Antimicrobial Lock Therapy: A Strategy for Managing Catheter-Related Bacteremia
Abstract
1. Introduction
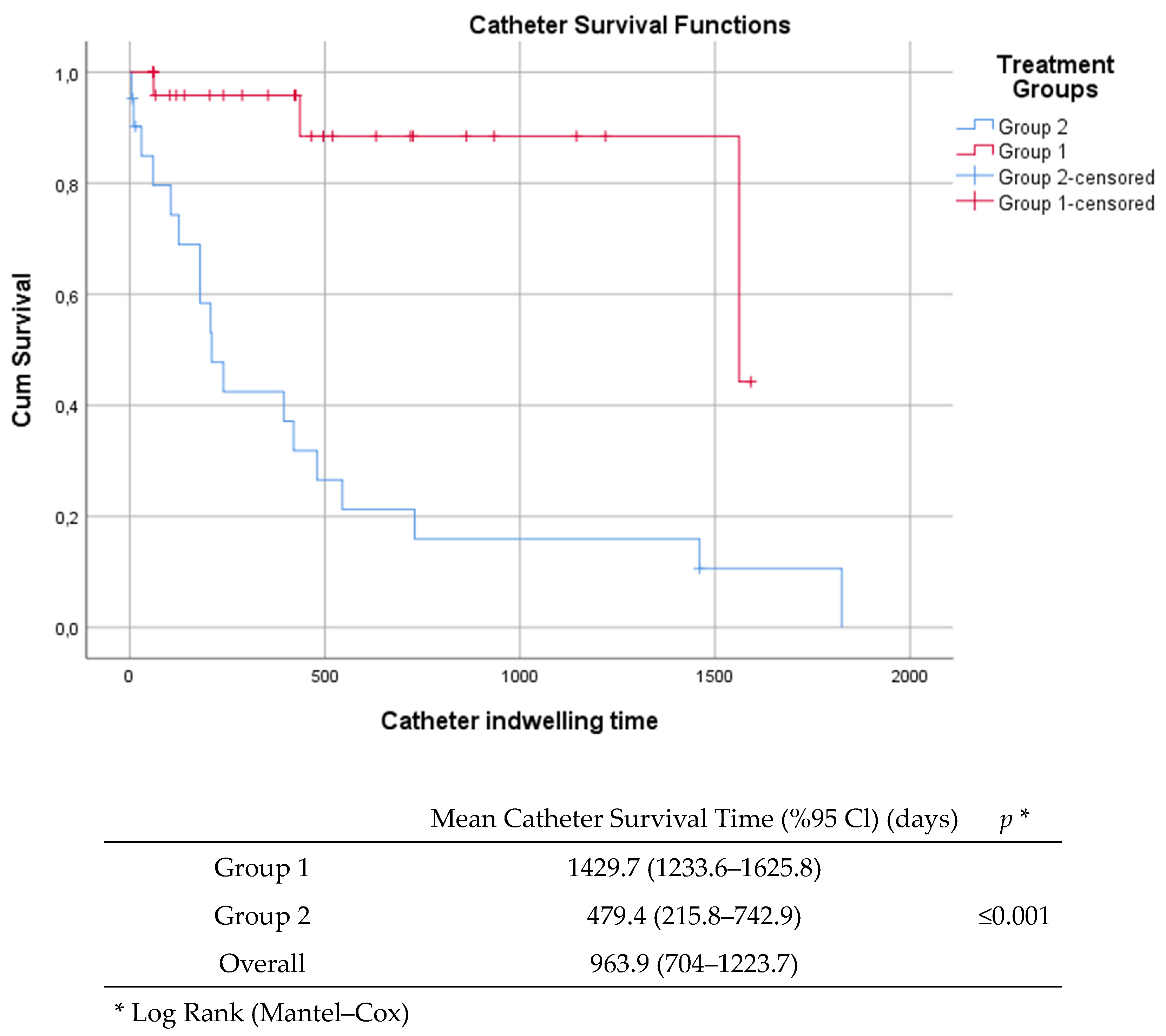
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Design and Setting
4.2. Participants
4.3. Data Collection
4.4. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Funalleras, G.; Fernández-Hidalgo, N.; Borrego, A.; Almirante, B.; Planes, A.M.; Rodríguez, D.; Ruiz, I.; Pahissa, A. Effectiveness of antibiotic-lock therapy for long-term catheter-related bacteremia due to Gram-negative bacilli: A prospective observational study. Clin. Infect. Dis. 2011, 53, e129–e132. [Google Scholar] [CrossRef] [PubMed]
- Alfieri, A.; Di Franco, S.; Passavanti, M.B.; Pace, M.C.; Simeon, V.; Chiodini, P.; Leone, S.; Fiore, M. Antimicrobial Lock Therapy in Clinical Practice: A Scoping Review. Microorganisms 2025, 13, 406. [Google Scholar] [CrossRef] [PubMed]
- Mayer, J.; Greene, T.; Howell, J.; Ying, J.; Rubin, M.A.; Trick, W.E.; Samore, M.H.; CDC Prevention Epicenters Program. Agreement in classifying bloodstream infections among multiple reviewers conducting surveillance. Clin. Infect. Dis. 2012, 55, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Alwazzeh, M.J.; Alnimr, A.; Al Nassri, S.A.; Alwarthan, S.M.; Alhajri, M.; AlShehail, B.M.; Almubarak, M.; Alghamdi, N.S.; Wali, H.A. Microbiological trends and mortality risk factors of central line-associated bloodstream infections in an academic medical center 2015–2020. Antimicrob. Resist. Infect. Control 2023, 12, 128. [Google Scholar] [CrossRef]
- Justo, J.A.; Bookstaver, P.B. Antibiotic lock therapy: Review of technique and logistical challenges. Infect. Drug Resist. 2014, 7, 343–363. [Google Scholar] [CrossRef]
- Raad, I.I.; Fang, X.; Keutgen, X.M.; Jiang, Y.; Sherertz, R.; Hachem, R. The role of chelators in preventing biofilm formation and catheter-related bloodstream infections. Curr. Opin. Infect. Dis. 2008, 21, 385–392. [Google Scholar] [CrossRef]
- Droste, J.C.; Jeraj, H.A.; MacDonald, A.; Farrington, K. Stability and in vitro efficacy of antibiotic-heparin lock solutions potentially useful for treatment of central venous catheter-related sepsis. J. Antimicrob. Chemother. 2003, 51, 849–855. [Google Scholar] [CrossRef]
- del Pozo, J.L. Role of antibiotic lock therapy for the treatment of catheter-related bloodstream infections. Int. J. Artif. Organs 2009, 32, 678–688. [Google Scholar] [CrossRef]
- Korbila, I.P.; Bliziotis, I.A.; Lawrence, K.R.; Falagas, M.E. Antibiotic-lock therapy for long-term catheter-related bacteremia: A review of the current evidence. Expert Rev. Anti Infect. Ther. 2007, 5, 639–652. [Google Scholar] [CrossRef]
