Patient Reported Outcome Measures (PROMs) in Surgery: Evaluation after Minimally Invasive Reduction and Percutaneous K-Wires Fixation for Intra-Articular Calcaneal Fractures
Abstract
1. Introduction
2. Materials and Methods
- Bilateral calcaneus fracture;
- Associated fractures;
- Conservative treatment;
- History of prior or subsequent lower limb surgeries;
- Severe comorbidities (uncontrolled diabetes, rheumatic diseases, vascular disruptions);
- Incomplete radiographic imaging assessment.
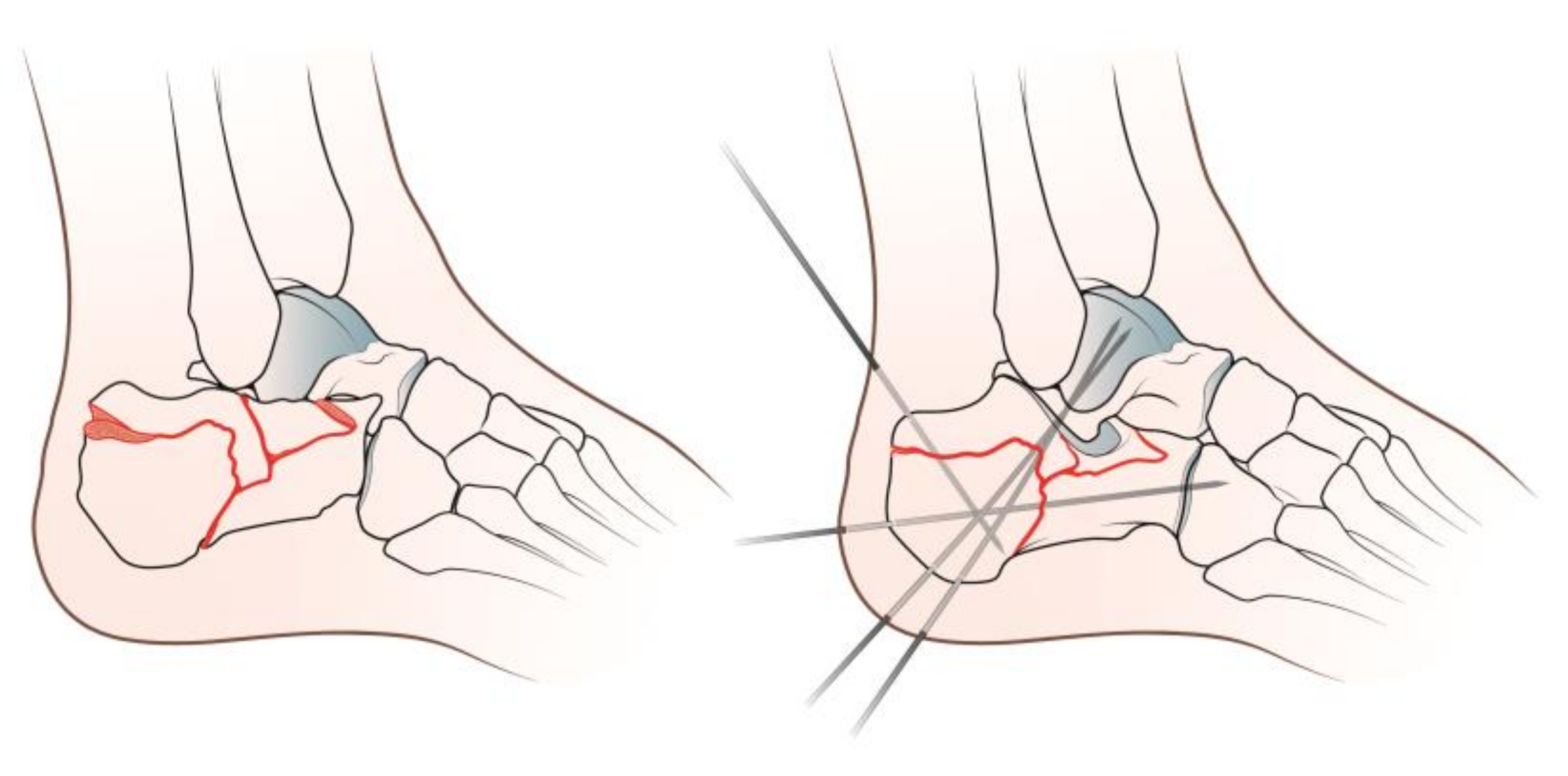
2.1. Surgical Procedure
2.2. Data Collection
2.3. Statistical Analysis
3. Results
4. Discussion
Limitations and Future Direction
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Duramaz, A.; Polat, Ö.; İlter, M.H.; Bayram, B.; Bayrak, A.; Baca, E. Could percutaneous fixation with crossed Schanz pins be an alternative to open reduction in the treatment of intra-articular calcaneal fractures? Int. Orthop. 2021, 45, 731–741. [Google Scholar] [CrossRef] [PubMed]
- Shi, F.; Wu, S.; Cai, W.; Zhao, Y. Comparison of 5 Treatment Approaches for Displaced Intra-articular Calcaneal Fractures: A Systematic Review and Bayesian Network Meta-Analysis. J. Foot Ankle Surg. 2020, 59, 1254–1264. [Google Scholar] [CrossRef] [PubMed]
- Giannini, S.; Cadossi, M.; Mosca, M.; Tedesco, G.; Sambri, A.; Terrando, S.; Mazzotti, A. Minimally-invasive treatment of calcaneal fractures: A review of the literature and our experience. Injury 2016, 47 (Suppl. S4), S138–S146. [Google Scholar] [CrossRef]
- McKeown, R.; Kearney, R.S.; Liew, Z.H.; Ellard, D.R. Patient experiences of an ankle fracture and the most important factors in their recovery: A qualitative interview study. BMJ Open 2020, 10, e033539. [Google Scholar] [CrossRef]
- Weldring, T.; Smith, S.M.S. Patient-Reported Outcomes (PROs) and Patient-Reported Outcome Measures (PROMs). Health Serv. Insights 2013, 6, 61–68. [Google Scholar] [CrossRef]
- Brauer, C.A.; Manns, B.J.; Ko, M.; Donaldson, C.; Buckley, R. An economic evaluation of operative compare with nonoperative management of displaced intra-articular calcaneus fractures. J. Bone Joint Surg. Am. 2005, 87, 2741–2749. [Google Scholar] [CrossRef] [PubMed]
- Radnay, C.S.; Clare, M.P.; Sanders, R.W. Subtalar fusion after displaced intra-articular calcaneal fractures: Does initial operative treatment matter? J. Bone Joint Surg. Am. 2009, 91, 541–546. [Google Scholar] [CrossRef]
- Gotha, H.E.; Zide, J.R. Current Controversies in Management of Calcaneus Fractures. Orthop. Clin. N. Am. 2017, 48, 91–103. [Google Scholar] [CrossRef]
