Abstract
Background: The declaration of the COVID-19 pandemic triggered global efforts to control and manage the virus impact. Scientists and researchers have been strongly involved in developing effective strategies that can help policy makers and healthcare systems both to monitor the spread and to mitigate the impact of the COVID-19 pandemic. Machine Learning (ML) and Artificial Intelligence (AI) have been applied in several fronts of the fight. Foremost is diagnostic assistance, encompassing patient triage, prediction of ICU admission and mortality, identification of mortality risk factors, and discovering treatment drugs and vaccines. Objective: This systematic review aims to identify original research studies involving actual patient data to construct ML- and AI-based models for clinical decision support for early response during the pandemic years. Methods: Following the PRISMA methodology, two large academic research publication indexing databases were searched to investigate the use of ML-based technologies and their applications in healthcare to combat the COVID-19 pandemic. Results: The literature search returned more than 1000 papers; 220 were selected according to specific criteria. The selected studies illustrate the usefulness of ML with respect to supporting healthcare professionals for (1) triage of patients depending on disease severity, (2) predicting admission to hospital or Intensive Care Units (ICUs), (3) search for new or repurposed treatments and (4) the identification of mortality risk factors. Conclusion: The ML/AI research community was able to propose and develop a wide variety of solutions for predicting mortality, hospitalizations and treatment recommendations for patients with COVID-19 diagnostic, opening the door for further integration of ML in clinical practices fighting this and forecoming pandemics. However, the translation to the clinical practice is impeded by the heterogeneity of both the datasets and the methodological and computational approaches. The literature lacks robust model validations supporting this desired translation.
1. Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first reported in Wuhan in December 2019 with common clinical symptoms, such as fever, cough, muscle or body aches, fatigue, congestion or runny nose. The virus was declared a potential health hazard for people with background diseases as it affects the upper-lower respiratory system and can cause lung infections and chronic lung obstruction. The World Health Organization (WHO) declared a pandemic crisis on 11 March 2020. An early estimation of the SARS-CoV-2 average reproduction rate (i.e., the average number of cases of infection caused by an identified infected individual) was 3.28 [1], explaining the perceived exponential growth of cases at the very beginning of the pandemic. The potential for health complications and the rapid spread of the virus induced governments around the world to dictate strict population control measures to prevent the spread of the virus. As a result of the panicked global response, demand for innovative healthcare resources increased dramatically. Over the course of this pandemic, intense research has addressed designing Artificial Intelligence (AI), Machine Learning (ML) and robotic solutions to improve diagnostic services, risk assessment, monitoring, and tele-assistance, aiming to reduce significantly the workload of front-line healthcare workers. Such pressure on the scientific community has generated a real tsunami of publications. A search under the term COVID-19 returns over four-hundred-thousand references in PubMed; this figure gives a good impression of the magnitude of the task of any review effort. In this setting, it is proposed that ML and AI can supplement data analysis, for instance collating candidate drug relationships, looking for pharmaceutical targets in the midst of massive amounts of data, finding biomarkers and simulating the reaction of main compounds, greatly accelerating the speed of research and improving quality and efficacy [2]. Hence, ML and AI promised great potential with respect to data-driven solutions to help humankind deal with COVID-19 [3].
Even after the declaration of the end of the pandemic by the WHO on 6 May 2023, COVID-19 is not a fully understood disease, with multiple biological and clinical manifestations. New symptoms of the disease continue to be reported [4], and the guidelines concerning which patients should be considered Persons Under Investigation (PUIs) for COVID-19 or tested for SARS-CoV-2 infection have been continually evolving during the pandemic years. Indeed, clinical needs are revised frequently [5]. One of the salient features of COVID-19 that has unfolded after several years into the pandemic is the evolution of the symptoms of the disease [6], often attributed to the evolution of the underlying virus [7], accompanied by the changes and uncertainties associated with the detection and testing methods [8]. This uncertainty in the case labeling seriously compromises the extrapolation of the results of Machine Learning (ML) algorithms (i.e., generalization or external validation) to different periods and sites of the pandemic. On the other hand, some risks factors were identified early on and remain as such through the evolution of the pandemic. Paramount risks are obesity [9,10,11] and age [12,13].
Previous reviews of the use of ML or AI tools in the context of COVID-19 are either very broad or deal with narrow issues. Broad reviews [14,15,16] tackle a wide variety of techniques and issues that are sometimes unrelated to clinical decision issues in COVID-19 patients, such as the epidemiological model of disease transmission [16]. Others deal with the problem of disease diagnosis in general [17]. Narrow reviews deal with specific aspects, such as the effects of age [12,13], obesity [10,18], drug repurposing [19], cardio-vascular risks [20], analysis of medical images [21,22], and testing devices [8].
This state of the art has been reviewed following research questions that had been raised previously in order to create a pathway for the realization of a specific study and not only to create a review of a specific topic [17,21,22]. This paper presents a systematic review of ML approaches that have been proposed in the early pandemic response to deal with relevant clinical decision issues: patient triage at admittance, prediction of intensive care unit (ICU) admittance, prediction of death outcome, and identification of mortality risks. Additionally, we review AI-based approaches for treatment design, specifically a search via AI tools for drugs targeting the COVID-19 pathogen, SARS-CoV-2.
2. Research Questions
The main aim of this paper is to review the diverse ML approaches that were proposed as a first response to the COVID-19 pandemic in order to alleviate the cognitive and administrative burden of healthcare providers. Most patients enter a hospital through the Emergency Department (ED); hence, ML tools may have a great impact there with respect to managing the expected overload. However, it is imperative to assess the quality of the studies from an ML methodological point of view in order to ascertain if these studies may be (have been) transferred effectively and in a timely manner to the clinical practice as actual support for the clinician.
This scientific objective is made concrete in the following Research Questions:
- RQ1
- Did studies follow open science standards? Specifically, have the data used been published in open access?
- RQ2
- Which ML models have been most frequently proposed and validated?
- RQ3
- Which variables/features are taken into account and which are the most significant risks found?
- RQ4
- Which validation protocols of ML models have been most frequently applied?
- RQ5
- Which performance measures are reported? Which are the performances achieved according to these measures?
3. Methods
Search Strategy
A systematic literature search was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. Literature searches were conducted in the Web of Science and IEEExplore sites. The search string contained the following terms: “(COVID-19 OR SARS-CoV-2 OR coronavirus) AND (machine learning OR deep learning OR artificial intelligence)”. The JabRef reference database manager was used to perform the literature search from January 2020 to June 2022. The selection process is as follows: titles and abstracts of the papers retrieved via the search are screened, removing those that do not meet the inclusion criteria (not duplicated, reporting actual predictive performance results over a dataset collected in a clinical setting, not being epidemiological studies based on aggregated data, giving a detailed specification of recorded variables, giving detailed descriptions of ML and statistical methods). Selected papers were analyzed according to the research questions enumerated above.
4. Results
4.1. Search Results
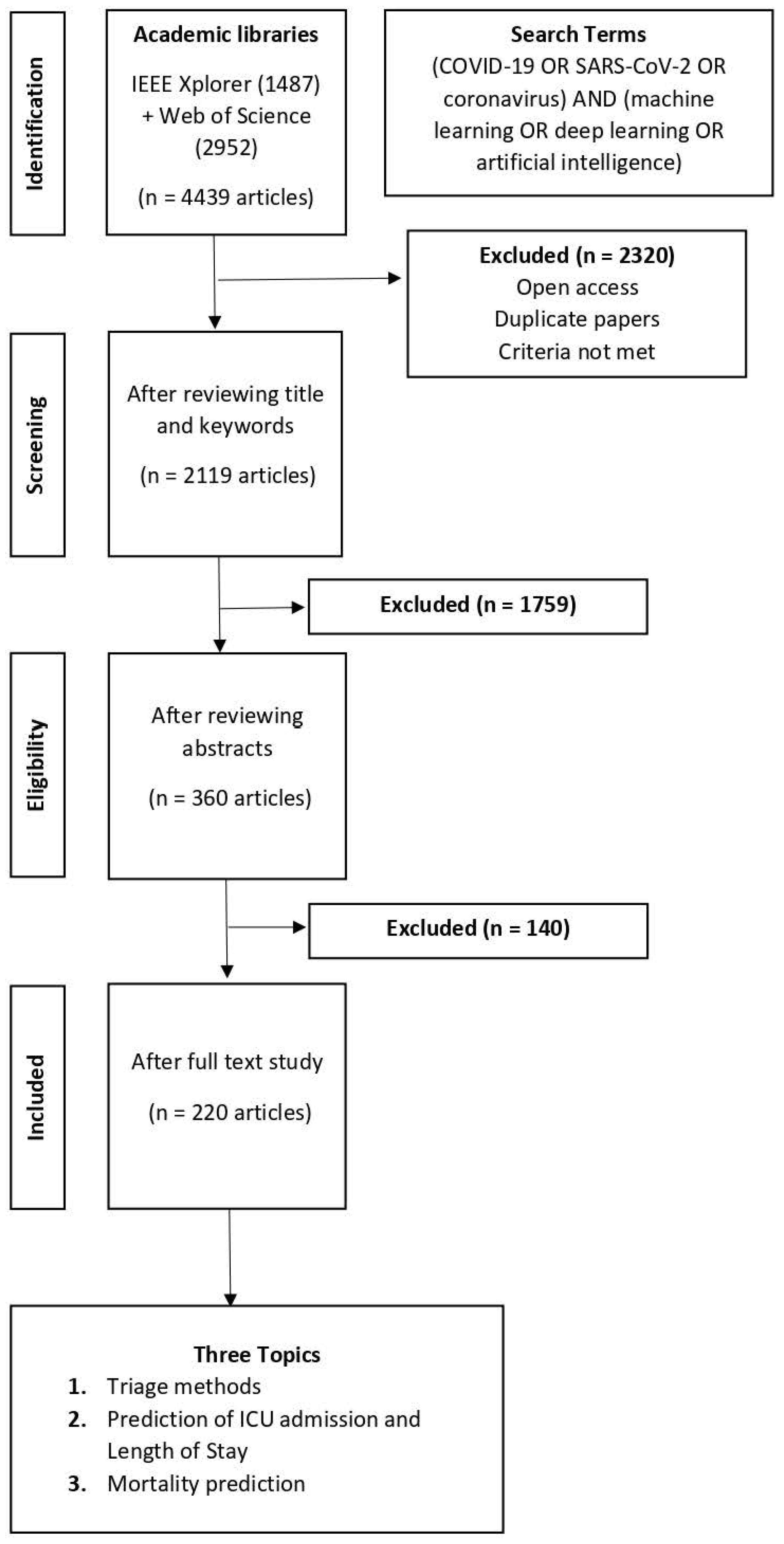
The bibliographic search yielded 2119 research papers. After screening titles and abstracts, 1759 did not meet the inclusion criteria. A further 140 studies were excluded in the next stage when the full texts of this set of articles were assessed, leaving 220 papers eligible for analysis. Figure 1 illustrates the pipeline of the paper-selection process. Table 1, Table 2 and Table 3 summarize the salient details of the selected papers distributed into the following clinical healthcare topics where ML has been proposed for decision assistance: (1) triage of patients at admission, (2) risk of COVID-19-related ICU admission and (3) risk factors for COVID-19-related death.
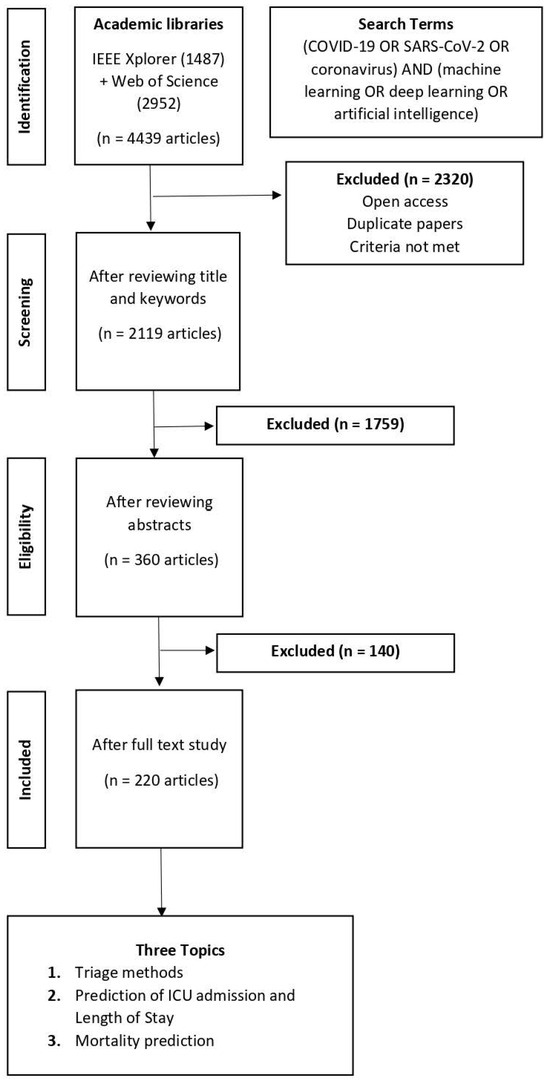
Figure 1.
Flowchart of the paper-selection process.

Table 1.
Studies reporting a patient triage system. Data segmentation (DS), Data Augmentation (DA), Dataset Source access (DSS), Training Dataset (Tr), Testing Dataset (Te), Accuracy (AC), F1-score (F1), Sensitivity (Se), Specificity (Sp), Recall (R), Cross-Validation (CV), External Validation (EV), Internal Validation (IV).

Table 2.
Studies predicting the transfer to ICU and Length of Stay (LoS) in for COVID-19 patients. Data segmentation (DS), Data Augmentation (DA), Dataset Source access (DSS), Training Dataset (Tr), Testing Dataset (Te), Accuracy (AC), F1-score (F1), Sensitivity (Se), Specificity (Sp), Recall (R), Cross-Validation (CV), External Validation (EV), Internal Validation (IV).

Table 3.
Studies predicting mortality and identifying risk factors in patients. Data segmentation (DS), Data Augmentation (DA), Dataset Source access (DSS), Training Dataset (Tr), Testing Dataset (Te), Accuracy (AC), F1-score (F1), Sensitivity (Se), Specificity (Sp), Recall (R), Cross-Validation (CV), External Validation (EV), Internal Validation (IV).
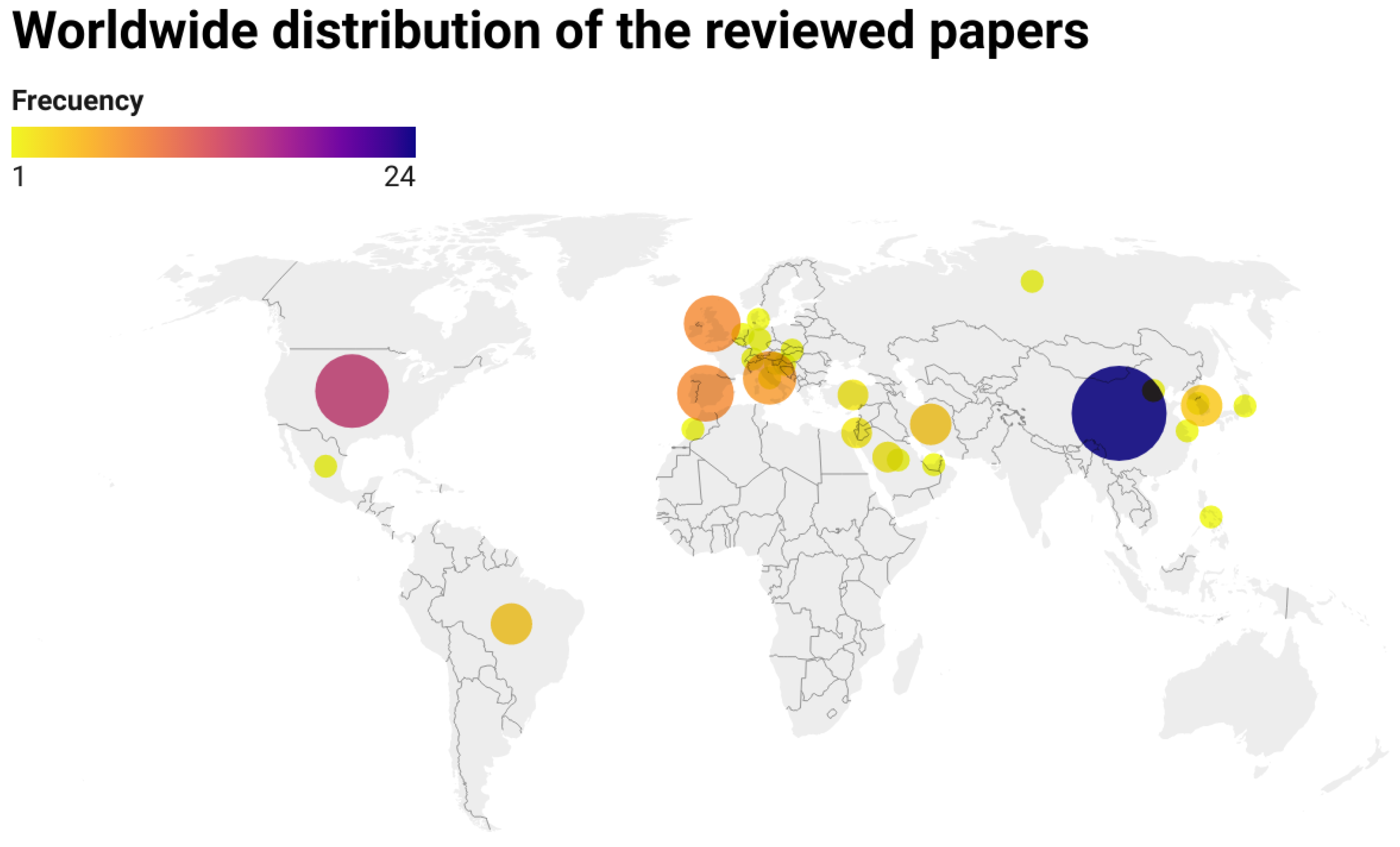
Geographical Distribution of the Authors
The corresponding authors of the articles came from 29 different countries. The authors from the United States and China produced the largest published output, with (24.74%) and (14.43%) articles, respectively. Authors from Asia (), Europe () and America () constituted 47.42%, 31.97% and 19.59% of the articles, respectively.
