Cardiac Laterality: Surgical Results of Right Atrial Isomerism
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Statistical Analysis
3. Results
3.1. Demographic Characteristics
3.2. Surgical Characteristics
3.3. Early Results
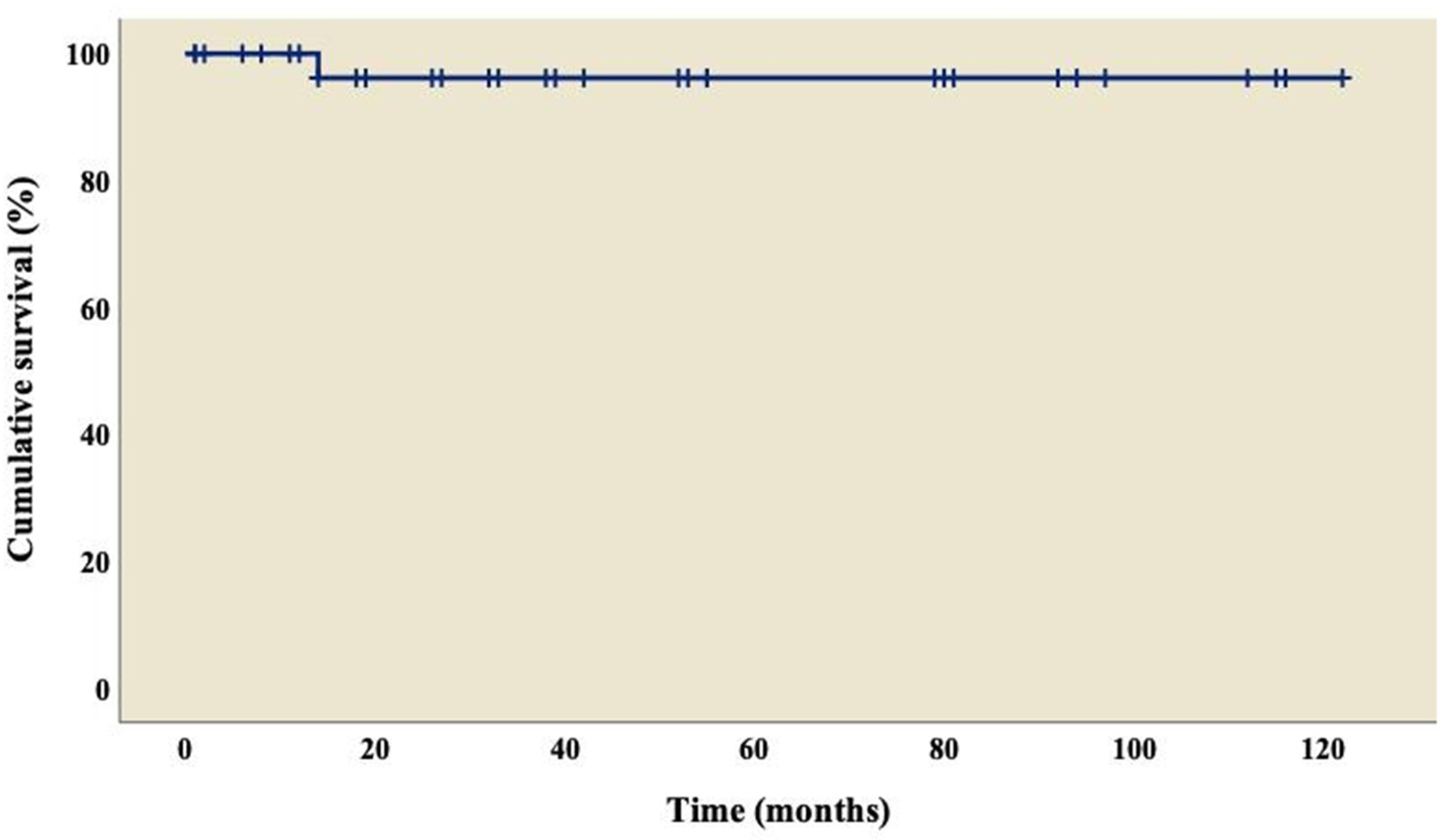
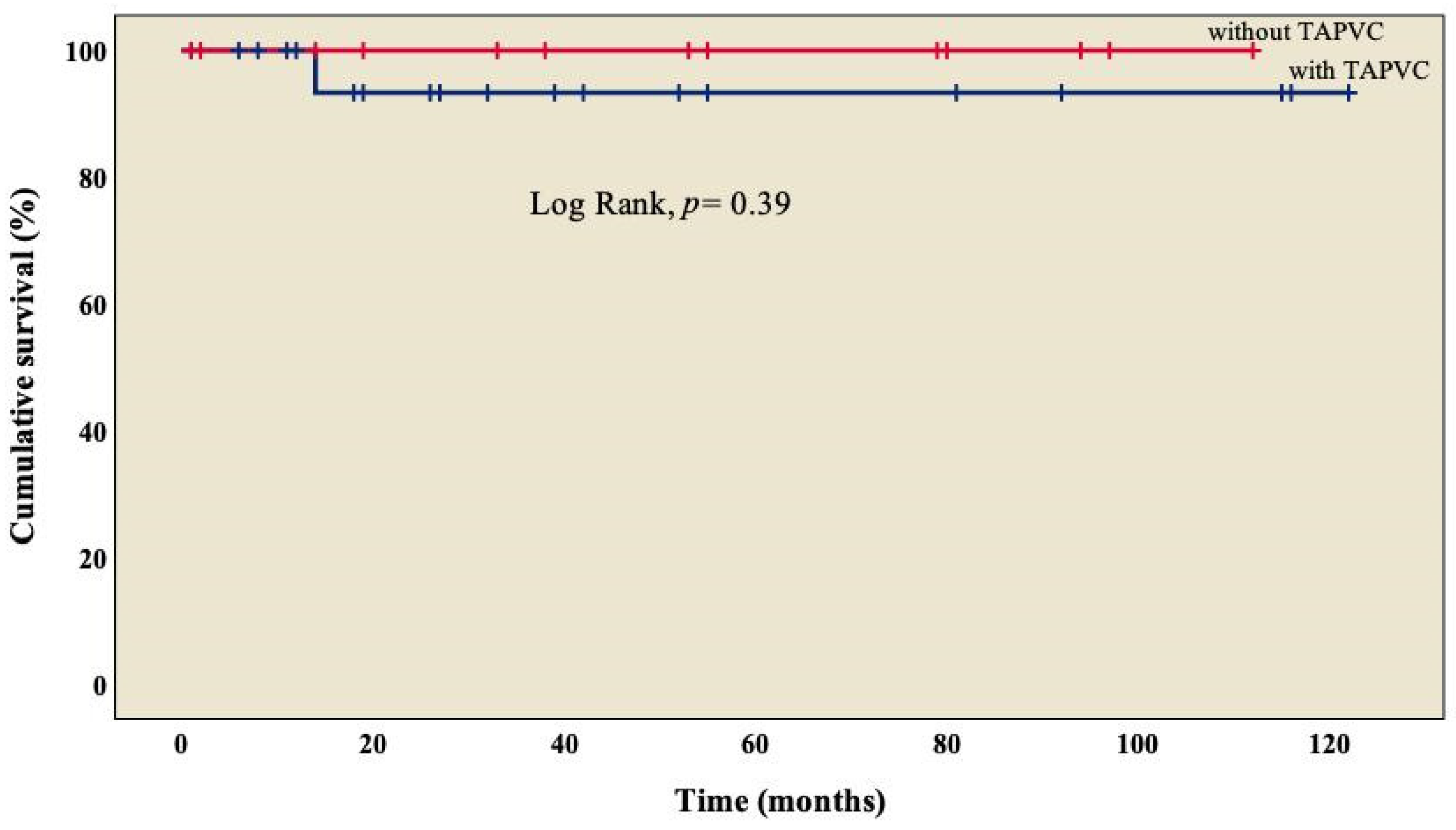
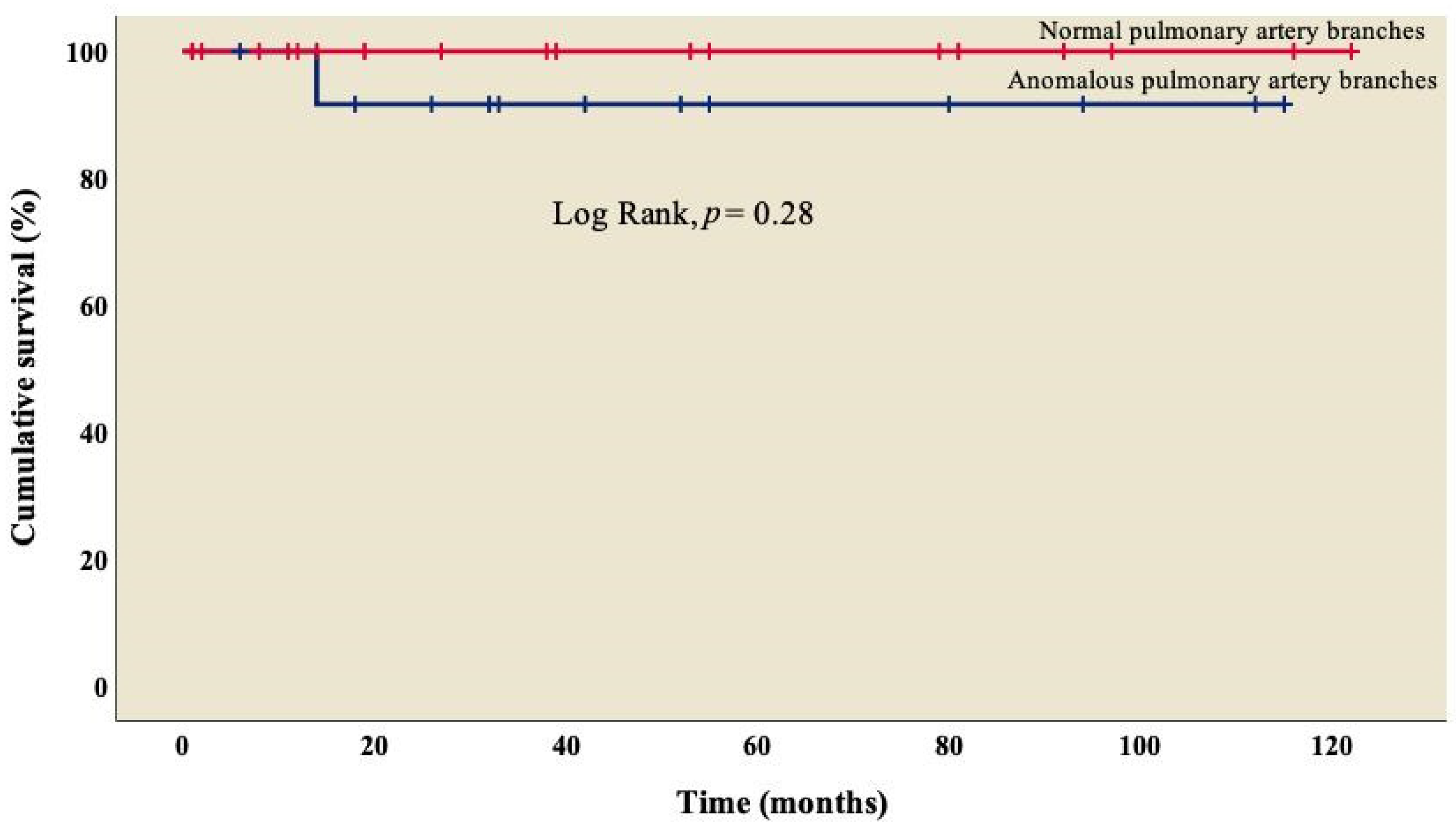
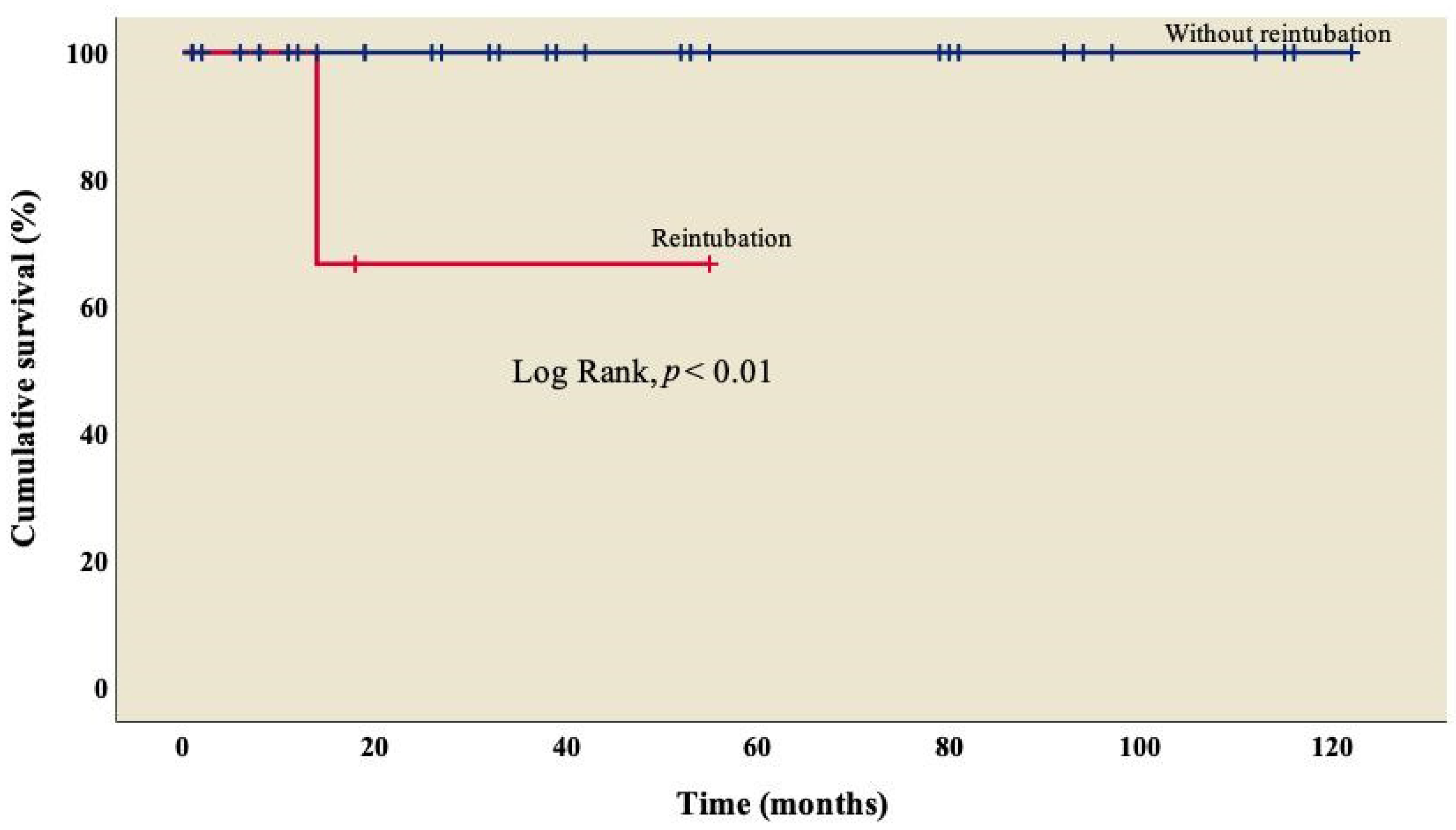
3.4. Follow-Up
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- García-Flores, E.; Calderón-Colmenero, J.; Borgonio-Cuadra, V.M.; Sandoval, J.P.; García-Montes, J.A.; Cazarín-Santos, B.G.; Miranda-Duarte, A.; Gamboa-Domínguez, A.; Rodríguez-Pérez, J.M.; Pérez-Hernández, N. Epigenetic Evaluation of the TBX20 Gene and Environmental Risk Factors in Mexican Paediatric Patients with Congenital Septal Defects. Cells 2023, 12, 586. [Google Scholar] [CrossRef]
- Monroy-Muñoz, I.E.; Pérez-Hernández, N.; Vargas-Alarcón, G.; Ortiz-San Juan, G.; Buendía-Hernández, A.; Calderón-Colmenero, J.; Ramírez-Marroquín, S.; Cervantes-Salazar, J.L.; Curi-Curi, P.; Martínez-Rodríguez, N.; et al. Cambiando el paradigma en las cardiopatías congénitas: De la anatomía a la etiología molecular [Changing the paradigm of congenital heart disease: From the anatomy to the molecular etiology]. Gac. Med. Mex. 2013, 149, 212–219. [Google Scholar]
- Icardo, J.M.; Rincón, J.M.G.; Ros, M.Á. Malformaciones cardíacas, heterotaxia y lateralidad. Rev. Esp. Cardiol. 2002, 55, 962–974. [Google Scholar] [CrossRef] [PubMed]
- Calderón-Colmenero, J.; Cervantes-Salazar, J.L.; Curi-Curi, P.J.; Ramírez-Marroquín, S. Problemática de las cardiopatías congénitas en México: Propuesta de regionalización [Congenital heart disease in Mexico. Regionalization proposal]. Arch. Cardiol. Mex. 2010, 80, 133–140. [Google Scholar] [PubMed]
