eHealth Literacy, Attitudes, and Willingness to Use an Artificial Intelligence-Assisted Wearable OTC-EHR System for Self-Medication: An Empirical Study Exploring AI Interventions
Abstract
1. Introduction
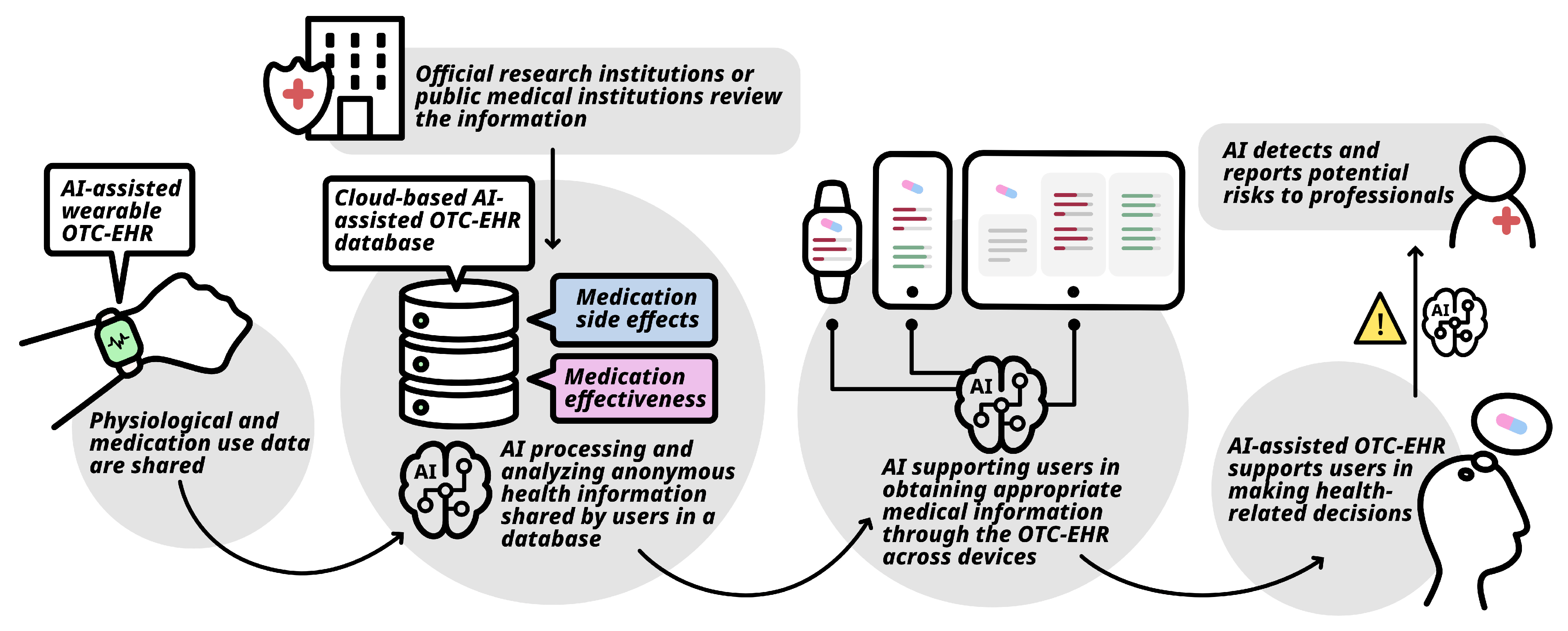
1.1. Application of OTC-EHR in Wearable Devices
1.2. The Definition of Wearable Devices and Potential Advantages in Health Management
1.3. Self-Medication, eHealth Literacy, and Interventions with Artificial Intelligence
1.4. Application of AI-Assisted Wearable-Device-Based OTC-EHRs
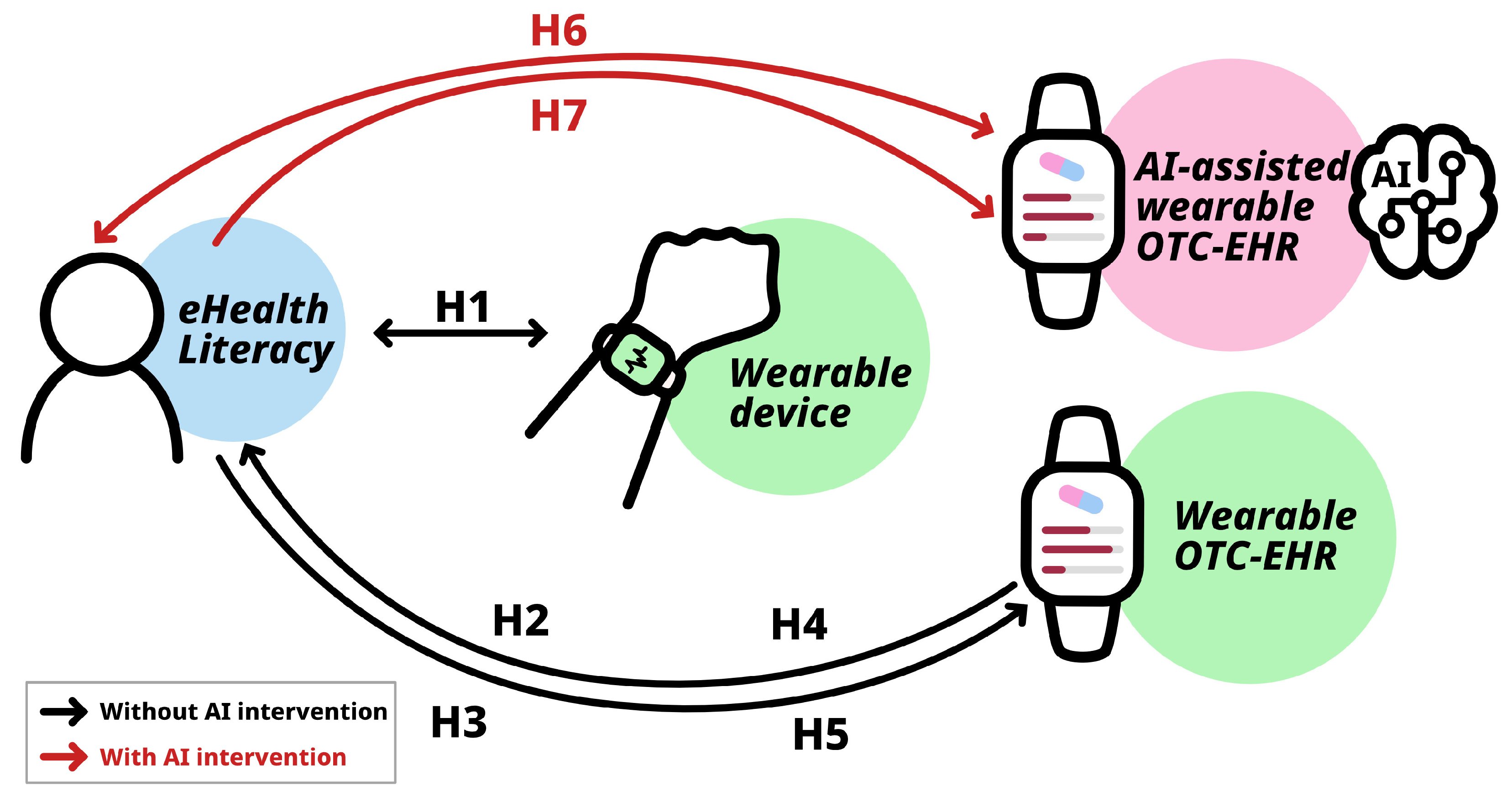
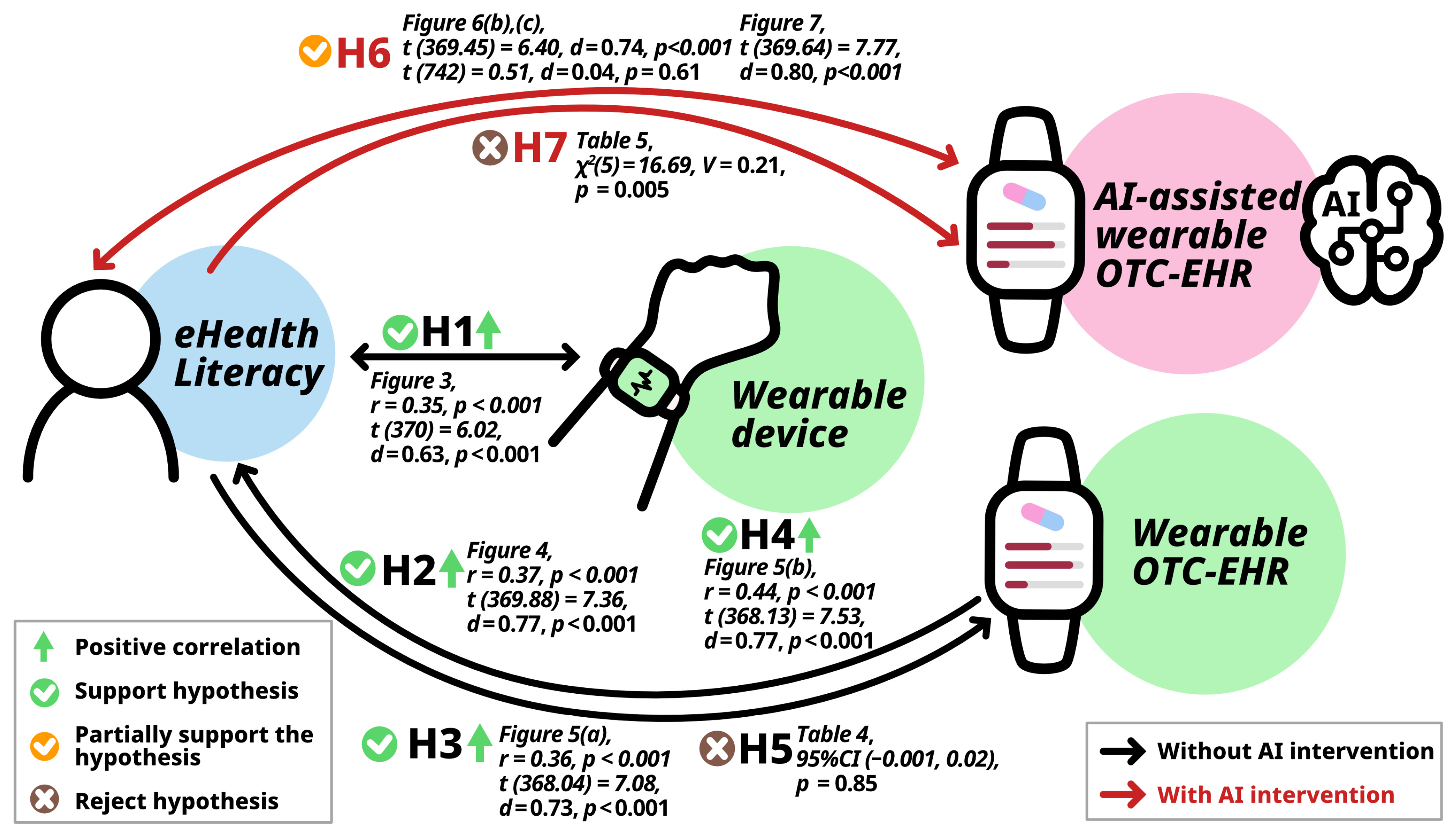
1.5. Research Hypotheses
2. Materials and Methods
2.1. Participants and Sample Size
2.2. Measures
2.2.1. Participant Characteristics
2.2.2. Usage of Wearable Devices
2.2.3. Attitudes Toward Utilizing Wearable OTC-EHR
2.2.4. Attitudes Toward AI Intervention for Wearable OTC-EHR
2.3. Statistical Analyses
3. Results
3.1. Characteristics of Participants
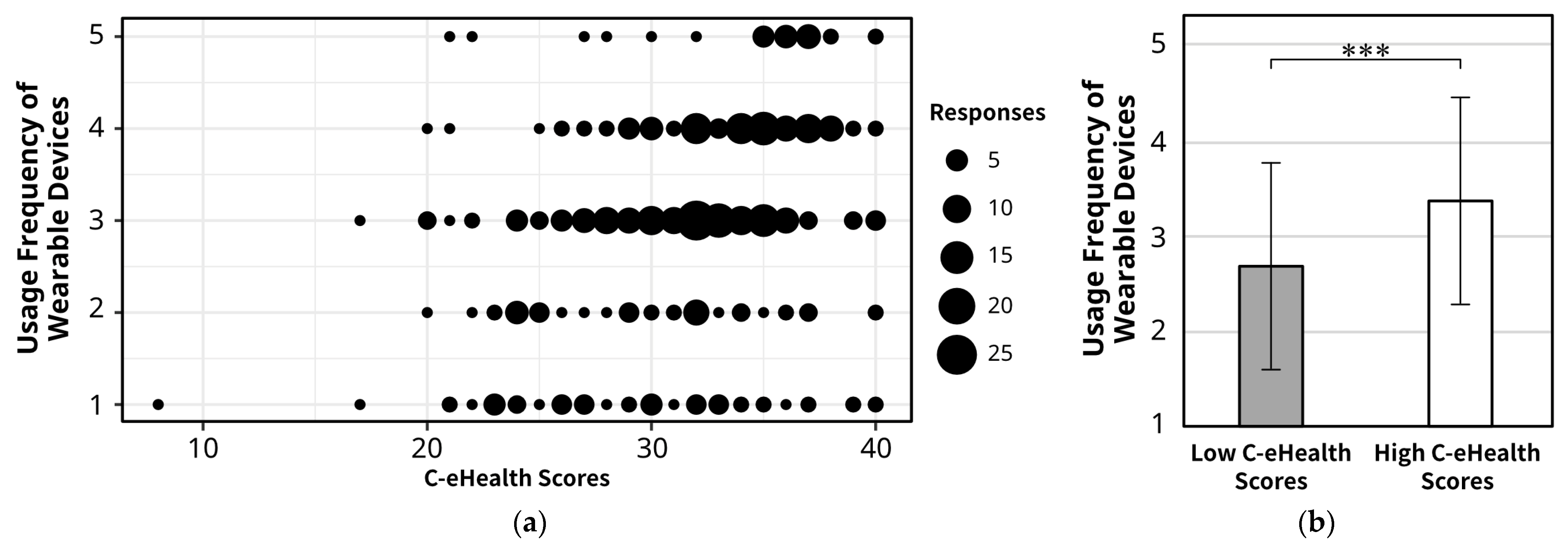
3.2. The Relationship Between eHealth Literacy and Wearable Device Usage
3.3. eHealth Literacy and Attitudes Toward Utilizing Wearable-Device-Based OTC-EHR
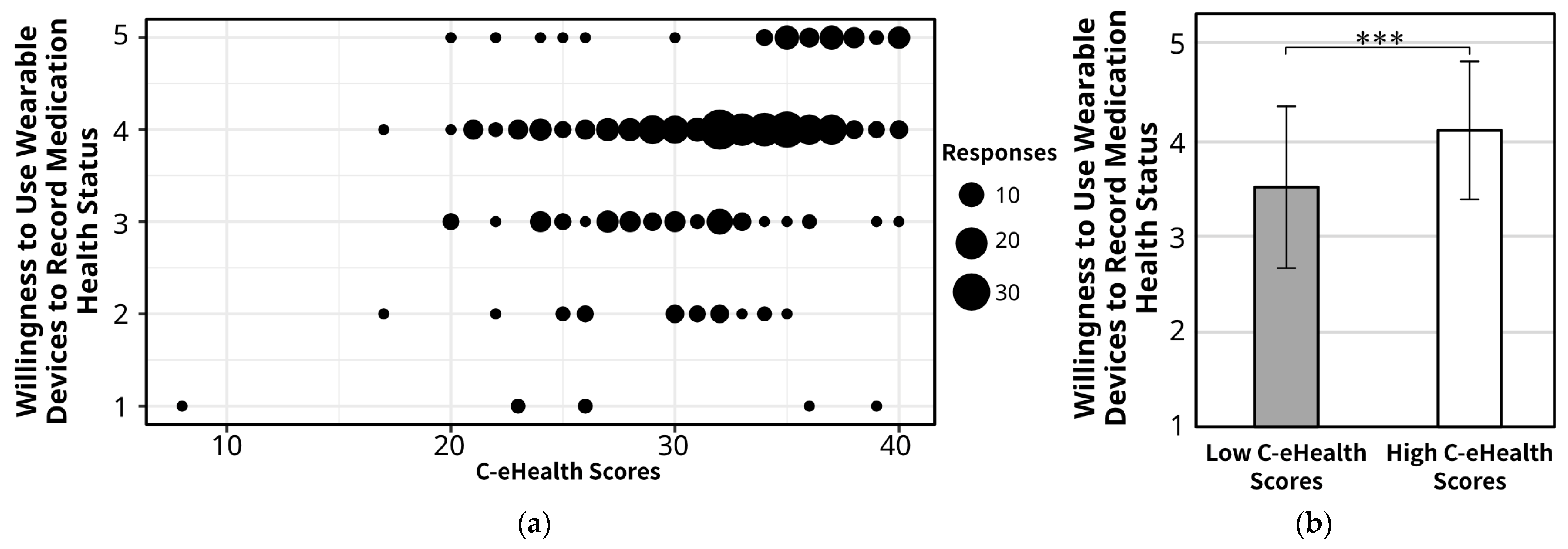
3.3.1. eHealth Literacy and Attitudes Toward Using Wearable-Device-Based OTC-EHR
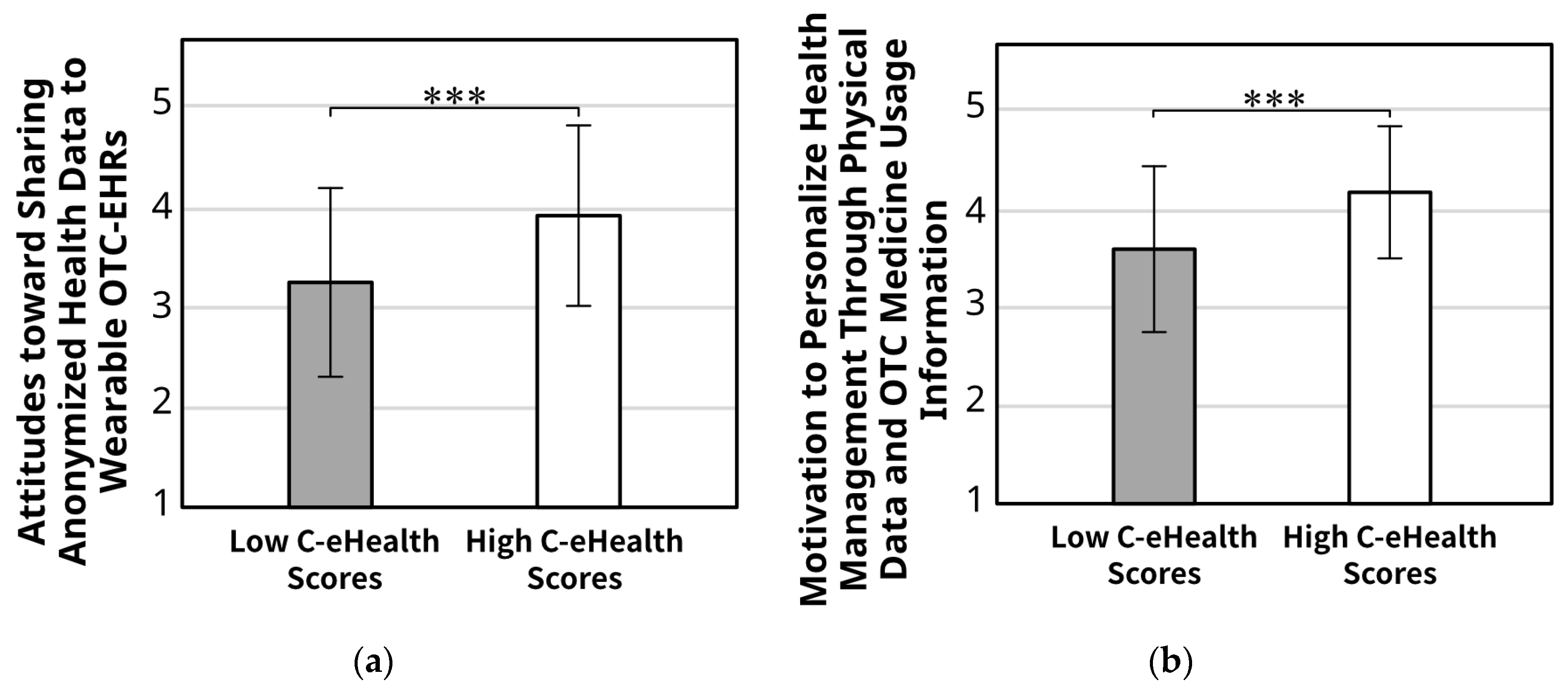
3.3.2. eHealth Literacy and Attitudes Toward Sharing Anonymized Health Data to Wearable-Device-Based OTC-EHR
3.3.3. eHealth Literacy and Motivation to Personalize Health Management Through Physiological Data and OTC Medicine Usage Information with Wearable-Device-Based OTC-EHRs
3.3.4. eHealth Literacy, Wearable Device Usage, Sharing Health Information, Motivation to Personalize Health Management Through Physiological Data, and Perceived Helpfulness of OTC-EHRs
3.4. Attitude Towards AI Intervention in Wearable-Device-Based OTC-EHRs Considering Ehealth Literacy
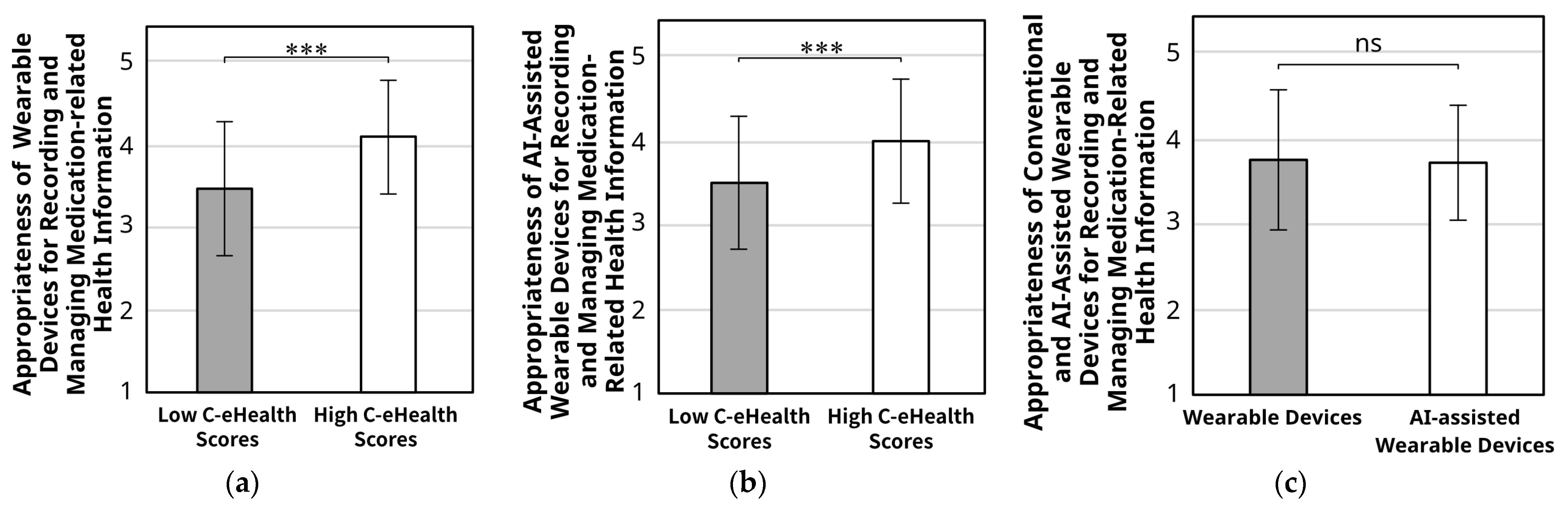
3.4.1. Whether Wearable Devices or AI-Assisted Wearable Devices Are Appropriate for Recording and Managing Medication-Related Health Information
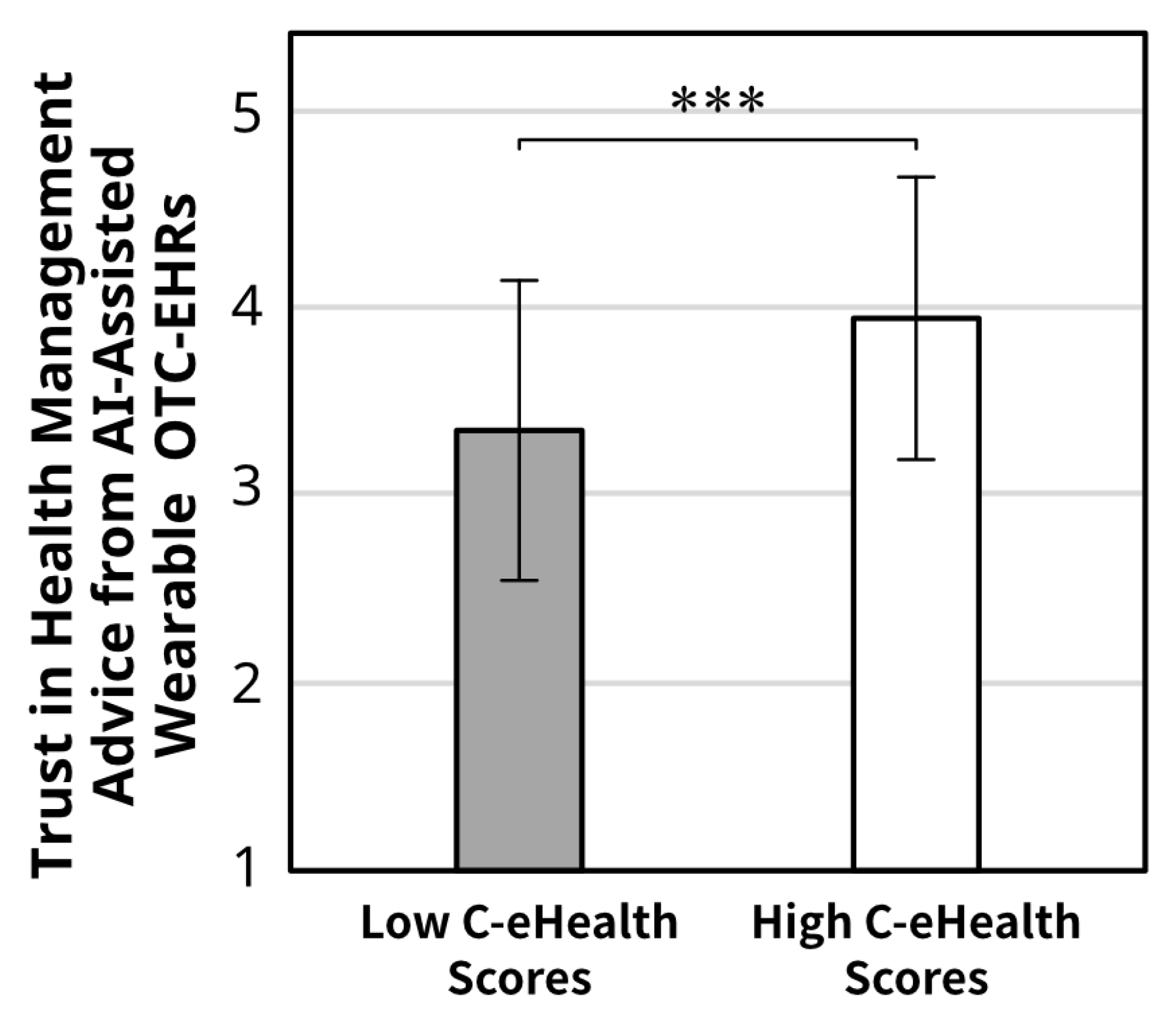
3.4.2. Trust in Health Management Advice from AI-Assisted Wearable OTC-EHRs
3.4.3. Attitudes Towards Approaches to Receiving Personalized Advice on Medication Decisions Considering AI Intervention
4. Discussion
4.1. eHealth Literacy and Wearable Device Use
4.2. Attitudes Toward Wearable OTC-EHRs
4.3. eHealth Literacy, Decision-Making, and AI Intervention
4.4. Contribution
4.5. Limitations and Future Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AI | Artificial Intelligence |
| OTC | Over-the-Counter |
| EHR | Electronic Health Record |
| OTC-EHR | Over-the-Counter Medication Electronic Health Record |
| HIT | Health Information Technology |
| FDA | Food and Drug Administration |
Appendix A
| Questions | Answer |
|---|---|
| I know what health resources are available on the Internet | “Strongly Disagree = 1” to “Strongly Agree = 5” |
| I know where to find helpful health resources on the Internet | |
| I know how to find helpful health resources on the Internet | |
| I know how to use the Internet to answer my questions about health | |
| I know how to use the health information I find on the Internet to help me | |
| I have the skills I need to evaluate the health resources I find on the Internet | |
