Basophils and Systemic Lupus Erythematosus in Murine Models and Human Patients
Simple Summary
Abstract
1. Introduction
1.1. General Characteristics and Ontogenesis of Basophils
1.2. Basophil Activation
1.3. Immunomodulatory Properties of Basophils
1.4. General Concepts on SLE Immunopathogenesis
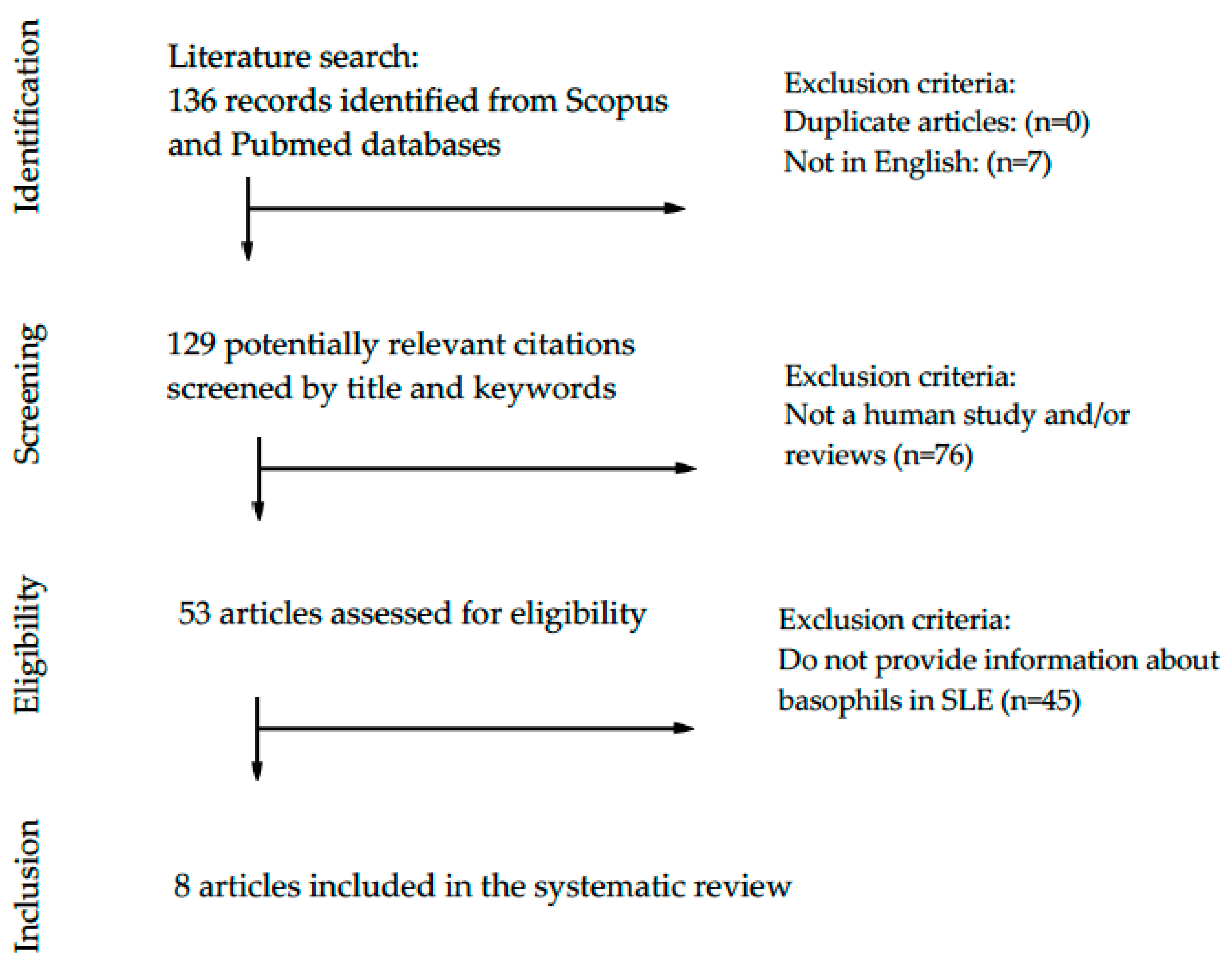
2. Materials and Methods
3. Results
3.1. Basophils and Lupus in Murine Models
3.2. Basophils and Systemic Lupus Erythematosus in Human Studies
4. Discussion
4.1. Basophils and SLE in Murine Experimental Models
4.2. Basophils and SLE in Human Patients
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Salinas, G.F.; Braza, F.; Brouard, S.; Tak, P.-P.; Baeten, D. The role of B lymphocytes in the progression from autoimmunity to autoimmune disease. Clin. Immunol. 2013, 146, 34–45. [Google Scholar] [CrossRef] [PubMed]
- Yurasov, S.; Wardemann, H.; Hammersen, J.; Tsuiji, M.; Meffre, E.; Pascual, V.; Nussenzweig, M.C. Defective B cell tolerance checkpoints in systemic lupus erythematosus. J. Exp. Med. 2005, 201, 703–711. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wang, F.-S.; Gershwin, M.E. Human autoimmune diseases: A comprehensive update. J. Intern. Med. 2015, 278, 369–395. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.H.; Gregersen, P.K. Genomics and the Multifactorial Nature of Human Autoimmune Disease. N. Engl. J. Med. 2011, 365, 1612–1623. [Google Scholar] [CrossRef] [PubMed]
- Manolio, T.A.; Collins, F.S.; Cox, N.J.; Goldstein, D.B.; Hindorff, L.A.; Hunter, D.J.; McCarthy, M.I.; Ramos, E.M.; Cardon, L.R.; Chakravarti, A.; et al. Finding the missing heritability of complex diseases. Nature 2009, 461, 747–753. [Google Scholar] [CrossRef]
- Zhao, Z.; Ren, J.; Dai, C.; Kannapell, C.C.; Wang, H.; Gaskin, F.; Fu, S.M. Nature of T cell epitopes in lupus antigens and HLA-DR determines autoantibody initiation and diversification. Ann. Rheum. Dis. 2019, 78, 380–390. [Google Scholar] [CrossRef]
- Gulati, G.; Brunner, H.I. Environmental triggers in systemic lupus erythematosus. Semin. Arthritis Rheum. 2018, 47, 710–717. [Google Scholar] [CrossRef]
- Lu, R.; Munroe, M.E.; Guthridge, J.M.; Bean, K.M.; Fife, D.A.; Chen, H.; Slight-Webb, S.R.; Keith, M.P.; Harley, J.B.; James, J.A. Dysregulation of innate and adaptive serum mediators precedes systemic lupus erythematosus classification and improves prognostic accuracy of autoantibodies. J. Autoimmun. 2016, 74, 182–193. [Google Scholar] [CrossRef]
- Bentham, J.; Morris, D.L.; Graham, D.S.C.; Pinder, C.L.; Tombleson, P.; Behrens, T.W.; Martín, J.; Fairfax, B.P.; Knight, J.C.; Chen, L.; et al. Genetic association analyses implicate aberrant regulation of innate and adaptive immunity genes in the pathogenesis of systemic lupus erythematosus. Nat. Genet. 2015, 47, 1457–1464. [Google Scholar] [CrossRef]
- Ducrest, S.; Meier, F.; Tschopp, C.; Pavlovic, R.; Dahinden, C.A. Flowcytometric analysis of basophil counts in human blood and inaccuracy of hematology analyzers. Allergy 2005, 60, 1446–1450. [Google Scholar] [CrossRef]
