Simple Summary
No consensus currently exists on immobilization protocols following shoulder surgery. The aim of this study was to identify patterns and types of sling used by surgeons from the United States and Europe for a variety of shoulder surgical procedures and further to identify factors associated with the variations. Four-hundred and ninety-nine surgeons with a median 15 years of experience responded, with 54.7% from the United States and 45.3% from Europe. United States surgeons reported higher abduction pillow sling use than European surgeons, whereas European surgeons reported more simple sling utilization. Increasing experience was negatively correlated with sling duration, meaning more experienced respondents tended to recommend shorter durations of sling use. Considerable variation exists in the immobilization patterns after a variety of shoulder surgical procedures advocated by surgeons with apparent influence from both geographic location and years of clinical experience. Future work is required to establish the most clinically beneficial protocols for immobilization following shoulder surgery.
Abstract
Background: There is currently no consensus on immobilization protocols following shoulder surgery. The aim of this study was to establish patterns and types of sling use for various surgical procedures in the United States (US) and Europe, and to identify factors associated with the variations. Methods: An online survey was sent to all members of the American Shoulder and Elbow Society (ASES) and European Society for Surgery of the Shoulder and Elbow (ESSSE). The survey gathered member data, including practice location and years in practice. It also obtained preferences for the type and duration of sling use after the following surgical procedures: arthroscopic Bankart repair, Latarjet, arthroscopic superior/posterosuperior rotator cuff repair (ARCR) of tears <3 cm and >3 cm, anatomic total shoulder arthroplasty (aTSA) and reverse TSA (rTSA), and isolated biceps tenodesis (BT). Relationships between physician location and sling type for each procedure were analyzed using Fisher’s exact tests and post-hoc tests using Bonferroni-adjusted p-values. Relationships looking at years in practice and sling duration preferred were analyzed using Spearman’s correlation tests. Results: In total, 499 surgeons with a median of 15 years of experience (IQR = 9–25) responded, with 54.7% from the US and 45.3% from Europe. US respondents reported higher abduction pillow sling use than European respondents for the following: Bankart repair (62% vs. 15%, p < 0.0001), Latarjet (53% vs. 12%, p < 0.001), ARCR < 3 cm (80% vs. 42%, p < 0.001) and >3 cm (84% vs. 61%, p < 0.001), aTSA (50% vs. 21%, p < 0.001) and rTSA with subscapularis repair (61% vs. 22%, p < 0.001) and without subscapularis repair (57% vs. 17%, p < 0.001), and isolated BT (18% vs. 7%, p = 0.006). European respondents reported higher simple sling use than US respondents for the following: Bankart repair (74% vs. 31%, p < 0.001), Latarjet (78% vs. 44%, p < 0.001), ARCR < 3 cm (50% vs. 17%, p < 0.001) and >3 cm (34% vs. 13%, p < 0.001), and aTSA (69% vs. 41%, p < 0.001) and rTSA with subscapularis repair (70% vs. 35%, p < 0.001) and without subscapularis repair (73% vs. 39%, p < 0.001). Increasing years of experience demonstrated a negative correlation with the duration of sling use after Bankart repair (r = −0.20, p < 0.001), Latarjet (r = −0.25, p < 0.001), ARCR < 3 cm (r = −0.14, p = 0.014) and >3 cm (r = −0.20, p < 0.002), and aTSA (r = −0.37, p < 0.001), and rTSA with subscapularis repair (r = −0.10, p = 0.049) and without subscapularis repair (r = −0.19, p = 0.022. Thus, the more experienced surgeons tended to recommend shorter durations of post-operative sling use. US surgeons reported longer post-operative sling durations for Bankart repair (4.8 vs. 4.1 weeks, p < 0.001), Latarjet (4.6 vs. 3.6 weeks, p < 0.001), ARCR < 3 cm (5.2 vs. 4.5 weeks p < 0.001) and >3 cm (5.9 vs. 5.1 weeks, p < 0.001), aTSA (4.9 vs. 4.3 weeks, p < 0.001), rTSR without subscapularis repair (4.0 vs. 3.6 weeks, p = 0.031), and isolated BT (3.7 vs. 3.3 weeks, p = 0.012) than Europe respondents. No significant differences between regions within the US and Europe were demonstrated. Conclusions: There is considerable variation in the immobilization advocated by surgeons, with geographic location and years of clinical experience influencing patterns of sling use. Future work is required to establish the most clinically beneficial protocols for immobilization following shoulder surgery. Level of Evidence: Level IV.
