Natriuretic Peptide-Based Novel Therapeutics: Long Journeys of Drug Developments Optimized for Disease States
Abstract
Simple Summary
Abstract
1. Introduction
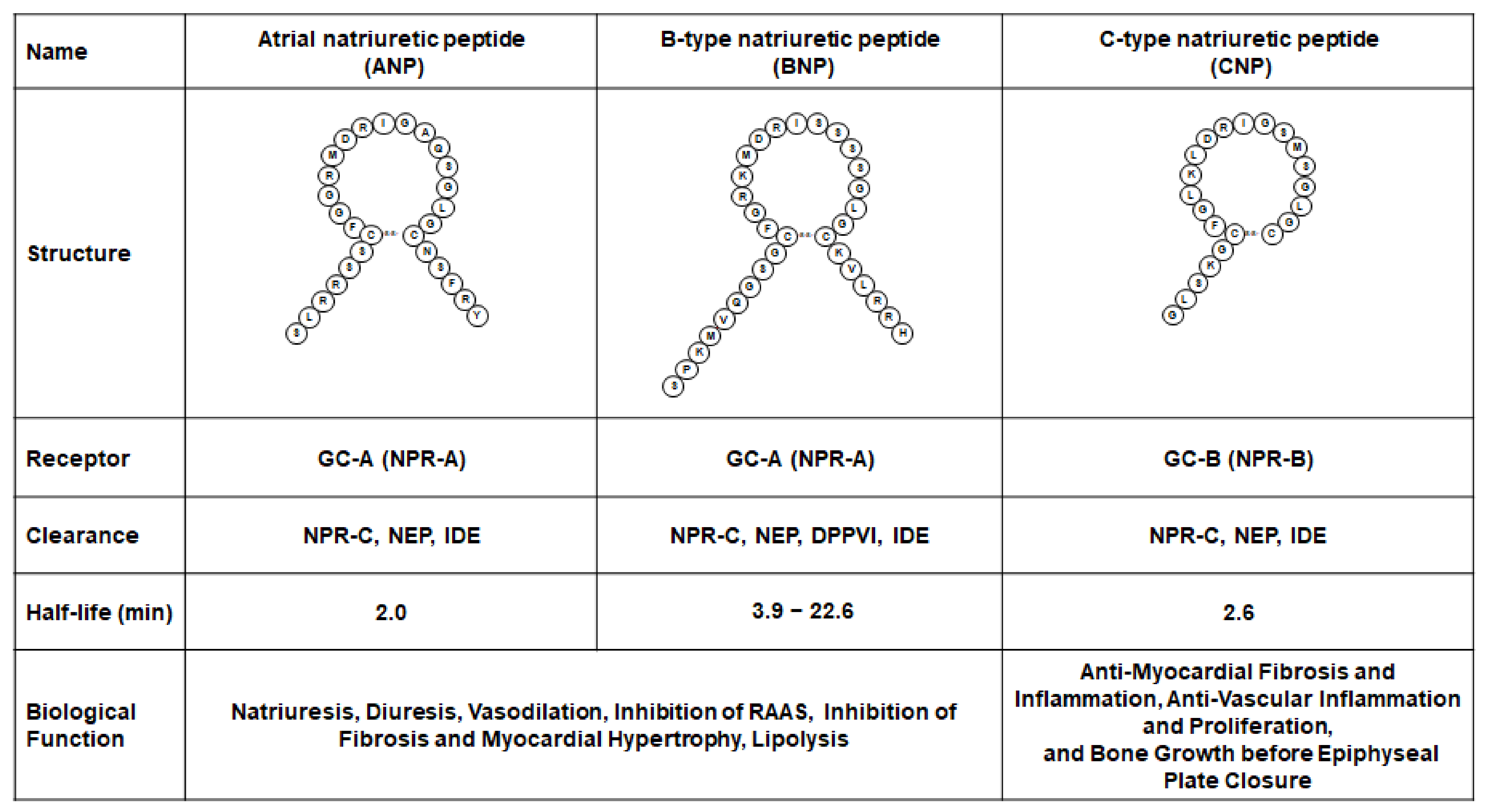
1.1. Biology of Natriuretic Peptides
1.2. Therapeutics of Native Natriuretic Peptides and the Directions
2. Designing with Natriuretic Peptides
2.1. Dual GC-A and GC-B Activator: Cenderitide (CD-NP)
2.2. Long Acting ANP: MANP
2.3. BNP Based Peptides
2.3.1. ASBNP.1 (ANX-042)
2.3.2. CRRL269
2.4. Long-Acting CNP
2.4.1. Vosoritide
2.4.2. TransCon CNP
3. Designing Natriuretic Peptides with Peptides from Other Systems
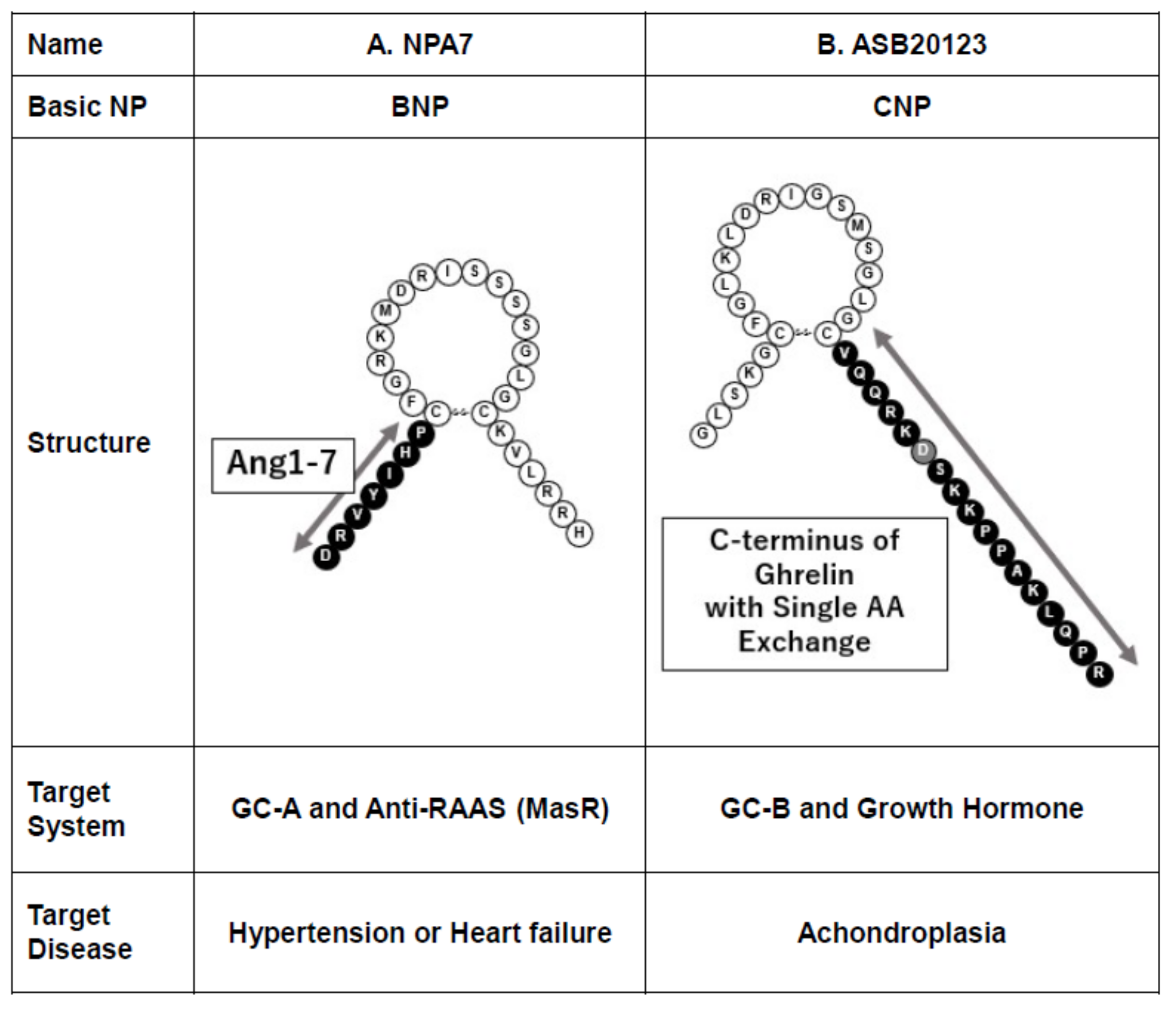
3.1. NPA7
3.2. ASB20123
4. Oral Drugs as Modulators for Endogenous Natriuretic Peptides
4.1. Difficulty in Developing Oral Drugs for Peptides
4.2. Sacubitril/Valsartan
4.3. Small Molecules Targeting GC-A Receptor
4.3.1. GC-A Activator
4.3.2. GC-A Positive Allosteric Modulator, MCUF-651
4.4. How to Use Novel Drugs of NP Systems, Properly?
5. Future Prospects for Drug Discovery of Natriuretic Peptides
5.1. Safety Verification
5.2. Barriers to Patent Validity and the Enormous Costs for Clinical Trials
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- De Bold, A.J. Heart atria granularity effects of changes in water-electrolyte balance. Proc. Soc. Exp. Biol Med. 1979, 161, 508–511. [Google Scholar] [CrossRef] [PubMed]
- de Bold, A.J. Atrial natriuretic factor of the rat heart. Studies on isolation and properties. Proc. Soc. Exp. Biol. Medicine. Soc. Exp. Biol. Med. 1982, 170, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Kangawa, K.; Matsuo, H. Purification and complete amino acid sequence of alpha-human atrial natriuretic polypeptide (alpha-hANP). Biochem. Biophys. Res. Commun. 1984, 118, 131–139. [Google Scholar] [CrossRef]
- Sudoh, T.; Minamino, N.; Kangawa, K.; Matsuo, H. C-type natriuretic peptide (CNP): A new member of natriuretic peptide family identified in porcine brain. Biochem. Biophys. Res. Commun 1990, 168, 863–870. [Google Scholar] [CrossRef]
- Potter, L.R. Natriuretic peptide metabolism, clearance and degradation. FEBS J. 2011, 278, 1808–1817. [Google Scholar] [CrossRef] [PubMed]
- Yasoda, A.; Nakao, K. Translational research of C-type natriuretic peptide (CNP) into skeletal dysplasias. Endocr. J. 2010, 57, 659–666. [Google Scholar] [CrossRef]
- Saito, Y. Roles of atrial natriuretic peptide and its therapeutic use. J. Cardiol. 2010, 56, 262–270. [Google Scholar] [CrossRef][Green Version]
- Ichiki, T.; Huntley, B.K.; Burnett, J.C., Jr. BNP molecular forms and processing by the cardiac serine protease corin. Adv. Clin. Chem. 2013, 61, 1–31. [Google Scholar]
- Ichiki, T.; Burnett, J.C., Jr. Atrial Natriuretic Peptide- Old But New Therapeutic in Cardiovascular Diseases. Circ. J. 2017, 81, 913–919. [Google Scholar] [CrossRef]
