4.1. Analysis of Findings
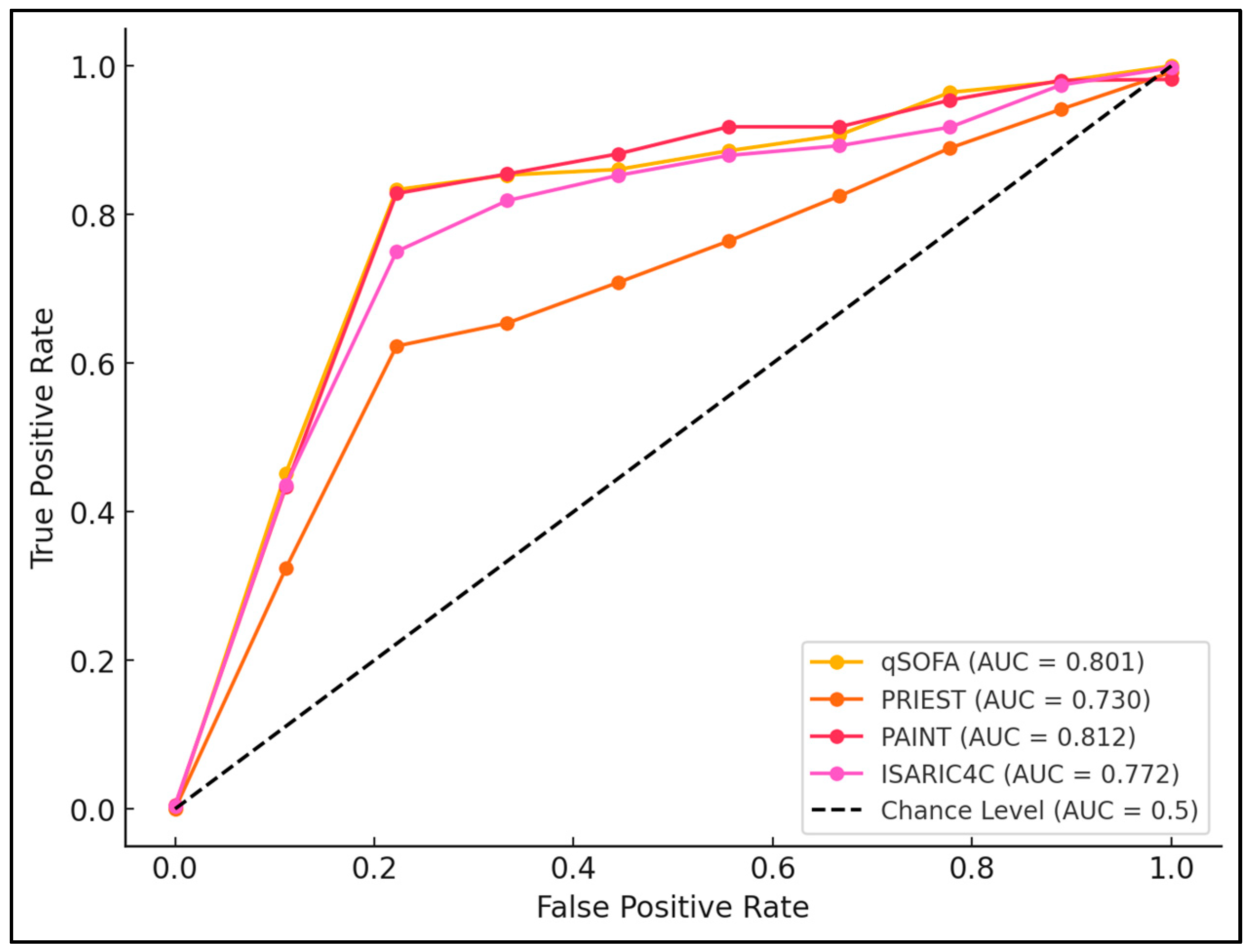
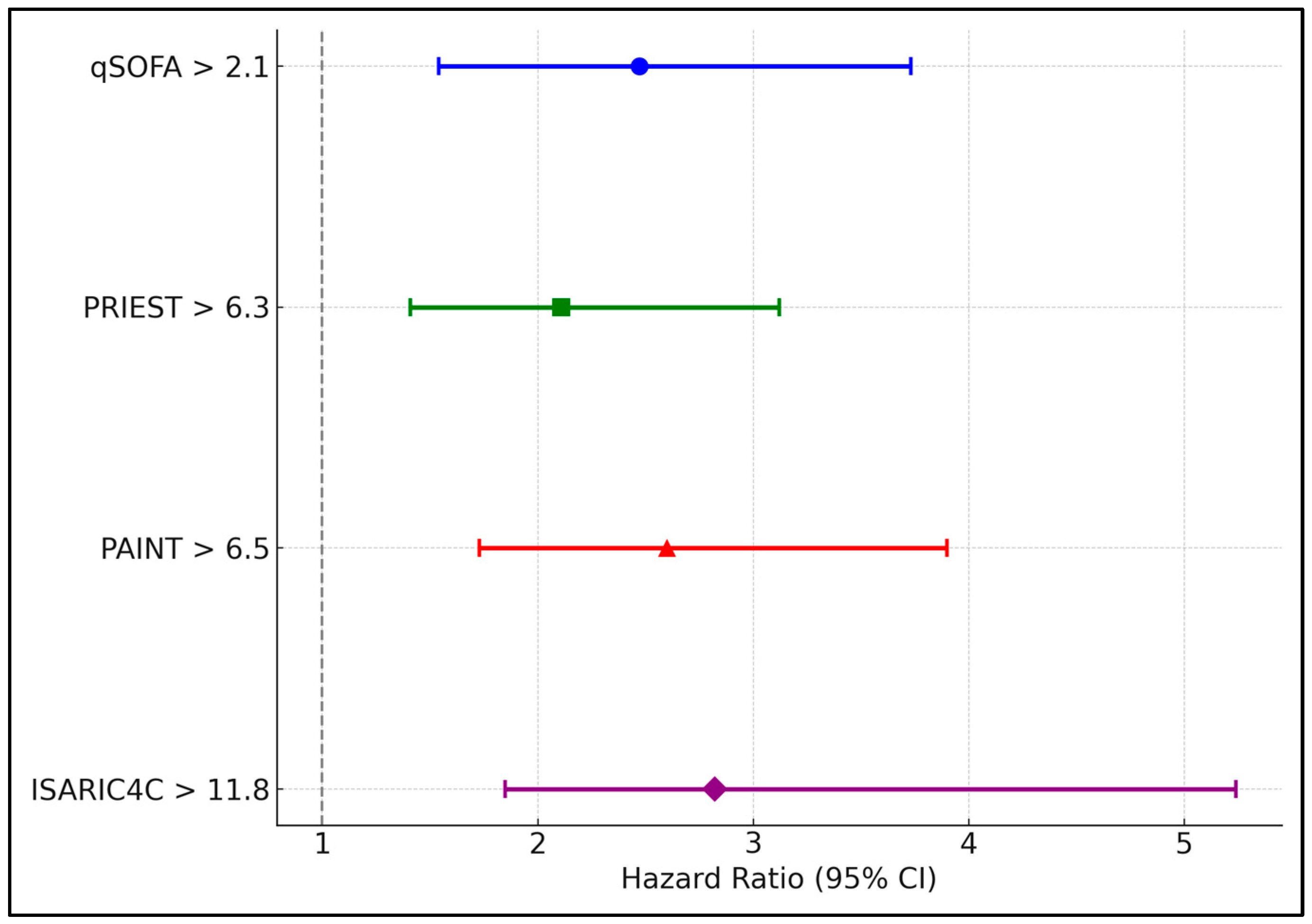
The findings from this study underscore the critical role of clinical scoring systems like ISARIC4C, qSOFA, PRIEST, and PAINT in the management and risk stratification of elderly COVID-19 patients. These scores serve not only as indicators of current patient status but also as prognostic tools that can predict the trajectory of COVID-19 complications. The ISARIC4C score emerged as a notably robust predictor, exhibiting the highest sensitivity and specificity for severe outcomes, including mortality. This could be attributed to the comprehensive factors included in the ISARIC4C scoring, which encompass a wider range of clinical symptoms and biomarkers compared to the more focused parameters of qSOFA and PRIEST. The broad spectrum of clinical variables considered by ISARIC4C may capture the complex pathology of COVID-19 more effectively, particularly in a population that is already vulnerable due to age and comorbidities.
