the procedure, the patient demonstrated gradual improvement and was mobilized by a physiotherapist on postoperative day one. The gradual resolution of paresis occurred within several days of hospitalization, leading to the patient’s discharge in a stable condition. Only mild, typical postoperative pain symptoms in the operated area remained. No CSF leakage was observed and the wound healed well.
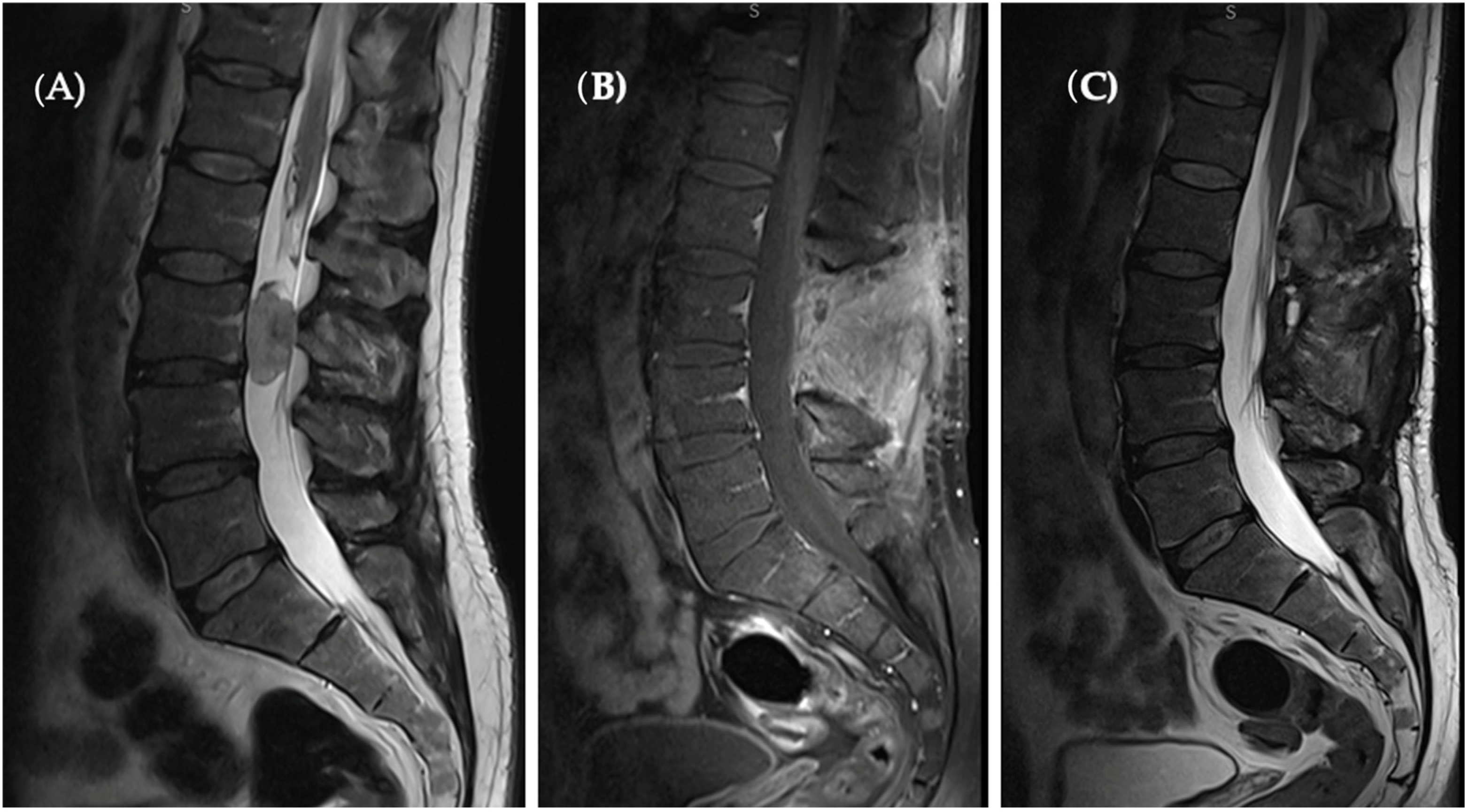
Subsequent MRI imaging undertaken after a one-year period displayed no evidence of tumor recurrence, precluding the necessity for adjuvant therapy (Figure 3).
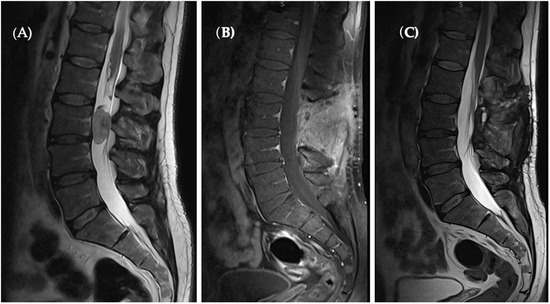
Figure 3.
(A) Pre-op T2 sagittal MRI revealed a hyperintense oval-shaped lesion located at the L3 level occupying spinal canal. (B) Sagittal T1 with contrast enhanced as well as T2 sagittal. (C) Sections present a complete tumor removal and no sign of recurrence.
