Abstract
Recently, the Internet of Things (IoT) has attracted wide attention from many fields, especially healthcare, because of its large capacities for information perception and collection. In this paper, we present an IoT-based home telehealth system for providing smart healthcare management for individuals, especially older people. Each client node of the system is mainly composed of an electronic water meter that records the user’s daily water usage, in order to analyze their living patterns and lifestyle as well as ascertain their well-being, and an unobtrusive sleep sensor that monitors the user’s physiological parameters during sleep, such as heart rate (HR), respiratory rate (RR), body movement (BM), and their states on the bed or outside the bed. The collected data can be transmitted to a remote centralized cloud service by a wireless home gateway for analyzing the living pattern and rhythm of users. Furthermore, the periodic feedback of results can be provided to users themselves, as well as their family and health advisers. In the present study, data was collected from a total of 18 older subjects for one year to evaluate the effectiveness of the proposed system. By analyzing living patterns and rhythm, preliminary results indicate the effectiveness of the telehealth system and suggest the potential of the system regarding improvement in the quality of life (QoL) of older people and promotion of their health.
1. Introduction
The world is experiencing rapid rates of aging population, which is manifested by an increasing median age in the population of a country or a region due to declining fertility rates and/or rising life expectancies. The rapidly aging global population has led to a significant increase in the prevalence of chronic diseases, such as asthma, chronic obstructive pulmonary disease (COPD), diabetes, heart failure, and hypertension, resulting in the rapidly increasing need for medical and welfare service resources. However, very low fertility rates in many countries and regions have resulted in serious shortages of doctors, nurses, and home caregivers. The situation has forced the medical community to resort to currently available advanced technologies to solve the shortage of medical and welfare service resources.
Telehealth (also called telemedicine) is one of the most recent forms of medical and healthcare services. Its purpose is to provide clinical health care from a distance by using information and communication/telecommunication technology (ICT). Telehealth refers to a broader spectrum of remote healthcare services. Therefore, telehealth is considered one of the ways to solve the problems mentioned above. As a result of technological progress with the goal of meeting the needs of older people, various health care/monitoring systems have been developed and applied over the past two decades. The solutions include telephone-based [1,2], video [3,4], web-based [5,6,7,8], and telemetry/remote monitoring [9,10,11,12,13]. These solutions and technologies have the potential to change the way healthcare is currently delivered [9,13,14,15,16], and many are in use in clinical settings, improving the diagnosis and treatment of diseases and establishing new healthcare management methods for individuals and healthcare providers and administrators. Especially during the COVID-19 pandemic, the use of telehealth has seen significant growth and has played a significant role in addressing the severe shortage of medical resources in many countries [17].
In the last few years, the “concept” of the Internet of Things (IoT) has attracted attention from various fields, including healthcare. Numerous researchers have explored the potential of IoT in the healthcare field, addressing diverse practical challenges [18,19,20,21,22,23,24]. For instance, Dziak et al. designed an approach to construct an IoT-based information system for healthcare applications [25]. Park et al. proposed an IoT system for remote patient monitoring at home [26]. Guan et al. developed a remote health monitoring system for collecting older individuals’ electrocardiogram (ECG) and motion signals via smart home gateway equipment [27]. Similarly, Abdelgawad et al. implemented an IoT-based health monitoring system to support active and assisted living with the goal of improving older people’s lifestyle [28]. Additionally, Kumar et al. designed and developed a wristwatch-based wireless sensor platform for IoT wearable health monitoring [29]. Stefanova-Pavlova et al. proposed a refined generalized net model capable of tracking the changes in the health status (diabetes) of adult patients [30]. Kalogeropoulos et al. introduced teleophthalmology’s role in diabetic retinopathy screening-a form of telehealth-offering a means to meet the rising demand for eye care among diabetes patients [31]. Alongside the mentioned literature review, we scrutinized various representative articles related to at-home health monitoring systems, comparing their characteristics and limitations. This step was essential as the proposed method in this article is tailored for a household context. The detailed outcomes of this review are summarized in Table 1. Furthermore, beyond the fundamental functions of telehealth monitoring, its utility and practical applications could be enhanced with additional value and features. Considering the emerging concern over solitary deaths or deaths in isolation, respectively referred to as “kodokushi” or “koritsushi” in Japanese, have recently been recognized as a social issue of concern in Japan [32,33], more efforts are needed to reduce the number of solitary deaths, especially for older people who are living alone and have a lack of social contact and connections. IoT technology can play an important role in preventing or reducing the number of solitary deaths due to its attributes, such as continuous, cost-effective, and long-term monitoring. It’s noteworthy that there have been few instances where IoT has been applied to address the social issue of solitary deaths.

Table 1.
A brief review of several at-home telehealth/telecare systems.
In the present article, the authors propose a novel IoT-based telehealth monitoring system not only to monitor the healthcare of users but also to potentially reduce the number of solitary deaths. Recognizing that solitary deaths typically occur at home, we developed a telehealth monitoring system centered around an electronic water meter for tracking daily water usage and an unobtrusive sleep monitoring device for capturing users’ vital signs during the night, including heart rate (HR), respiratory rate (RR), and body movement (BM). This approach enables continuous 24-h monitoring of users’ lifestyles. To validate the effectiveness of the proposed system, we employed 18 households from the Oyamada area in the city of Koriyama, Fukushima, to participate in the empirical trial of the system. Through analysis of the gathered data and providing direct feedback to the participating households, we gained valuable insights into their health conditions. Whenever assistance was needed for improving their well-being, designated care administrators or physicians extended their support by offering advice, suggestions, and care plans, ultimately enhancing their overall quality of life (QoL).