| I can tell high quality health resources from low quality health resources on the Internet | |
| I feel confident in using information from the Internet to make health decisions |
References
- Tang, G.; Izumi, K.; Izumisawa, M.; Koyama, S. Japanese Consumers’ Attitudes towards Obtaining and Sharing Health Information Regarding Over-the-Counter Medication: Designing an Over-the-Counter Electronic Health Record. Healthcare 2023, 11, 1166. [Google Scholar] [CrossRef]
- Tang, G.; Chang, Y.; Izumisawa, M.; Koyama, S. Design an OTC Medicine Vending System Combined with OTC-EHR and Test it with Non-Experts and Experts Through a User-Centered Design Approach. J. Sci. Des. 2024, 8, 1_11–11_20. [Google Scholar] [CrossRef]
- Kebodeaux, C.D. Prescription and over-the-counter medication record integration: A holistic patient-centered approach. J. Am. Pharm. Assoc. 2019, 59, S13–S17. [Google Scholar] [CrossRef] [PubMed]
- Mackert, M.; Mabry-Flynn, A.; Champlin, S.; Donovan, E.E.; Pounders, K. Health Literacy and Health Information Technology Adoption: The Potential for a New Digital Divide. J. Med. Internet Res. 2016, 18, e264. [Google Scholar] [CrossRef]
- Kruse, C.S.; Stein, A.; Thomas, H.; Kaur, H. The use of Electronic Health Records to Support Population Health: A Systematic Review of the Literature. J. Med. Syst. 2018, 42, 214. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.; Jiang, S. Frequent and diverse use of electronic health records in the United States: A trend analysis of national surveys. Digit. Health 2022, 8, 20552076221112840. [Google Scholar] [CrossRef]
- Persell, S.D.; Eder, M.; Friesema, E.; Connor, C.; Rademaker, A.; French, D.D.; King, J.; Wolf, M.S. EHR-based medication support and nurse-led medication therapy management: Rationale and design for a three-arm clinic randomized trial. J. Am. Heart Assoc. 2013, 2, e000311. [Google Scholar] [CrossRef] [PubMed]
- Persell, S.D.; Karmali, K.N.; Lazar, D.; Friesema, E.M.; Lee, J.Y.; Rademaker, A.; Kaiser, D.; Eder, M.; French, D.D.; Brown, T.; et al. Effect of Electronic Health Record-Based Medication Support and Nurse-Led Medication Therapy Management on Hypertension and Medication Self-management: A Randomized Clinical Trial. JAMA Intern. Med. 2018, 178, 1069–1077. [Google Scholar] [CrossRef]
- Kang, H.; Jung, E.H. The smart wearables-privacy paradox: A cluster analysis of smartwatch users. Behav. Inf. Technol. 2020, 40, 1755–1768. [Google Scholar] [CrossRef]
- Bieber, G.; Kirste, T.; Urban, B. Ambient interaction by smart watches. In Proceedings of the 5th International Conference on Pervasive Technologies Related to Assistive Environments, Crete, Greece, 6–8 June 2012; pp. 1–6. [Google Scholar]
- Masoumian Hosseini, M.; Masoumian Hosseini, S.T.; Qayumi, K.; Hosseinzadeh, S.; Sajadi Tabar, S.S. Smartwatches in healthcare medicine: Assistance and monitoring; a scoping review. BMC Med. Inform. Decis. Mak. 2023, 23, 248. [Google Scholar] [CrossRef] [PubMed]
- Case, M.A.; Burwick, H.A.; Volpp, K.G.; Patel, M.S. Accuracy of Smartphone Applications and Wearable Devices for Tracking Physical Activity Data. JAMA 2015, 313, 625–626. [Google Scholar] [CrossRef]