- Falcone, F.H.; Haas, H.; Gibbs, B.F. The human basophil: A new appreciation of its role in immune responses. Blood 2000, 96, 4028–4038. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, A.; Nakajima, S.; Kubo, M.; Egawa, G.; Honda, T.; Kitoh, A.; Nomura, T.; Hanakawa, S.; Sagita Moniaga, C.; Kim, B.; et al. Basophils are required for the induction of Th2 immunity to haptens and peptide antigens. Nat. Commun. 2013, 4. [Google Scholar] [CrossRef]
- Yoshimoto, T.; Yasuda, K.; Tanaka, H.; Nakahira, M.; Imai, Y.; Fujimori, Y.; Nakanishi, K. Basophils contribute to TH2-IgE responses in vivo via IL-4 production and presentation of peptide–MHC class II complexes to CD4+ T cells. Nat. Immunol. 2009, 10, 706–712. [Google Scholar] [CrossRef] [PubMed]
- Arinobu, Y.; Iwasaki, H.; Gurish, M.F.; Mizuno, S.; Shigematsu, H.; Ozawa, H.; Tenen, D.G.; Austen, K.F.; Akashi, K. Developmental checkpoints of the basophil/mast cell lineages in adult murine hematopoiesis. Proc. Natl. Acad. Sci. USA 2005, 102, 18105–18110. [Google Scholar] [CrossRef] [PubMed]
- Shen, T.; Kim, S.; Do, J.; Wang, L.; Lantz, C.; Urban, J.F.; Le Gros, G.; Min, B. T cell-derived IL-3 plays key role in parasite infection-induced basophil production but is dispensable for in vivo basophil survival. Int. Immunol. 2008, 20, 1201–1209. [Google Scholar] [CrossRef]
- Schroeder, J.T.; Chichester, K.L.; Bieneman, A.P. Human Basophils Secrete IL-3: Evidence of Autocrine Priming for Phenotypic and Functional Responses in Allergic Disease. J. Immunol. 2009, 182, 2432–2438. [Google Scholar] [CrossRef]
- Salter, B.M.; Oliveria, J.P.; Nusca, G.; Smith, S.G.; Tworek, D.; Mitchell, P.D.; Watson, R.M.; Sehmi, R.; Gauvreau, G.M. IL-25 and IL-33 induce Type 2 inflammation in basophils from subjects with allergic asthma. Respir. Res. 2016, 17, 5. [Google Scholar] [CrossRef]
- Hill, D.A.; Siracusa, M.C.; Abt, M.C.; Kim, B.S.; Kobuley, D.; Kubo, M.; Kambayashi, T.; LaRosa, D.F.; Renner, E.D.; Orange, J.S.; et al. Commensal bacterial–derived signals regulate basophil hematopoiesis and allergic inflammation. Nat. Med. 2012, 18, 538–546. [Google Scholar] [CrossRef]
- Reese, T.A.; Liang, H.-E.; Tager, A.M.; Luster, A.D.; Van Rooijen, N.; Voehringer, D.; Locksley, R.M. Chitin Induces Tissue Accumulation of Innate Immune Cells Associated with Allergy. Nature 2007, 447, 92–96. [Google Scholar] [CrossRef]
- Garman, S.C.; Wurzburg, B.A.; Tarchevskaya, S.S.; Kinet, J.-P.; Jardetzky, T.S. Structure of the Fc fragment of human IgE bound to its high-affinity receptor FceRIa. Nature 2000, 406, 259–266. [Google Scholar] [CrossRef]
- Hellman, L.T.; Akula, S.; Thorpe, M.; Fu, Z. Tracing the Origins of IgE, Mast Cells, and Allergies by Studies of Wild Animals. Front. Immunol. 2017, 8, 1749. [Google Scholar] [CrossRef] [PubMed]
- Kinet, J.P. The high-affinity IgE receptor (Fc epsilon RI): From physiology to pathology. Annu. Rev. Immunol. 1999, 17, 931–972. [Google Scholar] [CrossRef] [PubMed]