2. Materials and Methods
2.1. System Design
A centralized cloud service is the core of the system, and it is responsible for (i) collecting and storing the vital sign data from client devices and (ii) analyzing and visualizing the data to provide feedback to users. The system diagram of the proposed system is illustrated in Figure 1. Data collection and storage within this system were established on a CentOS server and were implemented using Node-RED, which is an open-source, low-code programming tool for IoT. Node-RED is a visual programming tool built on top of the Node.js server-side framework, which has recently gained popularity in the development of IoT applications due to its flexibility in rapidly prototyping software systems. Node-RED also serves as an event-processing engine that includes built-in function nodes for message transmission based on the Message Queuing Telemetry Transport (MQTT) protocol and PostgreSQL connections. It also allows writing ad hoc JavaScript functions to process incoming and outgoing data, thus greatly simplifying and expediting the development process.
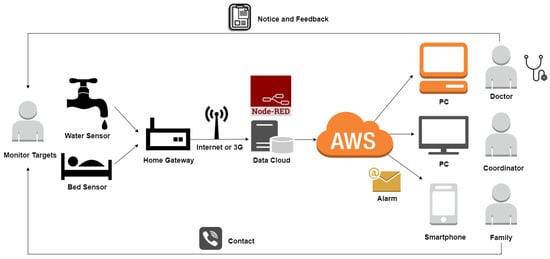
Figure 1.
Systemic diagram of the proposed unobtrusive health monitoring system for home healthcare.
As shown in Figure 1, the developed cloud service acts as an MQTT broker for distributed sensors and devices. Upon receiving an MQTT measurements message from a client, the central service collects data for vital signs during sleep and water usage, which is then stored in the PostgreSQL database. By utilizing the timer trigger function of the database, various data analyses can be executed in a timely manner to generate further derived data. These lightweight data are then uploaded in real-time to Amazon Web Services (AWS) to provide prompt feedback to users, their families or caregivers, and/or their doctors. For instance, as part of the systemic functions, when an abnormal condition is detected and identified, the server will automatically trigger a response to notify the predefined contact of the user, enabling them to take timely or emergency action. Figure 2 illustrates the module flow built using Node-RED for collecting and storing bed sensor and electronic water meter data in the local PostgreSQL database and remote AWS in real time.
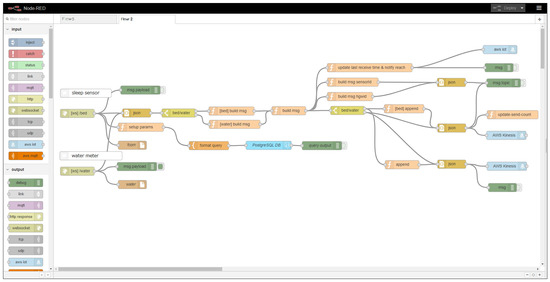
Figure 2.
The module flow built using Node-RED for data collection from the bed sensor and electronic water meter in real time.
2.2. Distributed Sensors
As a typical IoT-based system, the distributed sensors constitute the edge nodes of the proposed telehealth monitoring system. As depicted in Figure 3 and Figure 4, each edge node primarily consists of a sleep monitoring sensor and an electronic water meter. The sleep monitoring sensor (Anshin Hitsuji, NJI Corp., Koriyama, Japan) is primarily composed of 12 piezoelectric sensors and a control circuit with LAN communication functionality. The piezoelectric sensors are arranged in a matrix and enclosed within a soft and durable plastic container with dimensions of 800 mm × 100 mm × 5 mm. Placing the sleep monitoring sensor under the body or mattress during sleep allows for the measurement of HR, RR, and BM. Additionally, the sensor can determine whether a person is lying on the bed by sensing changes in pressure via the piezoelectric sensors. The sensor’s accuracy for HR and RR measurements reaches 96.9 ± 0.1% and 90.5 ± 0.7%, respectively [40]. Consequently, the sleep monitoring sensor transmits the measured HR, RR, BM, the status whether the user is lying on the bed, and measurement time, to our remote cloud service.
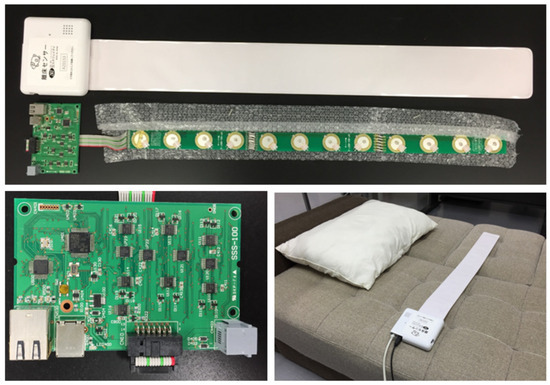
Figure 3.