The map shown in Figure 2 reveals that authorship was distributed across much of the world, preferably in the Northern Hemisphere. The majority of the studies from Asia focus largely on data collected in the region of Wuhan in China, where SARS-CoV-2 was first reported, reflecting the growing interest of researchers in understanding the beginnings of the health crisis. On the other hand, there are few studies from the Southern Hemisphere. Specifically, the selection does not include studies from Oceania and Africa matching our criteria for inclusion, while there are a few studies from Brazil.
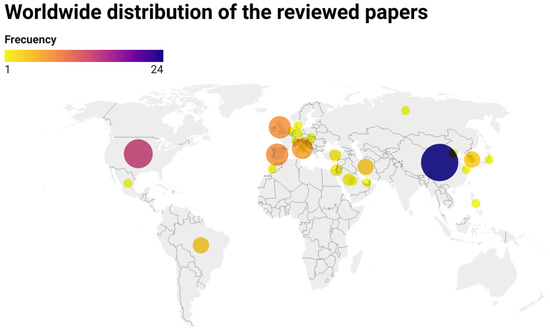
Figure 2.
Country distribution of the corresponding authors of the 220 papers that have been selected for this review. Frequency of country appearance is represented by the color and size of the dot in the figure.
4.2. RQ 1: Characteristics of Dataset Specifications
Sample size is one of the major limitations of the reviewed studies. A large percentage of papers (25%) did not report clearly the size of the dataset. Another large set of papers (40%) reported relatively small datasets with less than 500 subjects included in the study. The studies with dataset sizes in the range 1000 to 5000 samples make up 17% of the papers. Another 15% of the papers reported datasets in the range of 2000 to 10,000 samples. Finally, only 3% of the papers reported datasets with more than 40,000 samples.
Regarding the open access to the data supporting the studies, only 16% of the studies have published the data in open access repositories. Open data access is a cornerstone for open science [131], allowing reproducibility and independent validation of claimed results. In matters of public health, open access to data should be mandatory, also when published results may frame public health policies. However, 40% of the studies indicate that data cannot be shared for various reasons. Finally, the remaining 44% of papers did not give any comment on data availability.
Another critical issue relating datasets to ML training and validation is the class balance. Some studies reported heavily imbalanced datasets (17%). The majority of these works employed SMOTE in order to obtain balanced training data (13%). Some works applied random oversampling (3%), and 1% of papers applied other techniques such as bootstrap resampling. The remaining 83% of studies did report balanced datasets.
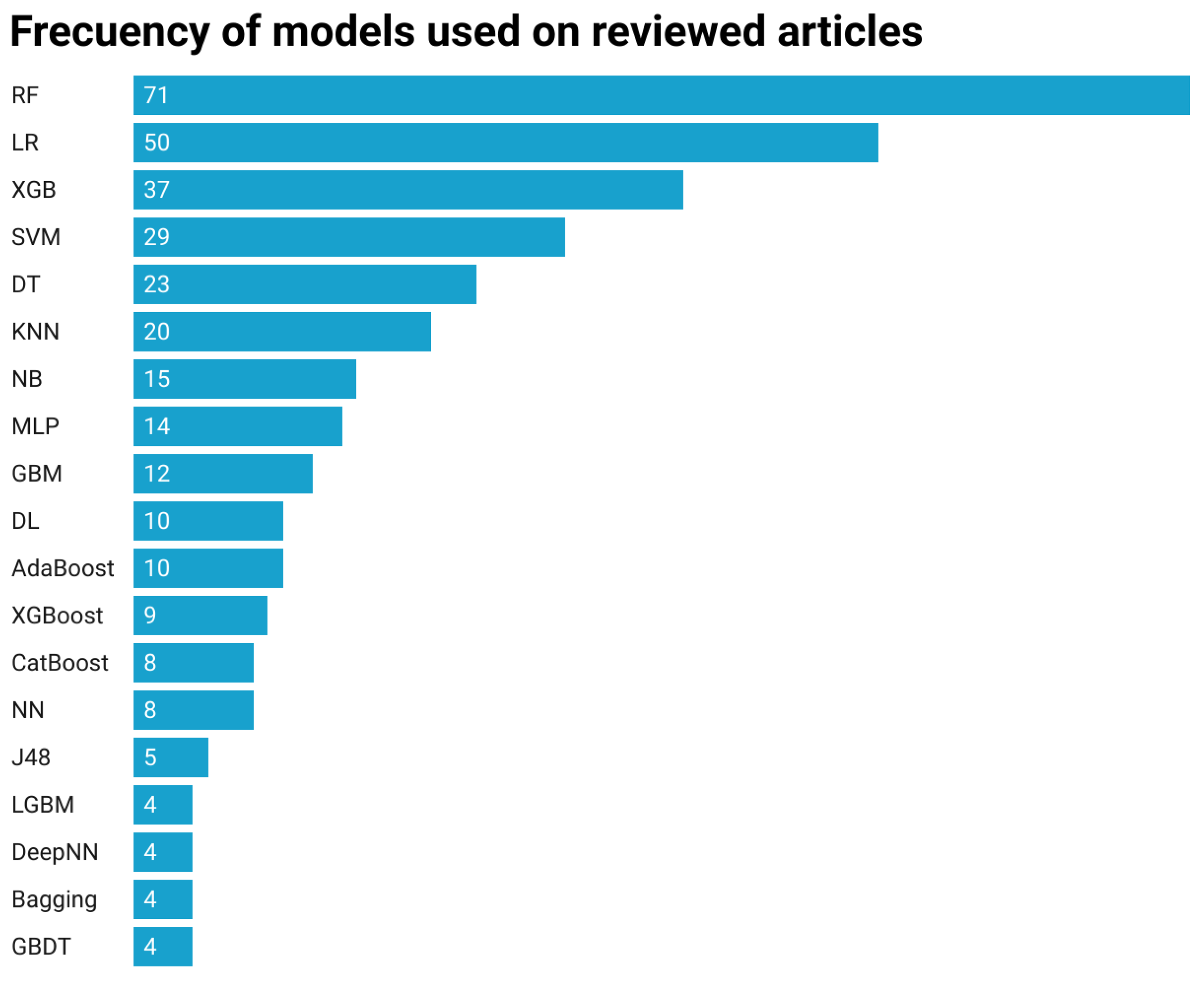
4.3. RQ 2: Machine Learning Algorithms
A majority of the selected studies have benchmarked models in order to achieve the highest accuracy and best performance according to the proposed casuistry. The most frequently used algorithms were Random Forest (RF), Logistic Regression (LR), Gradient Booster (XGB) and Support Vector Machines (SVM) with 18.88%, 13.29%, 9.84% and 7.71% frequency, respectively. These models are also the ones that have achieved the highest overall precision in comparison to the remaining ones. The frequency of appearance of ML algorithms over the selected papers is represented in Figure 3. Many papers did try several algorithms, so that these numbers include overlapping studies.
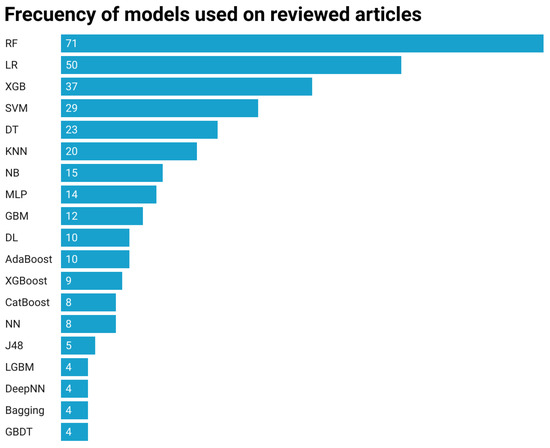
Figure 3.
Number of selected papers reporting results for specific ML algorithms. Acronyms: RF Random Forest, LR Logistic regression, GBM, LGBM, GBDT, XGB, XGBoost and CatBoost are competing implementations of gradient boosting, Adaboost Adaptive Boosting, DT and J48 are implementations of decision trees in R and Weka, respectively, SVM support vector machines, KNN k-nearest neighboor, DL and DeepNN are deep learning implementations, MLP multi-layer perceptron, NB naive Bayes and NN neural network.
Among the reported models, the LR approach is the most deeply rooted in classical statistics. It is a linear regression of a logistic function that can be interpreted as a posterior probability of the positive class; therefore, it allows one to assess the importance of each input variable as an odd ratio and the direction of the influence of the variables, i.e., if rising values increase or decrease the risk. For this reason, many studies applied only LR, also if the aim of the study was to assess the risks of specific factors like age, gender or others. The remaining approaches are ML approaches, which can provide some information on the influence or importance of input variables, but often they cannot provide the direction of the of the influence. The most popular ML algorithm is the well known RF which often provides the best accuracy results and variable importance based on the Gini index for data splits in the tree leaves. Another classical approach is the SVM that has been extensively used in medical studies for predictive model construction. However, it is not easy to assess variable importance from SVM, so this aspect is often omitted in studies exploiting SVMs. Boosting approaches such as Adaboost and diverse flavors of Gradient Boosting have also been popular in COVID-19 studies about clinical decision assistance, reporting sometimes optimal performances but lacking the explanatory ability of variable importance assessment. It is important to notice that diverse ML platforms, such as R packages, Python, Weka or Matlab toolboxes, provide slightly different implementations of the same models that may even appear with different names. In this review, we have not delved into this level of detail, but an exhaustive work of comparison should assess the differences of reported results of diverse implementations over the same datasets. Artificial Neural Networks (ANN), such as the popular Multi Layer Perceptron (MLP) offer a wide spectrum of potential models with many potential differences in hyperparameters and training algorithms. In this study, we found few Deep Learning (DL) approaches because datasets are often small relative to the large datasets required by DL training. Another inconvenience of ANNs is their reduced explainability. Variable importance in ANNs is rather difficult to estimate. In this review, it is not possible to conclude that any of the ML approaches found in the reviewed papers is superior and should be recommended over the remaining approaches.
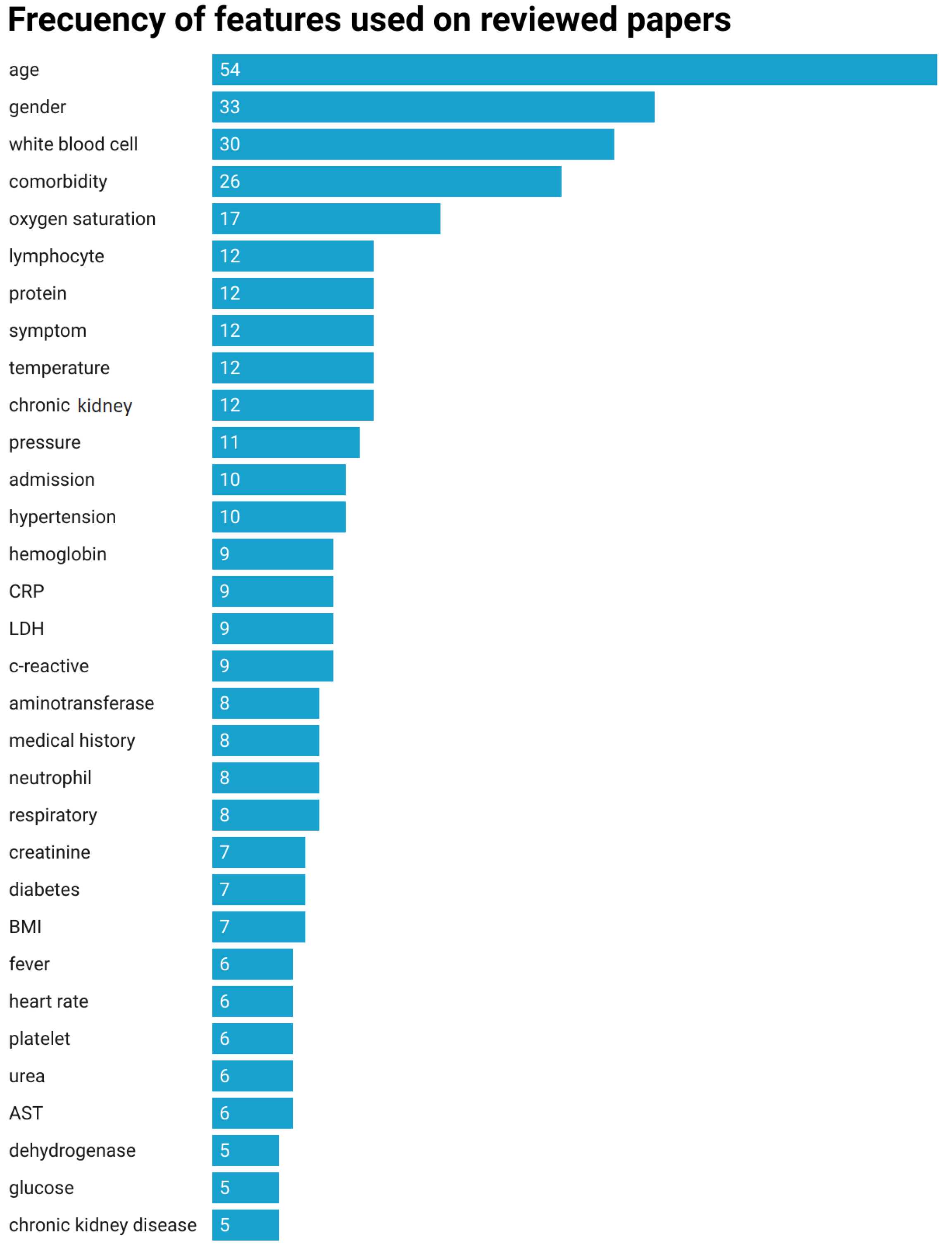
4.4. RQ 3: Features
In some studies, the number of predictors is very high, while others give only the number of predictors without more specifics. Some studies, which have gathered many variables, decided to consider ML approaches to estimate the importance of the variables and thus reduce the dimensionality by some feature-extraction or -selection process. Nonetheless, for the articles that specify the variables employed, their majority did use a common core set of variables. Other variables were usually context-dependent. Age, gender, white blood cell counting, comorbidities and blood oxygen saturation are the most frequently considered predictive variables. The most commonly used features and their respective frequencies of appearance in the studies are presented in Figure 4.
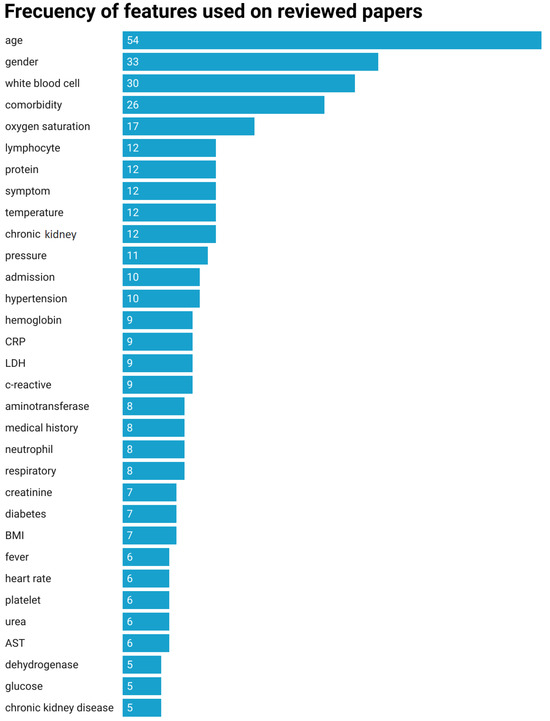
Figure 4.
Distribution of discriminant features over the selected papers.
4.5. RQ 4: Internal and External Validation
Data are often split into two or three datasets (train, validation and test) when it comes to validation of an ML predictive model. In most of the surveyed studies, 70–90% of the data were used to train the models including hyperparameter selection, while the rest served for external testing. Unfortunately, 16% of the studies did not give any information about the validation procedure followed. Although using a third partition of the dataset for internal validation and model hyperparameter selection was predominant, external validation was explicitly mentioned only in ten studies. The most commonly used method for internal validation was k-fold cross validation. Regarding the number of folds, over 60% of the studies reported k = 10, almost 26% of the others reported k = 5, setting k = 20, k = 8 and k = 3 was reported by 2% each and the remaining 9% of studies reported the use of cross validation but did not specify the number of folds used.
4.6. RQ 5: Evaluation Metrics
The metrics used to evaluate the performance of the model were collected and are compared in Table 1, Table 2 and Table 3. Accuracy, F1-score, sensitivity, AUC, specificity and recall were the metrics reported in the studies. Most studies reported accuracy score and AUC, while the least used metric was recall. There is strong variability in the reported results. For instance, the minimum and maximum AUC values reported for models predicting mortality was 0.997 and 0.57, respectively, while accuracy values ranged in the interval [0.56, 0.99].
5. Review of Surveyed Approaches
In this section, we provide a discourse review of the main approaches dealing with the identified critical clinical issues. Table 1, Table 2 and Table 3 provide summary details of the main characteristics of the papers for triage at hospital admission, admission to ICU and death, respectively.
5.1. Patient Triage Methods
The identification of telltale COVID-19 symptoms [132,133,134] and the early warning of COVID-19-positive cases [61,135,136,137] were the first steps towards the management of the disease [138,139,140]; classifying patients according to their severity is the next critical step. Numerous studies have presented models using ML techniques to predict patient outcomes [141] and severity assessment [142,143] in SARS-CoV-2-infected patients in different regions of the world [46,47], preventing severe disease progression while aiming to minimize costs for the patient, the healthcare system and society at large. It was shown that it is possible to discriminate between three states of the patients’ disease evolution and that it is possible to make accurate predictions of a patient’s hospital workload based on statistics concerning age, gender and daily clinical status (critical, severe or moderate) [32,49].
Thus, one of the primary research goals is guiding hospital staff with validated evidence giving advice on the optimal assignment of limited resources while improving patient outcomes [28,50]. Therefore, ML and AI tools have been proposed for the creation of triage assistant systems helping to speed up the decision of the admittance of patients into COVID-19 restricted areas and to determine which patients will require either standard or intensive care [25,37,144,145]. In this spirit, online calculation tools for early patient triage were proposed [29]. Some applications of an ML-based classifier aided in excluding patients regarding their severity within 1 h of hospital admission [30] on the basis of routine information. Some papers [38] reported the extensive comparison of several ML models, such as XGBoost, AdaBoost, RF and ExtraTrees. Some authors reduced the triage problem to a classification of patients into critically ill and non-critically ill in order to prioritize those in immediate need of urgent care [146], some proposing RF models [23] be fed with multimodal data or a variety of algorithms be tested (tree-based, function algorithms and lazy learning algorithms) for this task [42].
