The Use of Autogenous Bone Mixed with a Biphasic Calcium Phosphate in a Maxillary Sinus Floor Elevation Procedure with a 6-Month Healing Time: A Clinical, Radiological, Histological and Histomorphometric Evaluation
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
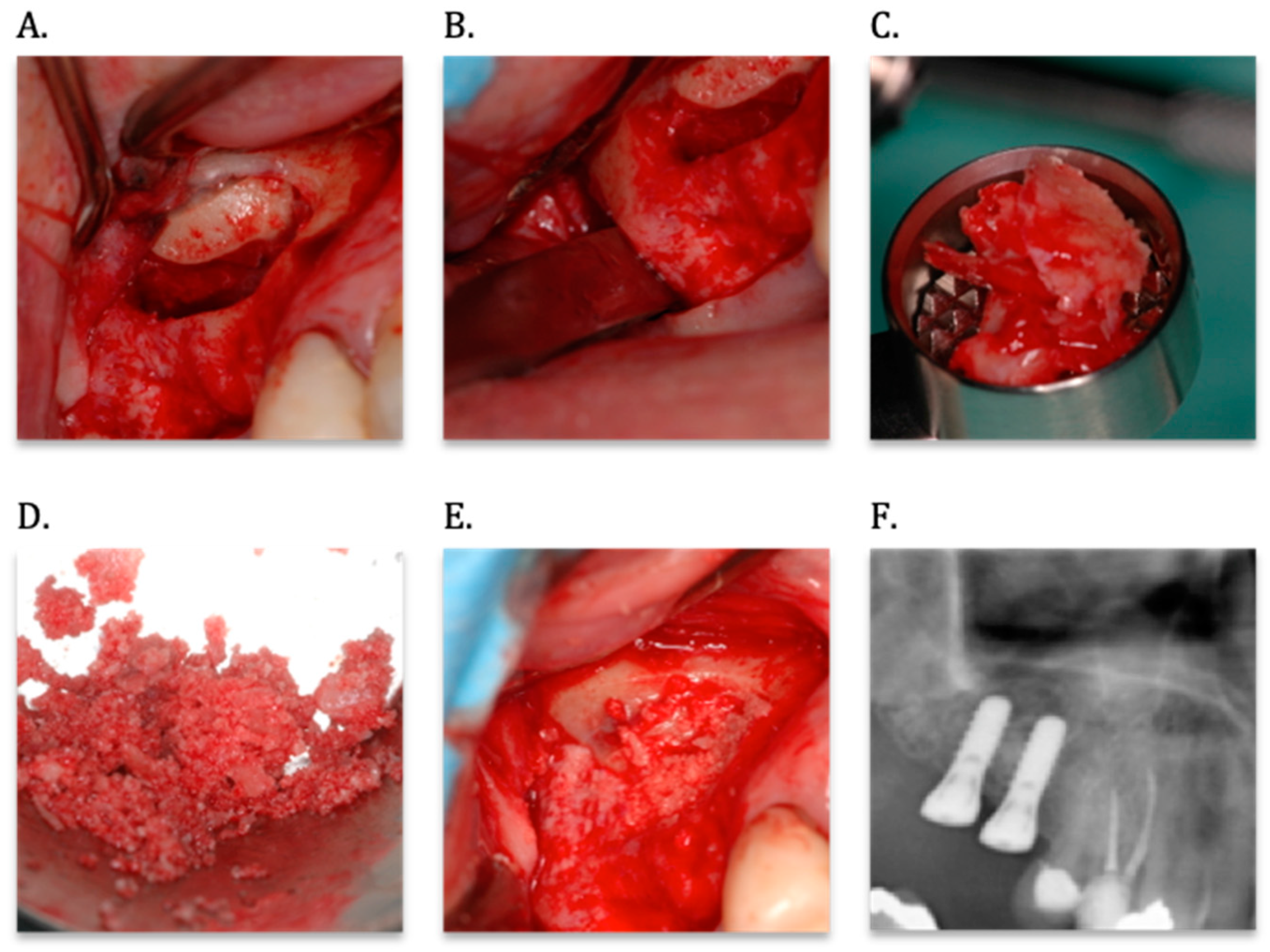
2.2. Maxillary Sinus Floor Elevation Procedure
2.3. Dental Implant Surgery and Biopsy Retrieval