The sleep monitoring sensor used in the study is mainly composed of 12 piezoelectric sensors as the upper image and a control circuit with LAN communication functionality as the bottom left image. The scenario of sleep monitoring sensor being placed on a bed is shown in the bottom right image.
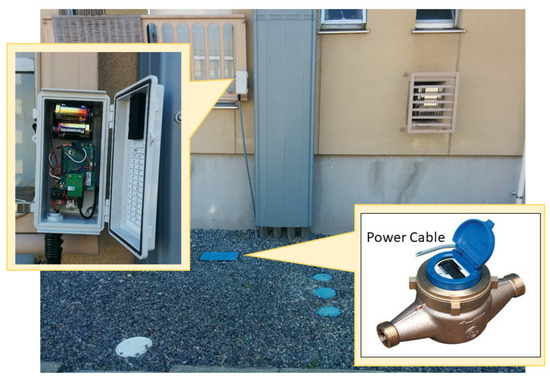
Figure 4.
The interface circuit using Arduino Uno R3 (left) and water meter (right) used in the system.
The electronic water meters (EKDA13, Azbil Kimmon Corp., Tokyo, Japan) were employed to measure daily water usage. Each meter is comprised of 8-bit telegraphic communication output, LSI, LCD, and a lithium battery. The exterior resembles that of a conventional home-used water meter, but unlike the latter, it can display the cumulative water usage and wirelessly transmit the data to the telecommunication metering system, once at each predefined time interval, such as every hour. To enable our wireless home gateway to receive water usage data from the electronic water meters, we designed a transformation interface circuit using Arduino Uno R3. This interface circuit receives the data and subsequently transmits them to our cloud service. A 3G communication unit with a SIM card (SORACOM IoT SIM, SORACOM INC., Tokyo, Japan) is connected to the gateway and is responsible for communication with the remote cloud service. Finally, the collected data are stored in a PostgreSQL database on the cloud services. The electronic water meter adopted in this study, along with its transformation communication interface between the home gateway and the water meter, is depicted in Figure 4. The obtained water data includes consumed water volume (unit: liters), measured time, and an ID for distinguishing the water meters. For the purpose of transmitting the two types of raw data from the sleep monitoring sensor and water meter, the JavaScript Object Notation (JSON) is employed to facilitate data transmission between the client home gateway and Node-RED on remote servers.
2.3. Subjects and Sensor Settings
A total of 18 local older people (11 males and 7 females, 77.2 ± 6.6 years old) were recruited for this study, with 10 of them selected to have electronic water meters installed in their homes (refer to Figure 4). The characteristics of the subjects are summarized in Table 2. Sleep monitoring devices (refer to Figure 3) were set under either their mattress or a thick bed quilt. The electronic water meter was installed to connect with each subject’s home’s original water meter in series to measure daily water usage. Home gateways with 3G communication units using the IoT connectivity service known as “SORACOM Air for cellular” (SORACOM INC., Tokyo, Japan) were also set up at each subject’s household. This study was approved by the Ethics Committee of Southern TOHOKU Hospital, Fukushima, Japan. Following a detailed explanation of the investigation’s objective, informed consent was obtained from each subject or their household before data collection.

Table 2.
A summary of subjects.
2.4. Data Collection and Evaluation
Based on the raw data, four aspects of data analysis were performed to assess the proposed system.
2.4.1. Long-Term Measurement of HR and RR
HR was recorded in seconds on a beat-by-beat basis, and RR was recorded on a breath-by-breath basis during sleep. The averaged HR and RR of each subject every night were calculated to track long-term changes and corresponding trends.
2.4.2. Measurement of BM
The accumulative time and number of BM durations during sleep, changing with sleep duration time, were measured. In the present study, we used the average BM rate (BMR) to assess the frequency of BM during sleep. The BMR was defined as the number of BM occurrences every hour. The BMR is considered an index related to the quality of sleep [41]. The average BMR was calculated for each subject every night.
2.4.3. Measurement of Daily Water Usage
The daily water usage data of each subject or their household was collected every hour. To understand their daily water usage habits, the variation of daily water usage was first analyzed. Through analysis, we can observe the time distributions of daily living activities, including cooking, washing, bathing, and using the toilet. Furthermore, we plotted the time distributions of averaged water usage over a 24-h period based on the one-year data to analyze the variation of water usage and outline the regular pattern of water usage.
2.5. Feedback on the Analyzed Results
By analyzing the collected data and utilizing the opportunity to provide feedback to the households, we regularly organized gatherings where designated care administrators or physicians would provide face-to-face feedback of these results to the residents involved. Through this feedback process, we gained insight into their health conditions. When they required assistance about how to improve their health, designated care administrators or physicians offered help, suggestions, and care plans, thereby enhancing their quality of life. These gatherings also provided a platform for mutual communication, strengthening their connections, and preventing isolation, thus reducing the risk of solitary deaths.