- Bordicchia, M.; Liu, D.; Amri, E.Z.; Ailhaud, G.; Dessi-Fulgheri, P.; Zhang, C.; Takahashi, N.; Sarzani, R.; Collins, S. Cardiac natriuretic peptides act via p38 MAPK to induce the brown fat thermogenic program in mouse and human adipocytes. J. Clin. Investig. 2012, 122, 1022–1036. [Google Scholar] [CrossRef]
- Miyashita, K.; Itoh, H.; Tsujimoto, H.; Tamura, N.; Fukunaga, Y.; Sone, M.; Yamahara, K.; Taura, D.; Inuzuka, M.; Sonoyama, T.; et al. Natriuretic peptides/cGMP/cGMP-dependent protein kinase cascades promote muscle mitochondrial biogenesis and prevent obesity. Diabetes 2009, 58, 2880–2892. [Google Scholar] [CrossRef] [PubMed]
- Coue, M.; Barquissau, V.; Morigny, P.; Louche, K.; Lefort, C.; Mairal, A.; Carpene, C.; Viguerie, N.; Arner, P.; Langin, D.; et al. Natriuretic peptides promote glucose uptake in a cGMP-dependent manner in human adipocytes. Sci. Rep. 2018, 8, 1097. [Google Scholar] [CrossRef] [PubMed]
- Ferraino, K.E.; Cora, N.; Pollard, C.M.; Sizova, A.; Maning, J.; Lymperopoulos, A. Adrenal angiotensin II type 1 receptor biased signaling: The case for “biased” inverse agonism for effective aldosterone suppression. Cell Signal. 2021, 82, 109967. [Google Scholar] [CrossRef] [PubMed]
- Guitart-Mampel, M.; Urquiza, P.; Borges, J.I.; Lymperopoulos, A.; Solesio, M.E.E. Impact of Aldosterone on the Failing Myocardium: Insights from Mitochondria and Adrenergic Receptors Signaling and Function. Cells 2021, 10, 1552. [Google Scholar] [CrossRef]
- Kuwahara, K. The natriuretic peptide system in heart failure: Diagnostic and therapeutic implications. Pharmacol. Ther. 2021, 227, 107863. [Google Scholar] [CrossRef]
- Miura, S.; Nakayama, A.; Tomita, S.; Matsuo, Y.; Suematsu, Y.; Saku, K. Comparison of aldosterone synthesis in adrenal cells, effect of various AT1 receptor blockers with or without atrial natriuretic peptide. Clin. Exp. Hypertens 2015, 37, 353–357. [Google Scholar] [CrossRef]
- Moyes, A.J.; Hobbs, A.J. C-type Natriuretic Peptide: A Multifaceted Paracrine Regulator in the Heart and Vasculature. Int. J. Mol. Sci. 2019, 20, 2281. [Google Scholar] [CrossRef]
- Kuhn, M. Molecular Physiology of Membrane Guanylyl Cyclase Receptors. Physiol Rev. 2016, 96, 751–804. [Google Scholar] [CrossRef]
- Friebe, A.; Sandner, P.; Schmidtko, A. cGMP: A unique 2nd messenger molecule—Recent developments in cGMP research and development. Naunyn Schmiedebergs Arch. Pharm. 2020, 393, 287–302. [Google Scholar] [CrossRef]
- Publication Committee for the VMAC Investigators. Intravenous nesiritide vs nitroglycerin for treatment of decompensated congestive heart failure: A randomized controlled trial. JAMA 2002, 287, 1531–1540. [Google Scholar]
- Hayashi, M.; Tsutamoto, T.; Wada, A.; Maeda, K.; Mabuchi, N.; Tsutsui, T.; Horie, H.; Ohnishi, M.; Kinoshita, M. Intravenous atrial natriuretic peptide prevents left ventricular remodeling in patients with first anterior acute myocardial infarction. J. Am. Coll. Cardiol. 2001, 37, 1820–1826. [Google Scholar] [CrossRef][Green Version]