2.4. Clinical Evaluation
2.5. Radiological Evaluation
2.6. Biopsy Processing and Analyses
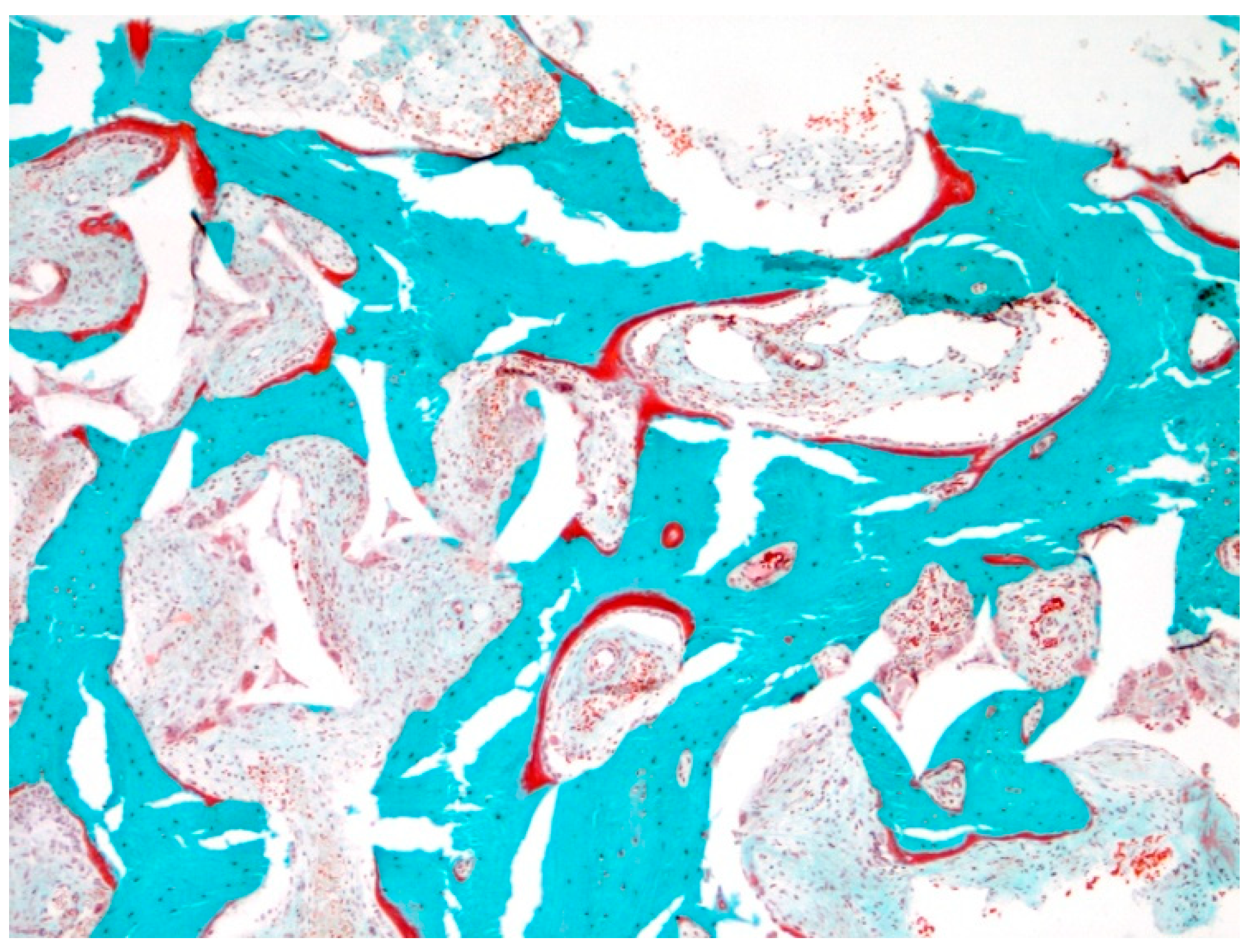
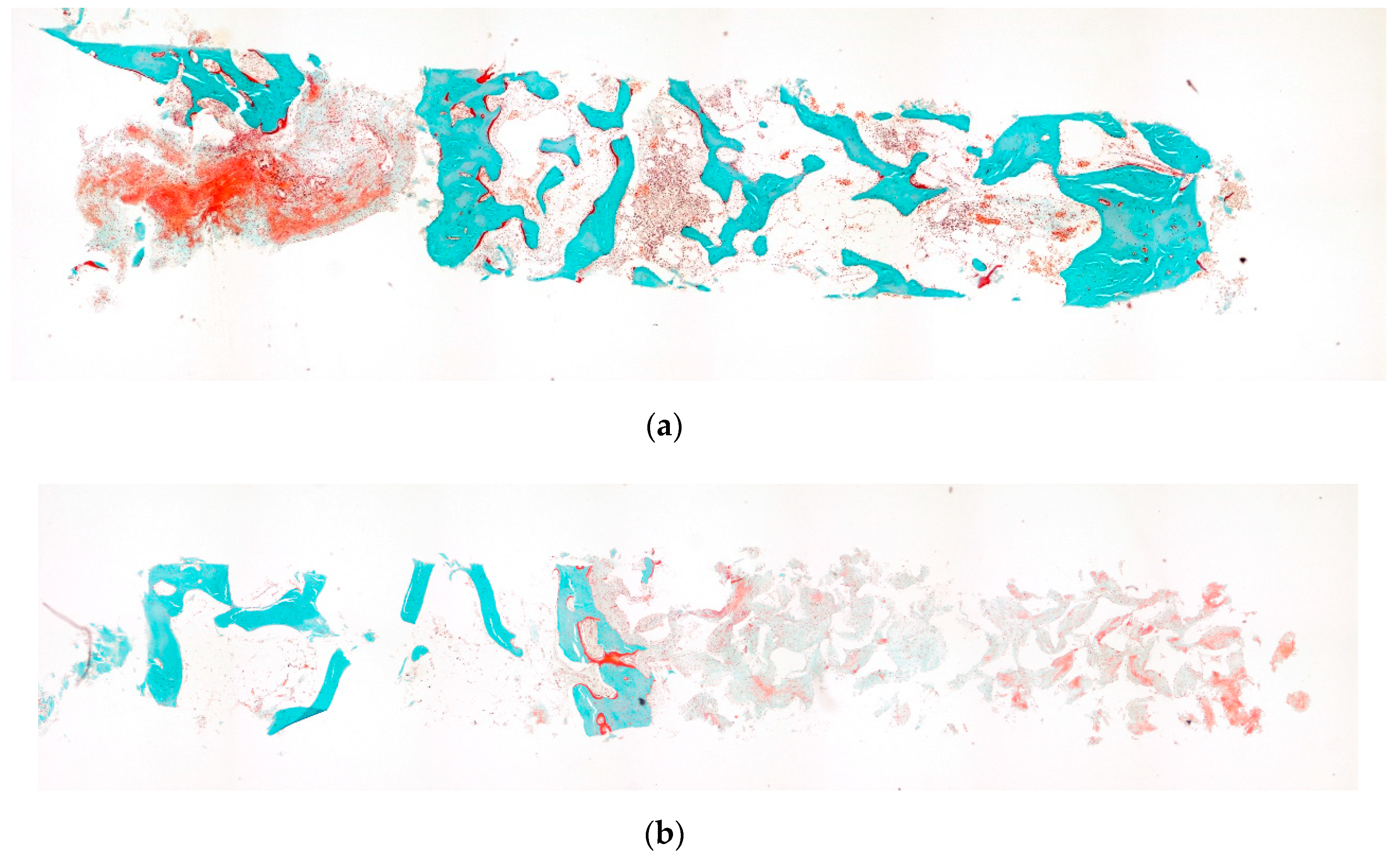
2.7. Qualitative Histological Analysis
2.8. Quantitative Histomorphometric Analysis
- Vital bone volume (BV/TV): percentage of the total section that is vital bone tissue (%).
- Bone surface (BS/TV): BS expressed as a fraction of the total vital bone volume (mm2/mm3).
- Thickness of bone trabeculae (Tb.Th; μm).
- Osteoid volume (OV/BV): percentage of the vital bone tissue section that is osteoid (%).
- Osteoid surface (OS/BS): osteoid-covered surfaces expressed as the percentage of the total BS (%), to measure new vital bone formation.
- Osteoid thickness (O.Th; μm)
- Number of osteoclasts (N.Oc/BPM) per mm2 total area.