- Shih, J.T.; Kuo, C.L.; Yeh, T.T.; Shen, H.C.; Pan, R.Y.; Wu, C.C. Modified Essex-Lopresti procedure with percutaneous calcaneoplasty for comminuted intra-articular calcaneal fractures: A retrospective case analysis. BMC Musculoskelet. Disord. 2018, 19, 77. [Google Scholar] [CrossRef]
- Tornetta, P., III. The Essex-Lopresti reduction for calcaneal fractures revisited. J. Orthop. Trauma 1998, 12, 469–473. [Google Scholar] [CrossRef]
- Forgon, M. Closed reduction and percutaneus osteosynthesis: Technique and results in 265 calcaneal fractures. In Major Fractures of the Pilon, the Talus and the Calcaneus; Tscherne, H., Schatzker, J., Eds.; Springer: Berlin/Heidelberg, Germany, 1992; pp. 207–213. [Google Scholar]
- Stehlik, J.; Stulik, J. Combined method of treating dislocated fractures of the calcaneus. Acta Chir. Orthop. Traumatol. Czech. 2002, 69, 209–218. [Google Scholar]
- Maccagnano, G.; Noia, G.; Cassano, G.D.; Sarni, A.L.; Quitadamo, R.; Stigliani, C.; Liuzza, F.; Vitiello, R.; Pesce, V. Quality of Life and Clinical Evaluation of Calcaneoplasty with a Balloon System for Calcaneal Fracture at 5 Years of Follow-Up. Adv. Orthop. 2021, 2021, 5530620. [Google Scholar] [CrossRef]
- Vittore, D.; Vicenti, G.; Caizzi, G.; Abate, A.; Moretti, B. Balloon-assisted reduction, pin fixation and tricalcium phosphate augmentation for calcanear fracture. Injury 2014, 45 (Suppl. S6), S72–S79. [Google Scholar] [CrossRef] [PubMed]
- Vosoughi, A.R.; Borazjani, R.; Ghasemi, N.; Fathi, S.; Mashhadiagha, A.; Hoveidaei, A.H. Different types and epidemiological patterns of calcaneal fractures based on reviewing CT images of 957 fractures. Foot Ankle Surg. 2022, 28, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Vicenti, G.; Carrozzo, M.; Solarino, G.; Caizzi, G.; De Crescenzo, A.; Portaluri, M.; Mori, C.M.; Vittore, D.; Moretti, B. Comparison of plate, calcanealplasty and external fixation in the management of calcaneal fractures. Injury 2019, 50 (Suppl. S4), S39–S46. [Google Scholar] [CrossRef]
- Lin, J.; Xie, C.; Chen, K.; Sun, S.; Zhou, K.; Zhou, C.; Shui, X.; Kong, J. Comparison of sinus tarsi approach versus extensile lateral approach for displaced intra-articular calcaneal fractures Sanders type IV. Int. Orthop. 2019, 43, 2141–2149. [Google Scholar] [CrossRef] [PubMed]
- Essex-Lopresti, P. The mechanism, reduction technique, and results in fractures of the os calcis. Br. J. Surg. 1952, 39, 395–419. [Google Scholar] [CrossRef]
- Sanders, R. Displaced intra-articular fractures of the calcaneus. J. Bone Joint Surg. Am. 2000, 82, 225–250. [Google Scholar] [CrossRef]