- Mohammed, S.F.; Korinek, J.; Chen, H.H.; Burnett, J.C.; Redfield, M.M. Nesiritide in acute decompensated heart failure: Current status and future perspectives. Rev. Cardiovasc Med. 2008, 9, 151–158. [Google Scholar] [PubMed]
- Nomura, F.; Kurobe, N.; Mori, Y.; Hikita, A.; Kawai, M.; Suwa, M.; Okutani, Y. Multicenter prospective investigation on efficacy and safety of carperitide as a first-line drug for acute heart failure syndrome with preserved blood pressure: COMPASS: Carperitide Effects Observed Through Monitoring Dyspnea in Acute Decompensated Heart Failure Study. Circ. J. 2008, 72, 1777–1786. [Google Scholar] [PubMed]
- Hata, N.; Seino, Y.; Tsutamoto, T.; Hiramitsu, S.; Kaneko, N.; Yoshikawa, T.; Yokoyama, H.; Tanaka, K.; Mizuno, K.; Nejima, J.; et al. Effects of carperitide on the long-term prognosis of patients with acute decompensated chronic heart failure: The PROTECT multicenter randomized controlled study. Circ. J. 2008, 72, 1787–1793. [Google Scholar] [CrossRef]
- O’Connor, C.M.; Starling, R.C.; Hernandez, A.F.; Armstrong, P.W.; Dickstein, K.; Hasselblad, V.; Heizer, G.M.; Komajda, M.; Massie, B.M.; McMurray, J.J.V.; et al. Effect of nesiritide in patients with acute decompensated heart failure. N. Engl. J. Med. 2011, 365, 32–43. [Google Scholar] [CrossRef]
- Kittleson, M.M. Nesiritide and Me. Circ. Heart Fail. 2018, 11, e005440. [Google Scholar] [CrossRef]
- McMurray, J.J.; Packer, M.; Desai, A.S.; Gong, J.; Lefkowitz, M.P.; Rizkala, A.R.; Rouleau, J.L.; Shi, V.C.; Solomon, S.D.; Swedberg, K.; et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N. Engl. J. Med. 2014, 371, 993–1004. [Google Scholar] [CrossRef]
- Drucker, D.J. Advances in oral peptide therapeutics. Nat. Rev. Drug Discov. 2020, 19, 277–289. [Google Scholar] [CrossRef]
- Schweitz, H.; Vigne, P.; Moinier, D.; Frelin, C.; Lazdunski, M. A new member of the natriuretic peptide family is present in the venom of the green mamba (Dendroaspis angusticeps). J. Biol. Chem. 1992, 267, 13928–13932. [Google Scholar] [CrossRef]
- Lisy, O.; Huntley, B.K.; McCormick, D.J.; Kurlansky, P.A.; Burnett, J.C., Jr. Design, synthesis, and actions of a novel chimeric natriuretic peptide: CD-NP. J. Am. Coll. Cardiol. 2008, 52, 60–68. [Google Scholar] [CrossRef]
- Martin, F.L.; Sangaralingham, S.J.; Huntley, B.K.; McKie, P.M.; Ichiki, T.; Chen, H.H.; Korinek, J.; Harders, G.E.; Burnett, J.C., Jr. CD-NP: A novel engineered dual guanylyl cyclase activator with anti-fibrotic actions in the heart. PLoS ONE 2012, 7, e52422. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ichiki, T.; Schirger, J.A.; Huntley, B.K.; Brozovich, F.V.; Maleszewski, J.J.; Sandberg, S.M.; Sangaralingham, S.J.; Park, S.J.; Burnett, J.C., Jr. Cardiac fibrosis in end-stage human heart failure and the cardiac natriuretic peptide guanylyl cyclase system: Regulation and therapeutic implications. J. Mol. Cell. Cardiol. 