- O’Grady, n.P.; Alexander, M.; Burns, L.A.; Dellinger, E.P.; Garland, J.; Heard, S.O.; Lipsett, P.A.; Masur, H.; Mermel, L.A.; Pearson, M.L.; et al. Guidelines for the prevention of intravascular catheter-related infections. Clin. Infect. Dis. 2011, 52, e162–e193. [Google Scholar] [CrossRef]
- Mermel, L.A.; Allon, M.; Bouza, E.; Craven, D.E.; Flynn, P.; O’Grady, N.P.; Raad, I.I.; Rijnders, B.J.; Sherertz, R.J.; Warren, D.K. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2009, 49, 1–45. [Google Scholar] [CrossRef]
- Bouhrour, n.; Nibbering, P.H.; Bendali, F. Medical Device-Associated Biofilm Infections and Multidrug-Resistant Pathogens. Pathogens 2024, 13, 393. [Google Scholar] [CrossRef]
- Fortún, J.; Grill, F.; Martín-Dávila, P.; Blázquez, J.; Tato, M.; Sánchez-Corral, J.; García-San Miguel, L.; Moreno, S. Treatment of long-term intravascular catheter-related bacteraemia with antibiotic-lock therapy. J. Antimicrob. Chemother. 2006, 58, 816–821. [Google Scholar] [CrossRef]
- Rijnders, B.J.; Van Wijngaerden, E.; Vandecasteele, S.J.; Stas, M.; Peetermans, W.E. Treatment of long-term intravascular catheter-related bacteraemia with antibiotic lock: Randomized, placebo-controlled trial. J. Antimicrob. Chemother. 2005, 55, 90–94. [Google Scholar] [CrossRef]
- Viale, P.; Pagani, L.; Petrosillo, N.; Signorini, L.; Colombini, P.; Macri, G.; Cristini, F.; Gattuso, G.; Carosi, G.; Italian Hospital and HIV Infection Group. Antibiotic lock-technique for the treatment of catheter-related bloodstream infections. J. Chemother. 2003, 15, 152–156. [Google Scholar] [CrossRef]
- O’Horo, J.C.; Silva, G.L.; Safdar, N. Anti-infective locks for treatment of central line-associated bloodstream infection: A systematic review and meta-analysis. Am. J. Nephrol. 2011, 34, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Tejwani, R.; Parry, M.F. Antimicrobial lock therapy as an adjunct to management of catheter-related bacteremia: A community hospital experience. Infect. Dis. Clin. Pract. 2011, 19, 256–261. [Google Scholar] [CrossRef]
- Schulin, T.; Voss, A. Coagulase-negative staphylococci as a cause of infections related to intravascular prosthetic devices: Limitations of present therapy. Clin. Microbiol. Infect. 2001, 7, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Blanco-Di Matteo, A.; Garcia-Fernandez, N.; Aguinaga Pérez, A.; Carmona-Torre, F.; Oteiza, A.C.; Leiva, J.; Del Pozo, J.L. In Vivo Effectiveness of Several Antimicrobial Locks to Eradicate Intravascular Catheter Coagulase-Negative Staphylococci Biofilms. Antimicrob. Agents Chemother. 2023, 67, e0126422. [Google Scholar] [CrossRef]
