Management of Teeth Affected by Molar Incisor Hypomineralization Using a Resin Infiltration Technique—A Systematic Review
Abstract
1. Introduction
1.1. MIH
1.2. ICON
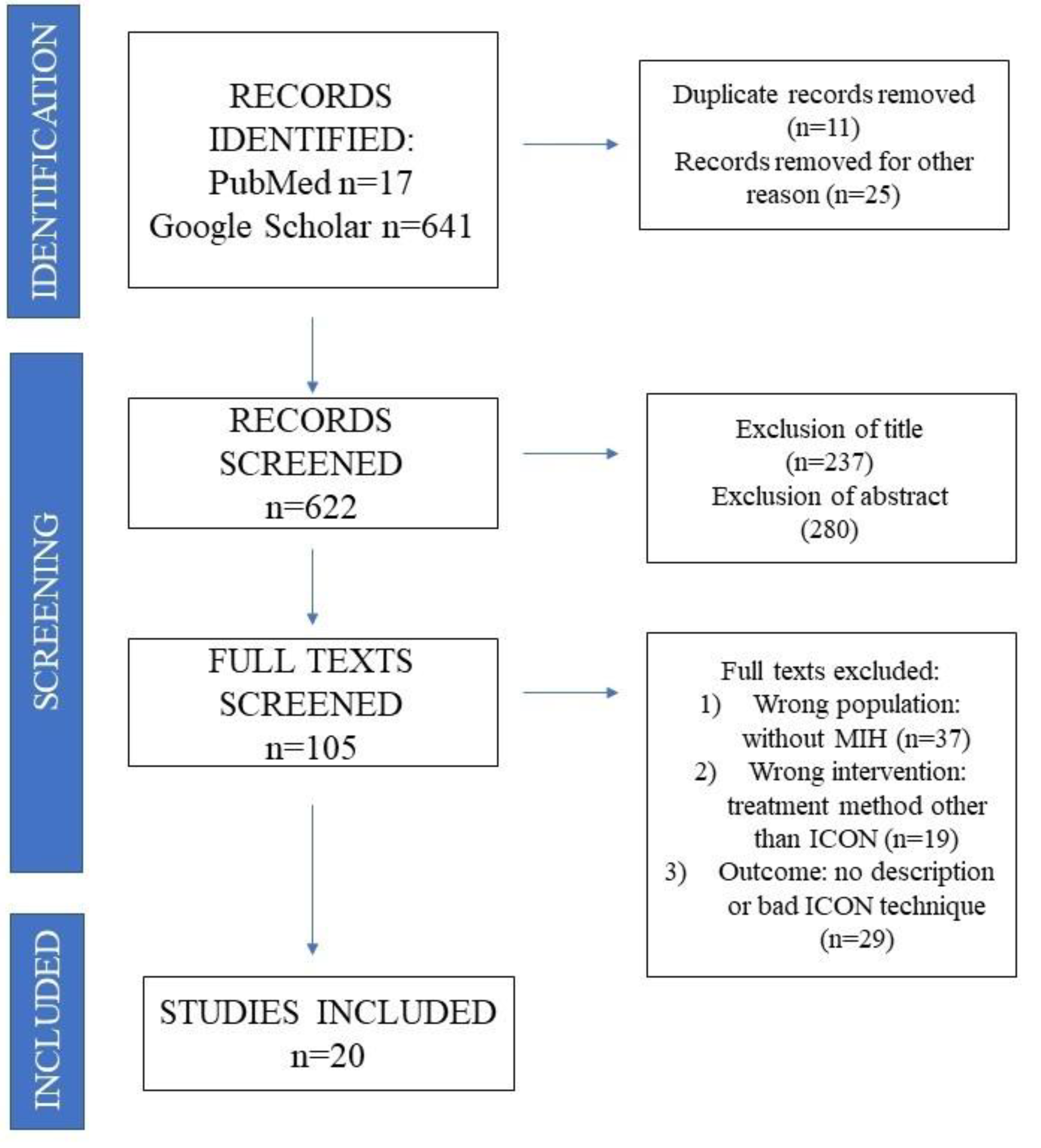
2. Materials and Methods
2.1. Protocol Registration
2.2. Data Sources and Search Strategy
2.3. Eligibility Criteria
- The research group consisted of children and adults with molar incisor hypomineralization, with visible hypomineralization of the front teeth. Research papers describing the early stages of MIH with different etiology were rejected.