Classification of COVID-19 severity into triage categories has was also carried out on clinical data and laboratory tests obtained during patient examination in ED [31] and 26 blood routine indicators and several demographic features [26] using a specifically developed RF-SMA-SVM model. A novel SV-LAR model was exhibited for triage based on blood sample routine data [34], in line with other approaches exploiting blood sample test data for early triage [48]
Some other studies also focused on the differential diagnosis of COVID-19 from other similar diseases or to detect patients with high risk of future lung diseases, such as a diagnostic model to aid in the early identification of suspected COVID-19 pneumonia patients [24] on admission in fever clinics. Others classified the diagnosis of the patients into three categories: COVID-19 pneumonia, non-COVID-19 pneumonia and the healthy ones [43]. Still, another approach [35] proposed a DL-based system for the classification of the severity of pneumonia considering two severity scales. Additional works discriminated between influenza H1N1 and COVID-19 patients [27] using an MLP algorithm.
Many authors work with models predicting severe COVID-19 based on proteomics data [39,40]; in this line of work, C-reactive protein [147,148], LDH [149,150,151], platelets [152,153] and D-dimer [45,154,155] were found to be most associated with predicting the severity of COVID-19.
Another line of research tried to detect different levels of severity risk for COVID-19 patients based on X-ray imaging [33,36,156]. Some authors concluded that using radiological features in conjunction with blood tests, early identification of patients with COVID-19, who are at risk of disease progression, can be achieved on admission to hospital [44]. Furthermore, a prognostic model using imaging data [41] not only predicts the severity of a patient’s illness, but also the time until the patient encounters his or her first critical event.
5.2. Prediction of ICU Admission, Progression and Length of Stay
The coronavirus disease took its toll on healthcare systems around the world, with some patients requiring lengthy general and intensive care. Under the pressure of an unprecedented burden on healthcare systems, there is a need for tools helping decision makers to plan resource allocation at the unit, hospital and national levels, which can be tackled with ML methods [157]. In essence, clinicians will be interested in ML approaches that are able to predict whether patients diagnosed with COVID-19 will require different levels of hospital care (transfer from the basic hospital to ICU) [52,53,158]. For instance, it is desirable to reliably prioritize patients with COVID-19 who are at risk of needing transfer to the ICU within the next 24 h, which has broad implications and utility for clinical practice and hospital operations, on the basis of risks of respiratory failure, shock, inflammation and renal failure in the progression of COVID-19 [59]. Dealing with children [159] is even more difficult, because the very low prevalence of severe COVID-19 means very scarce data. Despite these drawbacks, some researchers demonstrated a DL approach using a large feature set to predict both the risk of hospitalization of infected children and the risk of serious complications in hospitalized pediatric patients [68]. Another line of research deals with the prediction of ICU workload over a short-term time horizon [60] in order to attain optimal resource management.
Extensive evaluations of ML algorithms belonging to nine categories have been reported for prediction of clinical outcomes such as ICU admission or mortality, using data available from the initial COVID-19 detection [160]. Specifically, ICU admission has been predicted on the basis of demographic data [161] and comorbidities [162] and some early symptoms [163]. Accurate assessment of ICU admission, ICU length of stay and mortality of COVID-19 patients for optimal allocation of ICU resources has also been reported [54]. The Explainable Boosting Machine analysis [51] enables one to perform predictive modeling of COVID-19 in the ICU as well as the identification of risk factors. Large and exhaustive clinical databases extracted from the Electronic Health Records (EHR) allow the application of DL approaches to predict the probability of ICU admission and mortality [164]. In a quite different setting, behavioral AI techniques have been also applied to assist intensivists in dealing with the decisions concerning ICU eligibility [77] in Denmark.
ML methods can be used to gain knowledge about complex clinical situations anticipating future complications [74]. In this regard, optimally predicting mortality for COVID-19 patients in the ICU has been reported with DL techniques [63] and ML [58], while decision support tools applicable to critically ill patients with COVID-19 at high risk of 28-day mortality in the ICU allowed assistance in critical decisions such as end-of-life decisions and bed allocation in cases of limited ICU capacity [69]. Furthermore, supervised binary prediction classification using a time-sliding window-based approach to predict the risk of intubation 72 h from the end of the 24 h sampling period has been reported [165]. Multiple studies suggested that adopting early measures to treat patients at risk of deterioration could prevent or decrease status worsening and the need for mechanical ventilation; in this way, reference [67] reports a model that predicts the risk of deterioration for each hour, while the goal of the study in [73] was to monitor patient progression to a score of 5 or more on the WHO Clinical Progression Scale before they require mechanical ventilation.
COVID-19 hospital readmission has been another subject of research interest, due to its impact on the optimal management of hospital services. ML models can successfully predict COVID-19 readmission [65,75,166]. Considering risk factors, these works also categorized cases with a high risk of reinfection in order to classify patients, making the utilization of hospital resources more efficient. Alternatively, other works [55] focused the recovery of COVID-19 patients on dietary adaptation by performing an analysis of the energy intake of different food categories from different countries, comparing several ML algorithms to predict the recovery rate.
Alternatively, the monitoring of patients in need of respiratory support would provide goal-oriented tools for patient risk stratification and an alert system for self-care patients, detecting highly distressing states when resources are possibly constrained. Burdick et al. [57] focused on an ML algorithm to help efficient triage of patients and resource allocation by assessing ventilation needs among COVID-19 patients, achieving a precise prediction of the mechanical ventilation resource needs within 24 h. Bolourani et al. [167] proposed an ML model that predicts respiratory failure within 48 h of ED admission. Izadi et al. [168] aimed to identify patients who may be at increased risk of severe COVID-19 outcomes due to the onset of acute respiratory distress syndrome.
Based primarily on patient age and measures of oxygenation status during the ED stay, it was possible to identify patients with high risk of poor outcomes, i.e., those requiring intensive care, those requiring mechanical ventilation and those with high in-hospital mortality risk [72]. The study of Saadatmand et al. [62] predicted the requirement for oxygen-based treatment for hospitalized COVID-19 patients. Similarly, Aslam [64] identified the impact of particular attributes on the prediction of mortality and mechanical ventilation support [66] in COVID-19 patients. Igarashi et al. [71] introduced a model that can be implemented as a triage tool to detect the need for supplemental oxygen.
Finally, understanding that COVID-19 hospitalization times are often long and may vary substantially from patient to patient, some works [56,70,76] aimed to develop a reliable prediction model of ED length of stay for COVID-19 patients and to identify clinical factors, such as age and comorbidities, associated with ED length of stay. AI techniques have been shown also to predict hospital occupancy [169] and ICU admission [170].
5.3. Mortality Prediction
In the heat of the pandemic years, healthcare professionals often complained of their limitations with respect to determining with some precision the prognosis of patients with COVID-19 from the moment of admission through to subsequent phases. It has been reported that the course of COVID-19 sufferers unexpected changes so that apparently stable patients suddenly worsen. In these situations, even the most experienced clinicians may be unable to adjust and respond in a timely manner to the new situation. Thus, ML and AI models were proposed for clinical decision-making, helping detect complex patterns in large datasets [20,92,171,172]. Several studies have shown the capability of ML-based models to predict mortality at the level of individual patients [108,115,119,121], and the aggregate level of cities [119]. Routine clinical variables have been shown to provide enough predictive power for patient mortality [105,173], while other studies have shown a capacity to predict the mortality of new virus variants [174] or the effect of comorbidities in COVID-19 mortality [120].
Application of AI tools, namely DL architectures, to medical imaging, specifically CT scans, which are the ones more often done on patients with pneumonia complications, have been shown to be useful for the diagnosis and prognosis of diverse lung affections [175,176,177]. This approach also has value as a preliminary screening tool aiming to diminish the workload on hospital staff and reduce the rate of misdiagnosis of patients with COVID-19 [178,179,180]. The enhanced prediction of disease severity via AI on CT images allows improved mortality prediction [126,129,181,182,183,184,185,186,187] and discrimination from other forms of pneumonia not due to SARS-CoV-2 [188,189,190]. Some works [79,117] created a radiomics- and DL-based model showing the robustness of the approach on data from several sites. Moreover, AI allows one to efficiently combine medical imaging information with other sources of clinical and laboratory information [100,106,191]. For instance, Lu et al. [192] demonstrated over CT scan characteristics obtained via AI analysis that there is a positive correlation between blood glucose level on admission and lung lesions.
COVID-19 mortality has also been predicted on the basis of proteomics data. Yasar et al. [87] reported an association of variations in blood proteins with the severity of the patient’s condition. Additionally, Chen et al. [127] developed an ML procedure to find biomarkers that determine disease severity in individual immune cells.
Other approaches use heterogeneous variable selection from several clinical domains. Aznar-Gimeno et al. [109] created an easy-to-use web application that supports rapid decision-making in clinical practice through the construction of a prediction model from a large amount of data from several pandemic waves that predicts ICU admittance and mortality. Garrafa et al. [89] focused on an early warning model based on demographic and clinical variables to predict in-hospital mortality of patients with COVID-19 in the ED. Laino et al. [130] applied ML techniques to guide the management of patients with COVID-19 by developing an accurate in-hospital mortality risk score for COVID-19 based on ten variables. Vezzoli et al. [124] presented a risk score for in-hospital mortality where more severe patients were older, had a lower blood oxygenation, lower creatinine clearance levels and higher prevalence of elevated troponin.
Domínguez-Olmedo et al. [88] developed a model able to predict mortality in patients with COVID-19, which allows one to assess mortality from laboratory values with high precision using the XGBoost model. Sankaranarayanan et al. [96] presented an approach using GRU-D external NN, providing an alert system to flag mortality of COVID-19-positive patients using clinical variables and laboratory results in a 72 h period after the first positive PCR test result. Halasz et al. [78] developed an ML-based score for 30-day mortality prediction in patients with COVID-19 pneumonia. Ko et al. [111] developed an AI model, EDRnet, that forecasts the mortality rate of COVID-19 patients based on 28 blood biomarkers and patient age and sex. Vepa et al. [193] obtained data including age, gender, ethnicity, SPO2, RR, temperature, obesity [18], asthma, diabetes and hypertension, among others, for a period of almost two months. The results suggest that low albumin, elevated (CRP) and older age all correlate with mortality in hospitalized patients.
Some researchers have considered studying the geographic and demographic differences influencing both spread and mortality across geographical locations. Fidan et al. [84] employed clustering techniques to determine cities with similar risk levels, analyzing the incidence of cases and environmental parameters. Guzmán-Torres et al. [194] pointed out that conditions in each country may differ depending on different factors such as the general health status of the people, reporting that the main causes of death in Mexico are related to age, poor eating habits, chronic diseases and contact with infected people who do not have adequate care. Zawbaa et al. [82] proposed a comparison of the spread of the disease among nine different countries, revealing that average young age, hot climate, prevalence of Bacillus Calmette–Guérin (BCG) vaccine and malaria treatment are crucial elements decreasing the mortality impact of the virus.
5.4. Identification of Mortality Risk Factors
Casiraghi et al. [107] reported a system primarily designed to extract the most relevant radiological, clinical and laboratory variables to improve patient risk prediction and subsequently provide decision criteria to clinicians to support patient risk assessment. Dabbah et al. [110] documented several new and significant predictors of mortality in COVID-19; these included detailed anthropometry, acute renal failure, urinary tract infection and pneumonia. In contrast, Baqui et al. [90] considered demographic variables as the most relevant ones, namely the state of residence and its development index, the distance to the hospital (especially for rural and less developed areas), the level of education and the financing model of the hospital, and strain. The model presented by Hu et al. [104] could be valuable for clinicians who have to identify patients at high risk of death, based on age, high-sensitivity C-reactive protein level, lymphocyte count and dimer level, so that interventions can be taken at an earlier stage to reduce the risk of mortality in these patients.
For Sotoudeh et al. [83], the most important features in terms of prediction capacity, out of the many, were SPO2 (LDH), age, BUN, base excess, creatinine and WBC. Mahdavi et al. [80] reported promising results based on a reduced number of features such as SPO2, age and cardiovascular disorders utilizing SVM. The relevance of LDH is also found in the work of Krysko et al. [86], where high levels of LDH, IL-6, IGM, D-dimer, fibrinogen and glucose strongly influences the severity of cases.
Similar to Wang et al. [93] in their finding that lymphocyte and neutrophil levels in peripheral blood could represent prognostic markers indicating early warning implications, Li et al. [99] reported GBDT was revealed as the most effective model in terms of performance whereby leukomonocytes, urea, age and SPO2 turned out to be the most significant predictors. Liptak et al. [118] identified the elevated AST as the most important predictor for COVID-19-related hospitalizations.
Blagojevic et al. [81] focused on detecting the top 10 blood test characteristics that are strongly correlated with patient condition and based on these characteristics predicting the severity and clinical status. Additionally, recent studies have indicated that ferritin level is considered a strong biomarker for the prognosis of SARS-CoV-2 mortality [101], along with other severe respiratory diseases. Another frequently employed variable is the level of blood saturation [112,113,116].
The study of Zhao et al. [103] showed that, combined with the percentage of neutrophils, alanine aminotransferase, gender and albumin would be associated with survival in patients with COVID-19. Age [122,128] and gender [123] appear to be the most significant predictors of mortality [195], but in terms of symptom–comorbidity combinations, Pneumonia–Hypertension, Pneumonia–Diabetes and Acute Respiratory Distress Syndrome (ARDS)–Hypertension showed the most significant associations with COVID-19 mortality [114]. The study by Reina et al. [125] examined the hypothesis that pre-existing conditions (comorbidities) of patients may increase the severity of patients due to SARS-CoV-2.
The C-reactive protein has been consistently implicated in numerous studies as a significant indicator for patient outcome [95,97,98]. This parameter was also taken into consideration by Booth et al. [102], in conjunction with blood urea nitrogen, serum calcium, serum albumin and lactic acid for the prediction of mortality in patients up to 48 h prior to death. Fang et al. [94] crucially considered yroponin, brain natriuretic peptide, white blood cell count, aspartate aminotransferase and creatinine, together with the above-mentioned protein as indicators contributing to malignant progression. The combination of C-reactive protein and advanced age, for example, were the main factors for Di Castelnuovo et al. [91].
5.5. Treatments and Drugs
Given the high cost in time and resources for drug discovery, ML and AI proposed [196,197,198] to accelerate the drug-discovery process by using information about the biological, chemical and spatial properties of compounds and their potential targets; specifically, COVID-19 DL has been studied [199,200,201]. Thus, the COVID-19 pandemic is an opportunity for biotech, pharmaceutical and AI companies to cooperate in accelerating their research and development to identify new and rare drug molecules as well as personalized medicine [202]. Gawriljuk et al. [203] proposed a process of multiple iterations of ML models as a prioritization tool for discovery programs of antiviral drugs against COVID-19. Proteomics analysis of plasma from COVID-19 patients versus controls led via SVM feature selection to the identification of biomarkers, which can be useful for drug targeting and repurposing via in silico protein docking [204]. Some works use indirect information about the drug’s effect, such as features of the images of cells treated with specific drugs [205], so clustering these images may reveal similarities in the mode of action of the drugs. Other indirect information used is the construction of a graph representation of the biological network of COVID-19 that relates to the targets of the virus, making it easy to select the essential proteins in the biological network. In this approach, ref. [206] found five groups of suitable drugs that contain some candidates as potential treatments for COVID-19.
DL approaches have been deployed [207,208] to train the molecular descriptor dataset for robust drug discovery and feature extraction to combat COVID-19. Early on in the pandemic, some research teams focused on building the infrastructure for a global effort in this direction [209,210]. The application of DL approaches over chemical information allows one to obtain high-level representations of instances from a public drug bank database as well as SARS-CoV-2 amino acid sequences predicting affinity scores that agree with the SARS-CoV-2 inhibitors under evaluation at the time of writing the paper [211]. Other authors propose to resort to atomic-level simulation in order to obtain the input for DL approaches [212].
Repurposing is the use of an existing drug, usually a generic and low-cost one, for the treatment of a new disease or a disease different from the one the drug has been approved for. Repurposing current drugs for the treatment of COVID-19 provides a very rapid pathway for potentially effective treatment development [19,213,214,215], both because new drugs are not required to be developed and because, for many existing drugs, safety and efficacy has already been established based on previous trials. For instance, some authors claim that Naive Bayes achieved relatively high accuracy (72%) predicting the efficacy of repurposing drugs for COVID-19 [216]. The analysis was conducted in silico, based on the published sequences of some proteins of the SARS-CoV-2 virus. Thus, they do not take into account the evolution of the virus and the potential for changes in the target proteins. This is a general issue of AI approaches with respect to drug repurposing for COVID-19.
Some authors have compared prediction models of Drug Target Interactions (DTIs), exploiting the public Drugbank database and successfully identify interactions between drugs and proteins in the human cell [217,218]. Jin et al. [219] developed a DL approach using ComboNet for the prediction of chemical synergy against SARS-CoV-2, achieving a test ROC-AUC of 0.82, consisting of an NN architecture that jointly learns drug–target interactions and drug–drug synergy.
Burdick et al. [220] focused on precision medicines, as they may be useful in identifying a sub-population of COVID-19 patients most likely to benefit from hydroxychloroquine treatment in a clinical trial. Zeng et al. [221] utilized a network-based deep-learning methodology for drug repurposing, connecting drugs, diseases, proteins and pathways. The lack of reliable data about the effect of a drug on a new disease was resolved in [208] via a novel data-augmentation approach that exploits results from failed experiments that feed a graph neural network. Su et al. [222] applied multiple nonnegative matrix factorization approaches for feature extraction of virus–drug association, drug chemical structures and virus genome sequences as a preprocessing step for graph neural network processing that obtains drug–virus affinities. A similar matrix-factorization process for feature extraction coupled with graph neural representations was proposed by [223]. Other researchers applied a transfer learning approach [224,225] using a pre-trained DL-based drug–target interaction model to identify commercially available drugs that could act on SARS-CoV-2 viral proteins. Ke et al. [226] proposed a comparison of two models to detect drugs with potential antiviral effects, showing that adequate combination with other drugs at a lower dose of gemcitabine can overcome adverse pulmonary effects while simultaneously inhibiting SARS-CoV-2. Yang et al. [227] reported that Cathepsin L (CTSL) is a protease that can activate the protein that leads to SARS-CoV-2; nevertheless, as there is still a lack of clinically available CTSL inhibitors, they developed a DNN approach to identify small molecules and FDA-approved drugs that can block CTSL activity for drug development and repurposing for COVID-19.