2.9. Statistical Analysis
3. Results
3.1. Clinical Evaluation
3.2. Radiological Evaluation
3.3. Qualitative Histological Evaluation
3.4. Quantitative Histomorphometric Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ASBMR | American Society for Bone and Mineral Research |
| BCP | biphasic calcium phosphate |
| BIC | bone-to-implant contact |
| BPM | bone perimeter |
| BV/TV | bone volume/total volume |
| BS/TV | bone surface/total volume |
| C.M.T.B. | Christiaan M. ten Bruggenkate |
| CE | Conformité Européenne |
| HA | hydroxyapatite |
| MSFE | maxillary sinus floor elevation |
| NA | not available |
| N.Oc | number of osteoclasts |
| O.Th | osteoid thickness |
| OS/BS | osteoid surface/bone surface |
| OV/BV | osteoid volume/bone volume |
| SBC | Straumann® Bone Ceramic |
| Tb.Th | trabecular thickness |
| TRAP | tartrate resistant acid phosphate |
| β–TCP | β–tricalcium phosphate |
References
- Boyne, P.J.; James, R.A. Grafting of the maxillary sinus floor with autogenous marrow and bone. J. Oral Surg. 1980, 38, 613–616. [Google Scholar] [PubMed]
- Tatum, H., Jr. Maxillary and sinus implant reconstructions. Dent Clin. N. Am. 1986, 30, 207–229. [Google Scholar] [PubMed]
- Del Fabbro, M.; Rosano, G.; Taschieri, S. Implant survival rates after maxillary sinus augmentation. Eur. J. Oral Sci. 2008, 116, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Tan, W.C.; Zwahlen, M.; Lang, N.P. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. Part, I.; Lateral approach. J. Clin. Periodontol. 2008, 35, 216–240. [Google Scholar] [CrossRef]
- Burchardt, H. The biology of bone graft repair. Clin. Orthop. Relat. Res. 1983, 174, 28–42. [Google Scholar] [CrossRef]
- Jensen, O.T.; Shulman, L.B.; Block, M.S.; Iacono, V.J. Report of the Sinus Consensus Conference of 1996. Int. J. Oral Maxillofac. Implant. 1998, 13, 11–45. [Google Scholar]
- Tong, D.C.; Rioux, K.; Drangsholt, M.; Beirne, O.R. A review of survival rates for implants placed in grafted maxillary sinuses using meta-analysis. Int. J. Oral Maxillofac. Implant. 1998, 13, 175–182. [Google Scholar]
- Van den Bergh, J.P.; ten Bruggenkate, C.M.; Krekeler, G.; Tuinzing, D.B. Sinus floor elevation and grafting with autogenous iliac crest bone. Clin. Oral Implant. Res. 1998, 9, 429–435. [Google Scholar] [CrossRef]
- Klijn, R.J.; Meijer, G.J.; Bronkhorst, E.M.; Jansen, J.A. A meta-analysis of histomorphometric results and graft healing time of various biomaterials compared to autologous bone used as sinus floor augmentation material in humans. Tissue Eng. Part B Rev. 2010, 16, 493–507. [Google Scholar] [CrossRef]
- Misch, C.M. Autogenous Bone: Is It Still the Gold Standard? Implant Dent. 2010, 19, 361. [Google Scholar] [CrossRef]
- Nkenke, E.; Stelzle, F. Clinical outcomes of sinus floor augmentation for implant placement using autogenous bone or bone substitutes: A systematic review. Clin. Oral Implant. Res. 2009, 20 (Suppl. 4), 124–133. [Google Scholar] [CrossRef] [PubMed]
- Frenken, J.W.; Bouwman, W.F.; Bravenboer, N.; Zijderveld, S.A.; Schulten, E.A.J.M. The use of Straumann® Bone Ceramic in a maxillary sinus floor elevation procedure: A clinical radiological histological and histomorphometric evaluation with a 6-month healing period. Clin. Oral Implant. Res. 2010, 21, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Kalk, W.W.; Raghoebar, G.M.; Jansma, J.; Boering, G. Morbidity from iliac crest bone harvesting. Int. J. Oral Maxillofac. Implant. 1996, 54, 1424–1429. [Google Scholar] [CrossRef]
- Raghoebar, G.M.; Louwerse, C.; Kalk, W.W.; Vissink, A. Morbidity of chin bone harvesting. Clin. Oral Implant. Res. 2001, 12, 503–507. [Google Scholar] [CrossRef]