2014, 75, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.Y.; Chen, H.H.; Lisy, O.; Swan, S.; Cannon, C.; Lieu, H.D.; Burnett, J.C., Jr. Pharmacodynamics of a novel designer natriuretic peptide, CD-NP, in a first-in-human clinical trial in healthy subjects. J. Clin. Pharm. 2009, 49, 668–673. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, R.; Lee, C.Y.W.; Scott, C.; Bailey, K.R.; Schirger, J.A.; Chen, H.H.; Benike, S.L.; Cannone, V.; Martin, F.L.; Sangaralingham, S.J.; et al. A Human Study to Evaluate Safety, Tolerability, and Cyclic GMP Activating Properties of Cenderitide in Subjects With Stable Chronic Heart Failure. Clin. Pharm. 2018, 104, 546–552. [Google Scholar] [CrossRef]
- Ichiki, T.; Schirger, J.A.; Wanek, J.R.; Heublein, D.M.; Scott, C.G.; Sangaralingham, S.J.; Chen, H.H.; Burnett, J.C. Cardiorenal protection by subcutaneous cenderitide in experimental heart failure: A novel and safe therapeutic for humans with LVAD support. Eur. Heart J. 2018, 39, 1391–1392. [Google Scholar] [CrossRef]
- Ichiki, T.; Schirger, J.; Wanek, J.R.; Scott, C.; Sangaralingham, J.; Chen, H.H.; Burnett, J. Cenderitide: A Novel Therapeutic to Increase Endogenous Cardiac Natriuretic Peptides in Heart Failure. J. Am. Coll. Cardiol. 2020, 75, 788. [Google Scholar] [CrossRef]
- Cataliotti, A.; Costello-Boerrigter, L.C.; Chen, H.H.; Textor, S.C.; Burnett, J.C., Jr. Sustained blood pressure-lowering actions of subcutaneous B-type natriuretic peptide (nesiritide) in a patient with uncontrolled hypertension. Mayo Clin. Proc. 2012, 87, 413–415. [Google Scholar] [CrossRef]
- Macheret, F.; Heublein, D.; Costello-Boerrigter, L.C.; Boerrigter, G.; McKie, P.; Bellavia, D.; Mangiafico, S.; Ikeda, Y.; Bailey, K.; Scott, C.G.; et al. Human hypertension is characterized by a lack of activation of the antihypertensive cardiac hormones ANP and BNP. J. Am. Coll. Cardiol. 2012, 60, 1558–1565. [Google Scholar] [CrossRef]
- Crozier, I.G.; Nicholls, M.G.; Ikram, H.; Espiner, E.A.; Yandle, T.G. Plasma immunoreactive atrial natriuretic peptide levels after subcutaneous alpha-hANP injection in normal humans. J. Cardiovasc. Pharm. 1987, 10, 72–75. [Google Scholar] [CrossRef]
- Hodgson-Zingman, D.M.; Karst, M.L.; Zingman, L.V.; Heublein, D.M.; Darbar, D.; Herron, K.J.; Ballew, J.D.; de Andrade, M.; Burnett, J.C., Jr.; Olson, T.M. Atrial natriuretic peptide frameshift mutation in familial atrial fibrillation. N. Engl. J. Med. 2008, 359, 158–165. [Google Scholar] [CrossRef]
- McKie, P.M.; Cataliotti, A.; Huntley, B.K.; Martin, F.L.; Olson, T.M.; Burnett, J.C., Jr. A human atrial natriuretic peptide gene mutation reveals a novel peptide with enhanced blood pressure-lowering, renal-enhancing, and aldosterone-suppressing actions. J. Am. Coll. Cardiol. 2009, 54, 1024–1032. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Schaefer, J.J.; Iyer, S.R.; Harders, G.E.; Pan, S.; Sangaralingham, S.J.; Chen, H.H.; Redfield, M.M.; Burnett, J.C., Jr. Long-term blood pressure lowering and cGMP-activating actions of the novel ANP analog MANP. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2020, 318, R669–R676. [Google Scholar] [CrossRef] [PubMed]