- Cervantes-Salazar, J.; Calderón-Colmenero, J.; Ramírez-Marroquín, S.; Palacios-Macedo, A.; Cerdán, A.B.; Alarcón, A.V.; Curi-Curi, P.; de la Llata Romero, M.; Orellana, J.E.; Palacios, J.G. El Registro Mexicano de Cirugía Cardíaca Pediátrica. Primer informe. Evid. Med. Invest. Salud 2014, 7, 56–62. [Google Scholar]
- Madrigal, S.; Bonilla, C.; Sánchez, E. Heterotaxia: Situs ambiguo, síndrome de Ivermark o síndrome de asplenia-poliesplenia. Rev. Clín Esc. Med. UCR-HSJD 2019, 9, 70–76. [Google Scholar] [CrossRef]
- Sun, Y.; Wang, J.; Quan, X.; Zhang, M.; Zhang, L.; Wang, H. Right atrial isomerism in children older than 3 years. Springerplus 2016, 5, 1372. [Google Scholar]
- Kim, S.-J. Heterotaxy syndrome. Korean Circ. J. 2011, 41, 227–232. [Google Scholar] [CrossRef]
- Loomba, R.S.; Hlavacek, A.M.; Spicer, D.E.; Anderson, R.H. Isomerism or heterotaxy: Which term leads to better understanding? Cardiol. Young 2015, 25, 1037–1043. [Google Scholar] [CrossRef]
- Ramsdell, A.F. Left-right asymmetry and congenital cardiac defects: Getting to the heart of the matter in vertebrate left-right axis determination. Dev. Biol. 2005, 288, 1–20. [Google Scholar] [CrossRef]
- Blum, M.; Feistel, K.; Thumberger, T.; Schweickert, A. The evolution and conservation of left-right patterning mechanisms. Development 2014, 141, 1603–1613. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Belmont, J.W.; Ware, S.M. Genetics of human heterotaxias. Eur. J. Hum. Genet. 2006, 14, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Carro Hevia, A.; Santamarta Liébana, E.; Martín Fernández, M. Síndrome de heterotaxia. Cardiocore 2011, 46, 23–26. [Google Scholar] [CrossRef]
- Friedberg, M.K.; Silverman, N.H.; Moon-Grady, A.J.; Tong, E.; Nourse, J.; Sorenson, B.; Lee, J.; Hornberger, L.K. Prenatal detection of congenital heart disease. J. Pediatr. 2009, 155, 26–31. [Google Scholar] [CrossRef]
- Pepes, S.; Zidere, V.; Allan, L. Prenatal diagnosis of left atrial isomerism. Heart 2009, 95, 1974–1977. [Google Scholar] [CrossRef] [PubMed]