- Manini, T.M.; Mendoza, T.; Battula, M.; Davoudi, A.; Kheirkhahan, M.; Young, M.E.; Weber, E.; Fillingim, R.B.; Rashidi, P. Perception of Older Adults Toward Smartwatch Technology for Assessing Pain and Related Patient-Reported Outcomes: Pilot Study. JMIR Mhealth Uhealth 2019, 7, e10044. [Google Scholar] [CrossRef] [PubMed]
- Ayatollahi, H.; Lodewyk, K.; Wiebe, M.; Dennett, L.; Larsson, J.; Greenshaw, A.; Hayward, J. Wearables research for continuous monitoring of patient outcomes: A scoping review. PLoS Digit. Health 2025, 4, e0000860. [Google Scholar] [CrossRef]
- Shandhi, M.M.H.; Singh, K.; Janson, N.; Ashar, P.; Singh, G.; Lu, B.; Hillygus, D.S.; Maddocks, J.M.; Dunn, J.P. Assessment of ownership of smart devices and the acceptability of digital health data sharing. NPJ Digit. Med. 2024, 7, 44. [Google Scholar] [CrossRef]
- Prieto-Avalos, G.; Cruz-Ramos, N.A.; Alor-Hernandez, G.; Sanchez-Cervantes, J.L.; Rodriguez-Mazahua, L.; Guarneros-Nolasco, L.R. Wearable Devices for Physical Monitoring of Heart: A Review. Biosensors 2022, 12, 292. [Google Scholar] [CrossRef] [PubMed]
- King, C.E.; Sarrafzadeh, M. A Survey of Smartwatches in Remote Health Monitoring. J. Healthc. Inform. Res. 2018, 2, 1–24. [Google Scholar] [CrossRef]
- Lu, T.C.; Fu, C.M.; Ma, M.H.; Fang, C.C.; Turner, A.M. Healthcare Applications of Smart Watches. A Systematic Review. Appl. Clin. Inform. 2016, 7, 850–869. [Google Scholar] [CrossRef]
- Piwek, L.; Ellis, D.A.; Andrews, S.; Joinson, A. The Rise of Consumer Health Wearables: Promises and Barriers. PLoS Med. 2016, 13, e1001953. [Google Scholar] [CrossRef]
- Reeder, B.; David, A. Health at hand: A systematic review of smart watch uses for health and wellness. J. Biomed. Inform. 2016, 63, 269–276. [Google Scholar] [CrossRef]
- Dunn, J.; Kidzinski, L.; Runge, R.; Witt, D.; Hicks, J.L.; Schussler-Fiorenza Rose, S.M.; Li, X.; Bahmani, A.; Delp, S.L.; Hastie, T.; et al. Wearable sensors enable personalized predictions of clinical laboratory measurements. Nat. Med. 2021, 27, 1105–1112. [Google Scholar] [CrossRef]
- Isakadze, N.; Martin, S.S. How useful is the smartwatch ECG? Trends Cardiovasc. Med. 2020, 30, 442–448. [Google Scholar] [CrossRef]
- Al-Maroof, R.S.; Alhumaid, K.; Alhamad, A.Q.; Aburayya, A.; Salloum, S. User Acceptance of Smart Watch for Medical Purposes: An Empirical Study. Future Internet 2021, 13, 127. [Google Scholar] [CrossRef]
- Li, X.; Dunn, J.; Salins, D.; Zhou, G.; Zhou, W.; Schussler-Fiorenza Rose, S.M.; Perelman, D.; Colbert, E.; Runge, R.; Rego, S.; et al. Digital Health: Tracking Physiomes and Activity Using Wearable Biosensors Reveals Useful Health-Related Information. PLoS Biol. 2017, 15, e2001402. [Google Scholar] [CrossRef]
- Onorati, F.; Regalia, G.; Caborni, C.; Migliorini, M.; Bender, D.; Poh, M.Z.; Frazier, C.; Kovitch Thropp, E.; Mynatt, E.D.; Bidwell, J.; et al. Multicenter clinical assessment of improved wearable multimodal convulsive seizure detectors. Epilepsia 2017, 58, 1870–1879. [Google Scholar] [CrossRef]
- Niela-Vilen, H.; Auxier, J.; Ekholm, E.; Sarhaddi, F.; Asgari Mehrabadi, M.; Mahmoudzadeh, A.; Azimi, I.; Liljeberg, P.; Rahmani, A.M.; Axelin, A. Pregnant women’s daily patterns of well-being before and during the COVID-19 pandemic in Finland: Longitudinal monitoring through smartwatch technology. PLoS ONE 2021, 16, e0246494. [Google Scholar] [CrossRef] [PubMed]
