Beyond the Preston Curve: Analyzing Variations in Life Expectancy Around the World Using Multivariate Regression Circa 2000 and 2015
Abstract
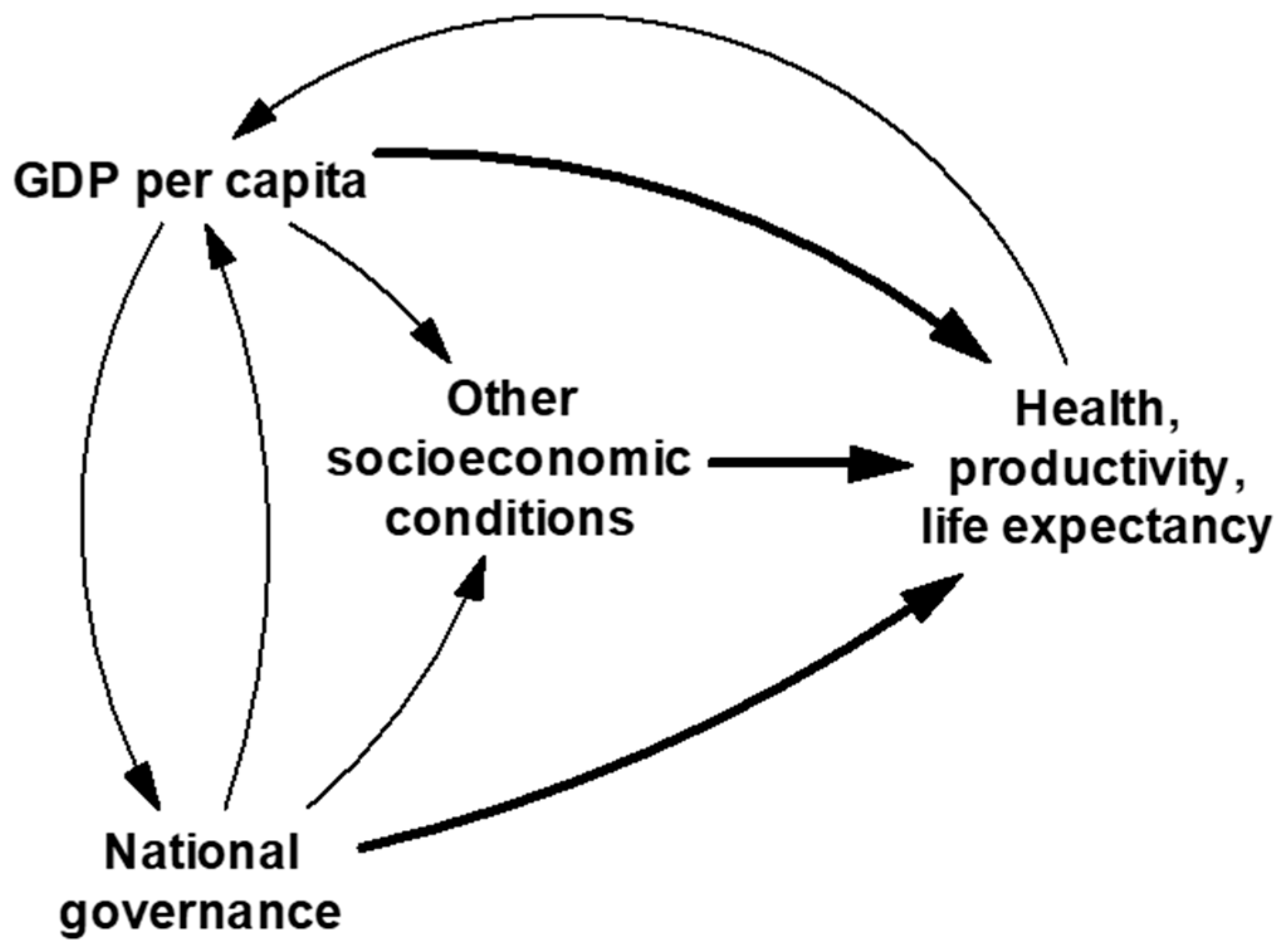
1. Introduction
2. Materials and Methods
2.1. Data
2.2. Analysis
3. Results
3.1. Regression Results
3.2. Results for the 15 Largest (Most Populous) Countries
4. Discussion
4.1. Summary and Contribution
4.2. Limitations and Extensions
5. Conclusions
Supplementary Materials
Funding
Data Availability Statement
Conflicts of Interest
References
- Preston, S.H. The changing relation between mortality and level of economic development. Popul. Stud. 1975, 29, 231–248, reprinted in Int. J. Epidem. 2007, 36, 484–490. [Google Scholar] [CrossRef]
- Riley, J.C. Estimates of regional and global life expectancy, 1800–2001. Popul. Devel. Rev. 2005, 31, 537–543. [Google Scholar] [CrossRef]
- World Bank. Life Expectancy at Birth, Total (Years). 2024. Available online: https://data.worldbank.org/indicator/sp.dyn.le00.in (accessed on 30 June 2025).