- Lai, W.W.; Geva, T.; Shirali, G.S.; Frommelt, P.C.; Humes, R.A.; Brook, M.M.; Pignatelli, R.H.; Rychik, J.; Task Force of the Pediatric Council of the American Society of Echocardiography; Paediatric Council of the American Society of Echocardiography. Guidelines and standards for performance of a pediatric echocardiogram: A report from the Task Force of the Paediatric Council of the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2006, 19, 1413–1430. [Google Scholar] [CrossRef]
- Kao, C.C.; Hsieh, C.C.; Cheng, P.J.; Chiang, C.H.; Huang, S.Y. Total Anomalous Pulmonary Venous Connection: From Embryology to a Prenatal Ultrasound Diagnostic Update. J. Med. Ultrasound 2017, 25, 130–137. [Google Scholar] [CrossRef]
- Chen, W.; Lu, Y.; Ma, L.; Yang, S.; Zou, M.; Li, W.; Chen, X. Outcomes of treatment for right atrial isomerism with functional single ventricle and extracardiac total anomalous pulmonary venous connection beyond neonatal period: Delayed surgical treatment, improving outcomes. Front. Cardiovasc. Med. 2022, 20, 914609. [Google Scholar] [CrossRef]
- Ortega-Zhindón, D.B.; Flores-Sarria, I.P.; Minakata-Quiróga, M.A.; Angulo-Cruzado, S.T.; Romero-Montalvo, L.A.; Cervantes-Salazar, J.L. Atrial isomerism: A multidisciplinary perspective [Isomorfismo cardiaco: Una perspectiva multidisciplinaria]. Arch. Cardiol. Mex. 2021, 91, 470–479. [Google Scholar]
- Carrillo-Álvarez, A.; Martínez-Gutiérrez, A.; Salvat-Germán, F. Reconocimiento del niño con riesgo de parada cardiorrespiratoria. An. Pediatría 2006, 65, 147–153. [Google Scholar] [CrossRef]
- Faraoni, D. Definition of postoperative bleeding in children undergoing cardiac surgery with cardiopulmonary bypass: One size doesn’t fit all. J. Thorac. Cardiovasc. Surg. 2018, 155, 2125–2126. [Google Scholar] [CrossRef]
- Chen, W.; Ma, L.; Cui, H.; Yang, S.; Xia, Y.; Zou, M.; Chen, X. Early-and middle-term surgical outcomes in patients with heterotaxy syndrome. Cardiology 2016, 133, 141–146. [Google Scholar] [CrossRef]