- The basic criterium for inclusion in the review was the use of the minimally invasive ICON system for the treatment of hypomineralization. Other descriptions of treatment methods were rejected.
- The research work papers included randomized clinical trials (RCTs), observational studies, cohort research, retrospectives, and case reports. Only publications in English were included for the review.
- Articles describing use of the ICON system have been included in the research.
2.4. Study Selection
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schwendicke, F.; Elhennawy, K.; Reda, S.; Bekes, K.; Manton, D.; Krois, J. Global burden of molar incisor hypomineralization. J. Dent. 2018, 68, 10–18. [Google Scholar] [CrossRef]
- Garot, E.; Denis, A.; Delbos, Y.; Manton, D.; Silva, M.; Rouas, P. Are hypomineralised lesions on second primary molars (HSPM) a predictive sign of molar incisor hypomineralisation (MIH)? A systematic review and a meta-analysis. J. Dent. 2018, 72, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Dong, B.; Yu, D.; Ren, Q.; Sun, Y. The prevalence of molar incisor hypomineralization: Evidence from 70 studies. Int. J. Paediatr. Dent. 2018, 28, 170–179. [Google Scholar] [CrossRef] [PubMed]
- Cury, J.A.; Tenuta, L.M. Enamel remineralization: Controlling the caries disease or treating early caries lesions? Braz. Oral. Res. 2009, 23, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Steffen, R.; Krämer, N.; Bekes, K. The Würzburg MIH concept: The MIH treatment need index (MIH TNI). Eur. Arch. Paediatr. Dent. 2017, 18, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Eckstein, A.; Helms, H.J.; Knösel, M. Camouflage effects following resin infiltration of postorthodontic white-spot lesions in vivo: One-year follow-up. Angle Orthod. 2015, 85, 374–380. [Google Scholar] [CrossRef]
- Gençer, M.D.G.; Kirzioğlu, Z. A comparison of the effectiveness of resin infiltration and microabrasion treatments applied to developmental enamel defects in color masking. Dent. Mater. J. 2019, 31, 295–302. [Google Scholar] [CrossRef]
- Cazzolla, A.P.; De Franco, A.R.; Lacaita, M.; Lacarbonara, V. Efficacy of 4-year treatment of icon infiltration resin on postorthodontic white spot lesions. BMJ Case Rep. 2018, 18, 2018bcr2018225639. [Google Scholar] [CrossRef]
- Mabrouk, R.; Yahia, S.; Oueslati, A.; Frih, N. Erosion Infiltration in the Management of Molar-Incisor Hypomineralization (MIH) Defects. Case Rep. Dent. 2020, 2020, 8888256. [Google Scholar] [CrossRef]
- Amir-Behghadami, M.; Janati, A. Population, intervention, comparison, outcomes and study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg. Med. J. 2020, 37, 387. [Google Scholar] [CrossRef]
- Krämer, N.; Khac, N.B.; Lücker, S.; Stachniss, V.; Frankenberger, F. Bonding strategies for MIH-affected enamel and dentin. Dent. Mater. 2018, 34, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, V.; Soares, I.; Bullio Fragelli, C.; Boldieri, T.; Manton, D.; Bussaneli, D.; Corceiro, R. Structural integrity of MIH-affected teeth after treatment with fluoride varnish or resin infiltration: An 18-Month randomized clinical trial. J. Dent. 2021, 2021, 105103570. [Google Scholar] [CrossRef] [PubMed]