- Cutler, D.; Deaton, A.; Lleras-Muney, A. The determinants of mortality. J. Econ. Perspect. 2006, 20, 97–120. [Google Scholar] [CrossRef]
- Braveman, P.A.; Cubbin, C.; Egerter, S.; Williams, D.R.; Pamuk, E. Socioeconomic disparities in health in the United States: What the patterns tell us. Am. J. Public Health 2010, 100 (Suppl. S1), S186–S196. [Google Scholar] [CrossRef]
- Chetty, R.; Stepner, M.; Abraham, S.; Lin, S.; Scuderi, B.; Turner, N.; Bergeron, A.; Cutler, D. The association between income and life expectancy in the United States, 2001–2014. JAMA 2016, 315, 1750–1766. [Google Scholar] [CrossRef]
- Bundy, J.D.; Mills, K.T.; He, H.; LaVeist, T.A.; Ferdinand, K.C.; Chen, J.; He, J. Social determinants of health and premature death among adults in the USA from 1999 to 2018: A national cohort study. Lancet Public Health 2023, 8, e422–e431. [Google Scholar] [CrossRef]
- Lin, R.T.; Chen, Y.M.; Chien, L.C.; Chan, C.C. Political and social determinants of life expectancy in less developed countries: A longitudinal study. BMC Public Health 2012, 12, 85. [Google Scholar] [CrossRef]
- Mondal, M.N.; Shitan, M. Impact of socio-health factors on life expectancy in the low and lower middle income countries. Iran. J. Public Health 2013, 42, 1354–1362. [Google Scholar]
- Bayati, M.; Akbarian, R.; Kavosi, Z. Determinants of life expectancy in eastern Mediterranean region: A health production function. Int. J. Health Policy Manag. 2013, 1, 57–61. [Google Scholar] [CrossRef]
- Tarca, V.; Tarca, E.; Moscalu, M. Social and economic determinants of life expectancy at birth in Eastern Europe. Healthcare 2024, 12, 1148. [Google Scholar] [CrossRef]
- Karma, E. Socioeconomic determinants of life expectancy: Southeastern European countries. Eur. J. Sust. Devel. 2023, 12, 23–34. [Google Scholar] [CrossRef]
- Roffia, P.; Bucciol, A.; Hashlamoun, S. Determinants of life expectancy at birth: A longitudinal study on OECD countries. Int. J. Health Econ. Manag. 2022, 23, 189–212. [Google Scholar] [CrossRef] [PubMed]
- Homer, J.B. Life Expectancy in the U.S. and other OECD Countries: A Multivariate Analysis of Economic, Social, and Behavioral Factors. 2024. Available online: https://www.academia.edu/121497712/Life_Expectancy_in_the_U_S_and_Other_OECD_Countries_A_Multivariate_Analysis_of_Economic_Social_and_Behavioral_Factors (accessed on 30 June 2025).