- Jacobs, J.P.; Pasquali, S.K.; Morales, D.L.; Jacobs, M.L.; Mavroudis, C.; Chai, P.J.; Tchervenkov, C.I.; Lacour-Gayet, F.G.; Walters, H., III; Quintessenza, J.A. Heterotaxy: Lessons learned about patterns of practice and outcomes from the congenital heart surgery database of the society of thoracic surgeons. World J. Pediatr. Congenit. Heart Surg. 2011, 2, 278–286. [Google Scholar] [CrossRef]
- Hashmi, A.; Abu-Sulaiman, R.; McCrindle, B.W.; Smallhorn, J.F.; Williams, W.G.; Freedom, R.M. Management and outcomes of right atrial isomerism: A 26-year experience. J. Am. Coll. Cardiol. 1998, 31, 1120–1126. [Google Scholar] [CrossRef] [PubMed]
- Baban, A.; Cantarutti, N.; Adorisio, R.; Lombardi, R.; Calcagni, G.; Mortari, E.P.; Dallapiccola, B.; Marino, B.; Iorio, F.S.; Carsetti, R. Long-term survival and phenotypic spectrum in heterotaxy syndrome: A 25-year follow-up experience. Int. J. Cardiol. 2018, 268, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Alongi, A.M.; Kirklin, J.K.; Deng, L.; Padilla, L.; Pavnica, J.; Romp, R.L.; Mauchley, D.C.; Cleveland, D.C.; Dabal, R. Surgical management of heterotaxy syndrome: Current challenges and opportunities. World J. Pediatr. Congenit. Heart Surg. 2020, 11, 166–176. [Google Scholar] [CrossRef]
- Lafuente, M.; Villalba, C.; Mouratian, M.; Villa, A.; Sciegatamtsac, A.; García, P. Presentación clínica y evolución del isomerismo derecho. Rev. Argent. Cardiol. 2015, 83, 400–405. [Google Scholar] [CrossRef]
- Loomba, R.S.; Nijhawan, K.; Anderson, R. Impact of era, type of isomerism, and ventricular morphology on survival in heterotaxy: Implications for therapeutic management. World J. Pediatr. Congenit. Heart Surg. 2016, 7, 54–62. [Google Scholar] [CrossRef]
- Bhaskar, J.; Galati, J.C.; Brooks, P.; Oppido, G.; Konstantinov, I.E.; Brizard, C.P.; d’Udekem, Y. Survival into adulthood of patients with atrial isomerism undergoing cardiac surgery. J. Thorac. Cardiovasc. Surg. 2015, 149, 1509–1514. [Google Scholar] [CrossRef] [PubMed]