Mekni et al. [228] focused on SVM methodology for the prediction of inhibitory activity of novel chemo-types against SARS-CoV-2, showing an accuracy of 0.88 for later utilization to predict the inhibitory activity of compounds commercially available. Kowalewski et al. [229] identified nasal cavity and respiratory tract conditions as a bottleneck for this infection, trained ML models to predict inhibitory activity and screened over 100,000 approved drugs and more than 14 million purchasable chemicals for potential candidates for new inhaled therapies. Alternatively, Pinto et al. [230] used multivariate statistical methods to select the most suitable candidates to inhibit the disease.
Finally, further clinical trials may depend on biomedical information obtained from existing data and find patterns and signatures in the underlying molecular biology of the COVID-19 mechanism and ML may have a prominent role in the design of new trials [231].
6. Discussion
- DQ1.
- Are predictive models capable of supporting a COVID-19 outbreak and how?
ML algorithms can neither be adequately trained nor validated without a large and well curated clinical dataset. In the early stages of an emerging infectious disease, collected data will often be noisy and incomplete. Although there may not be a large historical dataset of patients suffering from this disease, existing databases, assuming they have been properly mined, and patterns based on these data can contribute significantly to the choice of the most appropriate behaviour to adopt in each situation [232]. Many studies report the potential of the application of Big Data and AI technology to contribute to prevention, diagnosis, treatment and decision making concerning acute infectious public health events in the future. According to some authors, the COVID-19 pandemic has provided an excellent opportunity to integrate AI tools in clinical care, already introducing changes in hospital practices [233] in some advanced countries.
- DQ2.
- Are there demographic and cultural factors influencing the development of predictive methods to confront or address COVID-19?
Although most of the articles added to this study deal with data from Asian patients, there are several articles from European and American countries. In comparing these studies, while many utilise similar variables, cultural or demographic factors have been revealed to significantly affect the detection or increase in disease contraction, demonstrating the importance of these factors in the COVID-19 outbreak [173]. In addition, key genetic markers may serve as potential targets in the clinical prognosis and treatment of COVID-19.
- DQ3.
- Are there models with good performance capable of categorizing patients according to severity?
ML has proven its importance in nearly all domains and its techniques are being actively used against COVID-19 by researchers with satisfactory results [234]. Among all the articles collected in this study, various studies with very promising results have been reported. Most of the selected studies employed predictive referenced models to achieve the highest accuracy and best performance according to the proposed casuistry. Among all reported metrics with successful results, there are several studies that have achieved accuracy and AUC above 0.99 [27,35,60], showing high sensitivity values so that the most severe cases may not easily go unnoticed and can be detected in time. These are studies that use MLP, ResNet50 or RF models and obtain very good results with demographic and clinical variables, without the need for laboratory tests or CT images, which are variable and more difficult to obtain and collect.
- DQ4.
- Is translation possible from scientific research to clinical practice with the current data on the disease obtained during the pandemic?
Datasets used for diagnosis, prediction and prevention of COVID-19 are essentially classified into medical imaging datasets, speech-based datasets and textual datasets. On the one hand, medical imaging datasets, i.e., CT images, are mainly analyzed for automatic diagnosis, segmentation and augmentation of COVID-19. On the other hand, textual data support prediction and analysis of COVID-19 cases, surveying patient status, interventions and treatments.
Based on the study, developed models addressing COVID-19 through intelligent approaches generate reliable performance results if high fidelity and abundant data are involved. It is clear that large datasets are not typically used for the majority of the use cases previously specified. Despite the fact that some public datasets are available to work with this type of caseload, given the recent emergence of the disease and the lack of many years of study, the size of these datasets is limited compared to the requirements of ML approaches.
Data accessibility and openness is considered a critical bottleneck in COVID-19 research as a result of the rapid spread. Being able to apply such applications in the real world will only be possible with the availability of more open source data. This is considered one of the limitations to be addressed in order to further improve COVID-19 research.
This limitation primarily stems from the segregation of data at national, regional, hospital and departmental levels. Hence, the development of a central and uniform platform for investigators for sharing and accessing data would be a promising starting point. In addition to having erroneous or unstructured data, the datasets have a lot of noise and null values. Therefore, filtering, cleaning and noise reduction are other key challenges for the successful implementation of models developed using intelligent approaches.
A further consideration that must be addressed is the establishment of certain protocols or standards for data collection in healthcare facilities. As well as having erroneous or unstructured data, the datasets have a lot of noise and missing values. Therefore, filtering, cleaning and noise reduction are other important challenges to be considered for the creation of applications using intelligent approaches.
7. Insights into ML/AI Advances, Research Directions and Challenges
At the request of reviewers, we introduce here some thoughts about the future of ML/AI applications in clinical decision support for COVID-19 and other future pandemics. Modern ML and AI techniques are data driven; thus, the main and foremost issue in the usefulness of ML/AI techniques is the availability of large high-quality datasets. It is impossible to over-stress the importance of good data-gathering practices for the development of ML/AI support to the response to forthcoming pandemics. In contrast, the price to be paid by complacency and missing opportunities for implementation of strong data-gathering protocols will be a greater economic disruption and poorer health outcomes, i.e., more deaths. Current Electronic Health Record (EHR) systems are dispersed and do not interoperate outside some small clusters developed by the same company. Hence, international standards for EHR should be enforced as well as data-gathering protocols and open access to data in order to allow for cooperative analysis of data in order to raise alarms and to produce timely predictive models and risk assessments. Data access should not be blocked by commercial interests in the name of data privacy when it is most needed for democratic public health management. With the exception of some prominent personages, health data are easily anonymized to a level that impedes spurious uses.
Regarding ML/AI models, we think that LR will remain one of the most used models in the future, because its foundations are well understood and it has high explanatory value. Medical practitioners are well acquainted with the technique and they accept it with critical appraisal. Other statistical ML models, such as RF, SVM or gradient boosting approaches, do not provide a similar degree of explanations. They can be of value in some specific problems in order to provide more accurate predictions once the risk assessment has been well established. The availability of large datasets may allow the training of large neural network models, i.e., deep learning (DL) architectures, but still the explanatory capabilities of these approaches are limited and need to be improved. DL approaches seem better suited to signal processing and medical image processing, but their integration with clinical models requires additional research to achieve translation into the clinical practice. The recent large language models (LLMs) may provide such a link between the image-processing DL models and the clinical practice by producing explanations of findings that can be used by clinicians. In the emergence of a pandemic, this automated fast-track analysis of multi-source multi-modal data should provide a fast response to the new characteristics of healthcare needed for the pandemic. Well curated EHRs should be an invaluable source of data and qualitative information to train such models in the detection of new alarms and the generation of innovative solutions to face them.
8. Conclusions
Our review can lead to the conclusion that there is not a definitive ML approach for COVID-19 clinical decision assistance and that translation to clinical practice has not been demonstrated. Supporting this conclusion are the following facts: (a) there was a large variability in the methodological specifics for validation, with almost no intersite data considered; (b) the majority of studies treated small local datasets, which were not publicly available for reproducibility assessment; (c) findings and conclusions were often in contradiction when comparing studies, so that no solid grounds were laid after so much work; (d) there is extensive bias of selection in the studies as a major cause of the previous fact; (e) there is growing evidence of high variability in how the disease was diagnosed, treated and followed up on, which induces great uncertainties in the definition of the target variables; specifically, death with or by COVID-19 appears to need careful revision; (f) the disease presentation has been evolving in time; thus, predictive models can quickly become obsolete; (g) the actual code of the models is often not shared, even if the underlying tools are fairly standard; the lack of hyperparameter values may obscure reproducibility; (h) there is a high variability between studies of the considered predictive variables, leading to a wide diversity of biomarkers, though some like age are (almost) universally recognized.
Moreover, many of the reviewed studies dealt with sensitive personal data, which, even during a pandemic, must be carefully handled [235]. Therefore, this emergency situation has been a precious opportunity to behave in a more ethical and more responsible manner [232]. A limitation of our review is that it is almost impossible to cover all the (still) continuously appearing publications, which range in the tens of thousands. Most of the studies reviewed did include the gender variable in the data collection, often as the male/female dichotomy; however, there was not a systematic assessment of the gender effects of the pandemic or differential risks due to gender. A large epidemiological study should tackle this issue, which has only been raised partially in some papers.
As the concluding message from this review, the COVID-19 pandemic has shown that there is a strong need to standardize medical data gathering and statistical methodology, including both clinicians and policy makers in the loop, because data have been found in most of the studies to be sketchy and noisy, to the extent that such low quality of data may be considered one of the main limitations to the translation of existing ML and AI models to clinical practice. Moreover, methodological inconsistencies also impede the integration of ML approaches needed for this translation.
Author Contributions
Conceptualization, M.G., J.M.L.-G., J.E. and G.B.-Z.; methodology, M.G. and G.B.-Z.; formal analysis, M.G., G.B.-Z. and J.E.; investigation, G.B.-Z.; writing—original draft preparation, G.B.-Z. and J.M.L.-G.; writing—review and editing, M.G. and J.E. All authors have read and agreed to the published version of the manuscript.
Funding
The first author received research funds from the Basque Government as the head of the Grupo de Inteligencia Computacional, Universidad del Pais Vasco, UPV/EHU, from 2007 until 2025. The current code for the grant is IT1689-22. Additionally, the author participates in Elkartek project KK-2022/00051. The Spanish MCIN has also granted the authors a research project under code PID2020-116346GB-I00.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflict of interest.
Nomenclature
| Acronym | Definition |
| ML | Machine Learning |
| AI | Artificial Intelligence |
| DL | Deep learning |
| ICU | Intensive Care Unit |
| ED | Emergency Department |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analysis |
| XGB | Extreme Gradient Boosting |
| MLP | Multilayer Perceptron |
| RF | Random Forest |
| LR | Logistic Regression |
| KNN | K-Nearest neighbor |
| GBDT | Gradient Boosting Decision Tree |
| NN | Neural Network |
| DNN | Deep Neural Network |
| DT | Decision Tree |
| NB | Naive Bayes |
| SVM | Support Vector Machine |
| SGD | Stochastic Gradient Descent |
| LGBM | Light GB Machine |
| SGD | Stochastic Gradient Descent |
| ORL | Ordinal Logistic Regression |
| LWL | Locally Weighted Learning |
| AUC | Area Under Curve |
| LDH | lactate dehydrogenase |
| CTSL | Cathepsin L |
| DTI | Drug–target interaction |
| IPD | inpatient mortality probabilities |
| CRP | C-Reactive Protein |
| PCR | Polymerase Chain Reaction |
| PUI | persons under investigation |
| CT | Computerized tomography |
| AST | aspartate transaminase |
| BUN | blood urea nitrogen |
| WBC | white blood cell |
| IGM | gamma interferon-induced monokine |
| SPO2 | Oxygen saturation |
| RR | Respiratory Rate |
| SBP | Systolic Blood pressure |
| DBP | Diastolic Blood Pressure |
| IL-6 | Interleukin 6 |
| LOS | Length of Stay |
References
- Liu, Y.; Gayle, A.; Wilder-Smith, A.; Rocklöv, J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J. Travel Med. 2020, 27, taaa021. [Google Scholar] [CrossRef] [PubMed]
- Dong, J.; Wu, H.Q.; Zhou, D.; Li, K.; Zhang, Y.; Ji, H.; Tong, Z.; Lou, S.; Liu, Z. Application of Big Data and Artificial Intelligence in COVID-19 Prevention, Diagnosis, Treatment and Management Decisions in China. J. Med. Syst. 2021, 45, 84. [Google Scholar] [CrossRef] [PubMed]
- Alafif, T.; Tehame, A.; Bajaba, S.; Barnawi, A.; Zia, S. Machine and Deep Learning towards COVID-19 Diagnosis and Treatment: Survey, Challenges and Future Directions. Int. J. Environ. Res. Public Health 2021, 18, 1117. [Google Scholar] [CrossRef]
- Baby, S.T.; Xavier, S.B.; Kathrine, G.J.W. Prediction of Diabetes and Symptoms of COVID-19 Using Machine Learning Classifiers. In Proceedings of the 2022 International Conference on Applied Artificial Intelligence and Computing (ICAAIC), Salem, India, 9–11 May 2022; pp. 387–393. [Google Scholar] [CrossRef]
- Unberath, M.; Ghobadi, K.; Levin, S.; Hinson, J.; Hager, G.D. Artificial Intelligence-Based Clinical Decision Support for COVID-19-Where Art Thou? Adv. Intell. Syst. 2020, 2, 2000104. [Google Scholar] [CrossRef]
- Majumder, J.; Minko, T. Recent Developments on Therapeutic and Diagnostic Approaches for COVID-19. AAPS J. 2021, 23, 14. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, Q.; Inchakalody, V.P.; Merhi, M.; Mestiri, S.; Taib, N.; Moustafa Abo El-Ella, D.; Bedhiafi, T.; Raza, A.; Al-Zaidan, L.; Mohsen, M.O.; et al. Emerging COVID-19 variants and their impact on SARS-CoV-2 diagnosis, therapeutics and vaccines. Ann. Med. 2022, 54, 524–540. [Google Scholar] [CrossRef]