4. Materials and Methods
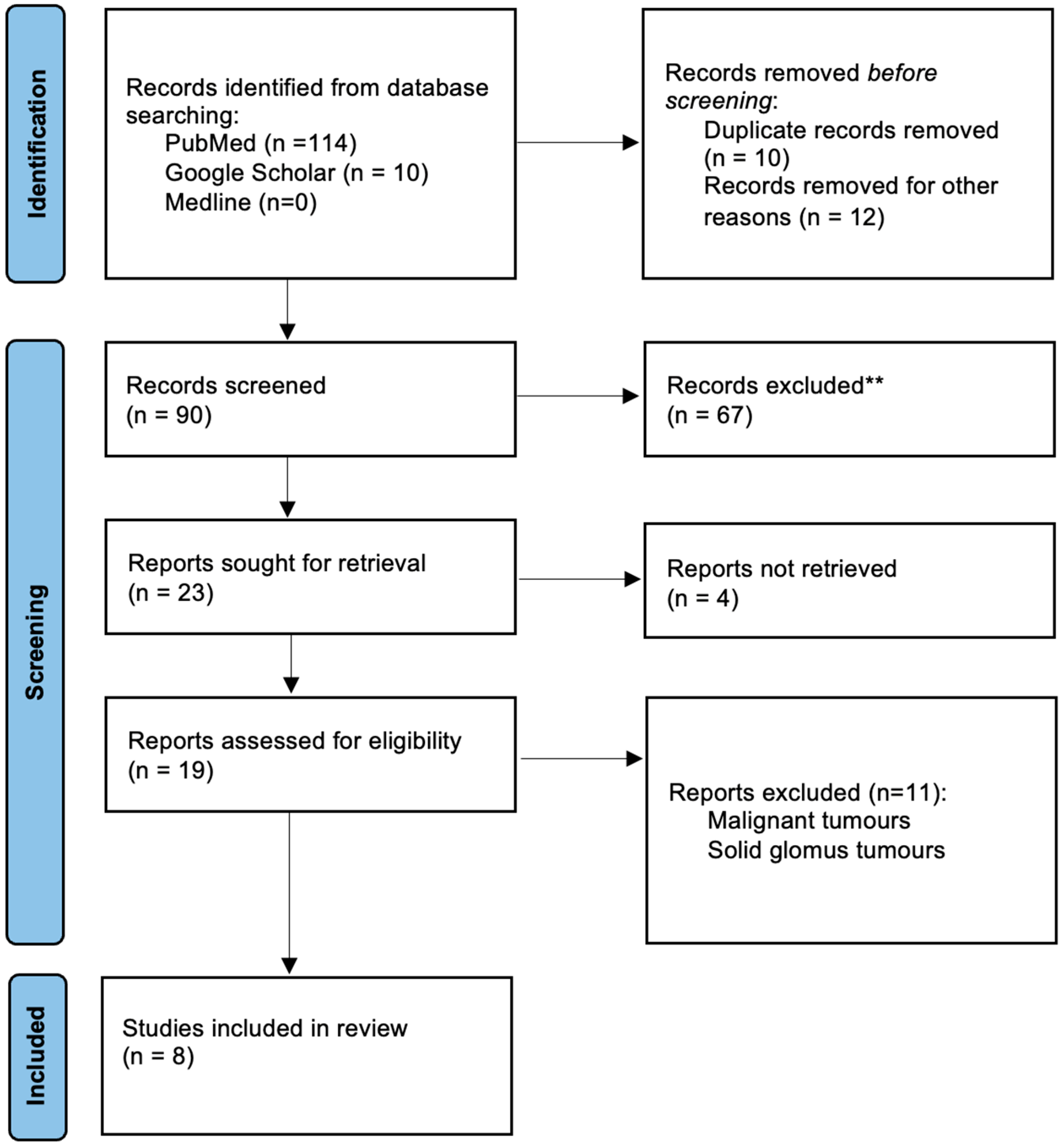
The authors conducted a comprehensive systematic review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, ensuring meticulous examination of relevant literature. The search, conducted in March 2024, included studies published in English without time restrictions. Renowned biomedical databases such as PubMed, Medline, and Google Scholar were utilized, with two queries created: one for PubMed and Medline (“glomangioma” AND “spine” OR “spinal”), and another for Google Scholar (“glomus tumors” OR “glomangioma” AND “spine” OR “spinal” NOT “hand” NOT “foot”). Initially, 124 records were identified, but after screening and eligibility assessments, 19 studies addressing spinal glomus tumors were included. Two independent researchers performed each review step. Notably, the focus was primarily on glomangiomas of the spine, excluding malignant glomus tumors and other benign types. Ultimately, only eight publications met the stringent inclusion criteria and were used in synthesizing the findings of this study (Figure 4).
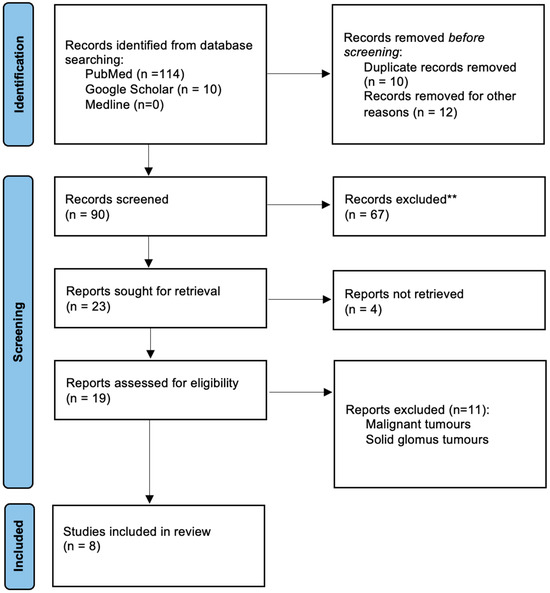
Figure 4.