- Dzhoyashvili, N.A.; Iyer, S.R.; Chen, H.H.; Burnett, J.C. MANP (M-Atrial Natriuretic Peptide) Reduces Blood Pressure and Furosemide-Induced Increase in Aldosterone in Hypertension. Hypertension 2022, 79, 750–760. [Google Scholar] [CrossRef] [PubMed]
- Dickey, D.M.; Yoder, A.R.; Potter, L.R. A familial mutation renders atrial natriuretic Peptide resistant to proteolytic degradation. J. Biol. Chem. 2009, 284, 19196–19202. [Google Scholar] [CrossRef] [PubMed]
- McKie, P.M.; Cataliotti, A.; Boerrigter, G.; Chen, H.H.; Sangaralingham, S.J.; Martin, F.L.; Ichiki, T.; Burnett, J.C., Jr. A novel atrial natriuretic peptide based therapeutic in experimental angiotensin II mediated acute hypertension. Hypertension 2010, 56, 1152–1159. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.H.; Wan, S.H.; Iyer, S.R.; Cannone, V.; Sangaralingham, S.J.; Nuetel, J.; Burnett, J.C., Jr. First-in-Human Study of MANP: A Novel ANP (Atrial Natriuretic Peptide) Analog in Human Hypertension. Hypertension 2021, 78, 1859–1867. [Google Scholar] [CrossRef]
- Pan, S.; Chen, H.H.; Dickey, D.M.; Boerrigter, G.; Lee, C.; Kleppe, L.S.; Hall, J.L.; Lerman, A.; Redfield, M.M.; Potter, L.R.; et al. Biodesign of a renal-protective peptide based on alternative splicing of B-type natriuretic peptide. Proc. Natl. Acad. Sci. USA 2009, 106, 11282–11287. [Google Scholar] [CrossRef]
- Meems, L.M.G.; Burnett, J.C., Jr. Innovative Therapeutics: Designer Natriuretic Peptides. JACC Basic Transl. Sci. 2016, 1, 557–567. [Google Scholar] [CrossRef]
- Chen, Y.; Harty, G.J.; Huntley, B.K.; Iyer, S.R.; Heublein, D.M.; Harders, G.E.; Meems, L.; Pan, S.; Sangaralingham, S.J.; Ichiki, T.; et al. CRRL269: A novel designer and renal-enhancing pGC-A peptide activator. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2018, 314, R407–R414. [Google Scholar] [CrossRef]
- Chen, Y.; Harty, G.J.; Zheng, Y.; Iyer, S.R.; Sugihara, S.; Sangaralingham, S.J.; Ichiki, T.; Grande, J.P.; Lee, H.C.; Wang, X.; et al. Crrl269. Circ. Res. 2019, 124, 1462–1472. [Google Scholar] [CrossRef]
- Lorget, F.; Kaci, N.; Peng, J.; Benoist-Lasselin, C.; Mugniery, E.; Oppeneer, T.; Wendt, D.J.; Bell, S.M.; Bullens, S.; Bunting, S.; et al. Evaluation of the therapeutic potential of a CNP analog in a Fgfr3 mouse model recapitulating achondroplasia. Am. J. Hum. Genet. 2012, 91, 1108–1114. [Google Scholar] [CrossRef] [PubMed]
- Rousseau, F.; Bonaventure, J.; Legeai-Mallet, L.; Pelet, A.; Rozet, J.M.; Maroteaux, P.; Le Merrer, M.; Munnich, A. Mutations in the gene encoding fibroblast growth factor receptor-3 in achondroplasia. Nature 1994, 371, 252–254. [Google Scholar] [CrossRef] [PubMed]