- Blanco-Di Matteo, A.; Garcia-Fernandez, N.; Aguinaga Pérez, A.; Carmona-Torre, F.; Oteiza, A.C.; Leiva, J.; Del Pozo, J.L. Pre-Emptive Antimicrobial Locks Decrease Long-Term Catheter-Related Bloodstream Infections in Hemodialysis Patients. Antibiotics 2022, 11, 1692. [Google Scholar] [CrossRef]
- Maya, I.D.; Carlton, D.; Estrada, E.; Allon, M. Treatment of dialysis catheter-related Staphylococcus aureus bacteremia with an antibiotic lock: A quality improvement report. Am. J. Kidney Dis. 2007, 50, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Freire, M.P.; Pierrotti, L.C.; Zerati, A.E.; Benites, L.; da Motta-Leal Filho, J.M.; Ibrahim, K.Y.; Araujo, P.H.; Abdala, E. Role of Lock Therapy for Long-Term Catheter-Related Infections by Multidrug-Resistant Bacteria. Antimicrob. Agents Chemother. 2018, 62, e00569-18. [Google Scholar] [CrossRef] [PubMed]
- von Dach, E.; Albrich, W.C.; Brunel, A.S.; Prendki, V.; Cuvelier, C.; Flury, D.; Gayet-Ageron, A.; Huttner, B.; Kohler, P.; Lemmenmeier, E.; et al. Effect of C-Reactive Protein-Guided Antibiotic Treatment Duration, 7-Day Treatment, or 14-Day Treatment on 30-Day Clinical Failure Rate in Patients with Uncomplicated Gram-Negative Bacteremia: A Randomized Clinical Trial. JAMA 2020, 323, 2160–2169. [Google Scholar] [CrossRef] [PubMed]
- Dias, R.F.; de Paula, A.C.R.B.; Hasparyk, U.G.; de Oliveira Rabelo Bassalo Coutinho, M.; Alderete, J.R.A.; Kanjongo, J.C.; Silva, R.A.M.; Guimarães, N.S.; Simões e Silva, A.C.; Nobre, V. Use of C-reactive protein to guide the antibiotic therapy in hospitalized patients: A systematic review and meta-analysis. BMC Infect. Dis. 2023, 23, 276. [Google Scholar] [CrossRef]

| Group 1 (n, %) | Group 2 (n, %) | Overall (n, %) | p | |
|---|---|---|---|---|
| Age (Sd) | 66.4 (13.7) | 66.2 (17.1) | 66.3 (15.4) | 0.951 |
| Sex (Female) | 8 (29.6) | 15 (55.6) | 23 (42.6) | 0.054 |
| Presence of comorbidity | ||||
| Hypertension | 16 (59.3) | 17 (63) | 33 (61.1) | 0.78 |
| Diabetes | 9 (33.3) | 12 (44.4) | 21 (38.9) | 0.577 |
| CCI median (Q1–3) | 6 (5–7) | 6 (4–7) | 6 (4–7) | 0.700 |
| Fever | 9 (33.3) | 16 (59.3) | 25 (46.3) | 0.056 |
| Follow up | ||||
| Duration of treatment (days), median (Q1–3) | 14 (10–14) | 14 (12–14) | 14 (10–14) | 0.599 |
| Catheter days, median (Q1–Q3) | 426 (129.5–723) | 180 (30–420) | 240 (84.5–588) | 0.052 |
| Time to follow-up culture (h), median (Q1–Q3) | 110 (96–120) | 33.5 (0–120) | 96 (44.5–120) | <0.0001 |
| Laboratory Parameters | ||||
| GPB | 20 (74.1) | 16 (59.3) | 36 (66.7) | 0.248 |