- Budiman-Mak, E.; Conrad, K.J.; Roach, K.E. The Foot Function Index: A measure of foot pain and disability. J. Clin. Epidemiol. 1991, 44, 561–570. [Google Scholar] [CrossRef]
- Roos, E.M.; Brandsson, S.; Karlsson, J. Validation of the foot and ankle outcome score for ankle ligament reconstruction. Foot Ankle Int. 2001, 22, 788–794. [Google Scholar] [CrossRef] [PubMed]
- McKeown, R.; Ellard, D.R.; Rabiu, A.R.; Karasouli, E.; Kearney, R.S. A systematic review of the measurement properties of patient reported outcome measures used for adults with an ankle fracture. J. Patient Rep. Outcomes 2019, 3, 70. [Google Scholar] [CrossRef] [PubMed]
- Martinelli, N.; Scotto, G.M.; Sartorelli, E.; Bonifacini, C.; Bianchi, A.; Malerba, F. Reliability, validity and responsiveness of the Italian version of the Foot Function Index in patients with foot and ankle diseases. Qual. Life Res. 2014, 23, 277–284. [Google Scholar] [CrossRef]
- De Boer, A.S.; Van Lieshout, E.M.; Den Hartog, D.; Weerts, B.; Verhofstad, M.H.; Schepers, T. Functional outcome and patient satisfaction after displaced intra-articular calcaneal fractures: A comparison among open, percutaneous, and nonoperative treatment. J. Foot Ankle Surg. 2015, 54, 298–305. [Google Scholar] [CrossRef] [PubMed]
- Biz, C.; Barison, E.; Ruggieri, P.; Iacobellis, C. Radiographic and functional outcomes after displaced intra-articular calcaneal fractures: A comparative cohort study among the traditional open technique (ORIF) and percutaneous surgical procedures (PS). J. Orthop. Surg. Res. 2016, 11, 92. [Google Scholar] [CrossRef] [PubMed]
- Cianni, L.; Vitiello, R.; Greco, T.; Sirgiovanni, M.; Ragonesi, G.; Maccauro, G.; Perisano, C. Predictive Factors of Poor Outcome in Sanders Type III and IV Calcaneal Fractures Treated with an Open Reduction and Internal Fixation with Plate: A Medium-Term Follow-Up. J. Clin. Med. 2022, 11, 5660. [Google Scholar] [CrossRef]
- Shams, A.; Gamal, O.; Mesregah, M.K. Minimally Invasive Reduction of Intraarticular Calcaneal Fractures with Percutaneous Fixation Using Cannulated Screws Versus Kirschner Wires: A Retrospective Comparative Study. Foot Ankle Spec. 2023, 16, 28–35. [Google Scholar] [CrossRef]
- Driessen, M.; Edwards, M.; Biert, J.; Hermans, E. Long-term results of displaced intra-articular calcaneal fractures treated with minimal invasive surgery using percutaneous screw fixation. Injury 2021, 52, 1054–1059. [Google Scholar] [CrossRef]
- Loucks, C.; Buckley, R. Bohler’s angle: Correlation with outcome in displaced intra-articular calcaneal fractures. J. Orthop. Trauma 1999, 13, 554–558. [Google Scholar] [CrossRef]