- Hunter, A.; Leckie, T.; Coe, O.; Hardy, B.; Fitzpatrick, D.; Goncalves, A.C.; Standing, M.K.; Koulouglioti, C.; Richardson, A.; Hodgson, L. Using Smartwatches to Observe Changes in Activity During Recovery from Critical Illness Following COVID-19 Critical Care Admission: 1-Year, Multicenter Observational Study. JMIR Rehabil. Assist. Technol. 2022, 9, e25494. [Google Scholar] [CrossRef] [PubMed]
- Auepanwiriyakul, C.; Waibel, S.; Songa, J.; Bentley, P.; Faisal, A.A. Accuracy and Acceptability of Wearable Motion Tracking for Inpatient Monitoring Using Smartwatches. Sensors 2020, 20, 7313. [Google Scholar] [CrossRef]
- Bajaj, R.K.; Meiring, R.M.; Beltran, F. Co-Design, Development, and Evaluation of a Health Monitoring Tool Using Smartwatch Data: A Proof-of-Concept Study. Future Internet 2023, 15, 111. [Google Scholar] [CrossRef]
- Aoyama, I.; Koyama, S.; Hibino, H. Self-medication behaviors among Japanese consumers: Sex, age, and SES differences and caregivers’ attitudes toward their children’s health management. Asia Pac. Fam. Med. 2012, 11, 7. [Google Scholar] [CrossRef]
- Chewning, B.; Sleath, B. Medication decision-making and management: A client-centered model. Soc. Sci. Med. 1996, 42, 389–398. [Google Scholar] [CrossRef]
- Ray, I.; Bardhan, M.; Hasan, M.M.; Sahito, A.M.; Khan, E.; Patel, S.; Jani, I.; Bhatt, P.K.; Sp, R.; Swed, S. Over the counter drugs and self-medication: A worldwide paranoia and a troublesome situation in India during the COVID-19 pandemic. Ann. Med. Surg. 2022, 78, 103797. [Google Scholar] [CrossRef]
- Makowska, M.; Boguszewki, R.; Nowakowski, M.; Podkowinska, M. Self-medication-related behaviors and poland’s COVID-19 lockdown. Int. J. Environ. Res. Public Health 2020, 17, 8344. [Google Scholar] [CrossRef]
- Masoumian Hosseini, M.; Masoumian Hosseini, S.T.; Qayumi, K.; Ahmady, S.; Koohestani, H.R. The Aspects of Running Artificial Intelligence in Emergency Care; a Scoping Review. Arch. Acad. Emerg. Med. 2023, 11, e38. [Google Scholar] [CrossRef] [PubMed]
- Norman, C.D.; Skinner, H.A. eHealth Literacy: Essential skills for consumer health in a networked world. J. Med. Internet Res. 2006, 8, e9. [Google Scholar] [CrossRef] [PubMed]
- Yáñez, J.A.; Chung, S.A.; Román, B.R.; Hernández-Yépez, P.J.; Garcia-Solorzano, F.O.; Del-Aguila-Arcentales, S.; Inga-Berrospi, F.; Mejia, C.R.; Alvarez-Risco, A. Prescription, over-the-counter (OTC), herbal, and other treatments and preventive uses for COVID-19. In Environmental and Health Management of Novel Coronavirus Disease (COVID-19); Academic Press: Cambridge, MA, USA, 2021; pp. 379–416. [Google Scholar]
- Tang, G.; Izumi, K.; Izumisawa, M.; Koyama, S. Analysis of Japanese consumers’ attitudes toward the digital transformation of OTC medicine purchase behavior and eHealth literacy: An online survey for digital experience design. Front. Digit. Health 2023, 5, 1173229. [Google Scholar] [CrossRef]
- Mitsutake, S.; Shibata, A.; Ishii, K.; Oka, K. Associations of eHealth literacy with health behavior among adult Internet users. J. Med. Internet Res. 2016, 18, e192. [Google Scholar] [CrossRef]
- Busse, T.S.; Nitsche, J.; Kernebeck, S.; Jux, C.; Weitz, J.; Ehlers, J.P.; Bork, U. Approaches to improvement of digital health literacy (eHL) in the context of person-centered care. Int. J. Environ. Res. Public Health 2022, 19, 8309. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Lee, E.H.; Chae, D. eHealth Literacy Instruments: Systematic Review of Measurement Properties. J. Med. Internet Res. 2021, 23, e30644. [Google Scholar] [CrossRef]