- Vigneswaran, T.V.; Jones, C.B.; Zidere, V.; Charakida, M.; Miller, O.I.; Simpson, J.M.; Sharland, G. Effect of prenatal laterality disturbance and its accompanying anomalies on survival. Am. J. Cardiol. 2018, 122, 663–671. [Google Scholar] [CrossRef]
- Alsoufi, B.; McCracken, C.; Schlosser, B.; Sachdeva, R.; Well, A.; Kogon, B.; Border, W.; Kanter, K. Outcomes of multistage palliation of infants with functional single ventricle and heterotaxy syndrome. J. Thorac. Cardiovasc. Surg. 2016, 151, 1369–1377e2. [Google Scholar] [CrossRef]
- Gilljam, T.; McCrindle, B.W.; Smallhorn, J.F.; Williams, W.G.; Freedom, R.M. Outcomes of left atrial isomerism over a 28-year period at a single institution. J. Am. Coll. Cardiol. 2000, 36, 908–916. [Google Scholar] [CrossRef] [PubMed]
- Banka, P.; Adar, A.; Schaetzle, B.; Sleeper, L.A.; Emani, S.; Geva, T. Changes in prognosis of heterotaxy syndrome over time. Pediatrics 2020, 146, e20193345. [Google Scholar] [CrossRef] [PubMed]
- Acherman, R.J.; Evans, W.N. Persistent right umbilical vein in isomerism. Prenat. Diagn. 2019, 39, 1220–1224. [Google Scholar] [CrossRef] [PubMed]
- Knowles, M.R.; Zariwala, M.; Leigh, M. Primary Ciliary Dyskinesia. Clin. Chest Med. 2016, 37, 449–461. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, M.P.; Omran, H.; Leigh, M.W.; Dell, S.; Morgan, L.; Molina, P.L.; Robinson, B.V.; Minnix, S.L.; Olbrich, H.; Severin, T.; et al. Congenital heart disease and other heterotaxic defects in a large cohort of patients with primary ciliary dyskinesia. Circulation 2007, 115, 2814–2821. [Google Scholar] [CrossRef]
- Nakhleh, N.; Francis, R.; Giese, R.A.; Tian, X.; Li, Y.; Zariwala, M.A.; Yagi, H.; Khalifa, O.; Kureshi, S.; Chatterjee, B.; et al. High prevalence of respiratory ciliary dysfunction in congenital heart disease patients with heterotaxy. Circulation 2012, 125, 2232–2242. [Google Scholar] [CrossRef]