Keywords:
sling; rehabilitation; Latarjet; Bankart; arthroplasty; prosthesis: reverse; complications; rehabilitation 1. Introduction
Over 500,000 surgical procedures on the shoulder joint are performed each year in the United States (US) [1]. The number of shoulder replacements performed each year increased 5.6-fold between 1998 and 2017 [2], while surgery for rotator cuff tears has increased by approximately 10% each year over the last decade [3,4,5,6,7,8]. A significant determinant of recovery following shoulder surgery is the prescribed rehabilitation protocol [9,10,11,12,13,14,15,16,17].
A wide spectrum of postoperative rehabilitation protocols has been described for patients following open and arthroscopic procedures [18,19,20]. Surgeons may potentially improve outcomes after rotator cuff repair by controlling and optimizing the mechanical environment following surgery, with a period of immobilization being a widely adopted strategy [21,22,23,24,25]. Immobilization protects the shoulder from excessive forces that may damage the tissues or repair constructs and lead to early failure [26]. However, this must be balanced with the increased risk of postoperative shoulder stiffness and decreased shoulder function [26]. At present, the optimum duration of immobilization and its basic utility for a range of shoulder procedures remain unproven [27], with differing data and recommendations [21,22,23,24,25].
There is a wide range of shoulder immobilization products and protocols used by surgeons following shoulder surgery [25]. However, patterns of sling use among surgeons are not known and, furthermore, there is no consensus on the optimum position and duration of shoulder immobilization following a range of surgical procedures. The aim of this study was to establish patterns and types of sling use for various surgical procedures in the US and Europe and to identify factors associated with the variations. The hypothesis was that the types and durations of postoperative immobilization would vary depending on years of experience, procedures, and surgeons’ geographic locations.
2. Materials and Methods
An 18-question internet survey was developed and emailed to the membership of the American Shoulder and Elbow Society (ASES) and the European Society for Surgery of the Shoulder and Elbow (SECEC-ESSSE) in 20 April 2020 (Table 1). A reminder email was sent out on 6 May 2020. The data was downloaded and stored in a secure location at the Johns Hopkins University School of Medicine Department of Orthopaedic Surgery. Three of the 18 questions targeted demographic information, including country and region of practice and years of independent clinical practice. The type of immobilization was determined, including simple sling, shoulder immobilizer, abduction pillow sling, neutral rotation sling, abduction pillow sling in neutral rotation, and abduction pillow (no sling) (Figure 1). The remaining questions related to the technique and duration of immobilization following a variety of shoulder surgeries, namely arthroscopic Bankart repair, Latarjet procedure, arthroscopic superior/posterosuperior rotator cuff repair (ARCR) of tears <3 cm and >3 cm, anatomic total shoulder arthroplasty (aTSA) and reverse TSA (rTSA), and isolated biceps tenodesis.

Table 1.
The 18 question survey a.
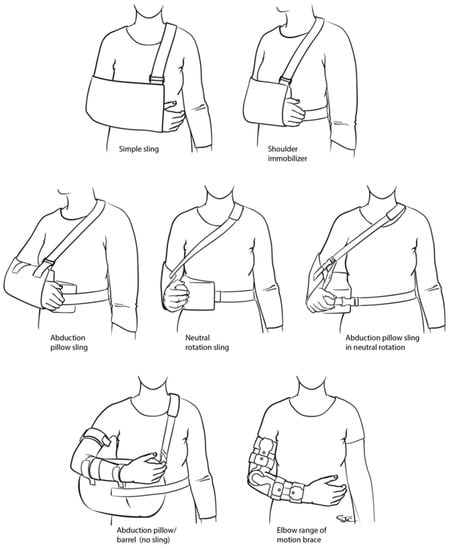
Figure 1.
Selected methods of upper limb immobilization utilized following shoulder surgery.
Since this study did not rely on patient data but solely on doctors’ answers to an online survey, an a priori approval by an ethical committee or written informed consent was not required. However, the participants (doctors) agreed by answering the survey to use their answers for research purposes.
Statistical Analysis
The responses were collected and tabulated using Microsoft Excel software version 16.69.1 (Microsoft Corporation, Redmond, WA, USA). Relationships between surgeon location and sling type were analyzed using Fisher’s exact tests and post-hoc tests using Bonferroni-adjusted p-values. Relationships between experience and sling duration were analyzed using Spearman’s correlation tests. The analysis was performed in RStudio (version 2022.12.0+353) (Posit Software, Boston, MA, USA) using a two-sided level of significance of 0.05.
3. Results
In total, 499 surveys were returned and completed. Some respondents did not answer some questions, and to maintain consistency, 499 was used as the denominator for all percentage calculations for the responses.