3. Results
As a result, the measurements of the three kinds of vital signs during sleep for all subjects, as well as their daily water usage data, were consistently taken for one year from April 2016. In total, about 400,000,000 records were gathered. The typical data obtained from two subjects for a single day are shown in Figure 5, where it can be seen that the HR, RR, and BM profiles of each subject during sleep and water usage distributions over a 24-h period. The short bars on the vertical axes indicate the time and duration of BM. By comparing the results, the different trends of HR in the two subjects during sleep can be observed: the top one is relatively stable and the bottom one seems to be more jittery. Different sleep habits can be seen, such as the top lasting about 9.5 h while leaving the bed one time and the bottom showed about 7.5 h of sleep while leaving 3 times, maybe to go to the toilet. The top one did not only record sleep at night, but it also recorded the nap activity of the subject. Through the two examples above, it can be seen that the different living habits of users can be recorded using the proposed system.
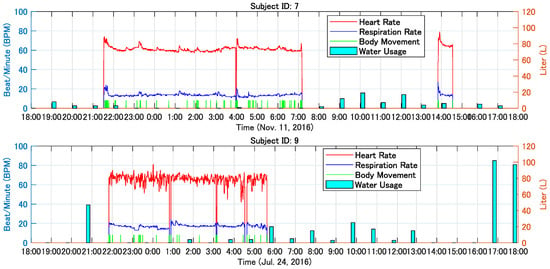
Figure 5.
Typical trends of HR, RR, BM, and water usage from two different subjects with time for one sleep cycle. Note that the measured time of data sent from water meters are not the same.
Figure 6 shows the daily water usage of two subjects over one year. The Y-axis denotes the volume of the daily consumed water in liters (L). The local area experiences summer from June to August every year, and therefore, it can be seen that the water usage during this period is relatively higher than other times. The blank periods denote no record or data loss.
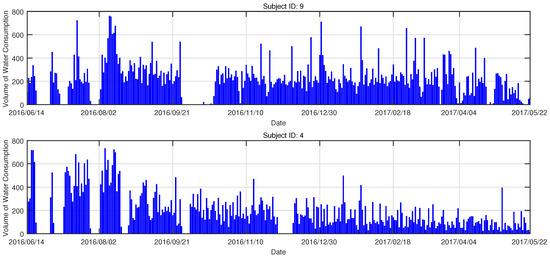
Figure 6.
Trends of the daily water usage from two subjects, respectively. X axis shows the period of about one year.
In order to analyze subjects’ daily habits and living patterns using water, we used the water usage data for about a year to generate histograms of the averaged water usage each hour for the 10 subjects whose homes were equipped with electronic water meters. These results are shown in Figure 7.
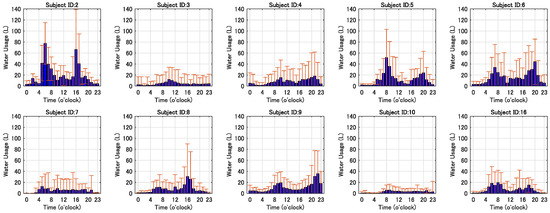
Figure 7.
The histograms display the means and deviations of water usage per hour over one year for ten subjects whose homes were equipped with electronic water meters. The subfigures for subjects with IDs 2, 4, 5, 6, 8, 9, and 16, respectively, exhibit the characteristic pattern of typical double-peak water usage.
Figure 8 shows histograms of sleep duration, latency, averaged HR, averaged RR, accumulated time of body movements, and leaving times of the subject with ID 13 while sleeping at night for one year. To track the long-term changes in the physical conditions of the subjects, we plotted the nightly averaged HR and RR as well as their standard deviations for the subjects. A typical example is shown in Figure 9. In the figure, the vertical axis denotes HR (beats/min) and RR (breaths/min). The curves and vertical bars with short horizontal lines at their upper and lower ends indicate the averaged values and standard deviations of detected HR and RR for the corresponding day.
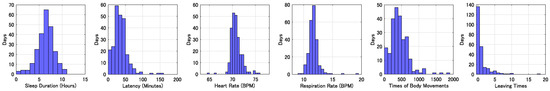
Figure 8.
The histograms of sleep duration, latency, average HR, average RR, the number of body movements, and leaving times of the subject with ID 13 each night for one year.
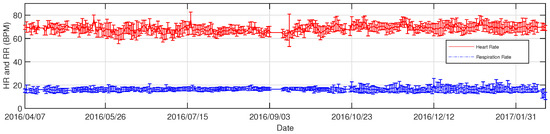
Figure 9.
The complete profiles of HR and RR from the subject with ID 13 for about one year. In this figure, the Y-axis denotes the HR (beats/min) and RR (breaths/min). The curves and vertical bars with short horizontal lines at their upper and lower ends indicate the mean values and standard deviations of the detected HR and RR for the corresponding day. Note that the vertical lines stand for the loss of data.
Figure 10 shows the trends of HR, RR, and BM from the subject with ID 13 during sleep for four days using a web-based GUI.
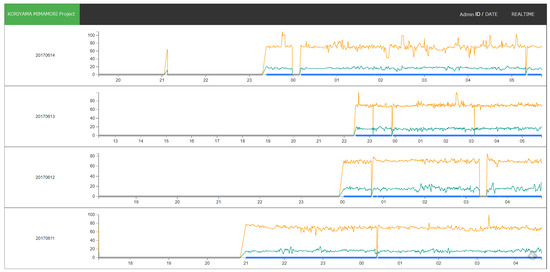
Figure 10.
