Understanding General Practitioners’ Antibiotic Prescribing Decisions in Out-of-Hours Primary Care: A Video-Elicitation Interview Study
Abstract
1. Introduction
2. Methods and Materials
2.1. Study Context
2.2. Organisation of the Video-Observations
2.3. Study Design
2.4. Data Analysis
2.5. Ethics
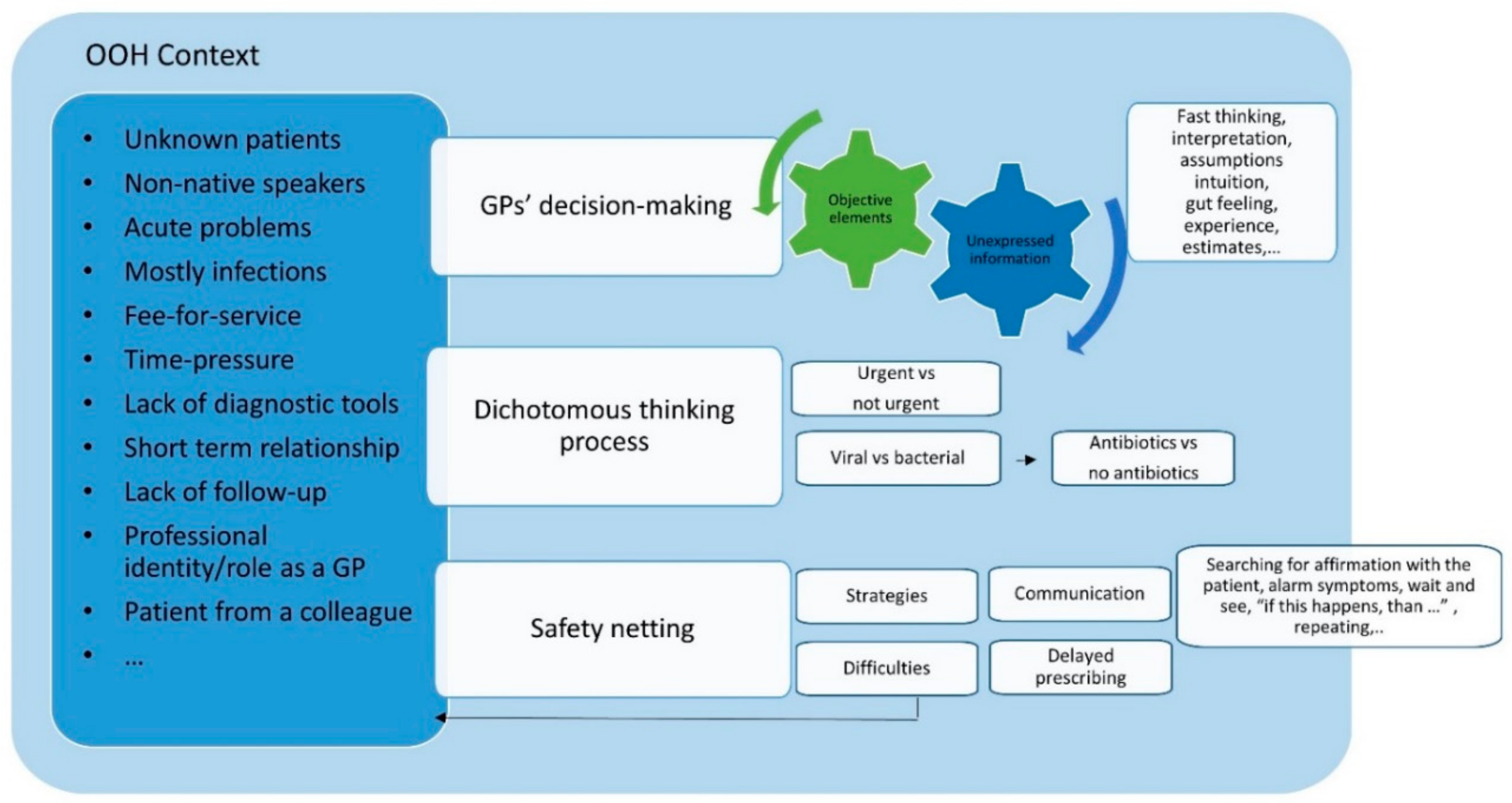
3. Results
- (1)
- Influence of unverified interpretation of information or assumptions
- (2)
- Dichotomous thinking and communication
- (3)
- Safety-netting: strategies and difficulties
3.1. Theme 1: Influence of Unverified Interpretation of Information or Assumptions
3.1.1. Exploring Ideas, Concerns and Expectations
3.1.2. Patient’s Presentation & GP’s Interpretation
3.2. Theme 2: Dichotomous Thinking and Communication
3.3. Theme 3: Safety-Netting: Strategies and Difficulties
4. Discussion
4.1. Main Findings
4.2. Strengths and Weaknesses/Limitations
4.3. Implications for Practice and Further Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- European Centre for Disease Prevention and Control, Antimicrobial Consumption Database (ESAC-Net). Available online: http://ecdc.europa.eu/en/healthtopics/antimicrobial-resistance-and-consumption/antimicrobial-consumption/esac-net-database/Pages/database.aspx (accessed on 10 February 2020).