- Zijderveld, S.A.; ten Bruggenkate, C.M.; Van Den Bergh, J.P.; Schulten, E.A.J.M. Fractures of the iliac crest after split-thickness bone grafting for preprosthetic surgery: Report of 3 cases and review of the literature. J. Oral Maxillofac. Surg. 2004, 7, 781–786. [Google Scholar] [CrossRef]
- Beirne, J.C.; Barry, H.J.; Brady, F.A.; Morris, V.B. Donor site morbidity of the anterior iliac crest following cancellous bone harvest. Int. J. Oral Maxillofac. Implant. 1996, 25, 268–271. [Google Scholar] [CrossRef]
- Vermeeren, J.I.J.F.; Wismeijer, D.; Van Waas, M.A.J. One-step reconstruction of the severely resorbed mandible with onlay bone grafts and endosteal implants: A 5-year follow-up. Int. J. Oral Maxillofac. Implant. 1996, 2, 112–115. [Google Scholar] [CrossRef]
- Haugen, H.J.; Lyngstadaas, S.P.; Rossi, F.; Perale, G. Bone grafts: Which is the ideal biomaterial? J. Clin. Periodontol. 2019, 46 (Suppl. 21), 92–102. [Google Scholar] [CrossRef]
- Rothermundt, C.; Whelan, J.; Dileo, P.; Strauss, S.; Coleman, J.; Briggs, T.; Seddon, B. What is the role of routine follow-up forlocalised limb soft tissue sarcomas? A retrospective analysis of 174 patients. Br. J. Cancer 2014, 110, 2420. [Google Scholar] [CrossRef]
- Corbella, S.; Taschieri, S.; Weinstein, R.; Del Fabbro, M. Histomorphometric outcomes after lateral sinus floor elevation procedure: A systematic review of the literature and meta-analysis. Clin. Oral Implant. Res. 2016, 27, 1106–1122. [Google Scholar] [CrossRef]
- De Grado, G.F.; Keller, L.; Idoux-Gillet, Y.; Wagner, Q.; Musset, A.M.; Benkirane-Jessel, N.; Offner, D. Bone substitutes: A review of their characteristics, clinical use, and perspectives for large bone defects management. J. Tissue Eng. 2018, 9. [Google Scholar] [CrossRef]
- Papageorgiou, S.N.; Papageorgiou, P.N.; Deschner, J.; Götz, W. Comparative effectiveness of natural and synthetic bone grafts in oral and maxillofacial surgery prior to insertion of dental implants: Systematic review and network meta-analysis of parallel and cluster randomized controlled trials. J. Dent. 2016, 48, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Bose, S.; Roy, M.; Bandyopadhyay, A. Recent advances in bone tissue engineering scaffolds. Trends Biotechnol. 2012, 30, 546–554. [Google Scholar] [CrossRef] [PubMed]
- El-Rashidy, A.A.; Roether, J.A.; Harhaus, L.; Kneser, U.; Boccaccini, A.R. Regenerating bone with bioactive glass scaffolds: A review of in vivo studies in bone defect models. Acta Biomater. 2017, 1–28. [Google Scholar] [CrossRef]
- Hutmacher, D.W. Scaffolds in Tissue Engineering Bone Andcartilage. The Biomaterials: Silver Jubilee Compendium; Elsevier Science: Oxford, UK, 2006; pp. 175–189. [Google Scholar]
- Janicki, P.; Schmidmaier, G. What should be the characteristics of the ideal bone graft substitute? Combining scaffolds with growth factors and/or stem cells. Injury 2011, S77–S81. [Google Scholar] [CrossRef]
- Jo, S.H.; Kim, Y.K.; Choi, Y.H. Histological Evaluation of the Healing Process of Various Bone Graft Materials after Engraftment into the Human Body. Materials 2018, 11, 714. [Google Scholar] [CrossRef]
- Delloye, C.; Cornu, O.; Druez, V.; Barbier, O. Bone allografts: What they can offer and what they cannot. J. ofBone Joint Surg. Br. Vol. 2007, 89, 574–579. [Google Scholar] [CrossRef]
- Wheeler, D.L.; Enneking, W.F. Allograft bone decreases in strength in vivo over time. Clin. Orthop. Relat. Res. 2005, 36–42. [Google Scholar] [CrossRef]
- Winkler, T.; Sass, F.A.; Duda, G.N.; Schmidt-Bleek, K. A review of biomaterials in bone defect healing, remaining shortcomings and future opportunities for bone tissue engineering THE UNSOLVED CHALLENGE. Bone Jt. Res. 2018, 7, 232–243. [Google Scholar] [CrossRef]
- MDR. Regulation (EU) 2017/745 of The European Parliament and of the Council of 5 April 2017 on Medical devices Retrieved. Available online: http://data.europa.eu/eli/reg/2017/2745/oj (accessed on 5 April 2017).