- Mazur, M.; Westland, S.; Guerra, F.; Corridore, D.; Vichi, M.; Maruotti, A.; Nardi, G.M.; Ottolenghi, L. Objective and subjective aesthetic performance of icon® treatment for enamel hypomineralization lesions in young adolescents: A retrospective single center study. J. Dent. 2018, 68, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Marouane, O.; Manton, D. The influence of lesion characteristics on application time of an infiltrate applied to MIH lesions on anterior teeth: An exploratory in vivo pilot study. J. Dent. 2021, 115, 103814. [Google Scholar] [CrossRef]
- Giannetti, L.; Murri Dello Diago, A.; Corciolani, E.; Spinas, E. Deep infiltration for the treatment of hypomineralized enamel lesions in a patient with molar incisor hypomineralization: A clinical case. J. Biol. Regul. Homeost. Agents. 2018, 32, 751–754. [Google Scholar]
- Crombie, F.; Manton, D.; Palamara, J.; Reynolds, E. Resin infiltration of developmentally hypomineralised enamel. Int. J. Paediatr. Dent. 2014, 24, 51–55. [Google Scholar] [CrossRef]
- De Oliveira Farias, J.; Alves Cunha, M.C.; Martins, V.L.; Mathias, P. Microinvasive esthetic approach for deep enamel white spot lesion. Dent. Res. J. 2022, 21, 1929. [Google Scholar]
- Murri Dello Diago, A.; Cadenaro, M.; Ricchiuto, R.; Banchelli, F.; Spinas, E.; Checchi, V.; Giannetti, L. Hypersensitivity in molar incisor hypomineralization: Superficial infiltration treatment. Appl. Sci. 2021, 11, 1823. [Google Scholar] [CrossRef]
- ElBaz, G.A.; Mahfouz, S.M. Efficacy of two different treatment modalities on masking white spot lesions in children with molar incisor hypomineralization. Egypt. Dent. J. 2017, 63, 21472154. [Google Scholar]
- Bhandari, R.; Thakur, S.; Singhal, P.; Chauhan, D.; Jayam, C.; Jain, T. Concealment effect of resin infiltration on incisor of grade I molar incisor hypomineralization patients: An in vivo study. J. Conserv. Dent. 2018, 21, 450–454. [Google Scholar] [CrossRef]
- Marouane, O.; Chtioui, F. Transillumination-aided infiltration: A diagnostic concept for treating enamel opacities. J. Esthet. Restor. Dent. 2020, 32, 451–456. [Google Scholar] [CrossRef] [PubMed]
- Marouane, O.; Douki, N.; Chtioui, F. A combined approach for the aesthetic management of stained enamel opacities: External bleaching followed by resin infiltration. J. Esthet. Restor. Dent. 2020, 32, 451–456. [Google Scholar] [CrossRef] [PubMed]
- Prud’homme, T.; Hyon, I.; Trutaud, S.D.; Lopez Cazaux, S. Different applicabilities of the etch–bleach–seal technique for treating opacities on permanent incisor damage by molar incisor hypomineralisation in three young patients. BMJ Case Rep. 2017, 29, bcr2017221442. [Google Scholar] [CrossRef] [PubMed]
- Natarajan, A.K.; Fraser, S.J.; Swain, M.V.; Drummond, B.K.; Gordon, K.C. Raman spectroscopic characterisation of resin-infiltrated hypomineralised enamel. Anal. Bioanal. Chem. 2015, 407, 5661–5671. [Google Scholar] [CrossRef] [PubMed]
- Chay, P.L.; Manton, D.J.; Palamara, J.E.A.P. The effect of resin infiltration and oxidative pre-treatment on microshear bond strength of resin composite to hypomineralised enamel. Int. J. Pediatr. Dent. 2013, 24, 252–267. [Google Scholar] [CrossRef]
- Athayde, G.; Reis, P.; Jorge, R.; Americano, G.; Fidalgo, T.; Mendes Soviero, V. Impact of masking hypomineralization opacities in anterior teeth on the aesthetic perception of children and parents: A randomized controlled clinical trial. J. Dent. 2022, 123, 104168. [Google Scholar] [CrossRef]