- Kaufmann, D.; Kraay, A.; Zoido-Lobaton, P. Governance matters: From measurement to action. Financ. Dev. Int. Monet. Fund 2000, 37, 6. [Google Scholar]
- Mackenbach, J.P.; Stirbu, I.; Roskam, A.J.R.; Schaap, M.M.; Menvielle, G.; Leinsalu, M.; Kunst, A.E. Socioeconomic inequalities in health in 22 European countries. N. Engl. J. Med. 2008, 358, 2468–2481. [Google Scholar] [CrossRef]
- Bradley, E.H.; Elkins, B.R.; Herrin, J.; Elbel, B. Health and social services expenditures: Associations with health outcomes. BMJ Qual. Saf. 2011, 20, 826–831. [Google Scholar] [CrossRef] [PubMed]
- National Research Council (US). US Health in International Perspective: Shorter Lives, Poorer Health; Woolf, S.H., Aron, L., Eds.; National Academies Press: Washington, DC, USA, 2013; 394p. [Google Scholar]
- Pickett, K.E.; Wilkinson, R.G. Income inequality and health: A causal review. Soc. Sci. Med. 2015, 128, 316–326. [Google Scholar] [CrossRef]
- McCullough, J.M.; Leider, J.P. Government spending in health and nonhealthy sectors associated with improvement in county health rankings. Health Aff. 2016, 35, 2037–2043. [Google Scholar] [CrossRef]
- Bor, J.; Cohen, G.H.; Galea, S. Population health in an era of rising income inequality: USA, 1980–2015. Lancet 2017, 389, 1475–1490. [Google Scholar] [CrossRef]
- Enroth, L.; Jasilionis, D.; Németh, L.; Strand, B.H.; Tanjung, I.; Sundberg, L.; Fors, S.; Jylhä, M.; Brønnum-Hansen, H. Changes in socioeconomic differentials in old age life expectancy in four Nordic countries: The impact of educational expansion and education-specific mortality. Eur. J. Ageing 2022, 19, 161–173. [Google Scholar] [CrossRef]
- IHME-CHAIN Collaborators. Effects of education on adult mortality: A global systematic review and meta-analysis. Lancet Public Health 2024, 9, e155–e165. [Google Scholar] [CrossRef]
- EPIC/AQLI. Air Pollution Remains the Greatest External Risk to Human Health as Most Countries Fail to Set or Meet Their Own Standards for Clean Air. Energy Policy Institute, University of Chicago: Chicago, IL, USA, 2024. Available online: https://epic.uchicago.edu/news/air-pollution-remains-the-greatest-external-risk-to-human-health-as-most-countries-fail-to-set-or-meet-their-own-standards-for-clean-air/ (accessed on 30 June 2025).
- Homer, J. Can good government save us? Extending a climate-population model to include governance and its effects. Systems 2022, 10, 37. [Google Scholar] [CrossRef]
- Memon, M.A.; Ting, H.; Cheah, J.-H.; Thurasamy, R.; Chuan, F.; Cham, T.H. Sample size for survey research: Review and recommendations. J. Appl. Struct. Equ. Model. 2020, 4, i–xx. [Google Scholar] [CrossRef]
- Kim, J.H. Multicollinearity and misleading statistical results. Korean J. Anesth. 2019, 72, 558–569. [Google Scholar] [CrossRef] [PubMed]
- Drèze, J.; Sen, A. China and India. In Hunger and Public Action; Oxford University Press: Oxford, UK, 1991; Chapter 11; pp. 204–225. ISBN 9780198283652. [Google Scholar]
- Prasad, A.; Lakhanpaul, M.; Narula, S.; Patel, V.; Piot, P.; Venkatapuram, S. Accounting for the future of health in India. Lancet 2017, 389, 680–682. [Google Scholar] [CrossRef] [PubMed]
- Freeman, T.; Gesesew, H.A.; Bambra, C.; Giugliani, E.R.J.; Popay, J.; Sanders, D.; Macinko, J.; Musolino, C.; Baum, F. Why do some countries do better or worse in life expectancy relative to income? An analysis of Brazil, Ethiopia, and the United States of America. Int. J. Equity Health 2020, 19, 202–220. [Google Scholar] [CrossRef]
- Roser, M. Why Is Life Expectancy in the US Lower than in Other Rich Countries? 2020. Available online: https://ourworldindata.org/us-life-expectancy-low (accessed on 30 June 2025).