Of the 499 surgeon respondents, 54.7% were US-based, with 45.3% based in Europe (Table 2). The median years of experience in independent clinical practice was 15 (IQR = 9–25), with respondents from Europe being more experienced than respondents from the United States (median 18 vs. 12 years, p = 0.000095). The response rate was 273/992 = 28% (ASES) and 226/618 = 37% (ESSSE).

Table 2.
Location of surgeon respondent.
3.1. Arthroscopic Bankart Repair (ABR)
The variation in the use of sling based on surgeon location is outlined in Table 3. Surgeons based in the US reported higher abduction pillow sling use than Europeans (62% vs. 15%, p < 0.0001), while Europeans reported higher simple sling use than Americans (74% vs. 31%, p < 0.001) (Table 3). For each additional decade of experience, the average sling duration in weeks decreased by 0.2 weeks (Figure 2A). On average, respondents from the US reported one week longer sling durations than Europeans (mean 4.8 weeks vs. 4 weeks, p < 0.001). The interaction between location and experience was significant, indicating that the relationship between experience and sling duration was significantly different for US and European surgeons. Experience did not influence sling duration for European surgeons, but it did for US surgeons (Figure 2B). There were no significant differences between regions within the US and Europe.

Table 3.
Variation in use of sling following arthroscopic Bankart repair based on surgeon location.
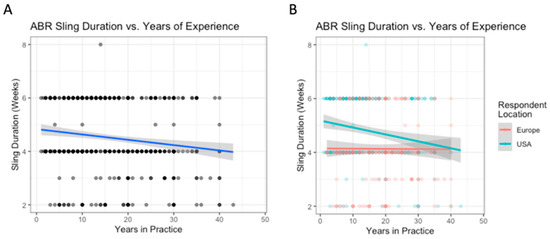
Figure 2.
Arthroscopic Bankart repair: the relationship between years of experience and sling duration (A); with breakdown by location (B).
3.2. Latarjet
The variation in use of sling based on surgeon location is outlined in Table 4. Surgeons based in the US reported higher abduction pillow sling use than Europeans (53% vs. 12%, p < 0.0001), while Europeans reported higher simple sling use than Americans (78% vs. 44%, p < 0.001) (Table 4). For each additional decade of experience, the average sling duration in weeks decreased by 0.25 weeks (Figure 3A). On average, respondents from the US reported 1 week longer sling durations than Europeans (mean 4.6 vs. 3.6 weeks, p < 0.001). The relationship between experience and sling duration was significantly different for US and European surgeons: experience influenced sling duration more for US surgeons than it did for European surgeons (Figure 3B). There were no significant differences between regions within the US and Europe.

Table 4.
Variation in use of sling following the Latarjet procedure based on surgeon location.
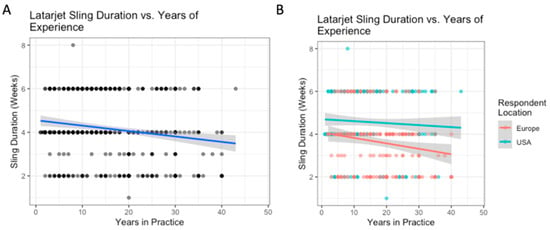
Figure 3.
Latarjet procedure: the relationship between years of experience and sling duration (A); with breakdown by location (B).
3.3. ARCR (Tears < 3 cm)
The variation in use of sling based on surgeon location is outlined in Table 5. Surgeons based in the US reported higher abduction pillow sling use than Europeans (80% vs. 42%, p < 0.0001), while Europeans reported higher simple sling use than Americans (50% vs. 17%, p < 0.001) (Table 5). For each additional decade of experience, the average sling duration in weeks decreased by 0.14 weeks (Figure 4A). On average, respondents from the US reported 1 week longer sling durations than Europeans (mean 5.2 weeks vs. 4.5 weeks, p < 0.001). There were no significant differences between regions within the US and Europe. The interaction between location and experience was significant, indicating that the relationship between experience and sling duration was significantly different for US and European surgeons. Experience did not influence sling duration for European surgeons, but it did for US surgeons (Figure 4B).

Table 5.
Variation in use of sling following the ARCR (tears < 3 cm) based on surgeon location.
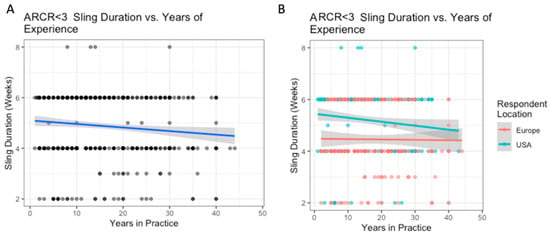
Figure 4.
ARCR (tears < 3 cm): the relationship between years of experience and sling duration (A); with breakdown by location (B).