- Okumu, M.; Logie, C.H.; Byansi, W.; Cohen, F.; Nyoni, T.; Nafula, C.N.; Hakiza, R.; Muzei, J.; Appiah-Kubi, J.; Adjabeng, B.; et al. eHealth literacy and digital health interventions: Key ingredients for supporting the mental health of displaced youth living in the urban slums of kampala, Uganda. Comput. Hum. Behav. 2025, 162, 108434. [Google Scholar] [CrossRef]
- Muller, S. Is there a civic duty to support medical AI development by sharing electronic health records? BMC Med. Ethics 2022, 23, 134. [Google Scholar] [CrossRef]
- Giordano, C.; Brennan, M.; Mohamed, B.; Rashidi, P.; Modave, F.; Tighe, P. Accessing Artificial Intelligence for Clinical Decision-Making. Front. Digit. Health 2021, 3, 645232. [Google Scholar] [CrossRef]
- Wong, J.; Horwitz, M.M.; Zhou, L.; Toh, S. Using machine learning to identify health outcomes from electronic health record data. Curr. Epidemiol. Rep. 2018, 5, 331–342. [Google Scholar] [CrossRef]
- Sheu, Y.H.; Magdamo, C.; Miller, M.; Das, S.; Blacker, D.; Smoller, J.W. AI-assisted prediction of differential response to antidepressant classes using electronic health records. NPJ Digit. Med. 2023, 6, 73. [Google Scholar] [CrossRef]
- Lauritsen, S.M.; Kristensen, M.; Olsen, M.V.; Larsen, M.S.; Lauritsen, K.M.; Jorgensen, M.J.; Lange, J.; Thiesson, B. Explainable artificial intelligence model to predict acute critical illness from electronic health records. Nat. Commun. 2020, 11, 3852. [Google Scholar] [CrossRef]
- Free, C.; Phillips, G.; Felix, L.; Galli, L.; Patel, V.; Edwards, P. The effectiveness of M-health technologies for improving health and health services: A systematic review protocol. BMC Res. Notes 2010, 3, 250. [Google Scholar] [CrossRef]
- Fraley, R.C.; Marks, M.J. The null hypothesis significance testing debate and its implications for personality research. In Handbook of Research Methods in Personality Psychology; The Guilford Press: New York, NY, USA, 2007; pp. 149–169. [Google Scholar]
- Richard, F.D.; Bond, C.F.; Stokes-Zoota, J.J. One hundred years of social psychology quantitatively described. Rev. Gen. Psychol. 2003, 7, 331–363. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Gignac, G.E.; Szodorai, E.T. Effect size guidelines for individual differences researchers. Personal. Individ. Differ. 2016, 102, 74–78. [Google Scholar] [CrossRef]
- Funder, D.C.; Ozer, D.J. Evaluating Effect Size in Psychological Research: Sense and Nonsense. Adv. Methods Pract. Psychol. Sci. 2019, 2, 156–168. [Google Scholar] [CrossRef]
- Long, C.; Zheng, L.; Liu, R.; Duan, Z. Structural Validation and Measurement Invariance Testing of the Chinese Version of the eHealth Literacy Scale Among Undergraduates: Cross-Sectional Study. J. Med. Internet Res. 2023, 25, e48838. [Google Scholar] [CrossRef]
- Norman, C.D.; Skinner, H.A. eHEALS: The eHealth Literacy Scale. J. Med. Internet Res. 2006, 8, e27. [Google Scholar] [CrossRef] [PubMed]
- Salloum, S.A.; Al-Emran, M.; Shaalan, K.; Tarhini, A. Factors affecting the E-learning acceptance: A case study from UAE. Educ. Inf. Technol. 2018, 24, 509–530. [Google Scholar] [CrossRef]