- Zimmermann, G.; Moghaddam, A. Allograft bone matrix versus synthetic bone graft substitutes. Inj. -Int. Care Inj. 2011, 42, S16–S21. [Google Scholar] [CrossRef]
- Kim, Y.; Nowzari, H.; Rich, S.K. Risk of prion disease transmission through bovine-derived bone substitutes: A systematic review. Clin. Implant Dent. Relat. Res. 2013, 15, 645–653. [Google Scholar] [CrossRef]
- Yamada, M.; Egusa, H. Current bone substitutes for implant dentistry. J. Prosthodont. Res. 2018, 62, 152–161. [Google Scholar] [CrossRef]
- Nery, E.B.; Lee, K.K.; Czajkowski, S.; Dooner, J.J.; Duggan, M.; Ellinger, R.F.; Henkin, J.M.; Hines, R.; Miller, M.; Olson, J.W.; et al. A Veterans Administration Cooperative Study of biphasic calcium phosphate ceramic in periodontal osseous defects. J. Periodontol. 1990, 61, 737–744. [Google Scholar] [CrossRef]
- Zerbo, I.R.; Bronckers, A.L.; de Lange, G.; Burger, E.H. Localisation of osteogenic and osteoclastic cells in porous beta-tricalcium phosphate particles used for human maxillary sinus floor elevation. Biomaterials 2005, 26, 1445–1451. [Google Scholar] [CrossRef] [PubMed]
- Joosten, U.; Joist, A.; Frebel, T.; Walter, M.; Langer, M. The use of an in situ curing hydroxyapatite cement as an alternative to bone graft following removal of enchondroma of the hand. J. Hand Surg. Br. Eur. Vol. 2000, 25, 288–291. [Google Scholar] [CrossRef] [PubMed]
- Costantino, P.D.; Friedman, C.D.; Jones, K.; Chow, L.C.; Pelzer, H.J.; Sisson, G.A. Hydroxyapatite cement: I. Basic chemistry and histologic properties. Arch. Otolaryngol. Head Neck Surg. 1991, 117, 384–397. [Google Scholar] [CrossRef] [PubMed]
- Costantino, P.D.; Friedman, C.D. Synthetic bone graft substitutes. Otolaryngol. Clin. N. Am. 1994, 27, 1037–1074. [Google Scholar]
- Jensen, S.S.; Aaboe, M.; Pinholt, E.M.; Hjorting-Hansen, E.; Melsen, F.; Ruyter, I.E. Tissue reaction and material characteristics of four bone substitutes. Int. J. Oral Maxillofac. Implant. 1996, 11, 55–66. [Google Scholar]
- Daculsi, G.; Laboux, O.; Malard, O.; Weiss, P. Current state of the art of biphasic calcium phosphate bioceramics. J. Mater. Sci. Mater. Med. 2003, 14, 195–200. [Google Scholar] [CrossRef]
- LeGeros, R.Z.; Lin, S.; Rohanizadeh, R.; Mijares, D.; LeGeros, J.P. Biphasic calcium phosphate bioceramics: Preparation properties and applications. J. Mater. Sci. Mater. Med. 2003, 14, 201–209. [Google Scholar] [CrossRef]
- Schopper, C.; Ziya-Ghazvini, F.; Goriwoda, W.; Moser, D.; Wanschitz, F.; Spassova, E.; Lagogiannis, G.; Auterith, A.; Ewers, R. HA/TCP compounding of a porous CaP biomaterial improves bone formation and scaffold degradation—A long-term histological study. J. Biomed. Mater. Res. B Appl. Biomater. 2005, 74, 458–467. [Google Scholar] [CrossRef]
- Zerbo, I.R.; Zijderveld, S.A.; De Boer, A.; Bronckers, A.L.J.J.; De Lange, G.; ten Bruggenkate, C.M.; Burger, E.H. Histomorphometry of human sinus floor augmentation using a porous beta-tricalcium phosphate: A prospective study. Clin. Oral Implant. Res. 2004, 15, 724–732. [Google Scholar] [CrossRef] [PubMed]