3.4. ARCR Cuff (Tears > 3 cm)
The variation in use of sling based on surgeon location is outlined in Table 6. Surgeons based in the US reported higher abduction pillow sling use than Europeans (84% vs. 61%, p < 0.0001), while Europeans reported higher simple sling use than Americans (34% vs. 13%, p < 0.001) (Table 6). For each additional decade of experience, the average sling duration in weeks decreased by 0.2 weeks (Figure 5A); however, experience did not influence sling duration for US and European surgeons when considered separately (Figure 5B). On average, respondents from the US reported 1 week longer sling durations than Europeans (mean 5.9 vs. 5.1 weeks, p < 0.001). Experience influences sling duration more for US-based surgeons than for Europeans (Figure 5B). There were no significant differences between regions within the US and Europe.

Table 6.
Variation in use of sling following ARCR (tears > 3 cm) based on surgeon location.
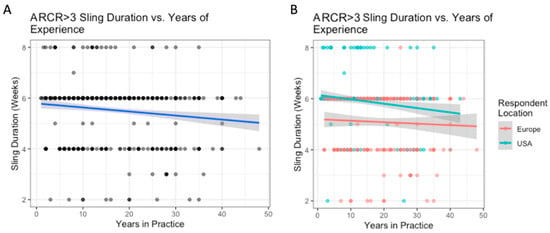
Figure 5.
ARCR (tears > 3 cm): the relationship between years of experience and sling duration (A); with breakdown by location (B).
3.5. aTSA
The variation in use of sling based on surgeon location is outlined in Table 7. Surgeons based in the US reported higher abduction pillow sling use than Europeans (50% vs. 21%, p < 0.0001), while Europeans reported higher simple sling use than Americans (69% vs. 41%, p < 0.001) (Table 6). On average, respondents from the US reported 1 week longer sling durations than Europeans (mean 4.9 weeks vs. 4.3 weeks, p < 0.001). For each additional decade of experience, the average sling duration in weeks decreased by 0.4 weeks (Figure 6). However, the relationship between experience and sling duration was not significantly different between European and US-based surgeons. There were no significant differences between regions within the US and Europe.

Table 7.
Variation in use of sling following aTSA based on surgeon location.
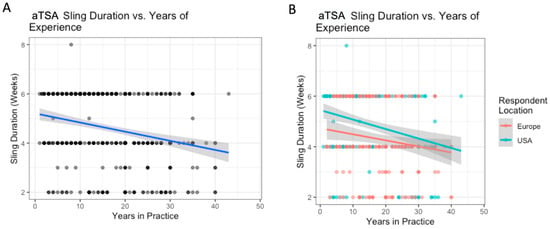
Figure 6.
ATSA: the relationship between years of experience and sling duration (A); with breakdown by location (B).
3.6. rTSA with Subscapularis Repair
The variation in use of sling based on surgeon location is outlined in Table 8. Surgeons based in the US reported higher abduction pillow sling use than Europeans (61% vs. 22%, p < 0.001), while Europeans reported higher simple sling use than Americans (69% vs. 35%, p < 0.001) (Table 8). There was no difference in sling durations between US and European respondents (mean 4.4 vs. 4.2 weeks, p = 0.414) and there were no significant differences between regions within the US and Europe. For each additional decade of experience, the average sling duration in weeks decreased by 0.1 weeks (p = 0.049) (Figure 7A). Experience did not influence sling duration differently for US and European surgeons (Figure 7B).

Table 8.
Variation in use of sling following rTSA with subscapularis repair based on surgeon location.
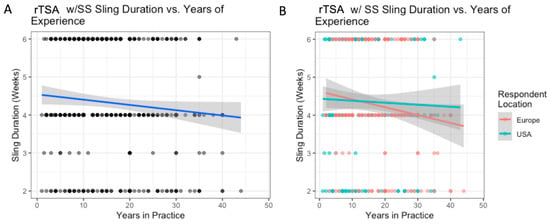
Figure 7.
rTSA with subscapularis repair: the relationship between years of experience and sling duration (A); with breakdown by location (B).
3.7. rTSA without Subscapularis Repair
Variation in use of sling based on surgeon location is outlined in Table 9. Surgeons based in the US reported higher abduction pillow sling use than Europeans (57% vs. 18%, p < 0.001), while Europeans reported higher simple sling use than Americans (73% vs. 39%, p < 0.001) (Table 9). For each additional decade of experience, the average sling duration in weeks decreased by 0.19 weeks (p = 0.022) (Figure 8A). Experience did not influence sling duration differently for US and European surgeons (Figure 7B). On average, respondents from the US reported 1 week longer sling durations than Europeans (mean 4.0 vs. 3.6 weeks, p = 0.031). There were no significant differences between regions within the US and Europe.