- Colliers, A.; Coenen, S.; Philips, H.; Remmen, R.; Anthierens, S. Optimising the quality of antibiotic prescribing in out-of-hours primary care in Belgium: A study protocol for an action research project. BMJ Open 2017, 7, 017522. [Google Scholar] [CrossRef] [PubMed]
- Smits, M.; Colliers, A.; Jansen, T.; Remmen, R.; Bartholomeeusen, S.; Verheij, R. Examining differences in out-of-hours primary care use in Belgium and the Netherlands: A cross-sectional study. Eur. J. Public Health Oxf. 2019, 29, 1018–1024. [Google Scholar] [CrossRef] [PubMed]
- Colliers, A.; Adriaenssens, N.; Anthierens, S.; Bartholomeeusen, S.; Philips, H.; Remmen, R.; Coenen, S. Antibiotic Prescribing Quality in Out-of-Hours Primary Care and Critical Appraisal of Disease-Specific Quality Indicators. Antibiotics 2019, 8, 79. [Google Scholar] [CrossRef]
- Hayward, G.N.; Fisher, R.; Spence, G.; Lasserson, D. Increase in antibiotic prescriptions in out-of-hours primary care in contrast to in-hours primary care prescriptions: Service evaluation in a population of 600 000 patients. J. Antimicrob. Chemother. 2016, 71, 2612–2619. [Google Scholar] [CrossRef] [PubMed]
- Debets, V.E.; Verheij, T.J.; van der Velden, A.W. Antibiotic prescribing during office hours and out-of-hours: A comparison of quality and quantity in primary care in the Netherlands. Br. J. Gen. Pract. 2017, 67, 178–186. [Google Scholar] [CrossRef] [PubMed]
- Huibers, L.; Moth, G.; Christensen, M.B.; Vedsted, P. Antibiotic prescribing patterns in out-of-hours primary care: A population-based descriptive study. Scand. J. Prim. Health Care 2014, 32, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Colliers, A.; Coenen, S.; Remmen, R.; Philips, H.; Anthierens, S. How do general practitioners and pharmacists experience antibiotic use in out-of-hours primary care? An exploratory qualitative interview study to inform a participatory action research project. BMJ Open 2018, 8, 023154. [Google Scholar]
- Williams, S.; Halls, A.; Tonkin-Crine, S.; Moore, M.; Latter, S.; Little, P.; Eyles, C.; Postle, K.; Leydon, G. General practitioner and nurse prescriber experiences of prescribing antibiotics for respiratory tract infections in UK primary care out-of-hours services (the UNITE study). J. Antimicrob. Chemother. 2017, 73, 795–803. [Google Scholar] [CrossRef]
- Parry, R.; Pino, M.; Faull, C.; Feathers, L. Acceptability and design of video-based research on healthcare communication: Evidence and recommendations. Patient Educ. Couns. 2016, 99, 1271–1284. [Google Scholar] [CrossRef]
- Asan, O.; Montague, E. Using video-based observation research methods in primary care health encounters to evaluate complex interactions. Inform. Prim. Care 2014, 21, 161. [Google Scholar] [CrossRef]
- Colliers, A.; Coenen, S.; Remmen, R.; Philips, H.; Anthierens, S. Looking Inside the Out-of-Hours Primary Care Consultation: General Practitioners’ and Researchers’ Experiences of Using Video Observations as a Method. Int. J. Qual. Methods 2019, 18. [Google Scholar] [CrossRef]
- Henry, S.G.; Fetters, M.D. Video elicitation interviews: A qualitative research method for investigating physician-patient interactions. Ann. Fam. Med. 2012, 10, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Paskins, Z.; McHugh, G.; Hassell, A.B. Getting under the skin of the primary care consultation using video stimulated recall: A systematic review. BMC Med Res. Methodol. 2014, 14, 101. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cabral, C.; Ingram, J.; Lucas, P.J.; Redmond, N.M.; Kai, J.; Hay, A.D.; Horwood, J. Influence of clinical communication on parents’ antibiotic expectations for children with respiratory tract infections. Ann. Fam. Med. 2016, 14, 141–147. [Google Scholar] [CrossRef]