Moreover, the utility of qSOFA and PRIEST in this setting prompts a discussion about their applicability across different clinical environments and populations. qSOFA, originally developed for quick sepsis evaluation, has shown its adaptability in gauging severity in other systemic infections, such as COVID-19, highlighting its potential as a universal triage tool in emergency settings. However, its performance, while significant, was not as pronounced as ISARIC4C, suggesting that while useful, qSOFA may require adjunctive scoring systems to improve accuracy in specific patient subsets [
25,
26]. Similarly, the PRIEST score, which is tailored more towards a general emergency presentation, reaffirms the need for specialized scores in managing elderly populations where typical presentations of diseases may be absent or altered.
The role of the PAINT score in this analysis also sheds light on the evolving landscape of clinical scoring systems. As newer scores like PAINT are developed and validated, there is a potential for them to be refined and perhaps even combined with traditional scores to enhance predictive accuracy and clinical utility. Integrating machine learning algorithms with these scoring systems could potentially offer real-time predictive analytics, improving outcome predictions and enabling personalized patient management strategies. Moving forward, it will be essential to validate the effectiveness of these scores in other cohorts and to assess their performance in prospective studies to ensure they can reliably inform clinical decisions and improve patient outcomes across diverse healthcare settings.
In a similar manner, the study conducted by Heydari et al. [
27] involved 894 patients presenting to the emergency department, where the AUROC for qSOFA was 0.799, demonstrating good predictive value for COVID-19 mortality comparable to CURB-65 (0.829) and PSI (0.830) but superior to SIRS (0.759). The demographic data indicated that non-surviving patients were significantly older and had more comorbidities than surviving ones. In a similar manner, the study by Liu et al. [
21], which included 140 critically ill COVID-19 patients, found that SOFA, with an AUROC of 0.890, outperformed qSOFA, which had an AUROC of 0.742. This suggests a higher predictive accuracy for SOFA in a critical care setting. While both qSOFA and SOFA are validated tools for predicting mortality, their performance varies significantly with the severity of the patient’s condition upon admission, underlining the importance of choosing an appropriate assessment tool based on patient acuity.
Similarly, Julio Alencar and colleagues investigated the efficacy of SIRS, qSOFA, and NEWS scores for predicting mortality, bacterial infection, and ICU admission among 2473 COVID-19 patients at a major Brazilian hospital [
28]. Their findings showed poor performance of the SIRS and qSOFA scores but high sensitivity of the NEWS score in predicting in-hospital death (0.851), early bacterial infection (0.851), and ICU admission (0.868), despite its low specificity. In a similar manner, a study by Cosmin Citu et al. [
29] evaluated the predictive value of SOFA and qSOFA scores for in-hospital mortality among 133 patients in Romania, revealing both scores as excellent predictors of mortality with ROC-AUC values of 0.800 for SOFA and 0.794 for qSOFA. Notably, regression analysis indicated that every one-point increase in the SOFA score increased the mortality risk by 1.82 and in the qSOFA score by 5.23.