- GBD Indonesia. The state of health in Indonesia’s provinces, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Glob. Health 2022, 10, e1632–e1645. [Google Scholar] [CrossRef]
- GBD Pakistan. The state of health in Pakistan and its provinces and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Glob. Health 2023, 11, e229–e243. [Google Scholar] [CrossRef]
- Aburto, J.M.; Calazans, J.; Queiroz, B.L.; Luhar, S.; Canudas-Romo, V. Uneven state distribution of homicides in Brazil and their effect on life expectancy, 2000–2015: A cross-sectional mortality study. BMJ Open 2021, 11, e044706. [Google Scholar] [CrossRef]
- Lawanson, O.I.; Umar, D.I. The life expectancy-economic growth nexus in Nigeria: The role of poverty reduction. SN Bus. Econ. 2021, 1, 127–152. [Google Scholar] [CrossRef]
- GBD Bangladesh. The burden of diseases and risk factors in Bangladesh, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Glob. Health 2023, 11, e1931–e1942. [Google Scholar] [CrossRef]
- Mitra, D.K.; Mridha, M.K. Sustaining progress in the health landscape of Bangladesh. Lancet 2023, 11, e1838–e1839. [Google Scholar] [CrossRef]
- Brainerd, E. Mortality in Russia since the fall of the Soviet Union. Compar. Econ. Stud. 2021, 63, 557–576. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, N.; Saito, E.; Kondo, N.; Inoue, M.; Ikeda, S.; Satoh, T.; Wada, K.; Stickley, A.; Katanoda, K.; Mizoue, T.; et al. What has made the population of Japan healthy? Lancet 2011, 378, 1094–1105. [Google Scholar] [CrossRef] [PubMed]
- Zazueta-Borboa, J.-D.; Vázquez-Castillo, P.; Gargiulo, M.; Aburto, J.M. The impact of violence and COVID-19 on Mexico’s life-expectancy losses and recent bounce-back, 2015-22. Int. J. Epidem. 2025, 54, dyaf034. [Google Scholar] [CrossRef]
- GBD Ethiopia. Progress in health among regions of Ethiopia, 1990-2019: A subnational country analysis for the Global Burden of Disease Study 2019. Lancet 2022, 399, 1322–1335. [Google Scholar] [CrossRef] [PubMed]
- Cruz, G.T.; Cruz, C.J.P.; Saito, Y. Is there compression or expansion of morbidity in the Philippines? Geriatr. Gerontol. Int. 2022, 22, 511–515. [Google Scholar] [CrossRef]
- Rauch, J.E. Egypt: An Economic Growth Success, Yet a Health Failure? Cairo Review of Global Affairs. 2023. Available online: https://www.thecairoreview.com/essays/egypt-an-economic-growth-success-yet-a-health-failure/ (accessed on 30 June 2025).
- Nguyen, T.T.; Trevisan, M. Vietnam a country in transition: Health challenges. BMJ Nutr. Prev. Health 2020, 3, e000069. [Google Scholar] [CrossRef]
- Milstein, B.; Payne, B.; Kelleher, C.; Homer, J.; Norris, T.; Roulier, M.; Saha, S. Organizing around vital conditions moves the social determinants agenda into wider action. Health Aff. Forefr. 2023. [Google Scholar] [CrossRef]
- Askew, I.; Raney, L.; Kerrigan, M.; Sridhar, A. Family planning saves maternal and newborn lives: Why universal access to contraception must be prioritized in national maternal and newborn health policies, financing, and programs. Int. J. Gynecol. Obs. 2024, 164, 536–540. [Google Scholar] [CrossRef]
- Greene, W.H. Econometric Analysis, 8th ed; Pearson: Chennai, India, 2018; 392p. [Google Scholar]