- Hasmun, N.; Vettore, M.V.; Lawson, J.A.; Elcock, C.; Zaitoun, H.; Rodd, H.D. Determinants of children’s oral health-related quality of life following aesthetic treatment of enamel opacities. J. Dent. 2020, 98, 103372. [Google Scholar] [CrossRef]
- Singh, A.; Singh, N.; Srivastava, M.; Khan, R.; Kariya, P.; Abdullah, A. Molar incisor hypomineralization: An update. J. Med. Radio. Patho. Sur. 2017, 4, 17–21. [Google Scholar] [CrossRef]
- Gandhi, S.; Crawford, P.; Shellis, P. The use of a ‘bleach-etch-seal’ deproteinization technique on MIH affected enamel. Int. J. Pediatr. Dent. 2012, 22, 427–434. [Google Scholar] [CrossRef]
- Horuztepe, S.A.; Baseren, M. Effect of resin infiltration on the color and microhardness of bleached white-spot lesions in bovine enamel (an in vitro study). J. Esthet. Restor. Dent. 2017, 29, 378–385. [Google Scholar] [CrossRef]
- Leal, S.; Oliveira, T.; Ribeiro, A. Do parents and children perceive molar-incisor hypomineralization as an oral health problem? Int. J. Paediatr. Dent. 2017, 27, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Arslan, S.; Zorba, Y.O.; Atalay, M.; Özcan, S.; Demirbuga, S.; Pala, K.; Percin, D.; Ozer, F. Effect of resin infiltration on enamel surface properties and Streptococcus mutans adhesion to artificial enamel lesions. Dent. Mater. J. 2015, 34, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Jandu, J.; Dzyuba, N.; Barry, S. White enamel lesions in children: Considering caries, chronological and congenital causes and their consequent care. Br. Dent. J. 2021, 230, 523–527. [Google Scholar] [CrossRef] [PubMed]
- Manoharan, V.; Kumar, S.; Arumugam, S.; Anand, V.; Krishnamoorthy, S.; Methippara, J. Is resin infiltration a microinvasive approach to white lesions of calcified tooth atructures?: A systemic review. Int. J. Clin. Pediatr. Dent. 2019, 12, 53–58. [Google Scholar]
- Knösel, M.; Vogel, R.; Sandoval, S. Infiltration of White-Spot-Lesions and developmental enamel defects. Rev. Clin. Periodoncia Implantol. Rehabil. Oral. 2017, 10, 101–106. [Google Scholar] [CrossRef][Green Version]
- Guerra, F.; Mazur, M.; Nardi, G.; Corridore, D.; Pasqualotto, D.; Rinaldo, F.; Ottolenghi, L. Dental hypomineralized enamel resin infiltration. Clinical indications and limits. Senses Sci. 2015, 2, 135–139. [Google Scholar]
- Vanderas, A.P.; Manetas, C.; Koulatzidou, M.; Papagiannoulis, L. Progression of proximal caries in the mixed dentition: A 4-year prospective study. Pediatr. Dent. 2003, 25, 229–234. [Google Scholar]
- Paris, S.; Soviero, V.M.; Seddig, S.; Meyer-Lueckel, H. Penetration depths of an infiltrant into proximal caries lesions in primary molars after different application times in vitro. Int. J. Paediatr. Dent. 2012, 22, 349–355. [Google Scholar] [CrossRef]
- Denis, M.; Atlan, A.; Vennat, E.; Tirlet, G.; Attal, J.P. White defects on enamel: Diagnosis and anatomopathology: Two essential factors for proper treatment (part 1). Int. Orthod. 2013, 11, 139–165. [Google Scholar] [CrossRef]
- Tam, C.P.; Manton, D.J. Esthetic management of incisors affected with molar incisor hypomineralisation. Clin. Dent. Rev. 2021, 5, 6. [Google Scholar] [CrossRef]
- Khanna, R.; Chandra, A.; Singh, R.K. Quantitative evaluation of masking effect of resin infiltration on developmental defects of enamel. Quintessence Int. 2020, 51, 448–455. [Google Scholar] [PubMed]
- Cohn, C. Revolutionizing Minimally Invasive Dentistry with Resin Infiltration. 2.22. Available online: www.oralhealthgroup.com (accessed on 7 January 2022).