| GNB | 7 (25.9) | 11 (40.7) | 18 (33.3) | |
| CRP (mg/L, normal range: 0–5) On admission | 90 (159–56) | 122.5 (69.5–158.5) | 123 (59.8–173.3) | 0.457 |
| CRP (mg/L, normal range: 0–5) (48/72 h) | 69.9 (57.4) | 119.5 (75.8) | 91.6 (69.9) | 0.013 |
| CRP (mg/L, normal range: 0–5) (discharge/death) | 15 (9–40) | 20.5 (11–65) | 16 (9–46) | 0.291 |
| WBC counts (×109/L, normal range: 4–10) on admission | 8509.4 (3247.6) | 11,323.3 (4713) | 9916.4 (4252.9) | 0.014 |
| WBC counts (×109/L, normal range: 4–10) (48/72 h) | 7310.7 (3039.9) | 9239 (5248.2) | 8154.4 (4215.1) | 0.117 |
| WBC counts (×109/L, normal range: 4–10) (discharge/death) | 6308.1 (3054.8) | 7262.7 (2869.2) | 6649 (2990.5) | 0.328 |
| Outcome | ||||
| Positive follow-up culture | 3/27 (11.1) | 2/10 (20) | 5/37 (13.5) | 0.482 |
| Catheter removal | 3/27 (11.1) | 18/21 (85.7) | 21/48 (43.8) | <0.0001 |
| In-hospital mortality | 0 (0) | 3/27 (11.1) | 3/54 (5.6) | 0.236 |
| Group 1 (n = 27, %) | Group 2 (n = 27, %) | |
|---|---|---|
| Ampicillin | 3 (11%) | 1 (3.7%) |
| Cephalosporin | 5 (18.5%) | 7 (25.9%) |
| Cefazolin | 3 (11%) | 6 (22.2%) |
| Ceftriaxone | 2 (7.4%) | 1 (3.7%) |
| Carbapenem | 4 (14.8%) | 6 (22.2%) |
| Aminoglycoside | 1 (3.7%) | 4 (14.8%) |
| Glycopeptide | 12 (44.4%) | 12 (44.4%) |
| Vancomycin | 11 (41%) | 6 (22.2%) |
| Teicoplanin | 1 (3.7%) | 6 (22.2%) |
| Lipopeptide | 2 (7.4%) | 0 (0%) |
| Others | 0 (0%) | 2 (7.4%) |
| Antimicrobial | Concentration (mg/mL) | Heparin Concentration (UI/mL) |
|---|---|---|
| Vancomycin | 2.5 | 2500 |
| Ampicillin | 10 | 3000 |
| Cefazolin | 5 | 2500 |
| Daptomycin | 5 | 2500 |
| Gentamicin | 5 | 2500 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aksoy, F.; Karakoc Parlayan, H.N.; Oncu Kurutas, G.; Yilmaz, G. Antimicrobial Lock Therapy: A Strategy for Managing Catheter-Related Bacteremia. Antibiotics 2025, 14, 461. https://doi.org/10.3390/antibiotics14050461
Aksoy F, Karakoc Parlayan HN, Oncu Kurutas G, Yilmaz G. Antimicrobial Lock Therapy: A Strategy for Managing Catheter-Related Bacteremia. Antibiotics. 2025; 14(5):461. https://doi.org/10.3390/antibiotics14050461
Chicago/Turabian StyleAksoy, Firdevs, Hanife Nur Karakoc Parlayan, Gulter Oncu Kurutas, and Gurdal Yilmaz. 2025. "Antimicrobial Lock Therapy: A Strategy for Managing Catheter-Related Bacteremia" Antibiotics 14, no. 5: 461. https://doi.org/10.3390/antibiotics14050461
APA StyleAksoy, F., Karakoc Parlayan, H. N., Oncu Kurutas, G., & Yilmaz, G. (2025). Antimicrobial Lock Therapy: A Strategy for Managing Catheter-Related Bacteremia. Antibiotics, 14(5), 461. https://doi.org/10.3390/antibiotics14050461