- Barua, D.; Goldstein, B. A Mechanistic Model of Early FcεRI Signaling: Lipid Rafts and the Question of Protection from Dephosphorylation. PLoS ONE 2012, 7, e51669. [Google Scholar] [CrossRef] [PubMed]
- Falcone, F.H.; Zillikens, D.; Gibbs, B.F. The 21st century renaissance of the basophil? Current insights into its role in allergic responses and innate immunity. Exp. Dermatol. 2006, 15, 855–864. [Google Scholar] [CrossRef] [PubMed]
- Dahinden, C.A.; Bischoff, S.C.; Brunner, T.; Krieger, M.; Takafuji, S.; de Weck, A.L. Regulation of mediator release by human basophils: Importance of the sequence and time of addition in the combined action of different agonists. Int. Arch. Allergy Appl. Immunol. 1991, 94, 161–164. [Google Scholar] [CrossRef]
- Bieneman, A.P.; Chichester, K.L.; Chen, Y.-H.; Schroeder, J.T. Toll-like receptor 2 ligands activate human basophils for both IgE-dependent and IgE-independent secretion. J. Allergy Clin. Immunol. 2005, 115, 295–301. [Google Scholar] [CrossRef]
- Ebo, D.G.; Bridts, C.H.; Mertens, C.H.; Hagendorens, M.M.; Stevens, W.J.; De Clerck, L.S. Analyzing histamine release by flow cytometry (HistaFlow): A novel instrument to study the degranulation patterns of basophils. J. Immunol. Methods 2012, 375, 30–38. [Google Scholar] [CrossRef]
- Kudo, I.; Murakami, M. Phospholipase A2 enzymes. Prostaglandins Other Lipid Mediat. 2002, 3–58. [Google Scholar] [CrossRef]
- Metcalfe, D.D.; Pawankar, R.; Ackerman, S.J.; Akin, C.; Clayton, F.; Falcone, F.H.; Gleich, G.J.; Irani, A.-M.; Johansson, M.W.; Klion, A.D.; et al. Biomarkers of the involvement of mast cells, basophils and eosinophils in asthma and allergic diseases. World Allergy Organ. J. 2016, 9, 7. [Google Scholar] [CrossRef]
- Sullivan, B.M.; Liang, H.-E.; Bando, J.K.; Wu, D.; Cheng, L.E.; McKerrow, J.K.; Allen, C.D.C.; Locksley, R.M. Genetic analysis of basophil function in vivo. Nat. Immunol. 2011, 12, 527–535. [Google Scholar] [CrossRef]
- Min, B.; Prout, M.; Hu-Li, J.; Zhu, J.; Jankovic, D.; Morgan, E.S.; Urban, J.F.; Dvorak, A.M.; Finkelman, F.D.; LeGros, G.; et al. Basophils Produce IL-4 and Accumulate in Tissues after Infection with a Th2-inducing Parasite. J. Exp. Med. 2004, 200, 507–517. [Google Scholar] [CrossRef] [PubMed]
- Siracusa, M.C.; Saenz, S.A.; Wojno, E.D.T.; Kim, B.S.; Osborne, L.C.; Ziegler, C.G.; Benitez, A.J.; Ruymann, K.R.; Farber, D.L.; Sleiman, P.M.; et al. Thymic stromal lymphopoietin-mediated extramedullary hematopoiesis promotes allergic inflammation. Immunity 2013, 39, 1158–1170. [Google Scholar] [CrossRef] [PubMed]
- Sokol, C.L.; Barton, G.M.; Farr, A.G.; Medzhitov, R. A mechanism for the initiation of allergen-induced T helper type 2 responses. Nat. Immunol. 2008, 9, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Poddighe, D.; Mathias, C.B.; Freyschmidt, E.J.; Kombe, D.; Caplan, B.; Marseglia, G.L.; Oettgen, H.C. Basophils are rapidly mobilized following initial aeroallergen encounter in naïve mice and provide a priming source of IL-4 in adaptive immune responses. J. Biol. Regul. Homeost. Agents 2014, 28, 91–103. [Google Scholar]