- Yüce, M.; Filiztekin, E.; Özkaya, K.G. COVID-19 diagnosis—A review of current methods. Biosens. Bioelectron. 2021, 172, 112752. [Google Scholar] [CrossRef]
- Popkin, B.M.; Du, S.; Green, W.D.; Beck, M.A.; Algaith, T.; Herbst, C.H.; Alsukait, R.F.; Alluhidan, M.; Alazemi, N.; Shekar, M. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes. Rev. 2020, 21, e13128. [Google Scholar] [CrossRef]
- Huang, Y.; Lu, Y.; Huang, Y.M.; Wang, M.; Ling, W.; Sui, Y.; Zhao, H.L. Obesity in patients with COVID-19: A systematic review and meta-analysis. Metabolism 2020, 113, 154378. [Google Scholar] [CrossRef]
- Fernández Villalobos, N.V.; Ott, J.J.; Klett-Tammen, C.J.; Bockey, A.; Vanella, P.; Krause, G.; Lange, B. Effect modification of the association between comorbidities and severe course of COVID-19 disease by age of study participants: A systematic review and meta-analysis. Syst. Rev. 2021, 10, 194. [Google Scholar] [CrossRef]
- Romero Starke, K.; Petereit-Haack, G.; Schubert, M.; Kämpf, D.; Schliebner, A.; Hegewald, J.; Seidler, A. The Age-Related Risk of Severe Outcomes Due to COVID-19 Infection: A Rapid Review, Meta-Analysis and Meta-Regression. Int. J. Environ. Res. Public Health 2020, 17, 5974. [Google Scholar] [CrossRef] [PubMed]
- Romero Starke, K.; Reissig, D.; Petereit-Haack, G.; Schmauder, S.; Nienhaus, A.; Seidler, A. The isolated effect of age on the risk of COVID-19 severe outcomes: A systematic review with meta-analysis. BMJ Glob. Health 2021, 6, e006434. [Google Scholar] [CrossRef] [PubMed]
- Gomes, R.; Kamrowski, C.; Langlois, J.; Rozario, P.; Dircks, I.; Grottodden, K.; Martinez, M.; Tee, W.Z.; Sargeant, K.; LaFleur, C.; et al. A Comprehensive Review of Machine Learning Used to Combat COVID-19. Diagnostics 2022, 12, 1853. [Google Scholar] [CrossRef] [PubMed]
- Abirami, R.S.; Kumar, G.S. Comparative Study Based on Analysis of Coronavirus Disease (COVID-19) Detection and Prediction Using Machine Learning Models. SN Comput. Sci. 2021, 3, 79. [Google Scholar] [CrossRef] [PubMed]
- John, C.C.; Ponnusamy, V.; Krishnan Chandrasekaran, S.; Nandakumar, R. A Survey on Mathematical, Machine Learning and Deep Learning Models for COVID-19 Transmission and Diagnosis. IEEE Rev. Biomed. Eng. 2022, 15, 325–340. [Google Scholar] [CrossRef] [PubMed]
- Ahsan, M.M.; Luna, S.A.; Siddique, Z. Machine-Learning-Based Disease Diagnosis: A Comprehensive Review. Healthcare 2022, 10, 541. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Cui, Z.; Ma, X.; Pan, F.; Li, L.; Wang, J.; Sun, P.; Li, H.; Yang, L.; Liang, B. The association of obesity with the progression and outcome of COVID-19: The insight from an artificial-intelligence-based imaging quantitative analysis on computed tomography. Diabetes/Metab. Res. Rev. 2022, 38, e3519. [Google Scholar] [CrossRef]
- Mohanty, S.; Harun Al Rashid, M.; Mridul, M.; Mohanty, C.; Swayamsiddha, S. Application of Artificial Intelligence in COVID-19 drug repurposing. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1027–1031. [Google Scholar] [CrossRef]
- Suri, J.; Puvvula, A.; Majhail, M.; Biswas, M.; Jamthikar, A.; Saba, L.; Faa, G.; Singh, I.; Oberleitner, R.; Turk, M.; et al. Integration of cardiovascular risk assessment with COVID-19 using artificial intelligence. Rev. Cardiovasc. Med. 2020, 21, 541–560. [Google Scholar] [CrossRef]
- Yadollahi, S.; Yadollahi, S.; Zanjani, E.; Khaleghi, F. Application of machine learning and medical imaging in the detection of COVID-19 patients: A review article. J. Family Med. Prim. Care 2022, 11, 2277–2283. [Google Scholar]
- Bhosale, Y.H.; Patnaik, K.S. Application of Deep Learning Techniques in Diagnosis of COVID-19 (Coronavirus): A Systematic Review. Neural Process. Lett. 2022, 55, 1–53. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Ouyang, L.; Bao, F.S.; Li, Q.; Han, L.; Zhang, H.; Zhu, B.; Ge, Y.; Robinson, P.; Xu, M.; et al. A Multimodality Machine Learning Approach to Differentiate Severe and Nonsevere COVID-19: Model Development and Validation. J. Med. Internet Res. 2021, 23, e23948. [Google Scholar] [CrossRef] [PubMed]
- Feng, C.; Wang, L.; Chen, X.; Zhai, Y.; Zhu, F.; Chen, H.; Wang, Y.; Su, X.; Huang, S.; Tian, L.; et al. A novel artificial intelligence-assisted triage tool to aid in the diagnosis of suspected COVID-19 pneumonia cases in fever clinics. Ann. Transl. Med. 2021, 9, 201. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; Bai, Y.; Chen, D.; He, L.; Zhu, J.; Ding, X.; Luo, L.; Ren, Y.; Xing, H.; Jin, X.; et al. Accurate classification of COVID19 patients with different severity via machine learning. Clin. Transl. Med. 2021, 11, e323. [Google Scholar] [CrossRef]
- Wu, P.; Ye, H.; Cai, X.; Li, C.; Li, S.; Chen, M.; Wang, M.; Heidari, A.A.; Chen, M.; Li, J.; et al. An Effective Machine Learning Approach for Identifying Non-Severe and Severe Coronavirus Disease 2019 Patients in a Rural Chinese Population: The Wenzhou Retrospective Study. IEEE Access 2021, 9, 45486–45503. [Google Scholar] [CrossRef]
- Elbaşi, E.; Zreikat, A.; Mathew, S.; Topcu, A. Classification of influenza H1N1 and COVID-19 patient data using machine learning. In Proceedings of the 2021 44th International Conference on Telecommunications and Signal Processing (TSP), Brno, Czech Republic, 26–28 July 2021. [Google Scholar] [CrossRef]
- Marcos, M.; Belhassen-Garcia, M.; Sanchez Puente, A.; Sampedro-Gomez, J.; Azibeiro, R.; Dorado-Díaz, P.I.; Marcano-Millán, E.; Garcia-Vidal, C.; Moreiro-Barroso, M.T.; Cubino-Bóveda, N.; et al. Development of a severity of disease score and classification model by machine learning for hospitalized COVID-19 patients. PLoS ONE 2021, 16, e0240200. [Google Scholar] [CrossRef] [PubMed]
- Liang, W.; Yao, J.; Chen, A.; Lv, Q.; Zanin, M.; Liu, J.; Wong, S.; Li, Y.; Lu, J.; Liang, H.; et al. Early triage of critically ill COVID-19 patients using deep learning. Nat. Commun. 2020, 11, 3543. [Google Scholar] [CrossRef]
- Soltan, A.; Kouchaki, S.; Zhu, T.; Kiyasseh, D.; Taylor, T.; Hussain, Z.B.; Peto, T.; Brent, A.J.; Eyre, D.W.; Clifton, D.A. Rapid triage for COVID-19 using routine clinical data for patients attending hospital: Development and prospective validation of an artificial intelligence screening test. Lancet Digit. Health 2020, 3, e78–e87. [Google Scholar] [CrossRef]
- Benito-León, J.; Del Castillo, M.; Estirado, A.; Ghosh, R.; Dubey, S.; Serrano, J.I. Using Unsupervised Machine Learning to Identify Age- and Sex-Independent Severity Subgroups Among Patients with COVID-19: Observational Longitudinal Study. J. Med. Internet Res. 2021, 23, e25988. [Google Scholar] [CrossRef]
- Subudhi, S.; Verma, A.; Patel, A. Prognostic machine learning models for COVID-19 to facilitate decision making. Int. J. Clin. Pract. 2020, 74, e13685. [Google Scholar] [CrossRef]
- Sayed, S.; Elkorany, A.; Sayed, S. Applying Different Machine Learning Techniques for Prediction of COVID-19 Severity. IEEE Access 2021, 9, 135697–135707. [Google Scholar] [CrossRef]
- Darapaneni, N.; Gupta, M.; Paduri, A.; Agrawal, R.; Padasali, S.; Kumari, A.; Purushothaman, P. A Novel Machine Learning Based Screening Method For High-Risk COVID-19 Patients Based On Simple Blood Exams. In Proceedings of the 2021 IEEE International IOT, Electronics and Mechatronics Conference (IEMTRONICS), Toronto, ON, Canada, 21–24 April 2021; pp. 1–6. [Google Scholar] [CrossRef]
- La Salvia, M.; Secco, G.; Torti, E.; Florimbi, G.; Guido, L.; Lago, P.; Salinaro, F.; Perlini, S.; Leporati, F. Deep Learning and Lung UltraSound for COVID-19 pneumonia detection and severity classification. Comput. Biol. Med. 2021, 136, 104742. [Google Scholar] [CrossRef]
- Udristoiu, A.L.; Ghenea, A.; Udristoiu, S.; Neaga, M.; Zlatian, O.; Vasile, C.; Popescu, M.; Eugen, T.; Salan, A.; Turcu, A.; et al. COVID-19 and Artificial Intelligence: An Approach to Forecast the Severity of Diagnosis. Life 2021, 11, 1281. [Google Scholar] [CrossRef]
- Quiroz-Juárez, M.A.; torres Gómez, A.; Hoyo-Ulloa, I.; de J. León-Montiel, R.; U’Ren, A.B. Identification of high-risk COVID-19 patients using machine learning. PLoS ONE 2021, 16, e0257234. [Google Scholar] [CrossRef]
- Laatifi, M.; Douzi, S.; Bouklouz, A.; Ezzine, H.; Jaafari, J.; Younes, Z.; Ouahidi, B.; Naciri, M. Machine learning approaches in COVID-19 severity risk prediction in Morocco. J. Big Data 2022, 9, 5. [Google Scholar] [CrossRef]
- Xiong, Y.; Ma, Y.; Ruan, L.; Li, D.; Lu, C.; Huang, L. Comparing different machine learning techniques for predicting COVID-19 severity. Infect. Dis. Poverty 2022, 11, 19. [Google Scholar] [CrossRef] [PubMed]
- Moulaei, K.; Shanbehzadeh, M.; Mohammadi-Taghiabad, Z.; Kazemi-Arpanahi, H. Comparing machine learning algorithms for predicting COVID-19 mortality. BMC Med. Inform. Decis. Mak. 2022, 22, 2. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.; Choi, J.W.; Jiao, Z.; Wang, D.; Wu, J.; Yi, T.; Halsey, K.; Eweje, F.; Tran, L.; Liu, C.; et al. An automated COVID-19 triage pipeline using artificial intelligence based on chest radiographs and clinical data. NPJ Digit. Med. 2022, 5, 5. [Google Scholar] [CrossRef] [PubMed]
- Huyut, M. Automatic Detection of Severely and Mildly Infected COVID-19 Patients with Supervised Machine Learning Models. IRBM 2022, 44, 100725. [Google Scholar] [CrossRef] [PubMed]
- Nishio, M.; Kobayashi, D.; Nishioka, E.; Matsuo, H.; Urase, Y.; Onoue, K.; Ishikura, R.; Kitamura, Y.; Sakai, E.; Tomita, M.; et al. Deep learning model for the automatic classification of COVID-19 pneumonia, non-COVID-19 pneumonia and the healthy: A multi-center retrospective study. Sci. Rep. 2022, 12, 8214. [Google Scholar] [CrossRef] [PubMed]
- Yuan, L.; Chen, J.; Feng, H.; Lv, J.; Lu, X.; Ji, M. Early Identification of COVID-19 Progression to Its Severe Form Using Artificial Intelligence. Iran. J. Radiol. 2022, 19, e112562. [Google Scholar] [CrossRef]
- Fu, Y.; Zhong, W.; Liu, T.; Li, J.; Xiao, K.; Ma, X.; Xie, L.; Jiang, J.; Zhou, H.; Liu, R.; et al. Early Prediction Model for Critical Illness of Hospitalized COVID-19 Patients Based on Machine Learning Techniques. Front. Public Health 2022, 10, 880999. [Google Scholar] [CrossRef] [PubMed]
- Park, M.; Jo, H.; Lee, H.; Jung, S.Y.; Hwang, H. Machine Learning-Based COVID-19 Patients Triage Algorithm Using Patient-Generated Health Data from Nationwide Multicenter Database. Infect. Dis. Ther. 2022, 11, 787–805. [Google Scholar] [CrossRef] [PubMed]
- Song, W.; Zhang, L.; Liu, L.; Sainlaire, M.; Karvar, M.; Kang, M.J.; Pullman, A.; Lipsitz, S.; Massaro, A.; Patil, N.; et al. Predicting Hospitalization of COVID-19 Positive Patients Using Clinician-guided Machine Learning Methods. J. Am. Med. Inform. Assoc. 2022, 29, 1661–1667. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Kim, G.W.; Seok, H.; Shin, H.J.; Lee, D.H. Early Triage of COVID-19 patients exploiting Data-Driven Strategies and Machine Learning Techniques. In Proceedings of the 2022 International Conference on Electronics, Information and Communication (ICEIC), Jeju, Republic of Korea, 6–9 February 2022; pp. 234–237. [Google Scholar] [CrossRef]
- Roimi, M.; Gutman, R.; Somer, J.; Arie, A.; Calman, I.; Bar Lavie, Y.; Gelbshtein, U.; Liverant-Taub, S.; Ziv, A.; Eytan, D.; et al. Development and validation of a machine learning model predicting illness trajectory and hospital utilization of COVID-19 patients: A nationwide study. J. Am. Med. Inform. Assoc. 2021, 28, 1188–1196. [Google Scholar] [CrossRef] [PubMed]
- Migrino, J.; Batangan, A. Using machine learning to create a decision tree model to predict outcomes of COVID-19 cases in the Philippines. West. Pac. Surveill. Response 2021, 12, 56. [Google Scholar] [CrossRef]
- Magunia, H.; Lederer, S.; Verbuecheln, R.; Gilot, B.; Koeppen, M.; Haeberle, H.; Mirakaj, V.; Hofmann, P.; Marx, G.; Bickenbach, J.; et al. Machine learning identifies ICU outcome predictors in a multicenter COVID-19 cohort. Crit. Care 2021, 25, 295. [Google Scholar] [CrossRef]
- Hernández-Pereira, E.; Fontenla-Romero, O.; Bolón-Canedo, V.; Cancela, B.; Guijarro-Berdiñas, B.; Alonso-Betanzos, A. Machine learning techniques to predict different levels of hospital care of COVID-19. Appl. Intell. 2021, 52, 6413–6431. [Google Scholar] [CrossRef]
- Podder, P.; Mondal, M.R. Machine Learning to Predict COVID-19 and ICU Requirement. In Proceedings of the 2020 11th International Conference on Electrical and Computer Engineering (ICECE), Dhaka, Bangladesh, 17–19 December 2020. [Google Scholar] [CrossRef]
- Dan, T.; Li, Y.; Zhu, Z.; Chen, X.; Quan, W.; Hu, Y.; Tao, G.; Zhu, L.; Zhu, J.; Jin, Y.; et al. Machine Learning to Predict ICU Admission, ICU Mortality and Survivors’ Length of Stay among COVID-19 Patients: Toward Optimal Allocation of ICU Resources. In Proceedings of the 2020 IEEE International Conference on Bioinformatics and Biomedicine (BIBM), Seoul, Republic of Korea, 16–19 December 2020. [Google Scholar] [CrossRef]
- Hossen, M.; Karmoker, D. Predicting the Probability of COVID-19 Recovered in South Asian Countries Based on Healthy Diet Pattern Using a Machine Learning Approach. In Proceedings of the 2020 2nd International Conference on Sustainable Technologies for Industry 4.0 (STI), Dhaka, Bangladesh, 19–20 December 2020; pp. 1–6. [Google Scholar] [CrossRef]
- Mahboub, B.; Albataineh, M.; Alshraideh, H.; Hamoudi, R.; Salameh, L.; Shamayleh, A. Prediction of COVID-19 Hospital Length of Stay and Risk of Death Using Artificial Intelligence-Based Modeling. Front. Med. 2021, 8, 592336. [Google Scholar] [CrossRef]
- Burdick, H.; Lam, C.; Mataraso, S.; Lynn-Palevsky, A.; Braden, G.; Dellinger, R.; McCoy, A.; Vincent, J.L.; Green-Saxena, A.; Barnes, G.; et al. Prediction of respiratory decompensation in COVID-19 patients using machine learning: The READY trial. Comput. Biol. Med. 2020, 124, 103949. [Google Scholar] [CrossRef] [PubMed]
- Pan, P.; Li, Y.; Xiao, Y.; Han, B.; Su, L.; Su, M.; Li, Y.; Zhang, S.; Jiang, D.; Chen, X.; et al. Prognostic Assessment of COVID-19 in the Intensive Care Unit by Machine Learning Methods: Model Development and Validation. J. Med. Internet Res. 2020, 22, e23128. [Google Scholar] [CrossRef]
- Cheng, F.Y.; Joshi, H.; Tandon, P.; Freeman, R.; Reich, D.; Mazumdar, M.; Kohli-Seth, R.; Levin, M.; Timsina, P.; Kia, A. Using Machine Learning to Predict ICU Transfer in Hospitalized COVID-19 Patients. J. Clin. Med. 2020, 9, 1668. [Google Scholar] [CrossRef] [PubMed]
- Lorenzen, S.; Nielsen, M.; Jimenez-Solem, E.; Petersen, T.; Perner, A.; Thorsen-Meyer, H.C.; Igel, C.; Sillesen, M. Using machine learning for predicting intensive care unit resource use during the COVID-19 pandemic in Denmark. Sci. Rep. 2021, 11, 18959. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.S.; Hou, Y.; Vasovic, L.V.; Steel, P.; Chadburn, A.; Racine-Brzostek, S.E.; Velu, P.; Cushing, M.M.; Loda, M.; Kaushal, R.; et al. Routine laboratory blood tests predict SARS-CoV-2 infection using machine learning. medRxiv 2020. [Google Scholar] [CrossRef] [PubMed]
- Saadatmand, S.; Salimifard, K.; Mohammadi, R.; Marzban, M.; Naghibzadeh tahami, A. Predicting the necessity of oxygen therapy in the early stage of COVID-19 using machine learning. Med. Biol. Eng. Comput. 2022, 60, 957–968. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Sollee, J.; Hsieh, C.; Vandal, N.; Shanahan, J.; Choi, J.W.; Tran, L.; Halsey, K.; Iheanacho, F.; Warren, J.; et al. COVID-19 mortality prediction in the intensive care unit with deep learning based on longitudinal chest X-rays and clinical data. Eur. Radiol. 2022, 32, 4446–4456. [Google Scholar] [CrossRef] [PubMed]
- Aslam, N. Explainable Artificial Intelligence Approach for the Early Prediction of Ventilator Support and Mortality in COVID-19 Patients. Computation 2022, 10, 36. [Google Scholar] [CrossRef]