- Epstein, R. Attending: Medicine, Mindfulness, and Humanity; Simon and Schuster: New York, NY, USA, 2017. [Google Scholar]
- van Braak, M.; de Groot, E.; Veen, M.; Welink, L.; Giroldi, E. Eliciting tacit knowledge: The potential of a reflective approach to video-stimulated interviewing. Perspect. Med Educ. 2018, 7, 386–393. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Maguire, M.; Delahunt, B. Doing a thematic analysis: A practical, step-by-step guide for learning and teaching scholars. AISHE J All Irel. J. Teach. Learn. High. Educ. 2017, 9, 3351. [Google Scholar]
- Matthys, J.; Elwyn, G.; Van Nuland, M.; Van Maele, G.; De Sutter, A.; De Meyere, M.; Deveugele, M. Patients’ ideas, concerns, and expectations (ICE) in general practice: Impact on prescribing. Br. J. Gen. Pract. 2009, 59, 29–36. [Google Scholar] [CrossRef]
- Heritage, J.; Maynard, D.W. Communication in Medical Care: Interaction Between Primary Care Physicians and Patients; Cambridge University Press: Cambridge, UK, 2006; Volume 20. [Google Scholar]
- Kahneman, D. Thinking, Fast and Slow; Macmillan: London, UK, 2011. [Google Scholar]
- Van den Bruel, A.; Thompson, M.; Buntinx, F.; Mant, D. Clinicians’ gut feeling about serious infections in children: Observational study. BMJ 2012, 345, 6144. [Google Scholar] [CrossRef]
- Butler, C.C.; Rollnick, S.; Pill, R.; Maggs-Rapport, F.; Stott, N. Understanding the culture of prescribing: Qualitative study of general practitioners’ and patients’ perceptions of antibiotics for sore throats. BMJ 1998, 317, 637–642. [Google Scholar] [CrossRef]
- Cabral, C.; Ingram, J.; Hay, A.D.; Horwood, J. “They just say everything’s a virus”—Parent’s judgment of the credibility of clinician communication in primary care consultations for respiratory tract infections in children: A qualitative study. Patient Educ. Couns. 2014, 95, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Cals, J.W.; Butler, C.C.; Hopstaken, R.M.; Hood, K.; Dinant, G.J. Effect of point of care testing for C reactive protein and training in communication skills on antibiotic use in lower respiratory tract infections: Cluster randomised trial. BMJ 2009, 338, 1374. [Google Scholar] [CrossRef] [PubMed]
- Coenen, S.; Van Royen, P.; Michiels, B.; Denekens, J. Optimizing antibiotic prescribing for acute cough in general practice: A cluster-randomized controlled trial. J. Antimicrob. Chemother. 2004, 54, 661–672. [Google Scholar] [CrossRef]
- Little, P.; Stuart, B.; Francis, N.; Douglas, E.; Tonkin-Crine, S.; Anthierens, S.; Cals, J.W.L.; Melbye, H.; Santer, M.; Moore, M.; et al. Antibiotic Prescribing for Acute Respiratory Tract Infections 12 Months After Communication and CRP Training: A Randomized Trial. Ann. Fam. Med. 2019, 17, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Veldhuijzen, W.; Mogendorff, K.; Ram, P.; van der Weijden, T.; Elwyn, G.; van der Vleuten, C. How doctors move from generic goals to specific communicative behavior in real practice consultations. Patient Educ. Couns. 2013, 90, 170–176. [Google Scholar] [CrossRef][Green Version]
- Cabral, C.; Horwood, J.; Symonds, J.; Ingram, J.; Lucas, P.J.; Redmond, N.M.; Kai, J.; Hay, A.D.; Barnes, R.K. Understanding the influence of parent-clinician communication on antibiotic prescribing for children with respiratory tract infections in primary care: A qualitative observational study using a conversation analysis approach. BMC Fam. Pract. 2019, 20, 102. [Google Scholar] [CrossRef] [PubMed]