- Charles, N.; Watford, W.T.; Ramos, H.L.; Hellman, L.; Oettgen, H.C.; Gomez, G.; Ryan, J.J.; O’Shea, J.J.; Rivera, J. Lyn kinase controls basophil GATA-3 transcription factor expression and induction of Th2 cell differentiation. Immunity 2009, 30, 533–543. [Google Scholar] [CrossRef] [PubMed]
- Weiss, J.E. Pediatric Systemic Lupus Erythematosus: More Than a Positive Antinuclear Antibody. Pediatr. Rev. 2012, 33, 62–74. [Google Scholar] [CrossRef][Green Version]
- Leuchten, N.; Hoyer, A.; Brinks, R.; Schoels, M.; Schneider, M.; Smolen, J.; Johnson, S.R.; Daikh, D.; Dörner, T.; Aringer, M.; et al. Performance of Antinuclear Antibodies for Classifying Systemic Lupus Erythematosus: A Systematic Literature Review and Meta-Regression of Diagnostic Data. Arthritis Care Res. 2018, 70, 428–438. [Google Scholar] [CrossRef]
- Omarjee, O.; Picard, C.; Frachette, C.; Moreews, M.; Rieux-Laucat, F.; Soulas-Sprauel, P.; Viel, S.; Lega, J.-C.; Bader-Meunier, B.; Walzer, T.; et al. Monogenic lupus: Dissecting heterogeneity. Autoimmun. Rev. 2019, 18, 102361. [Google Scholar] [CrossRef]
- Karasuyama, H.; Miyake, K.; Yoshikawa, S.; Yamanishi, Y. Multifaceted roles of basophils in health and disease. J. Allergy Clin. Immunol. 2018, 142, 370–380. [Google Scholar] [CrossRef]
- Poddighe, D.; Marseglia, G.L. Commentary: Basophil Activation-Dependent Autoantibody and Interleukin-17 Production Exacerbate Systemic Lupus Erythematosus. Front. Immunol. 2017, 8. [Google Scholar] [CrossRef]
- Charles, N.; Hardwick, D.; Daugas, E.; Illei, G.G.; Rivera, J. Basophils and the T helper 2 environment can promote the development of lupus nephritis. Nat. Med. 2010, 16, 701–707. [Google Scholar] [CrossRef] [PubMed]
- Pan, Q.; Gong, L.; Xiao, H.; Feng, Y.; Li, L.; Deng, Z.; Ye, L.; Zheng, J.; Dickerson, C.A.; Ye, L.; et al. Basophil Activation-Dependent Autoantibody and Interleukin-17 Production Exacerbate Systemic Lupus Erythematosus. Front. Immunol. 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- Dema, B.; Lamri, Y.; Pellefigues, C.; Pacreau, E.; Saidoune, F.; Bidault, C.; Karasuyama, H.; Sacré, K.; Daugas, E.; Charles, N. Basophils contribute to pristane-induced Lupus-like nephritis model. Sci. Rep. 2017, 7. [Google Scholar] [CrossRef] [PubMed]
- Dema, B.; Charles, N.; Pellefigues, C.; Ricks, T.K.; Suzuki, R.; Jiang, C.; Scheffel, J.; Hasni, S.; Hoffman, V.; Jablonski, M.; et al. Immunoglobulin E plays an immunoregulatory role in lupus. J. Exp. Med. 2014, 211, 2159–2168. [Google Scholar] [CrossRef]
- Liang, P.; Tang, Y.; Fu, S.; Lv, J.; Liu, B.; Feng, M.; Li, J.; Lai, D.; Wan, X.; Xu, A. Basophil count, a marker for disease activity in systemic lupus erythematosus. Clin. Rheumatol. 2015, 34, 891–896. [Google Scholar] [CrossRef]
- Dijkstra, D.; Meyer-Bahlburg, A. Human Basophils Modulate Plasma Cell Differentiation and Maturation. J. Immunol. 2017, 198, 229–238. [Google Scholar] [CrossRef]