- Xu, R.H.; Shi, L.S.; Xia, Y.; Wang, D. Associations among eHealth literacy, social support, individual resilience, and emotional status in primary care providers during the outbreak of the SARS-CoV-2 Delta variant. Digit. Health 2022, 8, 20552076221089789. [Google Scholar] [CrossRef]
- Park, H.; Moon, M.; Baeg, J.H. Association of eHealth literacy with cancer information seeking and prior experience with cancer screening. Comput. Inform. Nurs. 2014, 32, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Neter, E.; Brainin, E. eHealth literacy: Extending the digital divide to the realm of health information. J. Med. Internet Res. 2012, 14, e19. [Google Scholar] [CrossRef]
- Tennant, B.; Stellefson, M.; Dodd, V.; Chaney, B.; Chaney, D.; Paige, S.; Alber, J. eHealth literacy and Web 2.0 health information seeking behaviors among baby boomers and older adults. J. Med. Internet Res. 2015, 17, e70. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: Oxfordshire, UK, 1988. [Google Scholar]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef]
- Cramér, H. Mathematical Methods of Statistics; Princeton University Press: Princeton, NJ, USA, 1946. [Google Scholar]
- Shiu, L.S.; Liu, C.Y.; Lin, C.J.; Chen, Y.C. What are the roles of eHealth literacy and empowerment in self-management in an eHealth care context? A cross-sectional study. J. Clin. Nurs. 2023, 32, 8043–8053. [Google Scholar] [CrossRef]
- Juhn, Y.; Liu, H. Artificial intelligence approaches using natural language processing to advance EHR-based clinical research. J. Allergy Clin. Immunol. 2020, 145, 463–469. [Google Scholar] [CrossRef]
- Yang, X.; Chen, A.; PourNejatian, N.; Shin, H.C.; Smith, K.E.; Parisien, C.; Compas, C.; Martin, C.; Costa, A.B.; Flores, M.G.; et al. A large language model for electronic health records. NPJ Digit. Med. 2022, 5, 194. [Google Scholar] [CrossRef]
- Olsen, Q.; Dyda, A.; Woods, L.; Lobo, E.; Eden, R.; Krahe, M.A.; Richards, B.; Pather, N.; McGee, L.; Sullivan, C.; et al. Worldwide willingness to share health data high but privacy, consent and transparency paramount, a meta-analysis. NPJ Digit. Med. 2025, 8, 540. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.D.; See, K.A. Trust in automation: Designing for appropriate reliance. Hum. Factors 2004, 46, 50–80. [Google Scholar] [CrossRef]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User acceptance of computer technology: A comparison of two theoretical models. Manag. Sci. 1989, 35, 982–1003. [Google Scholar] [CrossRef]
- Elkhaili El Alami, L.S.; Nemoto, A.; Nakata, Y. General patients’ expectations on online accessibility to their electronic health records in Japan. Glob. Health Med. 2020, 2, 168–173. [Google Scholar] [CrossRef]
- Takahashi, Y.; Ohura, T.; Ishizaki, T.; Okamoto, S.; Miki, K.; Naito, M.; Akamatsu, R.; Sugimori, H.; Yoshiike, N.; Miyaki, K.; et al. Internet use for health-related information via personal computers and cell phones in Japan: A cross-sectional population-based survey. J. Med. Internet Res. 2011, 13, e110. [Google Scholar] [CrossRef]
- Bansal, G.; Zahedi, F.M.; Gefen, D. The impact of personal dispositions on information sensitivity, privacy concern and trust in disclosing health information online. Decis. Support. Syst. 2010, 49, 138–150. [Google Scholar] [CrossRef]