- Buckley, R.; Tough, S.; McCormack, R.; Pate, G.; Leighton, R.; Petrie, D.; Galpin, R. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: A prospective, randomized, controlled multicenter trial. J. Bone Joint Surg. Am. 2002, 84, 1733–1744. [Google Scholar] [CrossRef]
- Saris-Baglama, R.N.; Dewey, C.J.; Chisholm, G.B.; Plumb, E.; King, J.; Kosinski, M.; Bjorner, J.B.; Ware, J.E. QualityMetric Health OutcomesTM Scoring Software 4.0 Installation Guide; QualityMetric Incorporated: Lincoln, RI, USA, 2010; p. 14. [Google Scholar]
- Haefeli, M.; Elfering, A. Pain assessment. Eur. Spine J. 2006, 15 (Suppl. S1), S17–S24. [Google Scholar] [CrossRef]
- Nooijen, L.E.; Spierings, K.E.; Sanders, F.R.K.; Dingemans, S.A.; Halm, J.A.; Schepers, T. Determining the Correlation Between Lateral Radiograph Morphology and the Outcome Following Surgically Treated Intra-Articular Calcaneal Fractures. Foot Ankle Spec. 2021, 14, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Kitaoka, H.B.; Alexander, I.J.; Adelaar, R.S.; Nunley, J.A.; Myerson, M.S.; Sanders, M. Clinical Rating Systems for the Ankle-Hindfoot, Midfoot, Hallux, and Lesser Toes. Foot Ankle Int. 1994, 15, 349–353. [Google Scholar] [CrossRef]
- Su, Y.; Chen, W.; Zhang, T.; Wu, X.; Wu, Z.; Zhang, Y. Bohler’s angle’s role in assessing the injury severity and functional outcome of internal fixation for displaced intra-articular calcaneal fractures: A retrospective study. BMC Surg. 2013, 13, 40. [Google Scholar] [CrossRef] [PubMed]
- Field, J.; Holmes, M.M.; Newell, D. PROMs data: Can it be used to make decisions for individual patients? A narrative review. Patient Relat. Outcome Meas. 2019, 29, 233–241. [Google Scholar] [CrossRef] [PubMed]

| Preoperative (Degrees) Mean ± SD (Range) | Last Radiographic F.U. (Degrees) Mean ± SD (Range) | p-Value | |
|---|---|---|---|
| Böhler's angle + | 22.3 ± 15.1 (−15–55) | 30.8 ± 12 (0–60) | <0.05 |
| Gissane’s angle + | 126.3 ± 10.9 (110–150) | 118.5 ± 9.4 (102–145) | <0.05 |
| FFI | ||||
|---|---|---|---|---|
| Pain (Raw Subscore) | Disability (Raw Subscore) | Activity Limitations (Raw Subscore) | Total (Normalized Score) | |
| Score | 24.7 ± 21 (0–78) | 22.4 ± 19.1 (0–66) | 6 ± 8.5 (0–44) | 24.3 ± 19.9 (0.4–80.9) |
| FAOS | ||||||
|---|---|---|---|---|---|---|
| Pain (Raw Subscore) | Symptoms (Raw Subscore) | ADL (Raw Subscore) | Sport and Recreation (Raw Subscore) | QoL (Raw Subscore) | Total (Normalized Score) | |
| Score | 67.2 ± 30 (4–100) | 66.2 ± 28.3 (3–100) | 78.8 ± 23.2 (16–100) | 44.7 ± 24.6 (5–100) | 57 ± 30.9 (0–100) | 68 ± 24.8 (8.9–100) |
| FFI | ||||
|---|---|---|---|---|
| Pain (Median = 27) | Disability (Median = 18) | Activity Limitations (Median = 4) | Total (Median = 20) | |