- Swisher, M.; Jonas, R.; Tian, X.; Lee, E.S.; Lo, C.W.; Leatherbury, L. Increased postoperative and respiratory complications in patients with congenital heart disease associated with heterotaxy. J. Thorac. Cardiovasc. Surg. 2011, 141, 637–644, 644.e1-3. [Google Scholar] [CrossRef]
- McGovern, E.; Kelleher, E.; Potts, J.E.; O’Brien, J.; Walsh, K.; Nolke, L.; McMahon, C.J. Predictors of poor outcome among children with heterotaxy syndrome: A retrospective review. Open Heart 2016, 3, e000328. [Google Scholar] [CrossRef]
- Hosseinpour, A.R.; González-Calle, A.; Adsuar-Gómez, A. ¿Qué queremos decir con el término univentricular? Cir. Cardiov. 2015, 22, 193–194. [Google Scholar] [CrossRef][Green Version]
- Serrano, F.; Caffarena, J.M. Cirugía del corazón univentricular en segundo estadio: Técnicas y resultados. Cir. Cardiov. 2008, 15, 351–360. [Google Scholar] [CrossRef]
- Ozawa, Y.; Asakai, H.; Shiraga, K.; Shindo, T.; Hirata, Y.; Hirata, Y.; Inuzuka, R. Cardiac Rhythm Disturbances in Heterotaxy Syndrome. Pediatr. Cardiol. 2019, 40, 909–913. [Google Scholar] [CrossRef] [PubMed]
- Loomba, R.S.; Willes, R.J.; Kovach, J.R.; Anderson, R.H. Chronic Arrhythmias in the Setting of Heterotaxy: Differences between Right and Left Isomerism. Congenit. Heart Dis. 2016, 11, 7–18. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total n = 38 |
|---|---|
| Sex, n (%) | |
| Male | 22 (57.9) |
| Female | 16 (42.1) |
| Age (years), median (IQR) | 4 (2–9.2) |
| Weight (kg), median (IQR) | 14.3 (9.8–22.1) |
| Height (cm), mean (±SD) | 102 (29.1) |
| Previous surgery, n (%) | |
| 0 | 25 (65.8) |
| 1 | 12 (31.6) |
| 2 | 1 (2.6) |
| RACHS-1, n (%) | |
| 2 | 5 (13.2) |
| 3 | 33 (86.8) |
| Cardiac intrathoracic position, n (%) | |
| Levocardia | 21 (55.3) |
| Dextrocardia | 17 (44.7) |
| Atrioventricular valve regurgitation, n (%) | |