The trends of HR (orange lines), RR (green lines), and BM (blue lines) from the subject with ID 13 during sleep for four days are displayed in a web-based GUI.
4. Discussion
The goal of this study was to provide a solution that would allow older people to maintain their autonomy and to increase their QoL, as well as being able to notify and contact the designated people in the case of an emergency to avoid solitary death as much as possible. Whether the system is effective depends on several major factors, including accurate, long-term measurements of vital signs, timely data analysis and feedback, and rapid response when an emergency is detected. For the telehealth monitoring system, data measurements and collections can be achieved unconstrainedly, unlike wearable devices that need users to wear, like Fitbits and smartwatches. Wearable devices are designed to collect users’ personal health data, but their inconveniences are easy to forget, especially for older people. Therefore, the continuity of the long-term monitoring approach proposed in the present article is ensured because it doesn’t require cumbersome operations and is less likely to be forgotten. Other types of measurement devices for vital signs, for example, blood pressure monitors with Bluetooth communication [42] and wearable watches [43], are compatible with the proposed system, but they were not adopted in the current system due to their obtrusiveness and intrusiveness of usage.
Simple water usage data may not directly reflect the health conditions of users, but long-term information can be used to analyze and judge whether the daily living pattern of the users is regular or not, as a regular life is generally important for everyone, especially older people. For example, when there is no water usage over a certain time interval, e.g., 12 h, for older people living alone and rarely leaving their home, it may indicate that they have suddenly suffered a critical disease onset or a serious accident that makes self-aid impossible. Therefore, the data can be used to detect some emergencies. Certainly, there are some limitations to this method because a relatively long time, for example, several hours, is usually required to detect an emergency, meaning that the method may be helpless for rescuing some critical patients due to serious diseases, such as heart attacks and strokes. In addition, family activities such as cooking, laundry, bathing, and cleaning all require a certain level of physical effort. By analyzing changes and patterns in water usage, it is possible to assess whether users, especially those living alone, require support and care in their daily lives. This approach can serve as an indicator of an individual’s ability to carry out daily activities.
Further data analysis and comparison based on the telehealth monitoring system can detect normal/abnormal states, living patterns, and rhythms. For example, in Figure 7, it can be seen that the averaged water usage each hour between the subjects was significantly different, but most results clearly show water usage peaking twice in one day, i.e., two intervals of 7 to 12 o’clock and 16 to 20 o’clock. This normal state reflects one aspect of subjects’ regular life, which is significant for their health. On the contrary, a relatively ’abnormal state’ indicates a lack of habitual routines, irregular cooking with frequent reliance on takeout, and infrequent laundering or bathing. These abnormal states could be attributed to changes in physical or health conditions, as well as poor lifestyle habits. During the validation phase, the detection of these states was achieved through offline comparison of histogram graphs. It is important to note that the concepts of normal and abnormal states are relative and lack absolute significance. On the other hand, when an emergency is detected, a fast reaction from family members, relatives, or assigned healthcare caregivers is necessary. This work was supported by the local city government to develop and evaluate a solution to maintain the autonomy of the local older people living alone or the older family needing support, e.g., regular visiting and cooking, to improve their quality of life. Rapid aging is a serious social problem in Japan, which is caused by the current rapid aging and sub-replacement fertility. Based on the proposed telehealth monitoring system, older people can be monitored unobtrusively 24 h a day, while their privacy can also be protected as much as possible compared to other kinds of approaches, e.g., video monitoring systems [3,4]. The framework of the system is flexible and compatible with many other types of methods for collecting vital signs, such as infrared and Doppler radar. Thus, various telehealth monitoring systems can be rapidly derived and constructed to meet specific needs.
The proposed telehealth monitoring system is also helpful in preventing and quickly identifying solitary death (dying alone), which is an increasingly serious problem in Japan. According to the statistics [44] from the government of Japan, thousands of older people nationwide die alone every year. Solitary death results in high costs with regard to dealing with the remains and personal belongings of the deceased, which has a very negative impact on their family and neighbors. The phenomenon of solitary death is mainly attributed to a decreasing proportion of older Japanese people living in multi-generational housing and instead living alone [32,45]. Older people who live alone are more likely to lack social contacts with family and neighbors, and are therefore more likely to die alone and remain undiscovered. By introducing the proposed telehealth monitoring system, the life rhythms and living patterns of older people living alone can be recorded and analyzed. When remarkable changes are detected, the early warning and decision support functions of this system can promptly notify their families and health advisors for acquiring further responses. Further work related to data analysis is still in progress, and the results will be presented in the near future.
As mentioned above in Figure 6 and Figure 9, the entire procedure of data collection lasting about one year suffered from data loss (several blank intervals) due to several reasons below. First, the home gateway routers responsible for data communication were accidentally switched off by users. Second, data transmission units encountered troubles due to long-time communication overload. Additionally, traveling away from home or hospitalization were also reasons for some data loss. Despite several cases of data loss or blank periods, the time trend of daily water usage is clear, and changes in at-home activities can be identified using water usage. Because the continuity of the data is crucial for predicting the risk of potential diseases or detecting emergency states, we are currently addressing the mentioned issues to ensure data continuity and maintain the system’s reliability, such as detecting accidental interruptions in power supply and strengthening the load capacity of data transmission units.