Table 9.
Variation in use of sling following rTSA without subscapularis repair based on surgeon location.
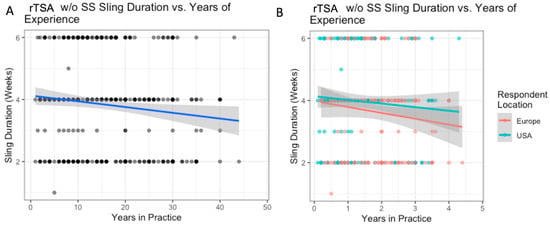
Figure 8.
rTSA without subscapularis repair: the relationship between years of experience and sling duration (A); with breakdown by location (B).
3.8. Isolated Biceps Tenodesis
The majority of respondents based in the US and Europe recommended simple sling immobilization following isolated biceps tenodesis procedures (77% and 82%, respectively, p = 0.899). However, respondents in the US reported higher abduction pillow sling use than Europeans (18% vs. 7%, p < 0.001) (Table 10). Experience did not influence the duration of immobilization within the US or Europe (Figure 9). There were no significant differences between regions within the US and Europe. US-based surgeons reported longer sling durations than their European counterparts. (3.7 vs. 3.3 weeks, p = 0.012). However, experience did not influence sling duration in either region.

Table 10.
Variation in use of sling following isolated biceps tenodesis based on surgeon location.
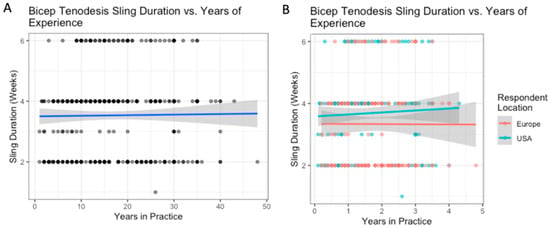
Figure 9.
Isolated biceps tenodesis: the relationship between years of experience and sling duration (A); with breakdown by location (B).
4. Discussion
The most important finding of this study was the differences in preferred immobilization methods between US-based surgeons and their European counterparts. An abduction pillow sling was the preferred method of immobilization for the majority of US-based surgeons, following Bankart repair, Latarjet procedure, ARCR of tears <3 cm and >3 cm, aTSA, and rTSA. This is in contrast to European surgeons who preferred a simple sling for all procedures except for ARCR of >3 cm in size.
Availability and cost play an important role in postoperative immobilization. For instance, some abduction braces are either not available in Europe, simply not reimbursed by healthcare systems, or are sold at a prohibitive cost. Furthermore, regarding compliance with postoperative immobilization and abduction brace wearing, a publication revealed that about 50% of European patients actually do not adhere to the suggested immobilization regimen [28]. Moreover, some European publications advise the abolition of postoperative immobilization after Latarjet procedures, small to medium rotator cuff repairs, and rTSAs [23,29,30]. Consequently, surgeon selection of immobilization strategy may be influenced not only by the availability and cost of equipment and historical use of one method over another, but also by patient preference and compliance and recent publications, explaining differences found between the two continents.
There was also a considerable variation in sling durations recommended by respondents in both the US and Europe. Respondents recommended from 0–8 weeks of sling immobilization following Bankart repair, Latarjet procedure, ARCR of tears <3 cm and >3 cm, aTSA, and rTSA, and 0–6 weeks of immobilization following isolated biceps tenodesis. More experienced clinicians were more likely to recommend shorter periods of immobilization across all procedures surveyed, with the exception of isolated biceps tenodesis. For the majority of procedures, US-based surgeons reported longer sling durations than Europeans. This study highlights the considerable variation in practice among shoulder surgeons in postoperative immobilization. Currently, the optimum duration of immobilization and its basic utility for a range of shoulder procedures remains unproven [27] with differing data and recommendations [21,22,23,24,25]. Future work is required to establish the most clinically beneficial protocols for immobilization following shoulder surgery. This is challenging due to the range of immobilization strategies and durations currently being used.
This study has several strengths. This represented the largest study of shoulder surgeon specialists that the authors are aware of, with representation across all regions of the US and Europe. The surgeons who responded represent a comprehensive mix of experienced surgeons and surgeons just starting their practice. This study has several limitations, including the cross-sectional nature of the study, with responses based on surgeon opinion at a single point in time. As such, the study is subject to selection and recall bias. Additionally, although the number of responses was high, the response rate was low, which may introduce a potential source of bias pending the responses of those who did not participate, as well as those who chose to participate. Further, not all questions were answered by all respondents, likely due to survey fatigue, so a correction was needed in some cases to determine the proper percentages for the responses. In addition, using an online–only response system may have introduced selection bias by omitting potential responders who are less ‘technologically adept’.