- Hoogland, A.I.; Mansfield, J.; Lafranchise, E.A.; Bulls, H.W.; Johnstone, P.A.; Jim, H.S.L. eHealth literacy in older adults with cancer. J. Geriatr. Oncol. 2020, 11, 1020–1022. [Google Scholar] [CrossRef] [PubMed]
- Neter, E.; Brainin, E. Perceived and Performed eHealth Literacy: Survey and Simulated Performance Test. JMIR Hum. Factors 2017, 4, e2. [Google Scholar] [CrossRef]
- Kohn, S.C.; de Visser, E.J.; Wiese, E.; Lee, Y.C.; Shaw, T.H. Measurement of Trust in Automation: A Narrative Review and Reference Guide. Front. Psychol. 2021, 12, 604977. [Google Scholar] [CrossRef] [PubMed]
| (i) Attitude towards using wearable devices to record health status |
| Question: Are you willing to use the wearable devices to record your health status during medication use? The responses ranged from “Completely Unwilling = 0” to “Very Willing = 5.” |
| (ii) Attitude towards sharing health data |
| Question: If the health information recorded by wearable devices during your medication use is anonymized and protected, are you willing to share this information? The responses ranged from “Completely Unwilling = 1” to “Very Willing = 5.” |
| (iii) Motivation to personalize health management through physiological data and OTC medicines usage information |
| Question: Are you willing to use physiological data recorded by wearable devices, combined with health information during OTC medicines use, to personalize your health management? The responses ranged from “Completely Unwilling = 1” to “Very Willing = 5.” |
| (iv) Perceived helpfulness from the wearable device-based OTC-EHR |
| Question: If you can check anonymized health information shared by other patients when purchasing OTC medicines, do you think this information could help you choose the appropriate medicines? The responses ranged from “Not Helpful at All = 1” to “Very Helpful = 5.” |
| (i) Regarding whether wearable devices or Ai-based wearable devices are appropriate for recording and managing medication-related health information |
| Question: Do you consider wearable devices to be appropriate digital tools for recording and managing health information related to medication use? The responses ranged from “Absolutely Not = 1” to “Absolutely Yes = 5.” |
| Question: Do you consider wearable devices combined with AI interventions to be an appropriate tool for recording and managing health information related to medication use? The responses ranged from “Absolutely Not = 1” to “Absolutely Yes = 5.” |
| (ii) Trust in Health Management Advice from AI-assisted wearable OTC-EHR |
| Question: Do you trust AI to analyze the health information related to medication use recorded and managed through wearable devices to provide you with medication advice? The responses ranged from “Absolutely Not = 1” to “Absolutely Yes = 5.” |
| (iii) Attitude towards approaches to get personalized advice regarding OTC medicines usage and medication decisions |
| Question: Which approach do you prefer for obtaining personalized OTC medication advice? Options: (A) I prefer to review medication information and make decisions on my own. (B) I prefer to review medication information, consider suggestions provided by AI, and then make my own decisions. (C) I prefer to review medication information myself and rely on AI to make decisions. (D) I prefer AI to make all decisions for me. (E) I prefer to review medication information myself and rely on doctors or pharmacists to make decisions. (H) I prefer doctors or pharmacists to make all decisions for me. |