- Wendt, D.J.; Dvorak-Ewell, M.; Bullens, S.; Lorget, F.; Bell, S.M.; Peng, J.; Castillo, S.; Aoyagi-Scharber, M.; O’Neill, C.A.; Krejci, P.; et al. Neutral Endopeptidase-Resistant C-Type Natriuretic Peptide Variant Represents a New Therapeutic Approach for Treatment of Fibroblast Growth Factor Receptor 3-Related Dwarfism. J. Pharm. Exp. Ther. 2015, 353, 132–149. [Google Scholar] [CrossRef] [PubMed]
- Savarirayan, R.; Irving, M.; Bacino, C.A.; Bostwick, B.; Charrow, J.; Cormier-Daire, V.; Le Quan Sang, K.H.; Dickson, P.; Harmatz, P.; Phillips, J.; et al. C-Type Natriuretic Peptide Analogue Therapy in Children with Achondroplasia. N. Engl. J. Med. 2019, 381, 25–35. [Google Scholar] [CrossRef]
- Savarirayan, R.; Tofts, L.; Irving, M.; Wilcox, W.; Bacino, C.A.; Hoover-Fong, J.; Ullot Font, R.; Harmatz, P.; Rutsch, F.; Bober, M.B.; et al. Once-daily, subcutaneous vosoritide therapy in children with achondroplasia: A randomised, double-blind, phase 3, placebo-controlled, multicentre trial. Lancet 2020, 396, 684–692. [Google Scholar] [CrossRef]
- Breinholt, V.M.; Rasmussen, C.E.; Mygind, P.H.; Kjelgaard-Hansen, M.; Faltinger, F.; Bernhard, A.; Zettler, J.; Hersel, U. TransCon CNP, a Sustained-Release C-Type Natriuretic Peptide Prodrug, a Potentially Safe and Efficacious New Therapeutic Modality for the Treatment of Comorbidities Associated with Fibroblast Growth Factor Receptor 3-Related Skeletal Dysplasias. J. Pharm. Exp. Ther. 2019, 370, 459–471. [Google Scholar] [CrossRef]
- Patel, V.B.; Zhong, J.C.; Grant, M.B.; Oudit, G.Y. Role of the ACE2/Angiotensin 1-7 Axis of the Renin-Angiotensin System in Heart Failure. Circ. Res. 2016, 118, 1313–1326. [Google Scholar] [CrossRef]
- Meems, L.M.G.; Andersen, I.A.; Pan, S.; Harty, G.; Chen, Y.; Zheng, Y.; Harders, G.E.; Ichiki, T.; Heublein, D.M.; Iyer, S.R.; et al. Design, Synthesis, and Actions of an Innovative Bispecific Designer Peptide. Hypertension 2019, 73, 900–909. [Google Scholar] [CrossRef]
- Nass, R.M.; Gaylinn, B.D.; Rogol, A.D.; Thorner, M.O. Ghrelin and growth hormone: Story in reverse. Proc. Natl. Acad. Sci. USA 2010, 107, 8501–8502. [Google Scholar] [CrossRef]
- Morozumi, N.; Yotsumoto, T.; Yamaki, A.; Yoshikiyo, K.; Yoshida, S.; Nakamura, R.; Jindo, T.; Furuya, M.; Maeda, H.; Minamitake, Y.; et al. ASB20123: A novel C-type natriuretic peptide derivative for treatment of growth failure and dwarfism. PLoS ONE 2019, 14, e0212680. [Google Scholar] [CrossRef]
- Yotsumoto, T.; Morozumi, N.; Nakamura, R.; Jindo, T.; Furuya, M.; Abe, Y.; Nishimura, T.; Maeda, H.; Ogasawara, H.; Minamitake, Y.; et al. Safety assessment of a novel C-type natriuretic peptide derivative and the mechanism of bone- and cartilage-specific toxicity. PLoS ONE 2019, 14, e0218229. [Google Scholar] [CrossRef] [PubMed]
- Cataliotti, A.; Schirger, J.A.; Martin, F.L.; Chen, H.H.; McKie, P.M.; Boerrigter, G.; Costello-Boerrigter, L.C.; Harty, G.; Heublein, D.M.; Sandberg, S.M.; et al. Oral human brain natriuretic peptide activates cyclic guanosine 3’,5’-monophosphate and decreases mean arterial pressure. Circulation 2005, 112, 836–840. [Google Scholar] [CrossRef] [PubMed]