- Homer, J. The growth and stagnation of US life expectancy: A dynamic simulation model and implications. Systems 2024, 12, 510. [Google Scholar] [CrossRef]
- Homer, J. Modeling global loss of life from climate change through 2060. Syst. Dyn. Rev. 2020, 36, 523–535. [Google Scholar] [CrossRef]
- Roy, D.; Rao, G.V. Stochastic Dynamics, Filtering and Optimization; Cambridge University Press: Cambridge, UK, 2017; 742p. [Google Scholar]
| Variable | Unit | Period | Countries | Best | Worst | Mean |
|---|---|---|---|---|---|---|
| Life expectancy at birth | years | 2000–2004 | 150 | 81.6 | 43.8 | 67.0 |
| 2015–2019 | 150 | 84.6 | 52.3 | 72.1 | ||
| GDP per capita | USD 2015 | 2000–2004 | 150 | USD 74,718 | USD 277 | USD 10,897 |
| 2015–2019 | 150 | USD 86,424 | USD 286 | USD 13,337 | ||
| Stability and peace | percent | 2000–2004 | 150 | 83.5 | 3.6 | 46.3 |
| 2015–2017 | 150 | 80.2 | 0.0 | 45.6 | ||
| Rule of law | percent | 2000–2004 | 150 | 89.4 | 15.9 | 47.3 |
| 2015–2017 | 150 | 91.4 | 13.9 | 48.6 | ||
| Control of corruption | percent | 2000–2004 | 150 | 98.3 | 18.9 | 48.1 |
| 2015–2017 | 150 | 94.5 | 15.0 | 47.7 | ||
| Voice and accountability | percent | 2000–2004 | 150 | 82.8 | 8.3 | 47.4 |
| 2015–2017 | 150 | 83.7 | 6.9 | 47.3 | ||
| Government effectiveness | percent | 2000–2004 | 150 | 93.4 | 14.6 | 49.1 |
| 2015–2017 | 150 | 94.8 | 9.4 | 49.6 | ||
| Regulatory quality | percent | 2000–2004 | 150 | 87.7 | 7.7 | 49.5 |
| 2015–2017 | 150 | 93.5 | 4.4 | 50.4 | ||
| Safe sanitation | percent | 2000–2002 | 149 | 100 | 3.6 | 66.6 |
| 2015–2017 | 149 | 100 | 7.1 | 74.2 | ||
| Years of schooling (age 25+) | years | 1996–2004 | 146 | 12.7 | 1.1 | 7.0 |
| 2013–2017 | 149 | 14.1 | 1.4 | 8.5 | ||
| CO2 emissions per capita | metric tons | 1999–2003 | 147 | 0.0 | 40.1 | 4.5 |
| 2014–2018 | 147 | 0.0 | 32.4 | 4.4 | ||
| Gini index (income inequality) | percent | 1996–2004 | 116 | 24.3 | 64.7 | 40.4 |
| 2012–2018 | 146 | 25.8 | 59.1 | 37.6 | ||
| Physicians per 1000 population | ratio | 1996–2004 | 142 | 5.88 | 0.02 | 1.51 |
| 2012–2018 | 142 | 7.82 | 0.03 | 1.86 | ||
| Undernourishment | percent | 2000–2002 | 136 | 1.5 | 68.6 | 15.2 |
| 2015–2017 | 138 | 1.3 | 59.1 | 11.0 | ||
| Poverty (USD 3.20 PPP 2011 per person per day) | percent | 1996–2004 | 116 | 0.1 | 98.5 | 37.7 |
| 2012–2018 | 118 | 0.0 | 91.0 | 23.3 | ||
| Female literacy (age 15+) | percent | 1996–2004 | 115 | 99.8 | 9.4 | 71.9 |
| 2012–2018 | 112 | 100 | 13.9 | 82.2 | ||
| Contraception (women aged 15–49 with partners) | percent | 1996–2004 | 133 | 86.5 | 4.3 | 49.1 |
| 2012–2018 | 112 | 86.2 | 5.7 | 51.2 |
| ° | Explanatory Variables for Life Expectancy | |||||||
|---|---|---|---|---|---|---|---|---|
| Constant | ln(GDPPC) | Govt Effective % | Sanitation % | Poverty % | Contracept % | Gini % | CO2 MT per Cap | |
| Earlier period (1996–2004) | ||||||||
| Model E1. All variables, N = 102, R-squared = 0.863, mean absolute error = 3.16 years | ||||||||
| Coefficient | 60.4 | 0.099 | 0.088 | −0.088 | 0.167 | −0.200 | −0.472 | |
| p-value | 2 × 10−28 | 0.005 | 0.002 | 0.001 | 2 × 10−7 | 7 × 10−5 | 0.003 | |
| VIF | 2.7 | 5.0 | 4.6 | 3.4 | 1.2 | 2.8 | ||