- Liang, P.; Tang, Y.; Lin, L.; Zhong, H.; Yang, H.; Zeng, Y.; Lv, J.; Li, X.; Lu, Y.; Xu, A. Low level of circulating basophil counts in biopsy-proven active lupus nephritis. Clin. Rheumatol. 2018, 37, 459–465. [Google Scholar] [CrossRef]
- Pellefigues, C.; Dema, B.; Lamri, Y.; Saidoune, F.; Chavarot, N.; Lohéac, C.; Pacreau, E.; Dussiot, M.; Bidault, C.; Marquet, F.; et al. Prostaglandin D2 amplifies lupus disease through basophil accumulation in lymphoid organs. Nat. Commun. 2018, 9. [Google Scholar] [CrossRef]
- Hasni, S.; Gupta, S.; Davis, M.; Poncio, E.; Temesgen-Oyelakin, Y.; Joyal, E.; Fike, A.; Manna, Z.; Auh, S.; Shi, Y.; et al. Safety and Tolerability of Omalizumab: A Randomized Clinical Trial of Humanized Anti-IgE Monoclonal Antibody in Systemic Lupus Erythematosus. Arthritis Rheumatol. 2019, 71, 1135–1140. [Google Scholar] [CrossRef]
- Webb, L.M.; Tait Wojno, E.D. The role of rare innate immune cells in Type 2 immune activation against parasitic helminths. Parasitology 2017, 144, 1288–1301. [Google Scholar] [CrossRef]
- Poddighe, D.; Brambilla, I.; Licari, A.; Marseglia, G.L. Pediatric rhinosinusitis and asthma. Respir. Med. 2018, 141, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Poddighe, D.; Mathias, C.B.; Brambilla, I.; Marseglia, G.L.; Oettgen, H.C. Importance of basophils in eosinophilic asthma: The murine counterpart. J. Biol. Regul. Homeost. Agents 2018, 32, 335–339. [Google Scholar] [PubMed]
- Perry, D.; Sang, A.; Yin, Y.; Zheng, Y.-Y.; Morel, L. Murine Models of Systemic Lupus Erythematosus. J. Biomed. Biotechnol. 2011, 2011, 271694. [Google Scholar] [CrossRef]
- Poddighe, D.; Vangelista, L. Effects of omalizumab on basophils: Potentials biomarkers in asthma and chronic spontaneous urticaria. Cell. Immunol. 2020. [Google Scholar] [CrossRef]

| Authorship | Disease | Mouse Model | Finding/Novelty | Brief Description |
|---|---|---|---|---|
| Charles et al. [41] | SLE | C57BL/6 Lyn−/− | Basophils may contribute to promote the development of lupus nephritis | “In SLE, self-reactive antibodies can target the kidney: the activation of basophils by autoreactive IgE causes their homing to lymph nodes, promoting Th2 cell differentiation and enhancing the production of self-reactive antibodies that cause lupus-like nephritis in mice lacking the protein tyrosine kinase Lyn.” |
| Pan et al. [42] | SLE | MRL-lpr | Basophil activation- dependent autoantibody can exacerbate SLE | “Increased activation of peripheral basophils was identified in MRL-lpr mice. Basophil-depleted MRL-lpr mice exhibited longer survival, improved renal function, and lower serum levels of autoantibodies and IL-17, while basophil-adoptive-transferred mice exhibited the opposite results.” |
| Dema et al. [43] | Pristane-induced lupus nephritis | Mcpt8DTR mice (C57BL/6 genetic background) | Basophils contribute to pristane-induced lupus-like nephritis (LN) model | “Pristane, when injected to non-lupus-prone mouse strains, induces an LN-like disease. In this inducible model, basophils were activated and accumulated in secondary lymphoid organs to promote autoantibody production. Basophil depletion by two distinct approaches dampened LN-like disease.” |