- Lagarde, M.; Vennat, E.; Attal, J.P.; Dursun, E. Strategies to optimize bonding of adhesive materials to molar-incisor hypomineralization-affected enamel: A systematic review. Int. J. Paediatr. Dent. 2020, 30, 405–420. [Google Scholar] [CrossRef] [PubMed]
| Publication | Type of Work | Assessed Parameters | Research Group | Findings |
|---|---|---|---|---|
| Kramer, 2018 [11] | In vitro laboratory studies | Assessment of the resin adhesion to hard tissues of a tooth with MIH | 53 freshly extracted human molars and incisors with MIH | ICON can fill porosities of the teeth enamel with MIH but has no impact on the effectiveness of bonding of the enamel with the composite |
| Nogueira, 2021 [12] | Randomized clinical studies | Assessment of the impact of fluoride lacquers or resin infiltration on retaining correct teeth structure affected by MIH | 51 patients aged 6–12 | ICON system had a positive impact on retaining integrity of teeth affected with MIH structure through reduction of risks related to damage caused to enamel |
| Mazur, 2018 [13] | Retrospective research | Assessment of impact of resin infiltration on the aesthetics of teeth with MIH | 76 teeth | Aesthetic effect proved to be highly effective in visual quality and spectrophotometric assessment |
| Marouane, 2021 [14] | Pilot study vivo | Assessment of change of characteristics of resin infiltration over time | Circumscribed MIH lesion with homogenous (14) and non-homogenous appearances (18), patients aged between 10 and 32 years of age | Non-homogeneous lesions require longer application of the infiltrate compared to homogenous lesions |
| Giannetti, 2018 [15] | Monitored clinical research | Assessment of efficiency of superficial infiltration with use of ICON in removal of changes caused by different factors | 17 patients with white cavities of enamel | Cases of MIH should probably be introduced to a more invasive treatment technique |
| Crombie, 2014 [16] | Laboratory research | Research on effectiveness of resin infiltration on lesions in teeth with MIH (with microscope in direction of penetration and with use of SEM microscope) | 21 teeth with lesions similar to characteristics of MIH | Resin infiltration can penetrate changes of enamel with MIH; however, pattern, scope, and change of created hardness are unpredictable |
| Farias, 2022 [17] | Case review | Assessment of effectiveness of ICON system in treatment of lesions with MIH etiology | 20 year old patient with extensive white spots on central incisor | After three sessions of 15% HCI acid erosion, satisfying effect of camouflage of white lesions had been achieved |
| Mabrouk, 2020 [9] | Case review | Assessment of effectiveness of ICON system in treatment of white lesions in enamel with MIH etiology | 29 year old patient with white lesions in enamel on maxillary central incisors | ICON infiltration technique is considered an effective microinvasive procedure in which degree of success is probably achieved due to motivation of patient |
| Diago, 2021 [18] | Cohort research | Research on effectiveness of resin infiltration method in treatment of hypersensitive teeth with MIH | 42 patients aged 8 to 14 with hypersensitivity of minimum on incisor tooth with MIH | Research provides vital and useful initial statistical data and indicates reduction of hypersensitivity in incisor teeth with MIH after only one resin infiltration |
| El-Baz, 2017 [19] | Cohort research | Assessment and comparison of effectiveness of resin infiltration and fluoride lacquer in lesions of MIH etiology (clinical and radiological) | 20 children aged between 9 and 14 | Resin infiltration is significantly better than the fluoride lacquer in masking white spots in children with MIH |
| Bhandari, 2018 [20] | Research in vivo | Assessment of aesthetic treatment results of resin infiltration in incisors with MIH | 22 lesions on incisors | Resin infiltration can mask unaesthetic changes of enamel in teeth with MIH |
| Marouane, 2020 [21] | Case review | Impact of use of transillumination during resin infiltration in aesthetic treatment of white spots with MIH etiology | Patient with opacities of enamel within incisors | Use of transillumination can help in achievement of predictable treatment results with use of ICON system |