Flowchart of the identification and selection of studies according to the 2020 PRISMA statement.
5. Results
Among the 19 reports identified in our systematic review that described cases of glomus tumors of the spine, only a limited number included cases of glomangioma, totaling eight instances. Key clinical characteristics extracted from these studies encompassed patient demographics (gender and age), tumor localization, neurological deficits, treatment modalities, time to diagnosis, malignant potential, recurrence rates, and additional therapeutic interventions when required. In the analyzed cases, there were four female and four male patients, with a median age of 48.6 years. The youngest patient was 26 and the oldest was 65 years old. Each patient underwent magnetic resonance imaging (MRI), revealing an intraspinal tumor mass, with six cases occupying intervertebral foramina and two located within the epidural space. Predominantly, tumors were situated at the thoracic level (five cases), but one was located on the cervico-thoracic junction with the remaining two in the cervical or lumbar regions. The most prevalent clinical presentation was chronic pain, while the remaining patients exhibited progressive paraparesis or an unsteady gait. The mean time to diagnosis circulates around 4 months. Surgical intervention alone was undertaken in most of the cases, except for one patient who received adjuvant therapy in the shape of radiotherapy. Among the surgically treated patients, none experienced recurrence during follow-up assessments, and histopathological examination did not reveal malignancy. Two patients exhibited uncertain malignancy through histopathology and only one required subsequent radiotherapy.
6. Discussion
To date, the literature records a total of 19 documented cases of glomus tumors associated with the spinal canal, among which only eight cases are specifically classified as glomangiomas (Table 2). The remaining tumors are solid glomus tumors, and there is one documented case of glomangiomyoma thus far [53]. In general, including solid glomus tumors, these lesions predominantly involve the thoracic level, followed by the lumbar spine, while cervical involvement is the least common, which is similar to the data obtained from the present systematic review on glomangiomas. Among glomangiomas of spinal origin, the intervertebral foramina remains the most common location followed by the epidural space. Despite the inclusion of case reports with systematic reviews encompassing glomus tumors as a collective entity, none have exclusively focused on glomangiomas. Additionally, variations in the reported number of cases are evident across the studies found. Notably, all glomangiomas referenced in the present review originate either from the epidural space or are situated within the intervertebral foramina. The case presented herein represents the sole example in the extant literature demonstrating an intradural location, thus posing diagnostic challenges due to their potential resemblance to more common spinal pathologies.

Table 2.
Summary of spinal glomangiomas in the literature.
Generally, the cornerstone of treatment for all intradural, extramedullary lesions remain radical surgical excision, which typically results in favorable long-term outcomes with minimal risk of recurrence [54,55]. However, approximately 10% of patients experience a recurrence after surgery due to incomplete removal [44]. In instances where total resection is unattainable, observation may be considered for small, asymptomatic tumors. The most employed surgical technique involves traditional microscopic tumor excision, and the same proven tactics were used by authors of the study, which enabled reaching a favorable outcome. Nevertheless, this classical method entails making an extended midline incision (typically two levels above and below the tumor), dissecting the paraspinal muscles subperiosteally, and performing multi-level laminectomies or facetectomies. This approach damages a significant portion of the structures within the posterior column, leading to decreased spinal stability and the potential for spinal deformity [56]. Moreover, surgical treatment inherently poses risks, highlighted by ACS-NSQIP data on spinal tumor surgery outcomes. According to their research, key adverse outcome predictors include, e.g., dependent functional status, emergency surgeries, and higher ASA classifications. This underscores the importance of preoperative risk stratification and enhanced post-discharge surveillance [57].
Minimally invasive endoscopic techniques are increasingly adopted in modern medical practice for precise and effective spinal tumor removal by utilizing small bone windows and multi-angled endoscopes to access and excise lesions that are challenging under a microscope [58]. Early pioneers like Burtscher and subsequent practitioners like Barami and Caballero-García have documented the successful applications of these methods, reporting excellent clinical outcomes across various studies and approaches [59,60,61]. The novel unilateral biportal endoscopy (UBE) technique in minimally invasive spinal surgery enhances instrument precision and view and is increasingly used for tumor treatments due to its flexibility, minimal trauma, and reduced pain [62,63]. It was first successfully applied to intradural extramedullary tumor excision by Kujur et al. [64].
Although intraoperative monitoring is commonly used during spine tumor surgeries without confirmed effectiveness through prospective trials, Kujur and colleagues’ analysis of surgeries performed without intraoperative nerve monitoring (IONM) highlighted its potential benefits in enhancing surgical safety by providing real-time spinal cord function assessment, contributing to safer procedures and improved resection outcomes [65]. However, the lack of validated procedures for responding to intraoperative alerts represents a significant gap that future research should address [66].
7. Alternative Treatment
Currently, robotic surgery is primarily used for precise screw placement in cases of spinal instability [67] and in hybrid surgeries involving extensive tumors extending into other cavities, as demonstrated by Iga et al., who combined spinal endoscopy with robot-assisted intrathoracic surgery using the da Vinci robot for a dumbbell-shaped tumor [68].