In the present study, we reported an IoT-based telehealth monitoring system that integrates sleep monitoring sensors and electronic water meters based on Node-RED, an open-source integration framework for IoT-based application development. There are currently several alternative technologies or frameworks similar to Node-RED, such as Eclipse Kura and Flogo. Here, we provided an example of how to construct an IoT-based health monitoring system using current popular IoT technologies. We believe that more health monitoring systems related to IoT will be constantly developed not only for older people but also for various other groups, contributing to improving people’s health and addressing the shortage of doctors, nurses, and home caregivers. Moreover, it may be beneficial to construct a next-generation telemedicine system that can predict users’ health levels and the risks of lifestyle-related diseases. Finally, the data collected from the sleep sensor also have the potential to be used for detecting various diseases such as cardiac arrhythmia, sleep apnea syndrome, and sleep disorders. Our research in this area is still in progress, and the results will be reported in the near future.
5. Conclusions
The increasing demand for home health care has led to the development of various home telehealth monitoring systems based on IoT and ICT. By integrating an unconstrained sleep monitoring sensor and an electronic water meter, and connecting them with a centralized cloud service, we successfully constructed an IoT-based home telehealth monitoring system aimed at monitoring users’ daily activities over the long term. Compared to existing healthcare monitoring solutions, this system conducts entirely unobtrusive measurements and provides continuous 24-h monitoring. Our results demonstrate the validity of the proposed system for daily, unconstrained sleep monitoring and living activities. Therefore, we consider it an ideal solution for long-term home healthcare monitoring. Finally, while users are living in their homes, sleep monitoring and water usage can be automatically and unconsciously recorded. This approach demonstrates its convenience compared to monitoring methods based on traditional video/audio communication and/or wearable devices.It also suggests that the proposed unobtrusive telehealth monitoring system has great potential for supporting long-term home healthcare monitoring.
Author Contributions
Conceptualization, Z.T. and L.J.; methodology, Z.T. and L.J.; software, Z.T.; validation, Z.T. and L.J.; data curation, L.J.; writing—original draft preparation, Z.T.; writing—review and editing, X.Z., L.J. and M.H.; visualization, L.J.; supervision, X.Z. and M.H.; project administration, Z.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research was partially funded by grants-in-aid from the Koriyama Demonstration Experiment Project of Health Monitoring System 2016–2019, Koriyama City, Fukushima, Japan.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Southern TOHOKU Hospital, Fukushima, Japan.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Acknowledgments
We thank Kaoru Sakatani, Hiroyuki Hashimoto, Kaori Matsumoto for providing great support and Tadao Munakata, Katsuhiko Nishimaki, and Satoshi Maeda for their help in implementing Node-RED based data collection and AWS-based data analysis. We would like to thank Lizhen Hu, Harumi Igarashi, Yuta Murayama, and Yutaka Sato for their advice and assistance during the course of this project. We also thank Koji Otani for providing many valuable suggestions on this paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Grant, J.S.; Elliott, T.R.; Weaver, M.; Bartolucci, A.A.; Giger, J.N. Telephone Intervention with Family Caregivers of Stroke Survivors After Rehabilitation. Stroke 2002, 33, 2060–2065. [Google Scholar] [CrossRef] [PubMed]
- Badger, T.A.; Segrin, C.; Hepworth, J.T.; Pasvogel, A.; Weihs, K.; Lopez, A.M. Telephone-delivered health education and interpersonal counseling improve quality of life for Latinas with breast cancer and their supportive partners. Psycho-Oncology 2013, 22, 1035–1042. [Google Scholar] [CrossRef] [PubMed]
- Dick, P.T.; Filler, R.; Pavan, A. Participant satisfaction and comfort with multidisciplinary pediatric telemedicine consultations. J. Pediatr. Surg. 1999, 34, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.S.; Callahan, C.W.; Sheets, S.J.; Moreno, C.N.; Malone, F.J. An Internet-based store-and-forward video home telehealth system for improving asthma outcomes in children. Am. J. Health-Syst. Pharm. 2003, 60, 1976–1981. [Google Scholar] [CrossRef]