| None | 8 (21.1) |
| Mild | 27 (71) |
| Moderate | 1 (2.6) |
| Severe | 2 (5.3) |
| Anomalous pulmonary venous connection, n (%) | |
| Partial | 2 (5.3) |
| Total | 13 (34.3) |
| Pulmonary venous connection, n (%) | |
| Right atrium | 15 (39.5) |
| Left atrium | 20 (52.6) |
| Both atriums | 3 (7.9) |
| Pulmonary artery branches, n (%) | |
| Normal | 15 (39.5) |
| Stenosis | 23 (60.5) |
| Characteristic, n (%) | Total n = 38 |
|---|---|
| Diagnosis | |
| AV canal | 24 (63.2) |
| Pulmonary stenosis | 21 (55.3) |
| PDA | 17 (44.7) |
| Pulmonary atresia | 15 (39.5) |
| TAPVC | 13 (34.3) |
| DORV | 9 (23.7) |
| Hypoplastic left ventricle | 6 (15.9) |
| PAPVC | 2 (5.3) |
| Surgery | |
| MBTS | 13 (34.3) |
| MBTS + TAPVC repair | 10 (26.3) |
| TCPC with an extracardiac conduit fenestrated without CPB | 6 (15.9) |
| BCPC without CPB | 3 (7.9) |
| MBTS + thrombectomy of pulmonary artery + TAPVC repair | 1 (2.6) |
| BCPC with CPB + TAPVC repair | 1 (2.6) |
| BCPC with CPB + RPA angioplasty + PAPVC repair | 1 (2.6) |
| TCPC with an extracardiac conduit fenestrated + PAPVC repair | 1 (2.6) |
| Mechanical AV valve replacement + MBTS + TAPVC repair | 1 (2.6) |
| BCPC takedown + MBTS | 1 (2.6) |
| Characteristic | Total n = 38 |
|---|---|
| Surgery with CPB, n (%) | 15 (39.5) |
| CPB (min), median (IQR) | 89 (67–107) |
| Aortic cross-clamp (min), median (IQR) | 55 (22–83) |
| Mechanical ventilation in PICU, n (%) | 34 (89.5) |
| Mechanical ventilation time (h), median (IQR) | 22 (10–126) |
| Reintubation, n (%) | 3 (7.9) |
| Days in PICU, n (%) | |
| <1 day | 2 (5.3) |
| 1–7 days | 27 (71) |
| 8–15 days | 8 (21.1) |
| >15 days | 1 (2.6) |
| Variable | Alive | Dead | OR | CI 95% | p | |||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | Lower | Upper | |||
| Previous surgery | 11 | 33.3 | 2 | 40 | 1.33 | 0.19 | 9.18 | 1 |
| Anomalous pulmonary venous connection | 13 | 39.4 | 0 | 0 | - | - | - | - |