Radiation therapy is a viable option for managing spinal cord neoplasms especially when facing unresectable lesions or residual disease post-surgery, or in cases where surgery is contraindicated due to medical comorbidities, performance status, lesion location, or rapidly recurring/progressive tumors [69]. Several studies have explored the use of stereotactic radiation therapy (SRT) or stereotactic radiosurgery (SRS) for the treatment of intradural extramedullary (IDEM) tumors, with generally positive outcomes and few transient complications reported.
Adjuvant chemotherapy plays a very limited role in benign spinal tumor treatment. Several studies evaluating various medical approaches aimed at inhibiting or stabilizing tumor growth were unable to show any clinical benefits for patients. Chemotherapy drugs may be utilized in the management of advanced or unresectable tumors, as shown specifically in [53]. Thus, adjuvant chemotherapy is not included in the standard therapy, regardless of the tumor’s location. The current literature lacks evidence supporting chemotherapy for benign glomus tumors, with no reported cases of malignant transformation or metastases in spinal canal glomangiomas. Hsieh et al. described a complex case involving uncertain malignancy and extensive penetration at the cervical level, requiring multiple rounds of radiotherapy [70]. In contrast, Hsieh reported no recurrence in a similar uncertain case, and Nagata documented long-term survival despite reoperation for a recurrent dumbbell-shaped tumor [71,72]. While glomus tumors in the spine have not progressed to malignancy, they have in other organs where systematic chemotherapy, particularly with agents like doxorubicin or ifosfamide, is advised despite unclear sensitivity. The PALETTE study found pazopanib effective in some sarcoma types but not in malignant glomus tumors [73,74]. Du et al. reported significant benefits from a genetically guided treatment combining Anlotinib and Tislelizumab for an esophageal MGT with metastases [74].
In summary, glomangiomas are uncommon soft tissue tumors, with spinal canal involvement being excitingly rare. Typically benign and slow-growing, similar to other tumors in this location, they predominantly present with local pain and neurological deficits resulting from spinal cord and nerve root compression. Despite limited documentation in the available literature, intradural glomangiomas have not been reported until now. However, the presented case highlights their potential presence within the dural sac. Regardless of location, complete surgical resection remains the preferred treatment, with minimally invasive approaches favored when feasible. Efforts are also underway to utilize robotic surgery or augmented reality to enhance surgical outcomes in spinal tumor treatment. Stereotactic surgery is a valuable option for cases where complete tumor removal is not possible or if the patient’s medical condition precludes surgery. Adjuvant chemotherapy or immunotherapy may be considered for tumors exhibiting malignant characteristics.
Author Contributions
Conceptualization, W.C. and J.L.; methodology, W.C. and P.P.; software, M.T.; validation, G.T., K.T. and G.S.; formal analysis, W.C. and M.T.; investigation, W.C., J.L., L.B. and P.P.; resources, L.B.; data curation, L.B., writing—original draft preparation, W.C., B.P. and P.P.; writing—review and editing, W.C.; visualization, M.T.; supervision, G.T.; project administration, K.T.; funding acquisition, G.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Intramedullary Spinal Cord Tumors—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/28723060/ (accessed on 22 April 2024).
- Kumar, N.; Tan, W.L.B.; Wei, W.; Vellayappan, B.A. An Overview of the Tumors Affecting the Spine—Inside to Out. Neurooncol. Pract. 2020, 7 (Suppl. S1), i10. [Google Scholar] [CrossRef]
- Patel, P.; Mehendiratta, D.; Bhambhu, V.; Dalvie, S. Clinical Outcome of Intradural Extramedullary Spinal Cord Tumors: A Single-Center Retrospective Analytical Study. Surg. Neurol. Int. 2021, 12, 145. [Google Scholar] [CrossRef]
- Júnior, E.C.S.; Dantas, F.; Caires, A.C.V.; Cariri, G.A.; Reis, M.T.D.; Botelho, R.V.; Dantas, F.L.R. Evaluation of Surgically Treated Primary Spinal Cord Tumors in a Single Brazilian Institution: A Case Series Study of 104 Patients. Cureus 2022, 14, e23408. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, H.S.; Yoon, Y.C.; Cha, M.J.; Lee, S.H.; Kim, E.S. Differentiating between Spinal Schwannomas and Meningiomas Using MRI: A Focus on Cystic Change. PLoS ONE 2020, 15, e0233623. [Google Scholar] [CrossRef]
- Montemurro, N.; Lorenzini, D.; Ortenzi, V.; Giorgetti, J. Stretched Intradural Extramedullary Tanycytic Ependymoma of the Thoracic Spine. Surg. Neurol. Int. 2022, 13, 426. [Google Scholar] [CrossRef]
- Chen, C.W.; Chen, I.H.; Hu, M.H.; Lee, J.C.; Huang, H.Y.; Hong, R.L.; Yang, S.H. Primary Intradural Extramedullary Spinal Mesenchymal Chondrosarcoma: Case Report and Literature Review. BMC Musculoskelet. Disord. 2019, 20, 408. [Google Scholar] [CrossRef]
- Primary Intradural Extramedullary Malignant Melanoma in the Thoracic Spine: Case Report and Literature Review. Available online: https://www.e-neurospine.org/journal/view.php?number=353 (accessed on 23 April 2024).