- Artinian, N.T.; Harden, J.K.; Kronenberg, M.W.; Vander Wal, J.S.; Daher, E.; Stephens, Q.; Bazzi, R.I. Pilot study of a Web-based compliance monitoring device for patients with congestive heart failure. Heart Lung J. Acute Crit. Care 2003, 32, 226–233. [Google Scholar] [CrossRef]
- Wantland, D.J.; Portillo, C.J.; Holzemer, W.L.; Slaughter, R.; McGhee, E.M. The effectiveness of Web-based vs. non-Web-based interventions: A meta-analysis of behavioral change outcomes. J. Med. Internet Res. 2004, 6, e40. [Google Scholar] [CrossRef]
- Lazakidou, A.A. Web-Based Applications in Healthcare and Biomedicine; Springer: New York City, NY, USA, 2010. [Google Scholar]
- Dhillon, J.S.; Ramos, C.; Wünsche, B.C.; Lutteroth, C. Designing a web-based telehealth system for elderly people: An interview study in New Zealand. In Proceedings of the 2011 24th International Symposium on Computer-Based Medical Systems (CBMS), Bristol, UK, 27–30 June 2011. [Google Scholar]
- Ohta, S.; Nakamoto, H.; Shinagawa, Y.; Tanikawa, T. A health monitoring system for elderly people living alone. J. Telemed. Telecare 2002, 8, 151–156. [Google Scholar] [CrossRef]
- DelliFraine, J.L.; Dansky, K. Home-based telehealth: A review and meta-analysis. J. Telemed. Telecare 2008, 14, 62–66. [Google Scholar] [CrossRef]
- Koch, S. Home telehealth—Current state and future trends. Int. J. Med. Inform. 2006, 75, 565–576. [Google Scholar] [CrossRef]
- Peng, Y.T.; Lin, C.Y.; Sun, M.T.; Landis, C.A. Multimodality Sensor System for Long-Term Sleep Quality Monitoring. Telemed. e-Health 2010, 16, 244–253. [Google Scholar] [CrossRef]
- Jiang, L.; Tang, Z.; Liu, Z.; Chen, W.; Kitamura, K.I.; Nemoto, T. Automatic sleep monitoring system for home healthcare. In Proceedings of the Proceedings of 2012 IEEE-EMBS International Conference on Biomedical and Health Informatics, Hong Kong, China, 5–7 January 2012; pp. 894–897. [Google Scholar]
- Jaana, M.; Paré, G. Home telemonitoring of patients with diabetes: A systematic assessment of observed effects. J. Eval. Clin. Pract. 2007, 13, 242–253. [Google Scholar] [CrossRef]
- Tamura, T.; Sekine, M.; Tang, Z.; Yoshida, M.; Takeuchi, Y.; Imai, M. Preliminary study of a new home healthcare monitoring to prevent the recurrence of stroke. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 5489–5492. [Google Scholar]
- Weiner, M.; Callahan, C.M.; Tierney, W.M.; Overhage, J.M.; Mamlin, B.; Dexter, P.R.; McDonald, C.J. USing information technology to improve the health care of older adults. Ann. Intern. Med. 2003, 139, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Bouabida, K.; Lebouché, B.; Pomey, M.P. Telehealth and COVID-19 Pandemic: An Overview of the Telehealth Use, Advantages, Challenges, and Opportunities during COVID-19 Pandemic. Healthcare 2022, 10, 2293. [Google Scholar] [CrossRef]
- Hassanalieragh, M.; Page, A.; Soyata, T.; Sharma, G.; Aktas, M.; Mateos, G.; Kantarci, B.; Andreescu, S. Health monitoring and management using Internet-of-Things (IoT) sensing with cloud-based processing: Opportunities and challenges. In Proceedings of the 2015 IEEE international conference on services computing, New York, NY, USA, 27 June–2 July 2015; pp. 285–292. [Google Scholar]
- Islam, S.R.; Kwak, D.; Kabir, M.H.; Hossain, M.; Kwak, K.S. The Internet of Things for Health Care: A Comprehensive Survey. IEEE Access 2015, 3, 678–708. [Google Scholar] [CrossRef]
- Yuehong, Y.I.N.; Zeng, Y.; Chen, X.; Fan, Y. The internet of things in healthcare: An overview. J. Ind. Inf. Integr. 2016, 1, 3–13. [Google Scholar]
- Scuro, C.; Sciammarella, P.F.; Lamonaca, F.; Olivito, R.S.; Carnì, D.L. IoT for Structural Health Monitoring. IEEE Instrum. Meas. Mag. 2018, 1094, 4–14. [Google Scholar] [CrossRef]
- Ruman, M.R.; Barua, A.; Rahman, W.; Jahan, K.R.; Roni, M.J.; Rahman, M.F. IoT based emergency health monitoring system. In Proceedings of the 2020 International Conference on Industry 4.0 Technology (I4Tech), IEEE, Pune, India, 13–15 February 2020; pp. 159–162. [Google Scholar]
- Siam, A.I.; Almaiah, M.A.; Al-Zahrani, A.; Elazm, A.A.; El Banby, G.M.; El-Shafai, W.; El-Samie, F.E.A.; El-Bahnasawy, N.A. Secure Health Monitoring Communication Systems Based on IoT and Cloud Computing for Medical Emergency Applications. Comput. Intell. Neurosci. 2021, 2021, 8016525. [Google Scholar] [CrossRef] [PubMed]
- Cao, S.; Lin, X.; Hu, K.; Wang, L.; Li, W.; Wang, M.; Le, Y. Cloud computing-based medical health monitoring IoT system design. Mob. Inf. Syst. 2021, 2021, 8278612. [Google Scholar] [CrossRef]