- Halberg, I.B.; Lyby, K.; Wassermann, K.; Heise, T.; Zijlstra, E.; Plum-Morschel, L. Efficacy and safety of oral basal insulin versus subcutaneous insulin glargine in type 2 diabetes: A randomised, double-blind, phase 2 trial. Lancet Diabetes Endocrinol. 2019, 7, 179–188. [Google Scholar] [CrossRef]
- Januzzi, J.L., Jr.; Prescott, M.F.; Butler, J.; Felker, G.M.; Maisel, A.S.; McCague, K.; Camacho, A.; Pina, I.L.; Rocha, R.A.; Shah, A.M.; et al. Association of Change in N-Terminal Pro-B-Type Natriuretic Peptide Following Initiation of Sacubitril-Valsartan Treatment With Cardiac Structure and Function in Patients With Heart Failure With Reduced Ejection Fraction. JAMA 2019, 322, 1085–1095. [Google Scholar] [CrossRef] [PubMed]
- Murphy, S.P.; Prescott, M.F.; Camacho, A.; Iyer, S.R.; Maisel, A.S.; Felker, G.M.; Butler, J.; Pina, I.L.; Ibrahim, N.E.; Abbas, C.; et al. Atrial Natriuretic Peptide and Treatment With Sacubitril/Valsartan in Heart Failure With Reduced Ejection Fraction. JACC Heart Fail. 2021, 9, 127–136. [Google Scholar] [CrossRef]
- Solomon, S.D.; McMurray, J.J.V.; Anand, I.S.; Ge, J.; Lam, C.S.P.; Maggioni, A.P.; Martinez, F.; Packer, M.; Pfeffer, M.A.; Pieske, B.; et al. Angiotensin-Neprilysin Inhibition in Heart Failure with Preserved Ejection Fraction. N. Engl. J. Med. 2019, 381, 1609–1620. [Google Scholar] [CrossRef]
- Solomon, S.D.; Vaduganathan, M.L.; Claggett, B.; Packer, M.; Zile, M.; Swedberg, K.; Rouleau, J.A.; Pfeffer, M.; Desai, A.; Lund, L.H.; et al. Sacubitril/Valsartan Across the Spectrum of Ejection Fraction in Heart Failure. Circulation 2020, 141, 352–361. [Google Scholar] [CrossRef]
- Docherty, K.F.; Vaduganathan, M.; Solomon, S.D.; McMurray, J.J.V. Sacubitril/Valsartan: Neprilysin Inhibition 5 Years After PARADIGM-HF. JACC Heart Fail. 2020, 8, 800–810. [Google Scholar] [CrossRef]
- Iwaki, T.; Oyama, Y.; Tomoo, T.; Tanaka, T.; Okamura, Y.; Sugiyama, M.; Yamaki, A.; Furuya, M. Discovery and dimeric approach of novel Natriuretic Peptide Receptor A (NPR-A) agonists. Bioorg. Med. Chem. 2017, 25, 1762–1769. [Google Scholar] [CrossRef]
- Iwaki, T.; Nakamura, Y.; Tanaka, T.; Ogawa, Y.; Iwamoto, O.; Okamura, Y.; Kawase, Y.; Furuya, M.; Oyama, Y.; Nagayama, T. Discovery and SAR of a novel series of Natriuretic Peptide Receptor-A (NPR-A) agonists. Bioorg. Med. Chem. Lett. 2017, 27, 4904–4907. [Google Scholar] [CrossRef]
- Iwaki, T.; Tanaka, T.; Miyazaki, K.; Suzuki, Y.; Okamura, Y.; Yamaki, A.; Iwanami, M.; Morozumi, N.; Furuya, M.; Oyama, Y. Discovery and in vivo effects of novel human natriuretic peptide receptor A (NPR-A) agonists with improved activity for rat NPR-A. Bioorg. Med. Chem. 2017, 25, 6680–6694. [Google Scholar] [CrossRef] [PubMed]