- Afrash, M.R.; Kazemi-Arpanahi, H.; Shanbehzadeh, M.; Nopour, R.; Mirbagheri, E. Predicting hospital readmission risk in patients with COVID-19: A machine learning approach. Inform. Med. Unlocked 2022, 30, 100908. [Google Scholar] [CrossRef] [PubMed]
- Boussen, S.; Cordier, P.Y.; Malet, A.; Simeone, P.; Cataldi, S.; Vaisse, C.; Roche, X.; Castelli, A.; Assal, M.; Pepin, G.; et al. Triage and monitoring of COVID-19 patients in intensive care using unsupervised machine learning. Comput. Biol. Med. 2021, 142, 105192. [Google Scholar] [CrossRef]
- Noy, O.; Coster, D.; Metzger, M.; Atar, I.; Shenhar-Tsarfaty, S.; Berliner, S.; Rahav, G.; Rogowski, O.; Shamir, R. A machine learning model for predicting deterioration of COVID-19 inpatients. Sci. Rep. 2022, 12, 2630. [Google Scholar] [CrossRef]
- Mahmud, S.; Soltanikazemi, E.; Boadu, F.; Dhakal, A.; Cheng, J. Deep Learning Prediction of Severe Health Risks for Pediatric COVID-19 Patients with a Large Feature Set in 2021 BARDA Data Challenge. arXiv 2022, arXiv:2206.01696v2. [Google Scholar]
- Elhazmi, A.; Al-Omari, A.; Sallam, H.; Mufti, H.; Rabie, A.; Alshahrani, M.; Mady, A.; Alghamdi, A.; Altalaq, A.; Azzam, M.; et al. Machine learning decision tree algorithm role for predicting mortality in critically ill adult COVID-19 patients admitted to the ICU. J. Infect. Public Health 2022, 15, 826–834. [Google Scholar] [CrossRef] [PubMed]
- Alabbad, D.; Almuhaideb, A.; Alsunaidi, S.; Alqudaihi, K.; Alamoudi, F.; Alhobaishi, M.; Alaqeel, N.; Alshahrani, M. Machine learning model for predicting the length of stay in the intensive care unit for COVID-19 patients in the eastern province of Saudi Arabia. Inform. Med. Unlocked 2022, 30, 100937. [Google Scholar] [CrossRef] [PubMed]
- Igarashi, Y.; Nishimura, K.; Ogawa, K.; Miyake, N.; Mizobuchi, T.; Shigeta, K.; Obinata, H.; Takayama, Y.; Tagami, T.; Seike, M.; et al. Machine Learning Prediction for Supplemental Oxygen Requirement in Patients with COVID-19. J. Nippon. Med. Sch. 2021, 89, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Heldt, F.; Vizcaychipi, M.; Peacock, S.; Cinelli, M.; McLachlan, L.; Andreotti, F.; Jovanović, S.; Dürichen, R.; Lipunova, N.; Fletcher, R.; et al. Early risk assessment for COVID-19 patients from emergency department data using machine learning. Sci. Rep. 2021, 11, 4200. [Google Scholar] [CrossRef]
- Garcia-Gutierrez, S.; Esteban-Aizpiri, C.; Lafuente, I.; Barrio, I.; Raúl, Q.L.; Quintana, J.; Uranga, A.; Orive, M.; González, N.; Anton, A.; et al. Machine learning-based model for prediction of clinical deterioration in hospitalized patients by COVID 19. Sci. Rep. 2022, 12, 7097. [Google Scholar] [CrossRef] [PubMed]
- Greco, M.; Angelotti, G.; Caruso, P.; Zanella, A.; Stomeo, N.; Costantini, E.; Protti, A.; Pesenti, A.; Grasselli, G.; Cecconi, M. Outcome prediction during an ICU surge using a purely data-driven approach: A supervised machine learning case-study in critically ill patients from COVID-19 Lombardy outbreak. Int. J. Med. Inform. 2022, 164, 104807. [Google Scholar] [CrossRef]
- Shanbehzadeh, M.; Yazdani, A.; Shafiee, M.; Kazemi-Arpanahi, H. Predictive modeling for COVID-19 readmission risk using machine learning algorithms. Bmc Med. Inform. Decis. Mak. 2022, 22, 139. [Google Scholar] [CrossRef]
- Etu, E.E.; Monplaisir, L.; Arslanturk, S.; Masoud, S.; Aguwa, C.; Markevych, I.; Miller, J. Prediction of Length of Stay in the Emergency Department for COVID-19 Patients: A Machine Learning Approach. IEEE Access 2022, 10, 42243–42251. [Google Scholar] [CrossRef]
- Metz, J.; Thoral, P.; Chorus, C.; Elbers, P.; van den Bogaard, B. Behavioural artificial intelligence technology for COVID-19 intensivist triage decisions: Making the implicit explicit. Intensive Care Med. 2021, 47, 1327–1328. [Google Scholar] [CrossRef]
- Halasz, G.; Sperti, M.; Villani, M.; Michelucci, U.; Agostoni, P.; Biagi, A.; Rossi, L.; Botti, A.; Mari, C.; Maccarini, M.; et al. A machine learning approach for mortality prediction in COVID-19 pneumonia Development and evaluation of the Piacenza score. J. Med. Internet Res. 2021, 23, e29058. [Google Scholar] [CrossRef] [PubMed]
- Meng, L.; Dong, D.; Li, L.; Niu, M.; Bai, Y.; Wang, M.; Qiu, X.; Zha, Y.; Tian, J. A Deep Learning Prognosis Model Help Alert for COVID-19 Patients at High-Risk of Death: A Multi-center Study. IEEE J. Biomed. Health Inform. 2020, 24, 3576–3584. [Google Scholar] [CrossRef] [PubMed]
- Mahdavi, M.; Choubdar, H.; Zabeh, E.; Rieder, M.; Safavi-Naeini, S.; Jobbagy, Z.; Ghorbani, A.; Abedini, A.; Kiani, A.; Khanlarzadeh, V.; et al. A machine learning based exploration of COVID-19 mortality risk. PLoS ONE 2020, 7, 16. [Google Scholar] [CrossRef] [PubMed]
- Blagojević, A.; Šušteršič, T.; Lorencin, I.; Baressi Šegota, S.; Andelić, N.; Milovanovic, D.; Baskić, D.; Baskic, D.; Petrović, N.; Sazdanović, P.; et al. Artificial intelligence approach towards assessment of condition of COVID-19 patients—Identification of predictive biomarkers associated with severity of clinical condition and disease progression. Comput. Biol. Med. 2021, 138, 104869. [Google Scholar] [CrossRef]
- Zawbaa, H.; El-Gendy, A.; Saeed, H.; Osama, H.; Ali, A.; Gomaa, D.; Abdelrahman, M.; Harb, H.; Madney, Y.M.; Abdelrahim, M. A study of the possible factors affecting COVID-19 spread, severity and mortality and the effect of social distancing on these factors: Machine learning forecasting model. Int. J. Clin. Pract. 2021, 75, e14116. [Google Scholar] [CrossRef]
- Sotoudeh, H.; Shafaat, O.; Sotoudeh, E.; Tasorian, B.; Sarrami, A.; Didehdar, M.; Tabatabaei, M. Accuracy of Machine Learning Models to Predict Mortality in COVID-19 Infection Using the Clinical and Laboratory Data at the Time of Admission. Cureus 2021, 13, e18768. [Google Scholar] [CrossRef]
- Fidan, H.; Yuksel, M. A comparative study for determining COVID-19 risk levels by unsupervised machine learning methods. Expert Syst. Appl. 2021, 190, 116243. [Google Scholar] [CrossRef]
- Shi, B.; Ye, H.; Zheng, L.; Lyu, J.; Chen, C.; Heidari, A.A.; Hu, Z.; Chen, H.; Wu, P. Evolutionary warning system for COVID-19 severity: Colony predation algorithm enhanced extreme learning machine. Comput. Biol. Med. 2021, 136, 104698. [Google Scholar] [CrossRef]
- Krysko, O.; Kondakova, E.; Vershinina, O.; Galova, E.; Blagonravova, A.; Gorshkova, E.; Bachert, C.; Ivanchenko, M.; Krysko, D.; Vedunova, M. Artificial Intelligence Predicts Severity of COVID-19 Based on Correlation of Exaggerated Monocyte Activation, Excessive Organ Damage and Hyperinflammatory Syndrome: A Prospective Clinical Study. Front. Immunol. 2021, 12, 3298. [Google Scholar] [CrossRef]
- Yaşar, Ş.; Colak, C.; Yologlu, S. Artificial Intelligence-Based Prediction of COVID-19 Severity on the Results of Protein Profiling. Comput. Methods Programs Biomed. 2021, 202, 105996. [Google Scholar] [CrossRef]
- Domínguez-Olmedo, J.L.; Gragera-Martínez, Á.; Mata, J.; Pachón Álvarez, V. Machine Learning Applied to Clinical Laboratory Data in Spain for COVID-19 Outcome Prediction: Model Development and Validation. J. Med. Internet Res. 2021, 23, e26211. [Google Scholar] [CrossRef]
- Garrafa, E.; Vezzoli, M.; Ravanelli, M.; Farina, D.; Borghesi, A.; Calza, S.; Maroldi, R. Early prediction of in-hospital death of COVID-19 patients: A machine-learning model based on age, blood analyses and chest X-ray score. eLife 2021, 10, e70640. [Google Scholar] [CrossRef] [PubMed]
- Baqui, P.; Marra, V.; Alaa, A.; Bica, I.; Ercole, A.; Schaar, M. Comparing COVID-19 risk factors in Brazil using machine learning: The importance of socioeconomic, demographic and structural factors. Sci. Rep. 2021, 11, 15591. [Google Scholar] [CrossRef] [PubMed]
- Di Castelnuovo, A.; Bonaccio, M.; Costanzo, S.; Gialluisi, A.; Antinori, A.; Berselli, N.; Blandi, L.; Bruno, R.; Cauda, R.; Guaraldi, G.; et al. Common cardiovascular risk factors and in-hospital mortality in 3894 patients with COVID-19: Survival analysis and machine learning-based findings from the multicentre Italian CORIST Study. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1899–1913. [Google Scholar] [CrossRef] [PubMed]
- Tezza, F.; Lorenzoni, G.; Azzolina, D.; Barbar, S.; Leone, L.; Gregori, D. Predicting in-Hospital Mortality of Patients with COVID-19 Using Machine Learning Techniques. J. Pers. Med. 2021, 11, 343. [Google Scholar] [CrossRef]
- Wang, X.; Che, Q.; Ji, X.; Meng, X.; Zhang, L.; Jia, R.; Lyu, H.; Bai, W.; Tan, L.; Gao, Y. Correlation between lung infection severity and clinical laboratory indicators in patients with COVID-19: A cross-sectional study based on machine learning. BMC Infect. Dis. 2021, 21, 192. [Google Scholar] [CrossRef] [PubMed]
- Fang, C.; Bai, S.; Chen, Q.; Zhou, Y.; Xia, L.; Qin, L.; Gong, S.; Xie, X.; Zhou, C.; Tu, D.; et al. Deep learning for predicting COVID-19 malignant progression. Med. Image Anal. 2021, 72, 102096. [Google Scholar] [CrossRef] [PubMed]
- Guan, X.; Zhang, B.; Fu, M.; Li, M.; Yuan, X.; Zhu, Y.; Peng, J.; Guo, H.; Lu, Y. Clinical and inflammatory features based machine learning model for fatal risk prediction of hospitalized COVID-19 patients: Results from a retrospective cohort study. Ann. Med. 2021, 53, 257–266. [Google Scholar] [CrossRef]
- Sankaranarayanan, S.; Balan, J.; Walsh, J.; Wu, Y.; Minnich, S.; Piazza, A.; Osborne, C.; Oliver, G.; Lesko, J.; Bates, K.; et al. COVID-19 mortality prediction from deep learning in a large multistate EHR and LIS dataset: Algorithm development and validation (Preprint). J. Med. Internet Res. 2021, 23, e30157. [Google Scholar] [CrossRef]
- Schöning, V.; Liakoni, E.; Baumgartner, C.; Exadaktylos, A.; Hautz, W.; Atkinson, A.; Hammann, F. Development and validation of a prognostic COVID-19 severity assessment (COSA) score and machine learning models for patient triage at a tertiary hospital. J. Transl. Med. 2021, 19, 56. [Google Scholar] [CrossRef]
- Zhu, J.; Ge, P.; Jiang, C.; Zhang, Y.; Li, X.; Zhao, Z.; Zhang, L.; Duong, T. Deep-learning artificial intelligence analysis of clinical variables predicts mortality in COVID-19 patients. J. Am. Coll. Emerg. Physicians Open 2020, 1, 1364–1373. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Lin, Y.; Zhu, T.; Fan, M.; Xu, S.; Qiu, W.; Chen, C.; Li, L.; Wang, Y.; Yan, J.; et al. Development and external evaluation of predictions models for mortality of COVID-19 patients using machine learning method. Neural Comput. Appl. 2021, 35, 13037–13046. [Google Scholar] [CrossRef] [PubMed]
- Quiroz, J.C.; Feng, Y.Z.; Cheng, Z.Y.; Rezazadegan, D.; Chen, P.K.; Lin, Q.T.; Qian, L.; Liu, X.F.; Berkovsky, S.; Coiera, E.; et al. Development and Validation of a Machine Learning Approach for Automated Severity Assessment of COVID-19 Based on Clinical and Imaging Data: Retrospective Study. JMIR Med. Inform. 2021, 9, e24572. [Google Scholar] [CrossRef] [PubMed]
- de Fátima, A.; Stremel, D.; Fachi, M.; Surek, M.; Wiens, A.; Stumpf Tonin, F.; Pontarolo, R. Diagnosis and prediction of COVID-19 severity: Can biochemical tests and machine learning be used as prognostic indicators? Comput. Biol. Med. 2021, 134, 104531. [Google Scholar] [CrossRef]
- Booth, A.; Abels, E.; McCaffrey, P. Development of a prognostic model for mortality in COVID-19 infection using machine learning. Mod. Pathol. 2020, 34, 522–531. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Chen, Q.; Liu, T.; Luo, P.; Zhou, Y.; Liu, M.; Xiong, B.; Zhou, F. Development and Validation of Predictors for the Survival of Patients with COVID-19 Based on Machine Learning. Front. Med. 2021, 8, 683431. [Google Scholar] [CrossRef]
- Hu, C.; Liu, Z.; Jiang, Y.; Shi, O.; Zhang, X.; Xu, K.; Suo, C.; Wang, Q.; Song, Y.; Yu, K.; et al. Early prediction of mortality risk among patients with severe COVID-19, using machine learning. Int. J. Epidemiol. 2020, 49, 1918–1929. [Google Scholar] [CrossRef]
- Zhou, K.; Ss, T.; Li, L.; Zang, Z.; Wang, J.; Li, J.; Liang, J.; Zhang, F.; Zhang, Q.; Ge, W.; et al. Eleven Routine Clinical Features Predict COVID-19 Severity Uncovered by Machine Learning of Longitudinal Measurements. Comput. Struct. Biotechnol. J. 2021, 19, 3640–3649. [Google Scholar] [CrossRef]
- Shi, W.; Peng, X.; Liu, T.; Cheng, Z.; Lu, H.; Yang, S.; Zhang, J.; Wang, M.; Gao, Y.; Shi, Y.; et al. A deep learning-based quantitative computed tomography model for predicting the severity of COVID-19: A retrospective study of 196 patients. Ann. Transl. Med. 2021, 9, 216. [Google Scholar] [CrossRef] [PubMed]
- Casiraghi, E.; Malchiodi, D.; Trucco, G.; Frasca, M.; Cappelletti, L.; Fontana, T.; Esposito, A.; Avola, E.; Jachetti, A.; Reese, J.; et al. Explainable Machine Learning for Early Assessment of COVID-19 Risk Prediction in Emergency Departments. IEEE Access 2020, 8, 196299–196325. [Google Scholar] [CrossRef] [PubMed]
- Ye, J.; Hua, M.; Zhu, F. Machine Learning Algorithms are Superior to Conventional Regression Models in Predicting Risk Stratification of COVID-19 Patients. Risk Manag. Healthc. Policy 2021, 14, 3159–3166. [Google Scholar] [CrossRef]
- Aznar-Gimeno, R.; Esteban, L.; Lezaun, G.; del Hoyo-Alonso, R.; Abadia-Gallego, D.; Paño-Pardo, J.; Esquillor-Rodrigo, M.; Lanas, A.; Serrano, M.T. A Clinical Decision Web to Predict ICU Admission or Death for Patients Hospitalised with COVID-19 Using Machine Learning Algorithms. Int. J. Environ. Res. Public Health 2021, 18, 8677. [Google Scholar] [CrossRef]
- Dabbah, M.; Reed, A.; Booth, A.; Yassaee, A.; Despotovic, A.; Klasmer, B.; Binning, E.; Aral, M.; Plans, D.; Morelli, D.; et al. Machine learning approach to dynamic risk modeling of mortality in COVID-19: A UK Biobank study. Sci. Rep. 2021, 11, 16936. [Google Scholar] [CrossRef] [PubMed]
- Ko, H.; Chung, H.; Kang, W.S.; Park, C.; Kim, D.W.; Kim, S.E.; Chung, C.R.; Ko, R.E.; Lee, H.; Seo, J.H.; et al. An Artificial Intelligence Model to Predict the Mortality of COVID-19 Patients at Hospital Admission Time Using Routine Blood Samples: Development and Validation of an Ensemble Model. J. Med. Internet Res. 2020, 22, e25442. [Google Scholar] [CrossRef]
- Sánchez-Montañés, M.; Rodriguez, P.; Serrano-López, A.; Olivas, E.; Alakhdar-Mohmara, Y. Machine Learning for Mortality Analysis in Patients with COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 8386. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.; Kher, V.; Desai, B.; Lei, X.; Cen, S.; Nanda, N.; Gholamrezanezhad, A.; Duddalwar, V.; Varghese, B.; Oberai, A. Machine learning based predictors for COVID-19 disease severity. Sci. Rep. 2021, 11, 4673. [Google Scholar] [CrossRef]
- Aktar, S.; Talukder, A.; Ahamad, M.; Kamal, A.; Khan, J.; Hossain, N.; Azad, A.K.M.; Quinn, J.; Summers, M.; Liaw, S.T.; et al. Machine Learning Approaches to Identify Patient Comorbidities and Symptoms That Increased Risk of Mortality in COVID-19. Diagnostics 2021, 11, 1383. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Cai, G.; Fang, W.; Li, H.Y.; Wang, S.Y.; Chen, L.; Yu, Y.; Liu, D.; Xu, S.; Cui, P.F.; et al. Machine Learning Based Early Warning System Enables Accurate Mortality Risk Prediction for COVID-19. Nat. Commun. 2020, 11, 5033. [Google Scholar] [CrossRef]
- Yu, L.; Halalau, A.; Dalal, B.; Abbas, A.; Ivascu, F.; Amin, M.; Nair, G. Machine learning methods to predict mechanical ventilation and mortality in patients with COVID-19. PLoS ONE 2021, 16, e0249285. [Google Scholar] [CrossRef]
- Shiri, I.; Salimi, Y.; Pakbin, M.; Hajianfar, G.; Haddadi Avval, A.; Sanaat, A.; Mostafaei, S.; Akhavanallaf, A.; Saberi Manesh, A.; Mansouri, Z.; et al. COVID-19 prognostic modeling using CT radiomic features and machine learning algorithms: Analysis of a multi-institutional dataset of 14,339 patients. Comput. Biol. Med. 2022, 145, 105467. [Google Scholar] [CrossRef]