- Intradural Extramedullary Malignant Tumors | Clinical Gate. Available online: https://clinicalgate.com/intradural-extramedullary-malignant-tumors/ (accessed on 23 April 2024).
- Izubuchi, Y.; Nakajima, H.; Honjoh, K.; Imamura, Y.; Nojima, T.; Matsumine, A. Primary Intradural Extramedullary Ewing Sarcoma: A Case Report and Literature Review. Oncol. Lett. 2020, 20, 2347–2355. [Google Scholar] [CrossRef]
- Palmisciano, P.; Chen, A.L.; Sharma, M.; Bin-Alamer, O.; Ferini, G.; Umana, G.E.; Aoun, S.G.; Haider, A.S. Intradural Extramedullary Spinal Metastases from Non-Neurogenic Primary Tumors: A Systematic Review. Anticancer. Res. 2022, 42, 3251–3259. [Google Scholar] [CrossRef]
- Jung, Y.-J.; Kim, S.-W.; Chang, C.-H.; Cho, S.-H. Intradural Extramedullary Non-Infiltrated Solitary Metastatic Tumor. J. Korean Neurosurg. Soc. 2005, 37, 466–468. [Google Scholar]
- Litak, J.; Czyżewski, W.; Szymoniuk, M.; Sakwa, L.; Pasierb, B.; Litak, J.; Hoffman, Z.; Kamieniak, P.; Roliński, J. Biological and Clinical Aspects of Metastatic Spinal Tumors. Cancers 2022, 14, 4599. [Google Scholar] [CrossRef]
- Szymoniuk, M.; Litak, J.; Sakwa, L.; Dryla, A.; Zezuliński, W.; Czyżewski, W.; Kamieniak, P.; Blicharski, T. Molecular Mechanisms and Clinical Application of Multipotent Stem Cells for Spinal Cord Injury. Cells 2022, 12, 120. [Google Scholar] [CrossRef]
- Srinivas, R.; Shanker, M.M.; Naleer, M. Intradural Extra Medullary Spinal Tumours—An Urban Institute’s Experience. Interdiscip. Neurosurg. 2023, 34, 101819. [Google Scholar] [CrossRef]
- Ariyaratne, S.; Jenko, N.; Iyengar, K.P.; James, S.; Mehta, J.; Botchu, R. Primary Benign Neoplasms of the Spine. Diagnostics 2023, 13, 2006. [Google Scholar] [CrossRef]
- Choi, J.H.; Ro, J.Y. Epithelioid Cutaneous Mesenchymal Neoplasms: A Practical Diagnostic Approach. Diagnostics 2020, 10, 233. [Google Scholar] [CrossRef]
- Szmyd, B.; Malicki, M.; Błaszczyk, M.; Karuga, F.F.; Braun, M.; Sołek, J.; Jabbar, R.; Jankowski, J.; Wysiadecki, G.; Radek, M. Glomangioma in the Hand: Diagnosis, Treatment, and Challenges. Neurol. Neurochir. Pol. 2023, 57, 387–391. [Google Scholar] [CrossRef]
- Kalekar, T.; Rangankar, V.; Ayapaneni, D.R.; Chanabasanavar, V.; Dhirawani, S. Multiple Paragangliomas in the Carotid Body, Adrenal and Extra-Adrenal Retroperitoneal Locations. Cureus 2021, 13, e18258. [Google Scholar] [CrossRef]
- Yeom, J.A.; Jeong, Y.J.; Ahn, H.Y.; Eom, J.S.; Lee, C.H.; Hwang, M.H. Tracheal Glomus Tumor: A Case Report with CT Imaging Features. Medicina 2022, 58, 791. [Google Scholar] [CrossRef]
- Shinohara, T.; Hirata, H. Glomus Tumor Originating from a Digital Nerve. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2053. [Google Scholar] [CrossRef]
- Serrano-Novillo, C.; Oliveras, A.; Ferreres, J.C.; Condom, E.; Felipe, A. Remodeling of Kv7.1 and Kv7.5 Expression in Vascular Tumors. Int. J. Mol. Sci. 2020, 21, 6019. [Google Scholar] [CrossRef]
- Mravic, M.; LaChaud, G.; Nguyen, A.; Scott, M.A.; Dry, S.M.; James, A.W. Clinical and Histopathological Diagnosis of Glomus Tumor: An Institutional Experience of 138 Cases. Int. J. Surg. Pathol. 2015, 23, 181. [Google Scholar] [CrossRef]
- Bedoui, Y.; Lebeau, G.; Guillot, X.; Dargai, F.; Guiraud, P.; Neal, J.W.; Ralandison, S.; Gasque, P. Emerging Roles of Perivascular Mesenchymal Stem Cells in Synovial Joint Inflammation. J. Neuroimmune Pharmacol. 2020, 15, 838–851. [Google Scholar] [CrossRef] [PubMed]
- Girolamo, F.; de Trizio, I.; Errede, M.; Longo, G.; d’Amati, A.; Virgintino, D. Neural Crest Cell-Derived Pericytes Act as pro-Angiogenic Cells in Human Neocortex Development and Gliomas. Fluids Barriers CNS 2021, 18, 14. [Google Scholar] [CrossRef] [PubMed]
- Mizutani, K.-I.; Kidoya, H.; Nakayama, K.; Hattori, Y. The Multiple Roles of Pericytes in Vascular Formation and Microglial Functions in the Brain. Life 2022, 12, 1835. [Google Scholar] [CrossRef] [PubMed]