Another study conducted an extensive assessment of seven risk stratification tools, including NEWS2, PRIEST, and PMEWS, in the Western Cape, South Africa [
30]. Among 446,084 patients, 3.45% experienced severe outcomes such as intubation, non-invasive ventilation, death, or ICU admission within 30 days. The tools showed moderate sensitivity and specificity, with a notable clinical decision-making accuracy for inpatient admission marked by a sensitivity of 0.77 and a specificity of 0.88. Despite good estimated discrimination (C-statistic between 0.79 and 0.82), the practical application at recommended thresholds would have significantly increased admissions with minimal reduction in false negatives. In a similar manner, the study by Suh et al. [
31] evaluated the modified PRIEST score (mPRIEST) in two New York City EDs, demonstrating that this tool effectively identified patients at very low risk of adverse outcomes, such as death or mechanical ventilation, with a sensitivity of 97.7% for those above the threshold value. The mPRIEST study, though smaller with outcomes available for only 306 patients, suggested strong potential for bedside application in identifying low-risk patients, contrasting with Marincowitz’s findings where the practical utility in reducing admissions was limited.
Regarding the ISARIC4C score, the studies by Joshua M. Riley [
32] and Rehab Abd Elfattah Mohamed et al. [
33] critically evaluate the performance of the 4C Mortality Score in predicting COVID-19 mortality across different populations and settings. Riley’s study involved 426 patients in an urban United States setting, demonstrating the utility of the 4C Mortality Score with an area under the receiver operator characteristic curve (AUROC) of 0.85, indicating robust predictive capability in a diverse inpatient population (54.5% Black or African American). The study noted a mortality rate of 16.7% among the cohort, underscoring the score’s relevance in pre-vaccine era clinical decision making. In a similar manner, the study by Mohamed et al. in Saudi Arabia assessed the 4C Score’s accuracy among a mixed group of 506 home-isolated and hospitalized COVID-19 patients. Their findings revealed a model with 71% sensitivity and 88.6% specificity, with an AUROC of 0.9. This study also identified hypoxia, high respiratory rate, C-reactive protein, and blood urea nitrogen as significant predictors of mortality within the model, suggesting that these factors are crucial in mortality risk stratification.
The study findings highlight that comorbidities significantly contribute to the poorer outcomes observed in the elderly population compared to younger patients following COVID-19. The most impactful contributors include higher rates of chronic health conditions, as evidenced by the CCI scores, with 65.65% of elderly patients having a CCI > 2 compared to 31.42% in younger patients (p < 0.001). Renal dysfunction, reflected in elevated blo BUN and creatinine levels, as well as impaired respiratory function indicated by lower oxygen saturation and PaO2/FiO2 ratios, were more pronounced in the elderly group. These physiological differences align with elevated clinical scores, such as qSOFA, PRIEST, and ISARIC4C, which further emphasize the greater severity of disease in older adults. The presence of these comorbidities, combined with frailty and reduced physiological reserves, underscores their substantial role in driving worse outcomes, including higher rates of ICU admission and mortality among the elderly.
The clinical utility of these findings is significant, particularly for healthcare settings managing elderly populations vulnerable to severe COVID-19. The demonstration that scores like ISARIC4C, qSOFA, PRIEST, and PAINT can predict severe outcomes means that healthcare providers can implement these tools for the early identification of high-risk patients, potentially directing more aggressive monitoring and therapeutic interventions sooner. For instance, higher scores at admission or the five-day mark could prompt earlier ICU admissions or the initiation of critical care interventions, thus potentially reducing mortality rates. This proactive approach could also facilitate better resource allocation within hospitals, ensuring that medical supplies and personnel are adequately prepared to handle cases likely to require intensive care. Furthermore, these scoring systems can be integrated into triage protocols, helping to streamline patient flow and prioritize treatment for those most likely to benefit from immediate care, thereby enhancing overall hospital efficiency and patient outcomes.