- Groeneveld, E.H.; van den Bergh, J.P.; Holzmann, P.; ten Bruggenkate, C.M.; Tuinzing, D.B.; Burger, E.H. Mineralization processes in demineralized bone matrix grafts in human maxillary sinus floor elevations. J. Biomed. Mater. Res. 1999, 48, 393–402. [Google Scholar] [CrossRef]
- Bouwman, W.F.; Bravenboer, N.; Frenken, J.W.F.H.; ten Bruggenkate, C.M.; Schulten, E.A.J.M. The use of a biphasic calcium phosphate in a maxillary sinus floor elevation procedure: A clinical radiological histological and histomorphometric evaluation with 9- and 12-month healing times. Int. J. Implant Dent. 2017, 3, 34. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, S.L. Sinus augmentation for dental implants: The use of alloplastic materials. J. Oral Maxillofac. Surg. 1997, 55, 1287–1293. [Google Scholar] [CrossRef]
- Schulten, E.A.J.M.; Prins, H.J.; Overman, J.R.; Helder, M.N.; ten Bruggenkate, C.M.; Klein-Nuland, J. A novel approach revealing the effect of collagenous membrane on osteoconduction in maxillary sinus floor elevation with β-tricalcium phosphate. Eur. Cells Mater. 2013, 25, 215–228. [Google Scholar] [CrossRef]
- Oostlander, A.E.; Bravenboer, N.; Sohl, E.; Holzmann, P.J. Dutch Initiative on Crohn and Colitis (ICC). Histomorphometric analysis reveals reduced bone mass and bone formation in patients with quiescent Crohn’s disease. Gastroenterology 2011, 140, 116–123. [Google Scholar] [CrossRef]
- Schenk, R.K.; Olah, A.J.; Herrmann, W. Preparation of calcified tissues for light microscopy. In Methods of Calcified Tissue Preparation; Dickson, G.R., Ed.; Elsevier Science Publishers: Amsterdam, The Netherlands, 1983; Volume 1, p. 56. [Google Scholar]
- Romeis, B. Trichromfaerbung nach Goldner Mikroskopische Technik; Urban & Schwarzenberg: Muenchen, Germany, 1989. [Google Scholar]
- Dempster, D.W.; Compston, J.E.; Drezner, M.K.; Glorieux, F.H.; Kanis, J.A.; Malluche, H.; Meunier, P.J.; Ott, S.M.; Recker, R.R.; Parfitt, A.M. Standardized nomenclature symbols and units for bone histomorphometry: A 2012 update of the report of the ASBMR Histomorphometry Nomenclature Committee. J. Bone Miner. Res. 2012. [Google Scholar] [CrossRef]
- Zijderveld, S.A.; Zerbo, I.R.; Van den Bergh, J.P.A.; Schulten, E.A.J.M.; ten Bruggenkate, C.M. Maxillary Sinus Floor Augmentation Using a β–Tricalcium Phosphate (Cerasorb) Alone Compared to Autogenous Bone Grafts. Int. J. Oral Maxillofac. Implant. 2005, 20, 432–440. [Google Scholar]

| Patient (N) | Gender/Age | Implant Site | T0 | T1 | Increase | T2 | T3 | T4 |
|---|---|---|---|---|---|---|---|---|
| 1 | M/53 | 15 | 8.0 | 16.2 | 8.2 | 16.1 | 16.2 | 16.0 |
| 16 | 6.1 | 14.1 | 8.0 | 15.0 | 15.0 | 15.0 | ||
| 2 | M/70 | 16 | 6.8 | 14.8 | 8.0 | 16.0 | 13.7 | 15.6 |
| 17 | 3.6 | 12.4 | 8.8 | 14.0 | 13.3 | 12.1 | ||
| 3 | M/68 | 14 | 5.6 | 11.5 | 5.9 | 12.1 | 11.3 | 10.4 |
| 15 | 4.6 | 14.1 | 9.5 | 14.1 | 13.0 | 12.9 | ||
| 16 | 4.3 | 14.1 | 9.8 | 14.2 | 12.7 | 12.6 | ||
| 4 | F/64 | 15 | 9.3 | 17.1 | 7.8 | 16.8 | 14.1 | 14.0 |
| 16 | 6.0 | 14.9 | 8.9 | 16.9 | 15.8 | 15.7 | ||
| 5 | M/51 | 16 | 9.0 | 18.1 | 9.1 | 17.6 | 16.2 | NA |
| 17 | 5.8 | 18.0 | 12.2 | 16.0 | 16.7 | NA | ||
| Mean | 61.2 | - | 6.3 | 15.0 | 8.7 | 15.3 | 14.4 | 13.8 |
| SD | - | - | 1.9 | 2.1 | 1.6 | 1.6 | 1.7 | 1.9 |
| Patient Group | T0 | T1 | Increase | T2 | T3 | T4 |