- Lipták, P.; Banovcin, P.; Rosoľanka, R.; Prokopič, M.; Kocan, I.; Žiačiková, I.; Uhrik, P.; Grendár, M.; Hyrdel, R. A machine learning approach for identification of gastrointestinal predictors for the risk of COVID-19 related hospitalization. PeerJ 2022, 10, e13124. [Google Scholar] [CrossRef]
- Yarbakhsh, R.; Mortazavi, S.; Mortazavi, S.; Parsaei, H.; Rad, D. Artificial intelligence effectively predicts the COVID-19 death rate in different UK cities. J. Intell. Fuzzy Syst. 2022, 43, 1853–1857. [Google Scholar] [CrossRef]
- Mohammad, R.; Aljabri, M.; Aboulnour, M.; Mirza, S.; Alshobaiki, A. Classifying the Mortality of People with Underlying Health Conditions Affected by COVID-19 Using Machine Learning Techniques. Appl. Comput. Intell. Soft Comput. 2022, 2022, 3783058. [Google Scholar] [CrossRef]
- Baik, S.M.; Lee, M.; Hong, K.S.; Park, D.J. Development of Machine-Learning Model to Predict COVID-19 Mortality: Application of Ensemble Model and Regarding Feature Impacts. Diagnostics 2022, 12, 1464. [Google Scholar] [CrossRef] [PubMed]
- Wan, T.K.; Huang, R.X.; Tulu, T.; Liu, J.D.; Vodencarevic, A.; Wong, C.W.; Chan, K.h. Identifying Predictors of COVID-19 Mortality Using Machine Learning. Life 2022, 12, 547. [Google Scholar] [CrossRef] [PubMed]
- Azizi, Z.; Shiba, Y.; Alipour, P.; Maleki, F.; Raparelli, V.; Norris, C.; Forghani, R.; Pilote, L.; Emam, K. Importance of sex and gender factors for COVID-19 infection and hospitalisation: A sex-stratified analysis using machine learning in UK Biobank data. BMJ Open 2022, 12, e050450. [Google Scholar] [CrossRef] [PubMed]
- Vezzoli, M.; Inciardi, R.; Oriecuia, C.; Paris, S.; Murillo, N.; Agostoni, P.; Ameri, P.; Bellasi, A.; Camporotondo, R.; Canale, C.; et al. Machine learning for prediction of in-hospital mortality in coronavirus disease 2019 patients: Results from an Italian multicenter study. J. Cardiovasc. Med. 2022, 23, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Reina Reina, A.; Barrera, J.; Valdivieso, B.; Gas Lopez, M.E.; Maté, A.; Trujillo, J. Machine learning model from a Spanish cohort for prediction of SARS-CoV-2 mortality risk and critical patients. Sci. Rep. 2022, 12, 5723. [Google Scholar] [CrossRef] [PubMed]
- Rana, A.; Singh, H.; Mavuduru, R.; Pattanaik, S.; Rana, P. Quantifying prognosis severity of COVID-19 patients from deep learning based analysis of CT chest images. Multimed. Tools Appl. 2022, 81, 18129–18153. [Google Scholar] [CrossRef]
- Chen, L.; Mei, Z.; Guo, W.; Ding, S.; Huang, T.; Cai, Y.D. Recognition of Immune Cell Markers of COVID-19 Severity with Machine Learning Methods. BioMed Res. Int. 2022, 2022, 6089242. [Google Scholar] [CrossRef]
- Mazloumi, R.; Abazari, S.R.; Nafarieh, F.; Aghsami, A.; Jolai, F. Statistical analysis of blood characteristics of COVID-19 patientsand their survival or death prediction using machine learningalgorithms. Neural Comput. Appl. 2022, 34, 14729–14743. [Google Scholar] [CrossRef]
- Agrawal, S.; Patil, N. Machine Learning based COVID-19 Mortality Prediction using Common Patient Data. In Proceedings of the 2022 IEEE 7th International Conference for Convergence in Technology (I2CT), Mumbai, India, 7–9 April 2022; pp. 1–6. [Google Scholar] [CrossRef]
- Laino, M.; Generali, E.; Tommasini, T.; Angelotti, G.; Aghemo, A.; Desai, A.; Morandini, P.; Stefanini, G.; Lleo, A.; Voza, A.; et al. An Individualized Algorithm to Predict Mortality in COVID-19 Pneumonia: A Machine Learning Based Study. Arch. Med. Sci. 2022, 18, 587. [Google Scholar] [CrossRef] [PubMed]
- Bertram, M.G.; Sundin, J.; Roche, D.G.; Sánchez-Tójar, A.; Thoré, E.S.J.; Brodin, T. Open science. Curr. Biol. 2023, 33, R792–R797. [Google Scholar] [CrossRef] [PubMed]
- Ali, O.; Ishak, M.K.; Bhatti, M.K.L. A Machine Learning Approach for Early COVID-19 Symptoms Identification. Comput. Mater. Contin. 2022, 70, 3803–3820. [Google Scholar] [CrossRef]
- Tadepalli, S.; Thulasiram, R. COVID-19 Early Symptom Prediction Using Blockchain and Machine Learning. In Blockchain and Applications: 3rd International Congress; Springer: Berlin/Heidelberg, Germany, 2022; pp. 243–251. [Google Scholar] [CrossRef]
- Silva, C.; Junior, A.; Lopes, R. Predictive Analysis of COVID-19 Symptoms in Social Networks through Machine Learning. Electronics 2022, 11, 580. [Google Scholar] [CrossRef]
- Chen, Z.; Li, M.; Wang, R.; Sun, W.; Liu, J.; Li, H.; Wang, T.; Lian, Y.; Zhang, J.; Wang, X. Diagnosis of COVID-19 via Acoustic Analysis and Artificial Intelligence by Monitoring Breath Sounds on Smartphones. J. Biomed. Inform. 2022, 130, 104078. [Google Scholar] [CrossRef]
- Lee, D.; Wang, C.; McAlister, F.; Ma, S.; Chu, A.; Rochon, P.; Kaul, P.; Austin, P.; Wang, X.; Kalmady, S.; et al. Factors associated with SARS-CoV-2 test positivity in long-term care homes: A population-based cohort analysis using machine learning. Lancet Reg. Health Am. 2022, 6, 100146. [Google Scholar] [CrossRef] [PubMed]
- Gorji, F.; Shafiekhani, S.; Namdar, P.; Abdollahzade, S.; Rafiei, S. Machine learning-based COVID-19 diagnosis by demographic characteristics and clinical data. Adv. Respir. Med. 2022, 90, 171–183. [Google Scholar] [CrossRef]
- Sharma, D.; Subramanian, M.; Malyadri, P.; Reddy, B.; Sharma, D.; Tahreem, M. Classification of COVID -19 by Using Supervised Optimized Machine Learning Technique. Mater. Today Proc. 2021, 56, 2058–2062. [Google Scholar] [CrossRef]
- Chadaga, K.; Chakraborty, C.; Prabhu, S.; Umakanth, S.; Bhat, V.; Sampathila, N. Clinical and Laboratory Approach to Diagnose COVID-19 Using Machine Learning. Interdiscip. Sci. Comput. Life Sci. 2022, 14, 452–470. [Google Scholar] [CrossRef]
- Thimoteo, L.; Vellasco, M.; Amaral, J.; Figueiredo, K.; Yokoyama, C.; Marques, E. Explainable Artificial Intelligence for COVID-19 Diagnosis Through Blood Test Variables. J. Control Autom. Electr. Syst. 2022, 33, 625–644. [Google Scholar] [CrossRef]
- Sridhar, A.; Chen, Z.H.; Mayfield, J.; Fohner, A.; Arvanitis, P.; Atkinson, S.; Braunschweig, F.; Chatterjee, N.; Zamponi, A.; Johnson, G.; et al. Identifying Risk of Adverse Outcomes in COVID-19 Patients via Artificial Intelligence-Powered Analysis of 12-Lead Intake Electrocardiogram. Cardiovasc. Digit. Health J. 2021, 3, 62–74. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, A.; Kapoor, A.; Mahajan, G.; Kapur, A. Use of Artificial Intelligence to Triage Patients with Flu-Like Symptoms Using Imaging in Non- COVID-19 Hospitals during COVID-19 Pandemic: An Ongoing 8-Month Experience. Indian J. Radiol. Imaging 2022, 31, 901–909. [Google Scholar] [CrossRef] [PubMed]
- Cabras, S. A Bayesian-Deep Learning Model for Estimating COVID-19 Evolution in Spain. Mathematics 2021, 9, 2921. [Google Scholar] [CrossRef]
- Soltan, A.; Yang, J.; Pattanshetty, R.; Novak, A.; Yang, Y.; Rohanian, O.; Beer, S.; Soltan, M.; Thickett, D.; Fairhead, R.; et al. Real-world evaluation of rapid and laboratory-free COVID-19 triage for emergency care: External validation and pilot deployment of artificial intelligence driven screening. Lancet Digit. Health 2022, 4, e266–e278. [Google Scholar] [CrossRef]
- Kim, H.J.; Han, D.; Kim, J.H.; Kim, D.; Ha, B.; Seog, W.; Lee, Y.K.; Lim, D.; Hong, S.; Park, M.J.; et al. An Easy-to-Use Machine Learning Model to Predict the Prognosis of Patients With COVID-19: Retrospective Cohort Study. J. Med. Internet Res. 2020, 22, e24225. [Google Scholar] [CrossRef]
- Mueller, Y.; Schrama, T.; Ruijten, R.; Schreurs, M.; Grashof, D.; van de Werken, H.; Jona Lasinio, G.; Alvarez-de la Sierra, D.; Kiernan, C.; Eiro, M.; et al. Stratification of hospitalized COVID-19 patients into clinical severity progression groups by immuno-phenotyping and machine learning. Nat. Commun. 2022, 13, 915. [Google Scholar] [CrossRef]
- Hou, W.; Zhao, Z.; Chen, A.; Li, H.; Duong, T. Machining learning predicts the need for escalated care and mortality in COVID-19 patients from clinical variables. Int. J. Med. Sci. 2021, 18, 1739–1745. [Google Scholar] [CrossRef]
- Campbell, T.W.; Wilson, M.P.; Roder, H.; MaWhinney, S.; Georgantas, R.W.; Maguire, L.K.; Roder, J.; Erlandson, K.M. Predicting prognosis in COVID-19 patients using machine learning and readily available clinical data. Int. J. Med. Inform. 2021, 155, 104594. [Google Scholar] [CrossRef]
- Vaid, A.; Somani, S.; Russak, A.; Freitas, J.; Chaudhry, F.; Paranjpe, I.; Johnson, K.; Lee, S.; Miotto, R.; Richter, F.; et al. Machine Learning to Predict Mortality and Critical Events in a Cohort of Patients With COVID-19 in New York City: Model Development and Validation. J. Med. Internet Res. 2020, 22, e24018. [Google Scholar] [CrossRef]
- Kar, S.; Chawla, R.; Haranath, S.; Ramasubban, S.; Ramakrishnan, N.; Vaishya, R.; Sibal, A.; Reddy, S. Multivariable mortality risk prediction using machine learning for COVID-19 patients at admission (AICOVID). Sci. Rep. 2021, 11, 12801. [Google Scholar] [CrossRef]
- Xu, W.; Sun, N.N.; Gao, H.N.; Chen, Z.Y.; Yang, Y.; Bin, J.; Tang, L.L. Risk factors analysis of COVID-19 patients with ARDS and prediction based on machine learning. Sci. Rep. 2021, 11, 2933. [Google Scholar] [CrossRef]
- Rahman, T.; Khandakar, A.; Haque, M.; Ibtehaz, N.; Kashem, S.; Islam, M.; Al-Maadeed, S.; Zughaier, S.; Doi, S.; Chowdhury, M. Development and Validation of an Early Scoring System for Prediction of Disease Severity in COVID-19 Using Complete Blood Count Parameters. IEEE Access 2021, 9, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Chung, H.; Ko, H.; Kang, W.S.; Kim, K.W.; Lee, H.; Park, C.; Song, H.O.; Choi, T.Y.; Seo, J.H.; Lee, J. Prediction and Feature Importance Analysis for Severity of COVID-19 in South Korea Using Artificial Intelligence: Model Development and Validation. J. Med. Internet Res. 2021, 23, e27060. [Google Scholar] [CrossRef] [PubMed]
- Rahman, T.; Al-Ishaq, F.; Al-Mohannadi, F.; Mubarak, R.; Al-Hitmi, M.; Islam, K.; Khandakar, A.; Ait Hssain, A.; Al-Madeed, S.; Zughaier, S.; et al. Mortality Prediction Utilizing Blood Biomarkers to Predict the Severity of COVID-19 Using Machine Learning Technique. Diagnostics 2021, 11, 1582. [Google Scholar] [CrossRef] [PubMed]
- Ikemura, K.; Goldstein, D.; Szymanski, J.; Bellin, E.; Stahl, L.; Yagi, Y.; Saada, M.; Simone, K.; Reyes, M.; Billett, H. Using Automated-Machine Learning to Predict COVID-19 Patient Mortality (Preprint). J. Med. Internet Res. 2020, 23, e23458. [Google Scholar] [CrossRef] [PubMed]
- Munera, N.; Garcia-Gallo, E.; Gonzalez, Á.; Zea, J.; Fuentes, Y.; Serrano, C.; Ruiz-Cuartas, A.; Rodríguez, A.; Reyes, L. A novel model to predict severe COVID-19 and mortality using an artificial intelligence algorithm to interpret chest X-Rays and clinical variables. ERJ Open Res. 2022, 8, 00010–2022. [Google Scholar] [CrossRef] [PubMed]
- Cihan, P. The machine learning approach for predicting the number of intensive care, intubated patients and death: The COVID-19 pandemic in Turkey. Sigma J. Eng. Nat. Sci. 2022, 40, 85–94. [Google Scholar] [CrossRef]
- Izquierdo, J.L.; Ancochea, J.; Soriano, J.B. Clinical Characteristics and Prognostic Factors for Intensive Care Unit Admission of Patients With COVID-19: Retrospective Study Using Machine Learning and Natural Language Processing. J. Med. Internet Res. 2020, 22, e21801. [Google Scholar] [CrossRef] [PubMed]
- Nino, G.; Linguraru, M.G. Developing artificial intelligence technology for pediatric pulmonology: Lessons from COVID-19. Pediatr. Pulmonol. 2022, 57, 1588. [Google Scholar] [CrossRef]
- Subudhi, S.; Verma, A.; Patel, A.; Hardin, C.; Khandekar, M.; Lee, H.; Mcevoy, D.; Stylianopoulos, T.; Munn, L.; Dutta, S.; et al. Comparing machine learning algorithms for predicting ICU admission and mortality in COVID-19. npj Digit. Med. 2021, 4, 87. [Google Scholar] [CrossRef]
- Shamout, F.; Shen, Y.; Wu, N.; Kaku, A.; Park, J.; Makino, T.; Jastrzębski, S.; Witowski, J.; Wang, D.; Zhang, B.; et al. An artificial intelligence system for predicting the deterioration of COVID-19 patients in the emergency department. npj Digit. Med. 2021, 4, 80. [Google Scholar] [CrossRef]
- Arévalo, J.; Gómez, J.; Casas, J.; Antón-Santos, J.; Melero-Bermejo, J.; López-Carmona, M.; Palacios, L.; Sanz-Cánovas, J.; Pesqueira-Fontán, P.; Peña-Fernández, A.; et al. The importance of association of comorbidities on COVID-19 outcomes: A machine learning approach. Curr. Med. Res. Opin. 2022, 38, 501–510. [Google Scholar] [CrossRef]
- Kalabarige, L.R.; Maringanti, H. Symptom Based COVID-19 Test Recommendation System Using Machine Learning Technique. Intell. Decis. Technol. 2022, 16, 181–191. [Google Scholar] [CrossRef]
- Li, X.; Ge, P.; Zhu, J.; Li, H.; Graham, J.; Singer, A.; Richman, P.; Duong, T. Deep learning prediction of likelihood of ICU admission and mortality in COVID-19 patients using clinical variables. PeerJ 2020, 8, e10337. [Google Scholar] [CrossRef]
- Arvind, V.; Kim, J.; Cho, B.; Geng, E.; Cho, S. Development of a machine learning algorithm to predict intubation among hospitalized patients with COVID-19. J. Crit. Care 2021, 62, 25–30. [Google Scholar] [CrossRef]
- Famiglini, L.; Campagner, A.; Carobene, A.; Cabitza, F. A robust and parsimonious machine learning method to predict ICU admission of COVID-19 patients. Med. Biol. Eng. Comput. 2022. [CrossRef] [PubMed]
- Bolourani, S.; Brenner, M.; Wang, P.; McGinn, T.; Hirsch, J.S.; Barnaby, D.; Zanos, T.P. A Machine Learning Prediction Model of Respiratory Failure Within 48 Hours of Patient Admission for COVID-19: Model Development and Validation. J. Med. Internet Res. 2021, 23, e24246. [Google Scholar] [CrossRef]
- Izadi, Z.; Gianfrancesco, M.; Hyrich, K.; Strangfeld, A.; Gossec, L.; Carmona, L.; Mateus, E.; Lawson-Tovey, S.; Trupin, L.; Rush, S.; et al. Machine learning algorithms to predict COVID-19 acute respiratory distress syndrome in patients with rheumatic diseases: Results from the global rheumatology alliance provider registry. Ann. Rheum. Dis. 2021, 80, 175–176. [Google Scholar] [CrossRef]
- Bouhamed, H.; Hamdi, M.; Gargouri, R. COVID-19 Patients’ Hospital Occupancy Prediction During the Recent Omicron Wave via some Recurrent Deep Learning Architectures. Int. J. Comput. Commun. Control 2022, 17, 4697. [Google Scholar] [CrossRef]
- Laino, M.; Ammirabile, A.; Lofino, L.; Lundon, D.; Chiti, A.; Francone, M.; Savevski, V. Prognostic findings for ICU admission in patients with COVID-19 pneumonia: Baseline and follow-up chest CT and the added value of artificial intelligence. Emerg. Radiol. 2022, 29, 243–262. [Google Scholar] [CrossRef] [PubMed]
- Lopes, F.P.P.; Kitamura, F.; Prado, G.; Kuriki, P.; Garcia, M. Machine learning model for predicting severity prognosis in patients infected with COVID-19: Study protocol from COVID-AI Brasil. PLoS ONE 2021, 16, e0245384. [Google Scholar] [CrossRef]
- van de Leur, R.; Bleijendaal, H.; Taha, K.; Mast, T.; Gho, J.; Linschoten, M.; Rees, B.; Henkens, M.; Heymans, S.; Sturkenboom, N.; et al. Electrocardiogram-based mortality prediction in patients with COVID-19 using machine learning. Neth. Heart J. 2022, 30, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Maria, A.; Dimitrios, V.; Ioanna, M.; Charalampos, M.; Gerasimos, M.; Constantinos, K. Clinical Decision Making and Outcome Prediction for COVID-19 Patients Using Machine Learning. In Pervasive Computing Technologies for Healthcare, Proceedings of the 15th EAI International Conference, Pervasive Health 2021, Virtual Event, 6–8 December 2021; Lewy, H., Barkan, R., Eds.; Springer: Cham, Switzerland, 2022; pp. 3–14. [Google Scholar]
- Huang, F.; Chen, L.; Guo, W.; Zhou, X.; Feng, K.; Huang, T.; Cai, Y. Identifying COVID-19 Severity-Related SARS-CoV-2 Mutation Using a Machine Learning Method. Life 2022, 12, 806. [Google Scholar] [CrossRef] [PubMed]
- Boddu, R.S.K.; Karmakar, P.; Bhaumik, A.; Nassa, V.K.; Vandana; Bhattacharya, S. Analyzing the impact of Machine learning and Artificial intelligence and its Effect on Management of lung cancer detection in COVID-19 pandemic. Mater. Today Proc. 2021, 56, 2213–2216. [Google Scholar] [CrossRef] [PubMed]