| Model E2. All variables except Gini and CO2, N = 102, R-squared = 0.832, MAE = 3.25 years | ||||||||
| Coefficient | 52.6 | 0.066 | 0.085 | -0.082 | 0.155 | |||
| p-value | 1 × 10−29 | 0.04 | 0.003 | 0.005 | 6 × 10−6 | |||
| VIF | 2.0 | 4.5 | 4.5 | 3.3 | ||||
| Model E3a. GDPPC only, N = 102, R-squared = 0.622, MAE = 4.88 years | ||||||||
| Coefficient | 19.3 | 5.8 | ||||||
| p-value | 8 × 10−7 | 8 × 10−23 | ||||||
| Model E3b. GDPPC only, N = 150, R-squared = 0.649, MAE = 4.54 years | ||||||||
| Coefficient | 21.1 | 5.5 | ||||||
| p-value | 6 × 10−12 | 2 × 10−35 | ||||||
| Later period (2012–2019) | ||||||||
| Model L1. All variables, N = 91, R-squared = 0.856, MAE = 2.05 years | ||||||||
| Coefficient | 56.8 | 0.136 | 0.107 | −0.053 | 0.033 | |||
| p-value | 2 × 10−40 | 2 × 10−7 | 2 × 10−5 | 0.02 | 0.14 | |||
| VIF | 1.8 | 5.3 | 4.7 | 2.2 | ||||
| Model L2. All variables except contracept, N = 91, R-squared = 0.853, MAE = 2.13 years | ||||||||
| Coefficient | 57.6 | 0.143 | 0.118 | −0.056 | ||||
| p-value | 6 × 10−42 | 4 × 10−8 | 1 × 10−6 | 0.02 | ||||
| VIF | 1.8 | 4.8 | 4.7 | |||||
| Model L3a. GDPPC only, N = 91, R-squared = 0.725, MAE = 3.03 years | ||||||||
| Coefficient | 30.2 | 4.9 | ||||||
| p-value | 6 × 10−19 | 1 × 10−26 | ||||||
| Model L3b. GDPPC only, N = 150, R-squared = 0.739, MAE = 3.02 years | ||||||||
| Coefficient | 30.2 | 4.9 | ||||||
| p-value | 2 × 10−30 | 5 × 10−45 | ||||||
| Earlier Model Errors | Later Model Errors | |||||||
|---|---|---|---|---|---|---|---|---|
| Country | Actual 2000–2004 | Model E1 (6 Factors) | Model E2 (4 Factors) | Model E3a (1 Factor) | Actual 2015–2019 | Model L1 (4 Factors) | Model L2 (3 Factors) | Model L3a (1 Factor) |
| China | 72.9 | −3.3 | −4.3 | −7.8 | 77.4 | −1.5 | −2.2 | −2.4 |
| India | 63.6 | −2.8 | −4.6 | −5.3 | 70.4 | na | na | −3.4 |
| USA | 77.0 | −5.0 | 1.0 | 4.9 | 78.6 | 2.0 | 2.0 | 5.3 |
| Indonesia | 66.7 | −2.8 | −5.1 | −3.3 | 70.1 | 1.6 | 1.4 | 0.3 |
| Pakistan | 62.6 | −3.8 | −6.2 | −2.9 | 66.2 | 0.9 | 1.5 | −0.4 |
| Brazil | 70.4 | −0.5 | 1.8 | 0.1 | 74.8 | −0.5 | −1.1 | −0.3 |
| Nigeria | 48.0 | 3.8 | 4.8 | 14.4 | 52.3 | na | na | 16.3 |
| Bangladesh | 66.5 | −4.4 | −6.8 | −9.2 | 71.7 | −5.9 | −6.6 | −5.9 |
| Russian Federation | 65.3 | 4.3 | 7.0 | 5.7 | 72.2 | na | na | 3.9 |
| Japan | 81.6 | na | na | −2.3 | 84.1 | −3.8 | −2.9 | −2.6 |
| Mexico | 74.0 | −4.2 | −2.3 | −2.2 | 74.3 | 0.7 | 0.5 | 0.8 |
| Ethiopia | 51.8 | −0.3 | −2.7 | 0.1 | 64.8 | −4.6 | −4.9 | −2.3 |
| Philippines | 69.8 | −4.2 | −4.1 | −6.7 | 71.5 | 0.4 | 0.5 | −1.6 |
| Egypt | 68.4 | 3.9 | 1.4 | −3.3 | 71.1 | 1.8 | 1.9 | −0.5 |
| Vietnam | 72.8 | −4.5 | −6.6 | −12.9 | 74.0 | 0.4 | 0.0 | −5.7 |
| Mean absolute error | 3.4 | 3.9 | 5.4 | 2.0 | 2.1 | 3.4 | ||
| Life Expectancy | Apparent Key Drivers of Life Expectancy Change | |||||
|---|---|---|---|---|---|---|
| Country | Earlier 2000–2004 | Later 2015–2019 | Change | Based on the 6-Factor Regression Model (in Order of Calculated Impact) | Based on the Research Literature | Reference Numbers |
| China | 72.9 | 77.4 | 4.5 | Improvements in poverty, sanitation, and government effectiveness, but worsening CO2 emissions | A “war against pollution” was announced in 2014 and reduced particulate air pollution (PM2.5) by 40% by 2022 | [24,28] |