- Van Uum, R.; Sjoukes, A.; Venekamp, R.; Schilder, A.; De Groot, E.; Damoiseaux, R. Pain management in acute otitis media: An exploration of general practitioners’ views and expectations alongside a trial of an educational intervention. BJGP Open 2018. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.; Dunn, L.; Watt, I.; Macleod, U. Safety-netting for primary care: Evidence from a literature review. Br. J. Gen. Pract. 2019, 69, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Brookes-Howell, L.; Wood, F.; Verheij, T.; Prout, H.; Cooper, L.; Hood, K.; Melbye, H.; Torres, A.; Godycki-Cwirko, M.; Fernandez-Vandellos, P. Trust, openness and continuity of care as key ingredients for acceptance of antibiotic prescribing decisions for children with RTIs: A four-country, primary care qualitative study. Fam. Pract. 2013, 3, 102–110. [Google Scholar]
- McNiff, J.; Whitehead, J. All You Need to Know about Action Research; Sage Publications: Thousand Oaks, CA, USA, 2011. [Google Scholar]
- Paskins, Z.; Sanders, T.; Croft, P.R.; Hassell, A.B. Exploring the added value of video-stimulated recall in researching the primary care doctor–patient consultation: A process evaluation. Int. J. Qual. Methods 2017, 16. [Google Scholar] [CrossRef]
- Zulman, D.M.; Haverfield, M.C.; Shaw, J.G.; Brown-Johnson, C.G.; Schwartz, R.; Tierney, A.A.; Zionts, D.L.; Safaeinili, N.; Fischer, M.; Thadaney Israni, S.; et al. Practices to Foster Physician Presence and Connection With Patients in the Clinical Encounter. JAMA 2020, 323, 70–81. [Google Scholar] [CrossRef] [PubMed]
| Number of Participating GPs | 21 |
|---|---|
| Age in years Mean (SD) Median Range (min-max) | 43.1 (13.69) 39 26-64 |
| Years in practice Mean (SD) Median Range (min-max) | 15.7 (12.96) 12 1-38 |
| Gender distribution Male Female | 8 13 |
| Type of GP practice they work in during regular office hours (outside OOH care) Solo Duo Group Community health centre | 2 1 17 1 |
| GP trainee (GP in specialty training) | 2 |
| Duration of the interviews in minutes Mean (SD) Range (min-max) | 43′ (35′-50′) 34′-57′ |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Colliers, A.; Coenen, S.; Bombeke, K.; Remmen, R.; Philips, H.; Anthierens, S. Understanding General Practitioners’ Antibiotic Prescribing Decisions in Out-of-Hours Primary Care: A Video-Elicitation Interview Study. Antibiotics 2020, 9, 115. https://doi.org/10.3390/antibiotics9030115
Colliers A, Coenen S, Bombeke K, Remmen R, Philips H, Anthierens S. Understanding General Practitioners’ Antibiotic Prescribing Decisions in Out-of-Hours Primary Care: A Video-Elicitation Interview Study. Antibiotics. 2020; 9(3):115. https://doi.org/10.3390/antibiotics9030115
Chicago/Turabian StyleColliers, Annelies, Samuel Coenen, Katrien Bombeke, Roy Remmen, Hilde Philips, and Sibyl Anthierens. 2020. "Understanding General Practitioners’ Antibiotic Prescribing Decisions in Out-of-Hours Primary Care: A Video-Elicitation Interview Study" Antibiotics 9, no. 3: 115. https://doi.org/10.3390/antibiotics9030115
APA StyleColliers, A., Coenen, S., Bombeke, K., Remmen, R., Philips, H., & Anthierens, S. (2020). Understanding General Practitioners’ Antibiotic Prescribing Decisions in Out-of-Hours Primary Care: A Video-Elicitation Interview Study. Antibiotics, 9(3), 115. https://doi.org/10.3390/antibiotics9030115