- de Picoli, C.C.; Birbrair, A.; Li, Z. Pericytes as the Orchestrators of Vasculature and Adipogenesis. Genes 2024, 15, 126. [Google Scholar] [CrossRef]
- El Ali, A.; Thériault, P.; Rivest, S. The Role of Pericytes in Neurovascular Unit Remodeling in Brain Disorders. Int. J. Mol. Sci. 2014, 15, 6453–6474. [Google Scholar] [CrossRef] [PubMed]
- Czyżewski, W.; Mazurek, M.; Sakwa, L.; Szymoniuk, M.; Pham, J.; Pasierb, B.; Litak, J.; Czyżewska, E.; Turek, M.; Piotrowski, B.; et al. Astroglial Cells: Emerging Therapeutic Targets in the Management of Traumatic Brain Injury. Cells 2024, 13, 148. [Google Scholar] [CrossRef]
- Supakul, S.; Yao, K.; Ochi, H.; Shimada, T.; Hashimoto, K.; Sunamura, S.; Mabuchi, Y.; Tanaka, M.; Akazawa, C.; Nakamura, T.; et al. Pericytes as a Source of Osteogenic Cells in Bone Fracture Healing. Int. J. Mol. Sci. 2019, 20, 1079. [Google Scholar] [CrossRef] [PubMed]
- Borroni, R.G.; Narula, N.; Diegoli, M.; Grasso, M.; Concardi, M.; Rosso, R.; Cerica, A.; Brazzelli, V.; Arbustini, E. A Novel Mutation of the Glomulin Gene in an Italian Family with Autosomal Dominant Cutaneous Glomuvenous Malformations. Exp. Dermatol. 2011, 20, 1032–1034. [Google Scholar] [CrossRef] [PubMed]
- Harrison, B.; Sammer, D. Glomus Tumors and Neurofibromatosis: A Newly Recognized Association. Plast. Reconstr. Surg. Glob. Open 2014, 2, e214. [Google Scholar] [CrossRef]
- Yanai, K.; Tajika, T.; Kuboi, T.; Hatori, Y.; Umeyama, T.; Arisawa, S.; Katayama, A.; Sano, T.; Chikuda, H. A Case of Solitary Digital Glomus Tumor Associated with Neurofibromatosis Type 1. SAGE Open Med. Case Rep. 2023, 11, 2050313X231193984. [Google Scholar] [CrossRef]
- Brems, H.; Park, C.; Maertens, O.; Pemov, A.; Messia, L.; Upadhyaya, M.; Claes, K.; Beert, E.; Peeters, K.; Mautner, V.; et al. Glomus Tumors in Neurofibromatosis Type 1: Genetic, Functional and Clinical Evidence of a Novel Association. Cancer Res. 2009, 69, 7393. [Google Scholar] [CrossRef] [PubMed]
- Dabek, B.; Kram, A.; Kubrak, J.; Kurzawski, M.; Wojcik, P.; Machnicki, M.M.; Stoklosa, T.; Rydzanicz, M.; Ploski, R.; Debiec-Rychter, M. A Rare Mutation in a Rare Tumor--SMARCB1-Deficient Malignant Glomus Tumor. Genes Chromosomes Cancer 2016, 55, 107–109. [Google Scholar] [CrossRef]
- Iwamura, R.; Komatsu, K.; Kusano, M.; Kubo, C.; Inaba, Y.; Shiba, E.; Nawata, A.; Tajiri, R.; Matsuyama, A.; Matoba, H.; et al. PDGFRB and NOTCH3 Mutations Are Detectable in a Wider Range of Pericytic Tumors, Including Myopericytomas, Angioleiomyomas, Glomus Tumors, and Their Combined Tumors. Mod. Pathol. 2023, 36, 100070. [Google Scholar] [CrossRef]
- Lin, J.; Luo, J.; Chen, H.; Li, Z.; Shi, Y.; Sun, H.; Zhang, Z.; Zhou, G.; Zhong, D. Clinicopathologic Features and BRAF Mutation Status of Tracheal Glomus Tumors—Characterization of 4 Cases and the Distinction from Low-Grade Neuroendocrine Tumors. Ann. Diagn. Pathol. 2021, 55, 151797. [Google Scholar] [CrossRef]
- Mosquera, J.M.; Sboner, A.; Zhang, L.; Chen, C.L.; Sung, Y.S.; Chen, H.W.; Agaram, N.P.; Briskin, D.; Basha, B.M.; Singer, S.; et al. Novel MIR143-NOTCH Fusions in Benign and Malignant Glomus Tumors. Genes Chromosomes Cancer 2013, 52, 1075–1087. [Google Scholar] [CrossRef] [PubMed]
- Saba, M.; Moser, A.; Rosenberg, J.; Qiao, J.H.; Chen, G. Rare Glomus Tumor Formation Following Trauma to the First Digit. Int. J. Surg. Case Rep. 2021, 86, 106324. [Google Scholar] [CrossRef]
- Lıu, T.; Zou, W.; Kong, J.; Han, S.; Wang, T.; Yan, W.; Xıao, J.; Liu, T. Turk Embolization in the Treatment of an Intraosseous Glomus Tumor in the Upper Thoracic Spine Complicating Compression Myelopathy: A Case Report and A Literature Review Kompresyon Miyelopatisi Ile Komplike Olan Üst Torasik Omurga İntraosseöz Glomus Tümörü Tedavisinde Embolizasyon: Bir Olgu Sunumu ve Literatür Derlemesi. Neurosurg 2015, 25, 479–484. [Google Scholar] [PubMed]