- Patel, N.; D’Silva, K.; Li, M.; Hsu, T.; DiIorio, M.; Fu, X.; Cook, C.; Prisco, L.; Martin, L.; Vanni, K.; et al. Assessing the Severity of COVID-19 Lung Injury in Rheumatic Diseases versus the General Population Using Deep Learning-Derived Chest Radiograph Scores. Arthritis Care Res. 2022, 75, 657–666. [Google Scholar] [CrossRef]
- Gadipudi, P.; Teja, P.; Yelamancheli, C.; Thaniserikaran, A.; Mohiuddin, R.; Joy, A. Detection of pneumonia progression in lungs of individuals affected with COVID-19 severely using deep learning techniques. In Proceedings of the 2022 3rd International Conference for Emerging Technology (INCET), Belgaum, India, 27–29 May 2022; pp. 1–5. [Google Scholar] [CrossRef]
- Zhang, X.; Lu, S.; Wang, S.; Yu, X.; Wang, S.J.; Yao, L.; Pan, Y.; Zhang, Y.D. Diagnosis of COVID-19 pneumonia via a novel deep learning architecture. J. Comput. Sci. Technol. 2022, 37, 0679. [Google Scholar] [CrossRef]
- Aftab, M.; Amin, R.; Koundal, D.; Aldabbas, H.; Alouffi, B.; Iqbal, Z. Classification of COVID-19 and Influenza Patients Using Deep Learning. Contrast Media Mol. Imaging 2022, 2022, 8549707. [Google Scholar] [CrossRef]
- Jingxin, L.; Mengchao, Z.; Yuchen, L.; Jinglei, C.; Yutong, Z.; Zhong, Z.; Lihui, Z. COVID-19 lesion detection and segmentation—A deep learning method. Methods 2021, 202, 62–69. [Google Scholar] [CrossRef]
- Shahin, O.; M. Abd El Aziz, R.; Taloba, A. Detection and classification of COVID-19 in CT-lungs screening using machine learning techniques. J. Interdiscip. Math. 2022, 25, 791–813. [Google Scholar] [CrossRef]
- Aswathy, A.; Anand, H.; Chandra, V. COVID-19 severity detection using machine learning techniques from CT-images. Evol. Intell. 2022, 16, 1423–1431. [Google Scholar] [CrossRef]
- Shahin, O.; Alshammari, H.; Taloba, A.; M. Abd El Aziz, R. Machine Learning Approach for Autonomous Detection and Classification of COVID-19 Virus. Comput. Electr. Eng. 2022, 101, 108055. [Google Scholar] [CrossRef]
- Chieregato, M.; Frangiamore, F.; Morassi, M.; Baresi, C.; Nici, S.; Bassetti, C.; Bnà, C.; Galelli, M. A hybrid machine learning/deep learning COVID-19 severity predictive model from CT images and clinical data. Sci. Rep. 2022, 12, 4329. [Google Scholar] [CrossRef]
- Venkataramana, L.; Prasad, D.; Shunmuganathan, S.; Mithumary, C.; Karthikeyan, R.; Monika, N. Classification of COVID-19 from tuberculosis and pneumonia using deep learning techniques. Med. Biol. Eng. Comput. 2022, 60, 2681–2691. [Google Scholar] [CrossRef] [PubMed]
- Aswathy, A.L.; Hareendran, A.; Vinod Chandra, S.S. COVID-19 diagnosis and severity detection from CT-images using transfer learning and back propagation neural network. J. Infect. Public Health 2021, 14, 1435–1445. [Google Scholar] [CrossRef]
- Purkayastha, S.; Xiao, Y.; Jiao, Z.; Thepumnoeysuk, R.; Halsey, K.; Wu, J.; Tran, L.; Hsieh, B.; Choi, J.W.; Wang, D.; et al. Machine Learning-Based Prediction of COVID-19 Severity and Progression to Critical Illness Using CT Imaging and Clinical Data. Korean J. Radiol. 2021, 22, 1213. [Google Scholar] [CrossRef]
- Gazzah, S.; Bayi, R.; Kaloun, S.; Bencharef, O. A Deep Learning to Distinguish COVID-19 from Others Pneumonia Cases. Intell. Autom. Soft Comput. 2021, 31, 677–693. [Google Scholar] [CrossRef]
- Elkamouny, M.; Ghantous, M. Pneumonia Classification for COVID-19 Based on Machine Learning. In Proceedings of the 2022 2nd International Mobile, Intelligent and Ubiquitous Computing Conference (MIUCC), Cairo, Egypt, 8–9 May 2022; pp. 135–140. [Google Scholar] [CrossRef]
- Liu, Q.; Pang, B.; Li, H.; Zhang, B.; Liu, Y.; Lai, L.; Le, W.; Li, J.; Xia, T.; Zhang, X.; et al. Machine learning models for predicting critical illness risk in hospitalized patients with COVID-19 pneumonia. J. Thorac. Dis. 2021, 13, 1215. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Ye, Q.; Ding, W.; Jiang, Y.; Wang, M.; Niu, Z.; Zhou, X.; Gao, Y.; Wang, C.; Menpes-Smith, W.; et al. Can Clinical Symptoms and Laboratory Results Predict CT Abnormality? Initial Findings Using Novel Machine Learning Techniques in Children With COVID-19 Infections. Front. Med. 2021, 8, 699984. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Cui, Z.; Pan, F.; Li, L.; Li, L.; Liang, B.; Yang, L.; Zheng, C. Glycemic status affects the severity of coronavirus disease 2019 in patients with diabetes mellitus: An observational study of CT radiological manifestations using an artificial intelligence algorithm. Acta Diabetol. 2021, 58, 575–586. [Google Scholar] [CrossRef] [PubMed]
- Vepa, A.; Saleem, A.; Rakhshan, K.; Daneshkhah, A.; Sedighi, T.; Shohaimi, S.; Omar, A.; Salari, N.; Chatrabgoun, O.; Dharmaraj, D.; et al. Using Machine Learning Algorithms to Develop a Clinical Decision-Making Tool for COVID-19 Inpatients. Int. J. Environ. Res. Public Health 2021, 18, 6228. [Google Scholar] [CrossRef]
- Guzmán-Torres, J.A.; Alonso-Guzmán, E.M.; Domínguez-Mota, F.J.; Tinoco-Guerrero, G. Estimation of the main conditions in (SARS-CoV-2) COVID-19 patients that increase the risk of death using Machine learning, the case of Mexico. Results Phys. 2021, 27, 104483. [Google Scholar] [CrossRef]
- Iacolare, B.; Perrone, V.; Sangiorgi, D.; Ghigi, A.; Giacomini, E.; Nappi, C.; Paoli, D.; Ancona, D.; Andretta, M.; Barbieri, A.; et al. POSA310 Artificial Intelligence Applied on Administrative Big Data to Predict the Severity of SARS-CoV-2 Infection. Value Health 2022, 25, S199–S200. [Google Scholar] [CrossRef]
- Ho, D. Addressing COVID-19 Drug Development with Artificial Intelligence. Adv. Intell. Syst. 2020, 2, 2000070. [Google Scholar] [CrossRef]
- Arora, G.; Joshi, J.; Mandal, R.; Shrivastava, N.; Virmani, R.; Sethi, T. Artificial Intelligence in Surveillance, Diagnosis, Drug Discovery and Vaccine Development against COVID-19. Pathogens 2021, 10, 1048. [Google Scholar] [CrossRef] [PubMed]
- Schultz, M.; Vera, D.; Sinclair, D. Can artificial intelligence identify effective COVID-19 therapies? Embo Mol. Med. 2020, 12, e12817. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ye, T.; Xi, H.; Juhas, M.; Li, J. Deep Learning Driven Drug Discovery: Tackling Severe Acute Respiratory Syndrome Coronavirus 2. Front. Microbiol. 2021, 12, 739684. [Google Scholar] [CrossRef] [PubMed]
- Werner, J.; Kronberg, R.; Stachura, P.; Ostermann, P.; Müller, L.; Schaal, H.; Bhatia, S.; Kather, J.; Borkhardt, A.; Pandyra, A.; et al. Deep Transfer Learning Approach for Automatic Recognition of Drug Toxicity and Inhibition of SARS-CoV-2. Viruses 2021, 13, 610. [Google Scholar] [CrossRef]
- Majumdar, S.; Nandi, S.; Ghosal, S.; Ghosh, B.; Mallik, W.; Dutta Roy, N.; Biswas, A.; Mukherjee, S.; Pal, S.; Bhattacharyya, N. Deep Learning-Based Potential Ligand Prediction Framework for COVID-19 with Drug–Target Interaction Model. Cogn. Comput. 2021. [Google Scholar] [CrossRef]
- Mikkili, I.; Peele, A.; Vekateswarulu, T.; Vidya Prabhakar, K.; Macamdas, D.; Sreerama, K. Potential of artificial intelligence to accelerate diagnosis and drug discovery for COVID-19. PeerJ 2021, 9, e12073. [Google Scholar] [CrossRef]
- Gawriljuk, V.; Zin, P.P.; Puhl, A.; Zorn, K.; Foil, D.; Lane, T.; Hurst, B.; Almeida Tavella, T.; Costa, F.; Lakshmanane, P.; et al. Machine Learning Models Identify Inhibitors of SARS-CoV-2. J. Chem. Inf. Model. 2021, 61, 4224–4235. [Google Scholar] [CrossRef]
- Suvarna, K.; Biswas, D.; Pai, M.G.; Acharjee, A.; Bankar, R.; Palanivel, V.; Salkar, A.; Verma, A.; Mukherjee, A.; Choudhury, M.; et al. Proteomics and Machine Learning Approaches Reveal a Set of Prognositc Markers for COVID-19 Severity With Drug Repurposing Potential. Front. Physiol. 2021, 12, 652799. [Google Scholar] [CrossRef]
- Han, L.; Shan, G.; Chu, B.; Wang, H.; Wang, Z.; Gao, S.; Zhou, W. Accelerating drug repurposing for COVID-19 treatment by modeling mechanisms of action using cell image features and machine learning. Cogn. Neurodyn. 2021, 17, 803–811. [Google Scholar] [CrossRef]
- Aghdam, R.; Habibi, M.; Taheri, G. Using informative features in machine learning based method for COVID-19 drug repurposing. J. Cheminform. 2021, 13, 70. [Google Scholar] [CrossRef] [PubMed]
- Jha, N.; Prashar, D.; Rashid, M.; Shafiq, M.; Khan, R.; Pruncu, C.; Siddiqui, S.; Saravana Kumar, M. Deep Learning Approach for Discovery of in Silico Drugs for Combating COVID-19. J. Healthc. Eng. 2021, 2021, 6668985. [Google Scholar] [CrossRef] [PubMed]
- Pham, T.H.; Qiu, Y.; Zeng, J.; Xie, L.; Zhang, P. A deep learning framework for high-throughput mechanism-driven phenotype compound screening and its application to COVID-19 drug repurposing. Nat. Mach. Intell. 2021, 3, 247–257. [Google Scholar] [CrossRef] [PubMed]
- Auwul, M.; Rahman, M.R.; Gov, E.; Shahjaman, M.; Moni, M.A. Bioinformatics and machine learning approach identifies potential drug targets and pathways in COVID-19. Briefings Bioinform. 2021, 22, bbab120. [Google Scholar] [CrossRef] [PubMed]
- Bhati, A.; Wan, S.; Alfè, D.; Clyde, A.; Bode, M.; Tan, L.; Titov, M.; Merzky, A.; Turilli, M.; Jha, S.; et al. Pandemic Drugs at Pandemic Speed: Infrastructure for Accelerating COVID-19 Drug Discovery with Hybrid Machine Learning- and Physics-based Simulations on High Performance Computers. Interface Focus 2021, 11, 20210018. [Google Scholar] [CrossRef]
- Abdel-Basset, M.; Hawash, H.; Elhoseny, M.; Chakrabortty, R.; Ryan, M. DeepH-DTA: Deep Learning for Predicting Drug-Target Interactions: A Case Study of COVID-19 Drug Repurposing. IEEE Access 2020, 8, 170433–170451. [Google Scholar] [CrossRef]
- Nguyen, T.; Pham, D.H.; Hiep, D.; Phuong-Thao, T.; Quang, D.; Ngo, S.T. Searching and designing potential inhibitors for SARS-CoV-2 Mpro from natural sources using atomistic and deep-learning calculations. RSC Adv. 2021, 11, 38495–38504. [Google Scholar] [CrossRef]
- Zhou, Y.; Wang, F.; Tang, J.; Nussinov, R.; Cheng, F. Artificial intelligence in COVID-19 drug repurposing. Lancet. Digit. Health 2020, 2, e667–e676. [Google Scholar] [CrossRef]
- Kolitz, S.; Kim, J.; Zhang, J.; Cha, Y.; Battula, S.; Kusko, R.; Krishnan, R.; Zeskind, B.; Kaufman, H. 477 Deep learning to drive COVID-19 rapid drug repurposing. J. Immunother. Cancer 2020, 8, A509. [Google Scholar] [CrossRef]
- Loucera, C.; Esteban-Medina, M.; Rian, K.; Marín Falco, M.; Dopazo, J.; Peña-Chilet, M. Drug repurposing for COVID-19 using machine learning and mechanistic models of signal transduction circuits related to SARS-CoV-2 infection. Signal Transduct. Target. Ther. 2020, 5, 290. [Google Scholar] [CrossRef] [PubMed]
- Mohapatra, S.; Nath, P.; Chatterjee, M.; Das, N.; Kalita, D.; Roy, P.; Satapathi, S. Repurposing therapeutics for COVID-19: Rapid prediction of commercially available drugs through machine learning and docking. PLoS ONE 2020, 15, e0241543. [Google Scholar] [CrossRef] [PubMed]
- El-Behery, H.; Attia, A.F.; El-Fishawy, N.; Torkey, H. Efficient machine learning model for predicting drug-target interactions with case study for COVID-19. Comput. Biol. Chem. 2021, 93, 107536. [Google Scholar] [CrossRef] [PubMed]
- Rajput, A.; Thakur, A.; Mukhopadhyay, A.; Kamboj, S.; Rastogi, A.; Gautam, S.; Jassal, H.; Kumar, M. Prediction of repurposed drugs for Coronaviruses using artificial intelligence and machine learning. Comput. Struct. Biotechnol. J. 2021, 19, 3133–3148. [Google Scholar] [CrossRef] [PubMed]
- Jin, W.; Stokes, J.; Eastman, R.; Itkin, Z.; Zakharov, A.; Collins, J.; Jaakkola, T.; Barzilay, R. Deep learning identifies synergistic drug combinations for treating COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2105070118. [Google Scholar] [CrossRef] [PubMed]
- Burdick, H.; Lam, C.; Mataraso, S.; Siefkas, A.; Braden, G.; Dellinger, R.; McCoy, A.; Vincent, J.L.; Green-Saxena, A.; Barnes, G.; et al. Is Machine Learning a Better Way to Identify COVID-19 Patients Who Might Benefit from Hydroxychloroquine Treatment?—The IDENTIFY Trial. J. Clin. Med. 2020, 9, 3834. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.; Song, X.; Ma, T.; Pan, Q.; Zhou, Y.; Hou, Y.; Zhang, Z.; Li, K.; Karypis, G.; Cheng, F. Repurpose Open Data to Discover Therapeutics for COVID-19 using Deep Learning. J. Proteome Res. 2020, 19, 4624–4636. [Google Scholar] [CrossRef]
- Su, X.; Hu, L.; You, Z.; Hu, P.; Wang, L.; Zhao, B. A deep learning method for repurposing antiviral drugs against new viruses via multi-view nonnegative matrix factorization and its application to SARS-CoV-2. Briefings Bioinform. 2021, 23, bbab526. [Google Scholar] [CrossRef]
- Santos, S.; Torres, M.; Sánchez, M.; Cernuzzi, L.; Paccanaro, A. Machine Learning and Network Medicine approaches for Drug Repositioning for COVID-19. Patterns 2021, 3, 100396. [Google Scholar] [CrossRef]
- Beck, B.R.; Shin, B.; Choi, Y.; Park, S.; Kang, K. Predicting commercially available antiviral drugs that may act on the novel coronavirus (SARS-CoV-2) through a drug-target interaction deep learning model. Comput. Struct. Biotechnol. J. 2020, 18, 784–790. [Google Scholar] [CrossRef] [PubMed]
- Bung, N.; Krishnan, S.; Bulusu, G.; Roy, A. De novo design of new chemical entities for SARS-CoV-2 using artificial intelligence. Future Med. Chem. 2021, 13, 575–585. [Google Scholar] [CrossRef] [PubMed]
- Ke, Y.Y.; Peng, T.T.; Yeh, T.K.; Huang, W.Z.; Chang, S.E.; Wu, S.H.; Hung, H.C.; Hsu, T.A.; Lee, S.J.; Song, J.S.; et al. Artificial intelligence approach fighting COVID-19 with repurposing drugs. Biomed. J. 2020, 43, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Li, Q.; Sun, J.; Tan, S.; Tang, Y.H.; Zhao, M.; Li, Y.Y.; Cao, X.; Zhao, J.C.; Yang, J.K. Potential Drug Discovery for COVID-19 Treatment Targeting Cathepsin L Using a Deep Learning-Based Strategy. Comput. Struct. Biotechnol. J. 2022, 20, 2442–2454. [Google Scholar] [CrossRef] [PubMed]
- Mekni, N.; Coronnello, C.; Langer, T.; De Rosa, M.; Perricone, U. Support Vector Machine as a Supervised Learning for the Prioritization of Novel Potential SARS-CoV-2 Main Protease Inhibitors. Int. J. Mol. Sci. 2021, 22, 7714. [Google Scholar] [CrossRef] [PubMed]
- Kowalewski, J.; Ray, A. Predicting novel drugs for SARS-CoV-2 using machine learning from a >10 million chemical space. Heliyon 2020, 6, e04639. [Google Scholar] [CrossRef]
- Pinto, G.P.; Vavra, O.; Marques, S.M.; Filipovic, J.; Bednar, D.; Damborsky, J. Screening of world approved drugs against highly dynamical spike glycoprotein of SARS-CoV-2 using CaverDock and machine learning. Comput. Struct. Biotechnol. J. 2021, 19, 3187–3197. [Google Scholar] [CrossRef] [PubMed]
- Zame, W.; Bica, I.; Shen, C.; Curth, A.; Lee, H.S.; Bailey, S.; Weatherall, J.; Wright, D.; Bretz, F.; Schaar, M. Machine Learning for Clinical Trials in the Era of COVID-19. Stat. Biopharm. Res. 2020, 12, 506–517. [Google Scholar] [CrossRef]
- da Motta, O.J.; Silva, E.; Siqueira-Batista, R. Bioethical aspects of artificial intelligence: COVID-19 & end of life. Rev. Assoc. Méd. Bras. 2020, 66, 5–6. [Google Scholar] [CrossRef]
- Jung, C.; Excoffier, J.B.; Raphaël-Rousseau, M.; Salaün-Penquer, N.; Ortala, M.; Chouaid, C. Evolution of hospitalized patient characteristics through the first three COVID-19 waves in Paris area using machine learning analysis. PLoS ONE 2022, 17, e0263266. [Google Scholar] [CrossRef] [PubMed]
- Asif, S.; Saba, T.; Alghanim, A. Exploring Prediction of COVID-19 and its Severity using Machine Learning. In Proceedings of the 2022 Fifth International Conference of Women in Data Science at Prince Sultan University (WiDS PSU), Riyadh, Saudi Arabia, 28–29 March 2022; pp. 117–122. [Google Scholar] [CrossRef]
- Cortes, U.; Cortes, A.; Garcia-Gasulla, D.; Perez-Arnal, R.; Avarez-Napagao, S.; Alvarez, E. The ethical use of high-performance computing and artificial intelligence: Fighting COVID-19 at Barcelona Supercomputing Center. AI Ethics 2022, 2, 325–340. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).