5. Conclusions
There is considerable variation in the immobilization advocated by surgeons with geographic location and years of clinical experience influencing patterns of sling use. Future work is required to establish the most clinically beneficial protocols for immobilization following various types of shoulder surgery. This is challenging due to the range of immobilization strategies and durations currently being used.
Author Contributions
Conceptualization, M.T.F., U.S., E.C. and A.L.; methodology, M.T.F., U.S., E.C. and A.L.; software, A.L. and I.R.M.; validation, I.R.M.; formal analysis, I.R.M.; investigation, M.T.F., U.S., E.C. and A.L.; resources, M.T.F., A.L. and I.R.M.; data curation, I.R.M.; writing—original draft preparation, M.T.F. and I.R.M.; writing—review and editing, M.T.F., U.S., E.C. and A.L.; visualization, M.T.F. and I.R.M.; supervision, M.T.F.; project administration, M.T.F. All authors have read and agreed to the published version of the manuscript.
Funding
FORE (Foundation for Research and Teaching in Orthopedics, Sports Medicine, Trauma, and Imaging in the Musculoskeletal System) Grant #FORE 2022-31.
Institutional Review Board Statement
Approved by Stanford Research Compliance office #56644.
Informed Consent Statement
N/A.
Data Availability Statement
The following was the link sent out to all members of the American Shoulder and Elbow Society and the European Society for Surgery of the Shoulder and Elbow in April of 2020. https://docs.google.com/spreadsheets/d/1iCKrhYmPvbhTiYyXcAdd5-Obiw1E6NUPVMXymYQKEAI/edit?usp=sharing (accessed on 21 January 2023). The initial survey was sent out on 20 April 2020 and a reminder email was sent out on 6 May 2020. The data was downloaded and stored in a secure location at the Johns Hopkins University School of Medicine Department of Orthopaedic Surgery.
Conflicts of Interest
Michael T. Freehill reports royalties from Smith & Nephew; consulting fees from Smith & Nephew, Stryker, and Conmed; research support from Smith & Nephew, Arthrex, National Institutes of Health, Major League Baseball; committee member- ASES, AOSSM, ISAKOS, AAOS. Iain R. Murray reports consulting fees from Stryker and Arthrex and Editorial board membership for Bone Joint Journal (BJJ) and Bone and Joint Research (BJR). Alexandre Lädermann reports personal fees from Arthrex, personal fees from Stryker, and personal fees from Medacta, outside the submitted work; he is the Founder of BeeMed and Med4cast, as well as the founder and president of FORE foundation. He owns stock options in Medacta and Follow Health. Emilio Calvo reports paid presenter or speaker for DePuy Synthes, A Johnson & Johnson Company; board or committee member for the European Society for Surgery of the Shoulder and Elbow; board or committee member for the International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine; paid consultant for Johnson & Johnson; editorial or governing board for Journal of Shoulder and Elbow Surgery; paid presenter or speaker and research support from Smith & Nephew; and paid presenter or speaker for Stryker; outside the submitted work. Uma Srikumaran reports Board or committee member for AAOS, American Shoulder and Elbow Surgeons, IASES; financial or material support from Arthrex, Inc, DePuy, A Johnson & Johnson Company; paid consultant, presenter, or speaker for Fx Shoulder; paid consultant for Orthofix, Inc.; stock or stock Options Quantum OPS, ROM3, Sonogen; other financial or material support from Stryker, Wright Medical Technology, Inc.; publishing royalties, financial or material support from Thieme; IP royalties; paid consultant; stock or stock Options from Tigon Medical.