| India | 63.6 | 70.4 | 6.8 | Improvements in sanitation and poverty | Also, improvements in parasitic disease control, literacy, and female education | [28,29] |
| USA | 77.0 | 78.6 | 1.7 | Improvement in CO2 emissions, but worsening government effectiveness | Also, reductions in crime and violence | [7,24,30,31] |
| Indonesia | 66.7 | 70.1 | 3.4 | Improvements in poverty, sanitation, and contraception, but worsening Gini | (no additional) | [32] |
| Pakistan | 62.6 | 66.2 | 3.6 | Improvements in sanitation, poverty, and contraception | (no additional) | [33] |
| Brazil | 70.4 | 74.8 | 4.4 | Improvements in sanitation and poverty, but worsening government effectiveness | Also, newly instituted universal health coverage | [30,34] |
| Nigeria | 48.0 | 52.3 | 4.3 | Improvements in sanitation | Also, improved educational attainment | [35] |
| Bangladesh | 66.5 | 71.7 | 5.2 | Improvements in sanitation, poverty, and contraception | (no additional) | [36,37] |
| Russian Federation | 65.3 | 72.2 | 6.9 | Improvements in government effectiveness, sanitation, and poverty | Also, reduced alcohol consumption following strong policy measures of 2006 and 2010 | [38] |
| Japan | 81.6 | 84.1 | 2.5 | Improvements in government effectiveness | Also, increased educational attainment and urbanization | [39] |
| Mexico | 74.0 | 74.3 | 0.3 | Improvements in sanitation, poverty, and Gini, but worsening government effectiveness | Also, increased violence | [40] |
| Ethiopia | 51.8 | 64.8 | 13.1 | Improvements in contraception and poverty | Reductions in violence and undernourishment, plus improved female education and community-based health services | [30,41] |
| Philippines | 69.8 | 71.5 | 1.8 | Improvements in sanitation, poverty, and contraception | (no additional) | [42] |
| Egypt | 68.4 | 71.1 | 2.7 | Worsening government effectiveness | Improved control of infectious and parasitic diseases | [43] |
| Vietnam | 72.8 | 74.0 | 1.2 | Improvements in poverty, sanitation, and government effectiveness | Improvement has been hindered by a steep increase in chronic disease due to a more sedentary lifestyle and worse nutrition | [44] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Homer, J. Beyond the Preston Curve: Analyzing Variations in Life Expectancy Around the World Using Multivariate Regression Circa 2000 and 2015. Systems 2025, 13, 577. https://doi.org/10.3390/systems13070577
Homer J. Beyond the Preston Curve: Analyzing Variations in Life Expectancy Around the World Using Multivariate Regression Circa 2000 and 2015. Systems. 2025; 13(7):577. https://doi.org/10.3390/systems13070577
Chicago/Turabian StyleHomer, Jack. 2025. "Beyond the Preston Curve: Analyzing Variations in Life Expectancy Around the World Using Multivariate Regression Circa 2000 and 2015" Systems 13, no. 7: 577. https://doi.org/10.3390/systems13070577
APA StyleHomer, J. (2025). Beyond the Preston Curve: Analyzing Variations in Life Expectancy Around the World Using Multivariate Regression Circa 2000 and 2015. Systems, 13(7), 577. https://doi.org/10.3390/systems13070577