- Cohen, P.R. Glomus Extradigital Tumor: A Case Report of an Extradigital Glomus Tumor on the Wrist and Comprehensive Review of Glomus Tumors. Cureus 2023, 15, e38737. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Qi, R.; Wu, Z.; Zhang, X.; Niu, J. The Clinicopathologic and Immunohistochemical Features of 60 Cutaneous Glomus Tumor: A Retrospective Case Series Study. An. Bras. Dermatol. 2024, 99, 238–243. [Google Scholar] [CrossRef]
- Li, X.; Zheng, J. Extradural Glomus Tumor of the Thoracic Spine: Case Report and Review of the Literature. Ann. Palliat. Med. 2021, 10, 9309317. [Google Scholar] [CrossRef]
- Zheng, Y.; Liu, X.; Mao, Y.; Lin, M. Glomus Tumor of the Crissum: A Case Report and Review of Literature. Indian. J. Pathol. Microbiol. 2022, 65, 164–166. [Google Scholar]
- Lee, W.Q.; Li, Y.; Yeo, N.E.M. Glomus Tumour: An Institutional Experience of 31 Cases. J. Orthop. Surg. Res. 2023, 18, 741. [Google Scholar] [CrossRef]
- Lee, M.W.; Lee, J.Y.; Park, S.M. Solitary Glomangioma on the Chin: A Rare Case Report. Oral. Maxillofac. Surg. Cases 2022, 8, 100248. [Google Scholar] [CrossRef]
- Almaghrabi, A.; Almaghrabi, N.; Al-Maghrabi, H. Glomangioma of the Kidney: A Rare Case of Glomus Tumor and Review of the Literature. Case Rep. Pathol. 2017, 2017, 1–7. [Google Scholar] [CrossRef]
- Chalise, S.; Jha, A.; Neupane, P.R. Glomangiomyoma of Uncertain Malignant Potential in the Urinary Bladder: A Case Report. JNMA J. Nepal. Med. Assoc. 2021, 59, 719–722. [Google Scholar] [CrossRef] [PubMed]
- Reha Çelik, M.; Şahin, N.; Akatli, A.N.; Ulutaş, H. Primary Pulmonary Glomangioma. Turk. J. Thorac. Cardiovasc. Surg. 2017, 25, 140–143. [Google Scholar] [CrossRef][Green Version]
- Lin, J.; Shen, J.; Yue, H.; Li, Q.; Cheng, Y.; Zhou, M. Gastric Glomus Tumor: A Clinicopathologic and Immunohistochemical Study of 21 Cases. Biomed. Res. Int. 2020, 2020, 5637893. [Google Scholar] [CrossRef]
- Choi, J.H.; Ro, J.Y. The 2020 WHO Classification of Tumors of Soft Tissue: Selected Changes and New Entities. Adv Anat Pathol 2021, 28, 44–58. [Google Scholar] [CrossRef] [PubMed]
- Costăchescu, B.; Niculescu, A.G.; Iliescu, B.F.; Dabija, M.G.; Grumezescu, A.M.; Rotariu, D. Current and Emerging Approaches for Spine Tumor Treatment. Int. J. Mol. Sci. 2022, 23, 15680. [Google Scholar] [CrossRef]
- Liao, Z.; Chen, C.; Wang, B.; Yang, C. Minimally Invasive Resection of a Glomus Tumor of the Thoracic Spine: A Case Report and Literature Review. J. Int. Med. Res. 2019, 47, 2746. [Google Scholar] [CrossRef]
- Bielewicz, J.; Kamieniak, M.; Szymoniuk, M.; Litak, J.; Czyżewski, W.; Kamieniak, P. Diagnosis and Management of Neuropathic Pain in Spine Diseases. J. Clin. Med. 2023, 12, 1380. [Google Scholar] [CrossRef] [PubMed]
- Bhimani, A.D.; Denyer, S.; Esfahani, D.R.; Zakrzewski, J.; Aguilar, T.M.; Mehta, A.I. Surgical Complications in Intradural Extramedullary Spinal Cord Tumors—An ACS-NSQIP Analysis of Spinal Cord Level and Malignancy. World Neurosurg. 2018, 117, e290–e299. [Google Scholar] [CrossRef] [PubMed]
- Karhade, A.V.; Vasudeva, V.S.; Dasenbrock, H.H.; Lu, Y.; Gormley, W.B.; Groff, M.W.; Chi, J.H.; Smith, T.R. Thirty-Day Readmission and Reoperation after Surgery for Spinal Tumors: A National Surgical Quality Improvement Program Analysis. Neurosurg. Focus. 2016, 41, E5. [Google Scholar] [CrossRef]
- Jang, J.W.; Lee, D.G.; Park, C.K. Rationale and Advantages of Endoscopic Spine Surgery. Int. J. Spine Surg. 2021, 15 (Suppl. S3), S11. [Google Scholar] [CrossRef] [PubMed]
- Barami, K.; Dagnew, E. Endoscope-Assisted Posterior Approach for the Resection of Ventral Intradural Spinal Cord Tumors: Report of Two Cases. Minim. Invasive Neurosurg. 2007, 50, 370–373. [Google Scholar] [CrossRef] [PubMed]