- Dziak, D.; Jachimczyk, B.; Kulesza, W.J. IoT-Based Information System for Healthcare Application: Design Methodology Approach. Appl. Sci. 2017, 7, 596. [Google Scholar] [CrossRef]
- Park, K.; Park, J.; Lee, J. An IoT System for Remote Monitoring of Patients at Home. Appl. Sci. 2017, 7, 260. [Google Scholar] [CrossRef]
- Guan, K.; Shao, M.; Wu, S. A Remote Health Monitoring System for the Elderly Based on Smart Home Gateway. J. Healthc. Eng. 2017, 2017, 5843504. [Google Scholar] [CrossRef]
- Abdelgawad, A.; Yelamarthi, K.; Khattab, A. IoT-Based Health Monitoring System for Active and Assisted Living. In Proceedings of the Smart Objects and Technologies for Social Good: Second International Conference, GOODTECHS 2016, Venice, Italy, 30 November–1 December 2017; pp. 11–20. [Google Scholar]
- Kumar, S.; Buckley, J.L.; Barton, J.; Pigeon, M.; Newberry, R.; Rodencal, M.; Hajzeraj, A.; Hannon, T.; Rogers, K.; Casey, D.; et al. A wristwatch-based wireless sensor platform for IoT health monitoring applications. Sensors 2020, 20, 1675. [Google Scholar] [CrossRef]
- Stefanova-Pavlova, M.; Andonov, V.; Stoyanov, T.; Angelova, M.; Cook, G.; Klein, B.; Vassilev, P.; Stefanova, E. Modeling telehealth services with generalized nets. Recent Contrib. Intell. Syst. 2017, 657, 279–290. [Google Scholar]
- Kalogeropoulos, D.; Kalogeropoulos, C.; Stefaniotou, M.; Neofytou, M. The role of tele-ophthalmology in diabetic retinopathy screening. J. Optom. 2020, 13, 262–268. [Google Scholar] [CrossRef]
- Nomura, M.; McLean, S.; Miyamori, D.; Kakiuchi, Y.; Ikegaya, H. Isolation and unnatural death of elderly people in the aging Japanese society. Sci. Justice 2016, 56, 80–83. [Google Scholar] [CrossRef]
- Nakazawa, E.; Yamamoto, K.; London, A.J.; Akabayashi, A. Solitary death and new lifestyles during and after COVID-19: Wearable devices and public health ethics. BMC Med. Ethics 2021, 22, 89. [Google Scholar] [CrossRef]
- Cheng, H.T.; Zhuang, W. Bluetooth-enabled in-home patient monitoring system: Early detection of Alzheimer’s disease. IEEE Wirel. Commun. 2010, 17, 74–79. [Google Scholar] [CrossRef]
- Tsukiyama, T. In-home health monitoring system for solitary elderly. Procedia Comput. Sci. 2015, 63, 229–235. [Google Scholar] [CrossRef]
- Chatrati, S.P.; Hossain, G.; Goyal, A.; Bhan, A.; Bhattacharya, S.; Gaurav, D.; Tiwari, S.M. Smart home health monitoring system for predicting type 2 diabetes and hypertension. J. King Saud-Univ.-Comput. Inf. Sci. 2022, 34, 862–870. [Google Scholar] [CrossRef]
- Dhruba, A.R.; Alam, K.N.; Khan, M.S.; Bourouis, S.; Khan, M.M. Development of an IoT-Based Sleep Apnea Monitoring System for Healthcare Applications. Comput. Math. Methods Med. 2021, 2021, 7152576. [Google Scholar] [CrossRef]
- Jeong, J.W.; Lee, W.; Kim, Y.J. A real-time wearable physiological monitoring system for home-based healthcare applications. Sensors 2022, 22, 104. [Google Scholar] [CrossRef]
- Wu, J.Y.; Wang, Y.; Ching, C.T.S.; Wang, H.M.D.; Liao, L.D. IoT-based wearable health monitoring device and its validation for potential critical and emergency applications. Front. Public Health 2023, 11, 1188304. [Google Scholar] [CrossRef] [PubMed]
- Tang, Z.; Jiang, L.; Hu, L.; Sato, Y.; Komuro, Y.; Sakatani, K. Preliminary Study of Sleep Quality Assessment for Elderly People Based on Unobtrusive Sleep Monitoring System. Trans. Jpn. Soc. Med. Biol. Eng. 2017, 55, 552–553. [Google Scholar]
- Lu, L.; Tamura, T.; Togawa, T. Detection of body movements during sleep by monitoring of bed temperature. Physiol. Meas. 1999, 20, 137. [Google Scholar] [CrossRef] [PubMed]
- AND Digital Blood Pressure Monitor Model UA-767. Available online: https://www.aandd.co.jp/adhome/products/me/ua767pbt-c.html (accessed on 17 October 2022).
- Zheng, Y.L.; Ding, X.R.; Poon, C.C.Y.; Lo, B.P.L.; Zhang, H.; Zhou, X.L.; Yang, G.Z.; Zhao, N.; Zhang, Y.T. Unobtrusive sensing and wearable devices for health informatics. IEEE Trans. Biomed. Eng. 2014, 61, 1538–1554. [Google Scholar] [CrossRef] [PubMed]
- Summary of the 2014 White Paper on Aging Society of Japan. Available online: http://www8.cao.go.jp/kourei/whitepaper/w-2014/gaiyou/s1_2_6.html (accessed on 17 October 2022).
- Morita, S.; Nishi, K.; Furukawa, S.; Hitosugi, M. A Survey of Solitary Deaths in Japan for Shortening Postmortem Interval Until Discover. Prilozi 2015, 36, 47–51. [Google Scholar] [CrossRef][Green Version]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).