| Anomalous pulmonary artery branches | 21 | 63.6 | 2 | 40 | 0.38 | 0.06 | 2.61 | 0.37 |
| Atrioventricular valve regurgitation | 25 | 81.8 | 3 | 60 | 0.33 | 0.05 | 2.46 | 0.28 |
| Atrioventricular valve replacement | 0 | 0 | 1 | 20 | 1.25 | 0.81 | 1.94 | 0.13 |
| Preoperative intubation | 4 | 12.1 | 2 | 40 | 4.83 | 0.61 | 38.39 | 0.17 |
| Preoperative inotrope use | 3 | 9.1 | 2 | 40 | 6.67 | 0.78 | 57.06 | 0.12 |
| Transoperative inotrope use | 26 | 78.8 | 5 | 100 | 0.78 | 0.66 | 0.94 | 0.56 |
| Postoperative inotrope use | 28 | 84.8 | 5 | 100 | 0.84 | 0.74 | 0.98 | 1 |
| Inhaled nitric oxide use | 2 | 6.1 | 2 | 40 | 10.33 | 1.05 | 102.08 | 0.08 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ortega-Zhindón, D.B.; Pérez-Hernández, N.; Rodríguez-Pérez, J.M.; García-Montes, J.A.; Calderón-Colmenero, J.; Rivera-Buendía, F.; Cervantes-Salazar, J.L. Cardiac Laterality: Surgical Results of Right Atrial Isomerism. Diseases 2023, 11, 170. https://doi.org/10.3390/diseases11040170
Ortega-Zhindón DB, Pérez-Hernández N, Rodríguez-Pérez JM, García-Montes JA, Calderón-Colmenero J, Rivera-Buendía F, Cervantes-Salazar JL. Cardiac Laterality: Surgical Results of Right Atrial Isomerism. Diseases. 2023; 11(4):170. https://doi.org/10.3390/diseases11040170
Chicago/Turabian StyleOrtega-Zhindón, Diego B., Nonanzit Pérez-Hernández, José Manuel Rodríguez-Pérez, José A. García-Montes, Juan Calderón-Colmenero, Frida Rivera-Buendía, and Jorge L. Cervantes-Salazar. 2023. "Cardiac Laterality: Surgical Results of Right Atrial Isomerism" Diseases 11, no. 4: 170. https://doi.org/10.3390/diseases11040170
APA StyleOrtega-Zhindón, D. B., Pérez-Hernández, N., Rodríguez-Pérez, J. M., García-Montes, J. A., Calderón-Colmenero, J., Rivera-Buendía, F., & Cervantes-Salazar, J. L. (2023). Cardiac Laterality: Surgical Results of Right Atrial Isomerism. Diseases, 11(4), 170. https://doi.org/10.3390/diseases11040170