| Age at surgery * | NS | NS | NS | NS |
| Age at PROMs collection * | NS | NS | NS | NS |
| PROMs F.U. * | NS | NS | NS | NS |
| Sex ° | NS | NS | NS | NS |
| Preoperative Gissane’s angle * | NS | NS | p < 0.05 | NS |
| Last F.U. Gissane’s angle * | NS | NS | p < 0.05 | NS |
| Preoperative Böhler's angle * | NS | NS | NS | NS |
| Last F.U. Böhler's angle * | NS | NS | NS | NS |
| FAOS | ||||||
|---|---|---|---|---|---|---|
| Pain (Median = 79) | Symptoms (Median = 72) | ADL (Median = 87) | Sport and Recreation (Median = 45) | QoL (Median = 56) | Total (Median = 72) | |
| Age at surgery * | NS | NS | NS | NS | NS | NS |
| Age at PROMs collection * | NS | NS | NS | NS | NS | NS |
| PROMs F.U. * | NS | NS | NS | NS | NS | NS |
| Sex ° | NS | NS | NS | NS | NS | NS |
| Preoperative Gissane’s angle * | p < 0.05 | p < 0.05 | p < 0.05 | NS | NS | p < 0.05 |
| Last F.U. Gissane’s angle * | NS | NS | NS | NS | NS | NS |
| Preoperative Böhler's angle * | NS | p < 0.05 | p < 0.05 | p < 0.05 | NS | NS |
| Last F.U. Böhler's angle * | NS | NS | NS | NS | NS | NS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brognara, L.; Mazzotti, A.; Arceri, A.; Artioli, E.; Casadei, G.; Bonelli, S.; Traina, F.; Faldini, C. Patient Reported Outcome Measures (PROMs) in Surgery: Evaluation after Minimally Invasive Reduction and Percutaneous K-Wires Fixation for Intra-Articular Calcaneal Fractures. Diseases 2023, 11, 57. https://doi.org/10.3390/diseases11020057
Brognara L, Mazzotti A, Arceri A, Artioli E, Casadei G, Bonelli S, Traina F, Faldini C. Patient Reported Outcome Measures (PROMs) in Surgery: Evaluation after Minimally Invasive Reduction and Percutaneous K-Wires Fixation for Intra-Articular Calcaneal Fractures. Diseases. 2023; 11(2):57. https://doi.org/10.3390/diseases11020057
Chicago/Turabian StyleBrognara, Lorenzo, Antonio Mazzotti, Alberto Arceri, Elena Artioli, Giacomo Casadei, Simone Bonelli, Francesco Traina, and Cesare Faldini. 2023. "Patient Reported Outcome Measures (PROMs) in Surgery: Evaluation after Minimally Invasive Reduction and Percutaneous K-Wires Fixation for Intra-Articular Calcaneal Fractures" Diseases 11, no. 2: 57. https://doi.org/10.3390/diseases11020057
APA StyleBrognara, L., Mazzotti, A., Arceri, A., Artioli, E., Casadei, G., Bonelli, S., Traina, F., & Faldini, C. (2023). Patient Reported Outcome Measures (PROMs) in Surgery: Evaluation after Minimally Invasive Reduction and Percutaneous K-Wires Fixation for Intra-Articular Calcaneal Fractures. Diseases, 11(2), 57. https://doi.org/10.3390/diseases11020057