References
- Jain, N.B.; Higgins, L.D.; Losina, E.; Collins, J.; Blazar, P.E.; Katz, J.N. Epidemiology of musculoskeletal upper extremity ambulatory surgery in the United States. BMC Musculoskelet. Disord. 2014, 15, 4. [Google Scholar] [CrossRef] [PubMed]
- Craig, R.S.; Lane, J.C.E.; Carr, A.J.; Furniss, D.; Collins, G.S.; Rees, J.L. Serious adverse events and lifetime risk of reoperation after elective shoulder replacement: Population based cohort study using hospital episode statistics for England. BMJ (Clin. Res. Ed.) 2019, 364, l298. [Google Scholar] [CrossRef] [PubMed]
- Vidal, C.; Lira, M.J.; de Marinis, R.; Liendo, R.; Contreras, J.J. Increasing incidence of rotator cuff surgery: A nationwide registry study in Chile. BMC Musculoskelet. Disord. 2021, 22, 1052. [Google Scholar] [CrossRef] [PubMed]
- MacDermid, J.C.; Bryant, D.; Holtby, R.; Razmjou, H.; Faber, K.; Balyk, R.; Boorman, R.; Sheps, D.; McCormack, R.; Athwal, G.; et al. Arthroscopic Versus Mini-open Rotator Cuff Repair: A Randomized Trial and Meta-analysis. Am. J. Sport. Med. 2021, 49, 3184–3195. [Google Scholar] [CrossRef]
- Wong, I.; Sparavalo, S.; King, J.P.; Coady, C.M. Bridging Allograft Reconstruction Is Superior to Maximal Repair for the Treatment of Chronic, Massive Rotator Cuff Tears: Results of a Prospective, Randomized Controlled Trial. Am. J. Sport. Med. 2021, 49, 3173–3183. [Google Scholar] [CrossRef] [PubMed]
- Lapner, P.; Li, A.; Pollock, J.W.; Zhang, T.; McIlquham, K.; McRae, S.; MacDonald, P. A Multicenter Randomized Controlled Trial Comparing Single-Row With Double-Row Fixation in Arthroscopic Rotator Cuff Repair: Long-Term Follow-up. Am. J. Sport. Med. 2021, 49, 3021–3029. [Google Scholar] [CrossRef]
- Yapp, L.Z.; Nicholson, J.A.; Robinson, C.M. Primary Arthroscopic Stabilization for a First-Time Anterior Dislocation of the Shoulder: Long-Term Follow-up of a Randomized, Double-Blinded Trial. J. Bone Jt. Surg. Am. 2020, 102, 460–467. [Google Scholar] [CrossRef]
- Jonsson, E.; Ekholm, C.; Salomonsson, B.; Demir, Y.; Olerud, P. Reverse total shoulder arthroplasty provides better shoulder function than hemiarthroplasty for displaced 3- and 4-part proximal humeral fractures in patients aged 70 years or older: A multicenter randomized controlled trial. J. Shoulder Elb. Surg. 2021, 30, 994–1006. [Google Scholar] [CrossRef]
- Bandara, U.; An, V.V.G.; Imani, S.; Nandapalan, H.; Sivakumar, B.S. Rehabilitation protocols following rotator cuff repair: A meta-analysis of current evidence. ANZ J. Surg. 2021, 91, 2773–2779. [Google Scholar] [CrossRef]
- Chan, K.; MacDermid, J.C.; Hoppe, D.J.; Ayeni, O.R.; Bhandari, M.; Foote, C.J.; Athwal, G.S. Delayed versus early motion after arthroscopic rotator cuff repair: A meta-analysis. J. Shoulder Elb. Surg. 2014, 23, 1631–1639. [Google Scholar] [CrossRef]
- Arndt, J.; Clavert, P.; Mielcarek, P.; Bouchaib, J.; Meyer, N.; Kempf, J.F. Immediate passive motion versus immobilization after endoscopic supraspinatus tendon repair: A prospective randomized study. Orthop. Traumatol. Surg. Res. OTSR 2012, 98, S131–S138. [Google Scholar] [CrossRef] [PubMed]
- Klintberg, I.H.; Gunnarsson, A.C.; Svantesson, U.; Styf, J.; Karlsson, J. Early loading in physiotherapy treatment after full-thickness rotator cuff repair: A prospective randomized pilot-study with a two-year follow-up. Clin. Rehabil. 2009, 23, 622–638. [Google Scholar] [CrossRef]
- Abtahi, A.M.; Granger, E.K.; Tashjian, R.Z. Factors affecting healing after arthroscopic rotator cuff repair. World J. Orthop. 2015, 6, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Chung, S.W.; Kim, J.Y.; Ok, J.H.; Park, I.; Oh, J.H. Is early passive motion exercise necessary after arthroscopic rotator cuff repair? Am. J. Sport. Med. 2012, 40, 815–821. [Google Scholar] [CrossRef] [PubMed]
- Denard, P.J.; Lädermann, A.; Burkhart, S.S. Prevention and management of stiffness after arthroscopic rotator cuff repair: Systematic review and implications for rotator cuff healing. Arthroscopy 2011, 27, 842–848. [Google Scholar] [CrossRef] [PubMed]