- Sangaralingham, S.J.; Whig, K.; Peddibhotla, S.; Kirby, R.J.; Sessions, H.E.; Maloney, P.R.; Hershberger, P.M.; Mose-Yates, H.; Hood, B.L.; Vasile, S.; et al. Discovery of small molecule guanylyl cyclase A receptor positive allosteric modulators. Proc. Natl. Acad. Sci. USA 2021, 118, e2109386118. [Google Scholar] [CrossRef] [PubMed]
- Macheret, F.; Boerrigter, G.; McKie, P.; Costello-Boerrigter, L.; Lahr, B.; Heublein, D.; Sandberg, S.; Ikeda, Y.; Cataliotti, A.; Bailey, K.; et al. Pro-B-type natriuretic peptide(1-108) circulates in the general community: Plasma determinants and detection of left ventricular dysfunction. J. Am. Coll. Cardiol. 2011, 57, 1386–1395. [Google Scholar] [CrossRef] [PubMed]
- Buglioni, A.; Cannone, V.; Cataliotti, A.; Sangaralingham, S.J.; Heublein, D.M.; Scott, C.G.; Bailey, K.R.; Rodeheffer, R.J.; Dessi-Fulgheri, P.; Sarzani, R.; et al. Circulating aldosterone and natriuretic peptides in the general community: Relationship to cardiorenal and metabolic disease. Hypertension 2015, 65, 45–53. [Google Scholar] [CrossRef]
- Asferg, C.L.; Nielsen, S.J.; Andersen, U.B.; Linneberg, A.; Moller, D.V.; Hedley, P.L.; Christiansen, M.; Goetze, J.P.; Esler, M.; Jeppesen, J.L. Relative atrial natriuretic peptide deficiency and inadequate renin and angiotensin II suppression in obese hypertensive men. Hypertension 2013, 62, 147–153. [Google Scholar] [CrossRef]
- Reginauld, S.H.; Cannone, V.; Iyer, S.; Scott, C.; Bailey, K.; Schaefer, J.; Chen, Y.; Sangaralingham, S.J.; Burnett, J.C., Jr. Differential Regulation of ANP and BNP in Acute Decompensated Heart Failure: Deficiency of ANP. JACC Heart Fail. 2019, 7, 891–898. [Google Scholar] [CrossRef]
- Bachmann, K.N.; Gupta, D.K.; Xu, M.; Brittain, E.; Farber-Eger, E.; Arora, P.; Collins, S.; Wells, Q.S.; Wang, T.J. Unexpectedly Low Natriuretic Peptide Levels in Patients With Heart Failure. JACC Heart Fail. 2021, 9, 192–200. [Google Scholar] [CrossRef]
- DiMasi, J.A.; Grabowski, H.G.; Hansen, R.W. Innovation in the pharmaceutical industry: New estimates of R&D costs. J. Health Econ. 2016, 47, 20–33. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ichiki, T.; Jinno, A.; Tsuji, Y. Natriuretic Peptide-Based Novel Therapeutics: Long Journeys of Drug Developments Optimized for Disease States. Biology 2022, 11, 859. https://doi.org/10.3390/biology11060859
Ichiki T, Jinno A, Tsuji Y. Natriuretic Peptide-Based Novel Therapeutics: Long Journeys of Drug Developments Optimized for Disease States. Biology. 2022; 11(6):859. https://doi.org/10.3390/biology11060859
Chicago/Turabian StyleIchiki, Tomoko, Atsushi Jinno, and Yoshihisa Tsuji. 2022. "Natriuretic Peptide-Based Novel Therapeutics: Long Journeys of Drug Developments Optimized for Disease States" Biology 11, no. 6: 859. https://doi.org/10.3390/biology11060859
APA StyleIchiki, T., Jinno, A., & Tsuji, Y. (2022). Natriuretic Peptide-Based Novel Therapeutics: Long Journeys of Drug Developments Optimized for Disease States. Biology, 11(6), 859. https://doi.org/10.3390/biology11060859