- Caballero-García, J.; Linares-Benavides, Y.J.; Leitão, U.L.S.; Aparicio-García, C.; López-Sánchez, M. Minimally Invasive Removal of Extra- and Intradural Spinal Tumors Using Full Endoscopic Visualization. Glob. Spine J. 2022, 12, 121. [Google Scholar] [CrossRef]
- Şentürk, S.; Ünsal, Ü.Ü. Percutaneous Full-Endoscopic Removal of Lumbar Intradural Extramedullary Tumor via Translaminar Approach. World Neurosurg. 2019, 125, 146–149. [Google Scholar] [CrossRef]
- Wang, T.; Yu, H.; Zhao, S.B.; Zhu, B.; Chen, L.; Jing, J.H.; Tian, D.S. Complete Removal of Intraspinal Extradural Mass with Unilateral Biportal Endoscopy. Front. Surg. 2022, 9, 1033856. [Google Scholar] [CrossRef] [PubMed]
- Pao, J.L.; Lin, S.M.; Chen, W.C.; Chang, C.H. Unilateral Biportal Endoscopic Decompression for Degenerative Lumbar Canal Stenosis. J. Spine Surg. 2020, 6, 438. [Google Scholar] [CrossRef]
- Peng, W.; Zhuang, Y.; Cui, W.; Chen, W.; Chu, R.; Sun, Z.; Zhang, S. Unilateral Biportal Endoscopy for the Resection of Thoracic Intradural Extramedullary Tumors: Technique Case Report and Literature Review. Int. Med. Case Rep. J. 2024, 17, 301. [Google Scholar] [CrossRef]
- Kujur, N.; Rao, S.C.S.; Rajagopalawarrier, B. Intradural Extramedullary Spinal Tumors: A Clinical Study and Management without the Aid of Nerve Monitoring. J. Spinal Surg. 2024, 11, 8–12. [Google Scholar] [CrossRef]
- Charalampidis, A.; Jiang, F.; Wilson, J.R.F.; Badhiwala, J.H.; Brodke, D.S.; Fehlings, M.G. The Use of Intraoperative Neurophysiological Monitoring in Spine Surgery. Global Spine J. 2020, 10 (Suppl. S1), 104S. [Google Scholar] [CrossRef] [PubMed]
- Amin, A.G.; Barzilai, O.; Bilsky, M.H. CT-Based Image-Guided Navigation and the DaVinci Robot in Spine Oncology: Changing Surgical Paradigms. HSS J. 2021, 17, 294–301. [Google Scholar] [CrossRef] [PubMed]
- Iga, N.; Kono, M.; Tomioka, Y.; Yamane, M. Combined Minimally Invasive Surgery for a Dumbbell Tumor Using Spinal Endoscopy and Robot-Assisted Intrathoracic Surgery: A Case Report. Ann. Jt. 2023, 8. [Google Scholar] [CrossRef]
- Xiao, Y.; Wang, Y.; Wei, F.; Zhuang, H. Long-Term Follow-up Results of Spine Tumor Treatment Using High-Dose Radiotherapy after 3-Dimensional-Printed Vertebral Bodies Implantation. Cancer Med. 2023, 12, 11483–11490. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Su, K.; Li, M.; Lu, S.; Che, Z.; Liang, Y.; Huang, L. Glomus Tumor of Uncertain Malignant Potential within the Cervical Spine: A Case Report. Ann. Palliat. Med. 2021, 10, 120182024-120112024. [Google Scholar] [CrossRef] [PubMed]
- Glomangioma at the Cervical Spine as an Extradural Dumbbell-Shaped Tumor—A Case Report—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/12197433/ (accessed on 18 April 2024).
- Nagata, K.; Hashizume, H.; Yamada, H.; Yoshida, M. Long-Term Survival Case of Malignant Glomus Tumor Mimicking “Dumbbell-Shaped” Neurogenic Tumor. Eur. Spine J. 2017, 26 (Suppl. S1), S42–S46. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, K.; Endo, M.; Fukushima, S.; Hirose, T.; Nabeshima, A.; Fujiwara, T.; Oda, Y.; Nakashima, Y. Metastatic Malignant Glomus Tumor Resistant to Pazopanib, a Multikinase Inhibitor: A Case Report and Review of Literature. In JOS Case Reports; Elsevier: Amsterdam, The Netherlands, 2024. [Google Scholar] [CrossRef]
- Wolter, N.E.; Adil, E.; Irace, A.L.; Werger, A.; Perez-Atayde, A.R.; Weldon, C.; Orbach, D.B.; Rodriguez-Galindo, C.; Rahbar, R. Malignant Glomus Tumors of the Head and Neck in Children and Adults: Evaluation and Management. Laryngoscope 2017, 127, 2873–2882. [Google Scholar] [CrossRef]
- Du, W.; Liu, Y.; Mao, J.; Shen, D.; Jin, B.; Wu, X. Combined Treatment for a Rare Malignant Glomus Tumor of the Esophagus with Pulmonary and Liver Metastases: A Case Report and Review of Literature. Front. Oncol. 2024, 14, 1340859. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).