| Marouane, 2018 [22] | Case review | Assessment of impact of ICON system after teeth whitening of teeth with discoloration with MIH etiology and traumatic etiology | 3 patients: 1 with discoloration of traumatic etiology and 2 with discoloration of MIH etiology | Removal of discoloration, mottling of enamel with use of external whitening constitute a vital stage of initial preparation for resin infiltration |
| Prud’homme, 2017 [23] | Case review | Use of etch-bleach-seal technique in treatment of lesions with MIH characteristics | 3 patients with yellow-brown lesions in incisors | Combining three techniques “microabrasion/etching/whitening/infiltration ICON” might be useful in treatment of yellow-brown mottling frontal in teeth with MIH. |
| Natarajan, 2015 [24] | Laboratory research in vitro | Assessment of pre-treatment preparation with use of HCI, NaOCl, and H2O2 on depth of penetration of resin infiltrators | 7 molar teeth showing brown mottling, marked without damage to surface of enamel | Pre-treatment preparation helps in deep resin penetration, and MIH part of structure seemed closer to structure of normal enamel |
| Chay, 2013 [25] | Laboratory research in vitro | Research of impact of resin infiltration of ICON on improvement of resin composite adhesion to enamel of teeth with MIH | 152 first permanent molar teeth extracted in children under 18 years old with MIH | Resin infiltration decreases composite bonding to hypomineralized enamel; increased bonding power has been observed in in the initial conditioning of enamel with 5.25% NaOCl, followed by resin infiltration |
| Athayde, 2022 [26] | Randomized controlled clinical trial | Assessment of impact of treatment of restricted opacity in front teeth with use of resin infiltration on aesthetic perceptions in children with MIH (and their parents) | 39 patients aged 8–18 | 15 min resin infiltration can mask opacities in permanent incisors with MIH, bring back aesthetics, and increase self-esteem |
| Hasmun, 2020 [27] | Pilot study | Impact of low invasion aesthetic treatment methods on teeth with MIH on improvement of self-esteem in young patients | 86 children aged 7–16 | After treatment with use of ICON system, self-esteem and social and emotional well-being of patients has increased |
| Singh, 2017 [28] | Cohort research | Assessment of clinical effects of resin infiltration in treatment of hypomineralization of molars and incisors | 12 patients (36 teeth with mild MIH) | Satisfactory aesthetic effect of resin infiltration on treatment of mild hypomineralization of molars and incisors |
| Gandhi, 2012 [29] | Laboratory research | Impact of enamel deproteinization with hypomineralization of molars and incisors (MIH) to sealing resin infiltration | 31 extracted teeth | No difference recorded in treatment with use of prior deproteinization and cases where process has not been performed |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bulanda, S.; Ilczuk-Rypuła, D.; Dybek, A.; Pietraszewska, D.; Skucha-Nowak, M.; Postek-Stefańska, L. Management of Teeth Affected by Molar Incisor Hypomineralization Using a Resin Infiltration Technique—A Systematic Review. Coatings 2022, 12, 964. https://doi.org/10.3390/coatings12070964
Bulanda S, Ilczuk-Rypuła D, Dybek A, Pietraszewska D, Skucha-Nowak M, Postek-Stefańska L. Management of Teeth Affected by Molar Incisor Hypomineralization Using a Resin Infiltration Technique—A Systematic Review. Coatings. 2022; 12(7):964. https://doi.org/10.3390/coatings12070964
Chicago/Turabian StyleBulanda, Sylwia, Danuta Ilczuk-Rypuła, Anna Dybek, Daria Pietraszewska, Małgorzata Skucha-Nowak, and Lidia Postek-Stefańska. 2022. "Management of Teeth Affected by Molar Incisor Hypomineralization Using a Resin Infiltration Technique—A Systematic Review" Coatings 12, no. 7: 964. https://doi.org/10.3390/coatings12070964
APA StyleBulanda, S., Ilczuk-Rypuła, D., Dybek, A., Pietraszewska, D., Skucha-Nowak, M., & Postek-Stefańska, L. (2022). Management of Teeth Affected by Molar Incisor Hypomineralization Using a Resin Infiltration Technique—A Systematic Review. Coatings, 12(7), 964. https://doi.org/10.3390/coatings12070964