| Authorship | Articles Title | Findings |
|---|---|---|
| Charles et al. [41] | Basophils and the T-helper 2 environment can promote the development of lupus nephritis | In SLE, the presence of elevated serum IgE, self-reactive IgE, and activated CD62L+ and HLA-DR+ basophils are associated with active lupus nephritis and correlate with disease severity. |
| Dema et al. [44] | Immunoglobulin E plays an immunoregulatory role in lupus | The autoreactive IgE in SLE patients is associated with basophil activation and correlates with disease severity. |
| Liang et al. [45] | Basophil count, a marker for disease activity in systemic lupus erythematosus. | Different basophil counts in patients with active and nonactive disease, respectively. |
| Dijkstra. [46] | Human basophils modulate plasma cell differentiation and maturation | Basophils intensify proliferation and class switching in B-cell differentiation into plasma cells and production of immunoglobulins. |
| Pan et al. [42] | Basophil Activation-Dependent Autoantibody and Interleukin-17 Production Exacerbate Systemic Lupus Erythematosus | The presence of autoreactive IgE can mediate basophil activation in SLE. Basophils can amplify autoantibody production by B cells and promote Th17 differentiation. |
| Liang et al. [47] | Low level of circulating basophil counts in biopsy-proven active lupus nephritis | Prognostic value of basophil count in lupus nephritis. |
| Pellefigues et al. [48] | Prostaglandin D2 amplifies lupus disease through basophil accumulation in lymphoid organs | SLE patients have increased expression of PTGDR on basophils and elevated PGD2 metabolites. |
| Hasni et al. [49] | Safety and tolerability of omalizumab: A randomized clinical trial of humanized anti-IgE monoclonal antibody in systemic lupus erythematosus. | Omalizumab may improve SLE activity by decreasing IFN-I production and impairing pDC and basophil activation. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dossybayeva, K.; Abdukhakimova, D.; Poddighe, D. Basophils and Systemic Lupus Erythematosus in Murine Models and Human Patients. Biology 2020, 9, 308. https://doi.org/10.3390/biology9100308
Dossybayeva K, Abdukhakimova D, Poddighe D. Basophils and Systemic Lupus Erythematosus in Murine Models and Human Patients. Biology. 2020; 9(10):308. https://doi.org/10.3390/biology9100308
Chicago/Turabian StyleDossybayeva, Kuanysh, Diyora Abdukhakimova, and Dimitri Poddighe. 2020. "Basophils and Systemic Lupus Erythematosus in Murine Models and Human Patients" Biology 9, no. 10: 308. https://doi.org/10.3390/biology9100308
APA StyleDossybayeva, K., Abdukhakimova, D., & Poddighe, D. (2020). Basophils and Systemic Lupus Erythematosus in Murine Models and Human Patients. Biology, 9(10), 308. https://doi.org/10.3390/biology9100308