|---|---|---|---|---|---|---|
| 6-month mixed | 6.3 | 14.8 | 8.7 | 15.3 | 14.4 | 13.8 |
| 6-month (*) | 6.5 | 15.2 | 8.7 | 14.6 | 13.4 | NA |
| 9-month (**) | 6.4 | 13.9 | 7.5 | 14.1 | 13.3 | 13.2 |
| 12-month (**) | 4.4 | 13.8 | 9.3 | 13.6 | 13.4 | 13.8 |
| Patient (N) | Gender/Age | Biopsy Location | BV/TV (%) | BS/TV (mm2/mm3) | Tb.Th (µm) | OV/BV (%) | OS/BS (%) | O.Th (µm) | N.Oc/BPM 1/mm2 |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F/53 | 16 | 40.5 | 2.4 | 335.8 | 6.9 | 38.8 | 342.2 | 0.62 |
| 2 | M/70 | 16 | 29.2 | 6.8 | 85.5 | 3.2 | 11.1 | 10.7 | 1.52 |
| 3 | M/68 | 14 | 19.7 | 6.9 | 57.5 | 7.6 | 17.9 | 11.6 | - |
| - | - | 15 | 29.3 | 6.5 | 91.2 | 3.5 | 12.9 | 11.7 | 2.54 |
| 4 | F/64 | 15 | 42.4 | 3.5 | 290.0 | 5.1 | 35.3 | 97.5 | 1.91 |
| 5 | M/51 | 16 | 18.3 | 2.2 | 163.4 | 16.3 | 39.8 | 481.9 | 1.58 |
| mean | - | - | 29.9 | 4.7 | 170.6 | 7.1 | 26.0 | 159.3 | 1.79 |
| SD | - | - | 10.1 | 2.3 | 116.6 | 4.8 | 13.4 | 203.5 | 0.5 |
| Patient Group | BV/TV (%) | SD ± | BS/TV (mm2/mm3) | SD ± | Tb.Th (µm) | SD ± | OV/BV (%) | SD ± | OS/BS (%) | SD ± | O.Th (µm) | SD ± | N.Oc/BPM 1/mm2 | SD ± |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 6-month mixed | 29.9 | 10.1 | 4.7 | 2.3 | 170.6 | 116.6 | 7.1 | 4.8 | 26.0 | 13.4 | 159.3 | 203.5 | 1.79 | 0.5 |
| 6-month (*) | 27.3 | 4.9 | 4.5 | 1.1 | 132.1 | 38.4 | 7.5 | 4.3 | 41.3 | 28.5 | 13.3 | 4.7 | 1.1 | 1.3 |
| 9-month (**) | 35.2 | 9.5 | 4.2 | 1.9 | 224.7 | 150.0 | 8.8 | 3.8 | 42.4 | 12.1 | 93.9 | 135.8 | 1.8 | 1.1 |
| 12-month (**) | 28.2 | 3.2 | 8.3 | 1.3 | 66.7 | 5.4 | 3.4 | 2.5 | 8.2 | 5.3 | 13.6 | 1.0 | *** | - |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bouwman, W.F.; Bravenboer, N.; ten Bruggenkate, C.M.; Schulten, E.A.J.M. The Use of Autogenous Bone Mixed with a Biphasic Calcium Phosphate in a Maxillary Sinus Floor Elevation Procedure with a 6-Month Healing Time: A Clinical, Radiological, Histological and Histomorphometric Evaluation. Coatings 2020, 10, 462. https://doi.org/10.3390/coatings10050462
Bouwman WF, Bravenboer N, ten Bruggenkate CM, Schulten EAJM. The Use of Autogenous Bone Mixed with a Biphasic Calcium Phosphate in a Maxillary Sinus Floor Elevation Procedure with a 6-Month Healing Time: A Clinical, Radiological, Histological and Histomorphometric Evaluation. Coatings. 2020; 10(5):462. https://doi.org/10.3390/coatings10050462
Chicago/Turabian StyleBouwman, Wilhelmus F., Nathalie Bravenboer, Christiaan M. ten Bruggenkate, and Engelbert A. J. M. Schulten. 2020. "The Use of Autogenous Bone Mixed with a Biphasic Calcium Phosphate in a Maxillary Sinus Floor Elevation Procedure with a 6-Month Healing Time: A Clinical, Radiological, Histological and Histomorphometric Evaluation" Coatings 10, no. 5: 462. https://doi.org/10.3390/coatings10050462
APA StyleBouwman, W. F., Bravenboer, N., ten Bruggenkate, C. M., & Schulten, E. A. J. M. (2020). The Use of Autogenous Bone Mixed with a Biphasic Calcium Phosphate in a Maxillary Sinus Floor Elevation Procedure with a 6-Month Healing Time: A Clinical, Radiological, Histological and Histomorphometric Evaluation. Coatings, 10(5), 462. https://doi.org/10.3390/coatings10050462