- Hsu, J.E.; Horneff, J.G.; Gee, A.O. Immobilization After Rotator Cuff Repair: What Evidence Do We Have Now? Orthop. Clin. N. Am. 2016, 47, 169–177. [Google Scholar] [CrossRef]
- Sharareh, B.; Edwards, T.B.; Shah, A.; Shybut, T. Variation in technique and postoperative management of the Latarjet procedure among orthopedic surgeons. J. Shoulder Elb. Surg. 2021, 30, e157–e164. [Google Scholar] [CrossRef] [PubMed]
- Steinmetz, R.G.; Guth, J.J.; Matava, M.J.; Brophy, R.H.; Smith, M.V. Return to Play Following Non-Surgical Management of Superior Labrum Anterior-Posterior Tears: A Systematic Review. J. Shoulder Elb. Surg. 2022, 31, 1323–1333. [Google Scholar] [CrossRef]
- Kelley, T.D.; Clegg, S.; Rodenhouse, P.; Hinz, J.; Busconi, B.D. Functional Rehabilitation and Return to Play After Arthroscopic Surgical Stabilization for Anterior Shoulder Instability. Sport. Health 2021, 14, 19417381211062852. [Google Scholar] [CrossRef]
- McIsaac, W.; Lalani, A.; Silveira, A.; Chepeha, J.; Luciak-Corea, C.; Beaupre, L. Rehabilitation after arthroscopic Bankart repair: A systematic scoping review identifying important evidence gaps. Physiotherapy 2022, 114, 68–76. [Google Scholar] [CrossRef]
- Paterson, W.H.; Throckmorton, T.W.; Koester, M.; Azar, F.M.; Kuhn, J.E. Position and duration of immobilization after primary anterior shoulder dislocation: A systematic review and meta-analysis of the literature. J. Bone Jt. Surg. Am. 2010, 92, 2924–2933. [Google Scholar] [CrossRef] [PubMed]
- Sheps, D.M.; Silveira, A.; Beaupre, L.; Styles-Tripp, F.; Balyk, R.; Lalani, A.; Glasgow, R.; Bergman, J.; Bouliane, M. Early Active Motion Versus Sling Immobilization After Arthroscopic Rotator Cuff Repair: A Randomized Controlled Trial. Arthroscopy 2019, 35, 749–760.e742. [Google Scholar] [CrossRef]
- Tirefort, J.; Schwitzguebel, A.J.; Collin, P.; Nowak, A.; Plomb-Holmes, C.; Lädermann, A. Postoperative Mobilization After Superior Rotator Cuff Repair: Sling Versus No Sling: A Randomized Prospective Study. J. Bone Jt. Surg. Am. 2019, 101, 494–503. [Google Scholar] [CrossRef] [PubMed]
- Whelan, D.B.; Kletke, S.N.; Schemitsch, G.; Chahal, J. Immobilization in External Rotation Versus Internal Rotation After Primary Anterior Shoulder Dislocation: A Meta-analysis of Randomized Controlled Trials. Am. J. Sport. Med. 2016, 44, 521–532. [Google Scholar] [CrossRef]
- Belk, J.W.; Wharton, B.R.; Houck, D.A.; Bravman, J.T.; Kraeutler, M.J.; Mayer, B.; Noonan, T.J.; Seidl, A.J.; Frank, R.M.; McCarty, E.C. Shoulder Stabilization Versus Immobilization for First-Time Anterior Shoulder Dislocation: A Systematic Review and Meta-analysis of Level 1 Randomized Controlled Trials. Am. J. Sport. Med. 2022, 3635465211065403. [Google Scholar] [CrossRef]
- Boland, K.; Smith, C.; Bond, H.; Briggs, S.; Walton, J. Current concepts in the rehabilitation of rotator cuff related disorders. J. Clin. Orthop. Trauma 2021, 18, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Handoll, H.H.; Hanchard, N.C.; Goodchild, L.; Feary, J. Conservative management following closed reduction of traumatic anterior dislocation of the shoulder. Cochrane Database Syst. Rev. 2006, Cd004962. [Google Scholar] [CrossRef]
- Grubhofer, F.; Gerber, C.; Meyer, D.C.; Wieser, K.; Ernstbrunner, L.; Catanzaro, S.; Bouaicha, S. Compliance with wearing an abduction brace after arthroscopic rotator cuff repair: A prospective, sensor-controlled study. Prosthet. Orthot. Int. 2019, 43, 440–446. [Google Scholar] [CrossRef]
- Lädermann, A.; Denard, P.J.; Tirefort, J.; Collin, P.; Nowak, A.; Schwitzguebel, A.J. Subscapularis- and deltoid-sparing vs traditional deltopectoral approach in reverse shoulder arthroplasty: A prospective case-control study. J. Orthop. Surg. Res. 2017, 12, 112. [Google Scholar] [CrossRef]
- Goetti, P.; Martinho, T.; Seurot, A.; Bothorel, H.; Läderman, A. Is there a benefit of sling immobilization after open Latarjet surgery for anterior shoulder instability? A randomized control trial. Rev. De Chir. Orthopédique Et Traumatol. 2022, 108, S257–S258. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).