| Characteristics | Respondents N (%) | C-eHealth Scores (Mean ± SD) |
|---|---|---|
| Age brackets (years) | ||
| 18–29 | 135 (36.29%) | 31.46 ± 5.36 |
| 30–39 | 199 (53.50%) | 31.88 ± 4.45 |
| 40–49 | 30 (8.06%) | 31.07 ± 5.71 |
| Over 50 | 8 (2.15%) | 29.50 ± 5.95 |
| Gender | ||
| Female | 136 (36.56%) | 31.86 ± 5.47 |
| Male | 235 (63.17%) | 31.44 ± 4.60 |
| Others | 1 (0.27%) | 37.00 ± 0.00 |
| Occupation | ||
| Medical practitioner | 31 (8.33%) | 34.10 ± 5.74 |
| Non-medical practitioner | 341 (91.67%) | 31.38 ± 4.80 |
| Total | 372 (100.00%) | 31.61± 4.93 |
| Effects | Estimate | SE | 95% CI | p | |
|---|---|---|---|---|---|
| LL | UL | ||||
| Fixed effects | |||||
| Intercept | 1.11 | 0.24 | 0.64 | 1.59 | <0.001 |
| eHealth literacy | 0.00 | 0.01 | −0.01 | 0.02 | 0.85 |
| Attitude towards using wearable-device-based OTC-EHRs | 0.25 | 0.06 | 0.14 | 0.37 | <0.001 |
| Attitude towards sharing health information to wearable-device-based OTC-EHRs | 0.25 | 0.05 | 0.16 | 0.34 | <0.001 |
| Motivation to personalize health management through physiological data | 0.19 | 0.06 | 0.07 | 0.31 | 0.001 |
| Question: Which Approach Do You Prefer to Obtain Personalized OTC Medication Advice? | ||||||
| Respondents % (N) | I prefer to review medication information and make decisions on my own | I prefer to review medication information, consider suggestions provided by AI, and then make my own decisions | I prefer to review medication information myself and rely on AI to make decisions | I prefer AI to make all decisions for me | I prefer to review medication information myself and rely on doctors or pharmacists to make decisions | I prefer doctors or pharmacists to make all decisions for me |
| High C-eHealth | 34 (19.54%) | 55 (31.61%) | 14 (8.05%) | 42 (24.14%) | 13 (7.47%) | 16 (9.20%) |
| Low C-eHealth | 21 (10.61%) | 62 (31.31%) | 5 (2.53%) | 63 (31.82%) | 29 (14.65%) | 18 (9.09%) |
| Total | 55 (14.78%) | 117 (31.45%) | 19 (5.11%) | 105 (28.23%) | 42 (11.29%) | 34 (9.14%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tang, G.; Xu, Z.; Koyama, S. eHealth Literacy, Attitudes, and Willingness to Use an Artificial Intelligence-Assisted Wearable OTC-EHR System for Self-Medication: An Empirical Study Exploring AI Interventions. Systems 2025, 13, 1070. https://doi.org/10.3390/systems13121070
Tang G, Xu Z, Koyama S. eHealth Literacy, Attitudes, and Willingness to Use an Artificial Intelligence-Assisted Wearable OTC-EHR System for Self-Medication: An Empirical Study Exploring AI Interventions. Systems. 2025; 13(12):1070. https://doi.org/10.3390/systems13121070
Chicago/Turabian StyleTang, Guyue, Zhidiankui Xu, and Shinichi Koyama. 2025. "eHealth Literacy, Attitudes, and Willingness to Use an Artificial Intelligence-Assisted Wearable OTC-EHR System for Self-Medication: An Empirical Study Exploring AI Interventions" Systems 13, no. 12: 1070. https://doi.org/10.3390/systems13121070
APA StyleTang, G., Xu, Z., & Koyama, S. (2025). eHealth Literacy, Attitudes, and Willingness to Use an Artificial Intelligence-Assisted Wearable OTC-EHR System for Self-Medication: An Empirical Study Exploring AI Interventions. Systems, 13(12), 1070. https://doi.org/10.3390/systems13121070







